Purpose of review
Due to the stringent measures including quarantine of infected individuals and social distancing, the COVID-19 pandemic has posted great challenges for HIV-1 care in China. In this mini-review, I will discuss the situation in Shenzhen city as a window of China to reflect our strategies in fighting the concurrent HIV/AIDS and COVID-19 pandemics.
Recent findings
Prevention of nosocomial infection, minimizing the follow-up visits to the hospital, maintaining the delivery of PreP/PEP services and testing for SARS-Cov-2 and HIV when someone have fever or respiratory symptoms were the four major approaches to maintain uninterrupted HIV care in Shenzhen. None of 15 000 PLWH seeking HIV care at Shenzhen were diagnosed with COVID-19 during this pandemic.
Summary
This article share the experience unprecedented from Shenzhen. We have to adapt our care and service to continue to engage PLWH to avoid poor outcomes. More research is needed to know the long-term implications of pandemic for the health of PLWH.
Keywords: antiretroviral therapy, coronavirus, nosocomial infection, people living with HIV, SARS-Co-2
INTRODUCTION
Novel coronavirus pneumonia, which was named coronavirus disease 2019 (COVID-19) by the WHO, is a new acute viral disease mainly transmitted through small droplets that infect the respiratory tract. COVID-19 had spread rapidly since the first reports from Wuhan, China in December 2019, and the outbreak was declared as a pandemic by the WHO on 12 March 2020. As of 25 June 2020, more than 9.4 million cases have been confirmed worldwide, and 480 000 people have died in this pandemic [1]. Shenzhen, located in the southern part of China and adjacent to Hong Kong, is a pioneering area for China's economic reform and the relaxing policy. Each year, a large number of migrant workers move to the city for job opportunities, and it only takes 4 h to reach Shenzhen from Wuhan by high-speed train. Therefore, the situation of prevention and control of the COVID-19 epidemic in Shenzhen is challenging. Shenzhen Third People's Hospital is the only hospital specialized in management of infectious diseases in Shenzhen and is responsible for inpatient and outpatient care of individuals affected by both COVID-19 and HIV infection. The hospital is one of the largest HIV treatment sites in China and manages nearly 15 000 people living with HIV (PLWH). During the epidemic period from January to June, 462 patients with COVID-19 were admitted to the hospital, with 39 from abroad and 3 deaths. The COVID-19 pandemic presented several barriers and challenges to the HIV care continuum. For example, in Wuhan, hospital visits were banned because of the implementation of city lockdown or traffic controls [2▪▪]. In the whole country, PLWH are faced with ART (antiretroviral therapy) interruption; according to the reports, approximately 32.6% of the PLWH are at risk of ART interruption; and 48.6% do not know where to acquire antiretroviral drugs in the near future [3▪,4]. Moreover, high-risk populations cannot get access to preexposure and postexposure prophylaxis (PrEP and PEP) services on time, which might result in resurgence of new cases of HIV infection [5▪]. In this report, we would like to share our experience regarding how our hospital managed PLWH during the pandemic and how we were able to maintain zero cases of COVID-19 among PLWH.
Box 1.
no caption available
Promptly relocate the resources of the hospital after the outbreak to prevent nosocomial infection
The Shenzhen government has attached great importance to the Third People's hospital, because it is the only hospital specialized in infectious diseases. A large amount of funding has been invested in the renovation and construction of the hospital and refurbishment of equipment for the treatment of respiratory diseases after SARS outbreak in 2003. Negative-pressure rooms were well equipped, and the layout of the hospital was separated into various zones based on the type of disease, transmission routes and patients. Our hospital admitted the first case of a COVID-19 patient on 11 January 2020, which was also the first case in Guangdong Province. In the following days, the number of cases increased significantly, and the maximum number of patients admitted was 50 for 1 day, already exceeding the hospital capacity for management of patients with respiratory diseases. The hospital immediately adjusted its layout and suspended the treatment for patients in the other departments under the coordination of the Shenzhen Municipal Health Commission. Patients with noncommunicable diseases were transferred to other hospitals for uninterrupted care. The layout of the hospital was divided into three main zones, contaminated, potentially contaminated, and clean, from inside to the outside and from north to the south (Fig. 1). As HIV infection is not an airborne infectious disease, the wards and clinics for PLWH were moved to the clean zone at the outermost and southernmost areas of the hospital, completely separated from the COVID-19 zone. The entrances and exits are also divided into COVID-19 exclusive and other relatively clean ones. Entry into all zones follows a strict disinfection procedure. Alcohol spray is used every 2 h in the HIV care facilities, and the medical staff strictly implement wearing face mask, hand hygiene and disinfection, which effectively protects the patients from coronavirus infection in the hospital [6].
FIGURE 1.
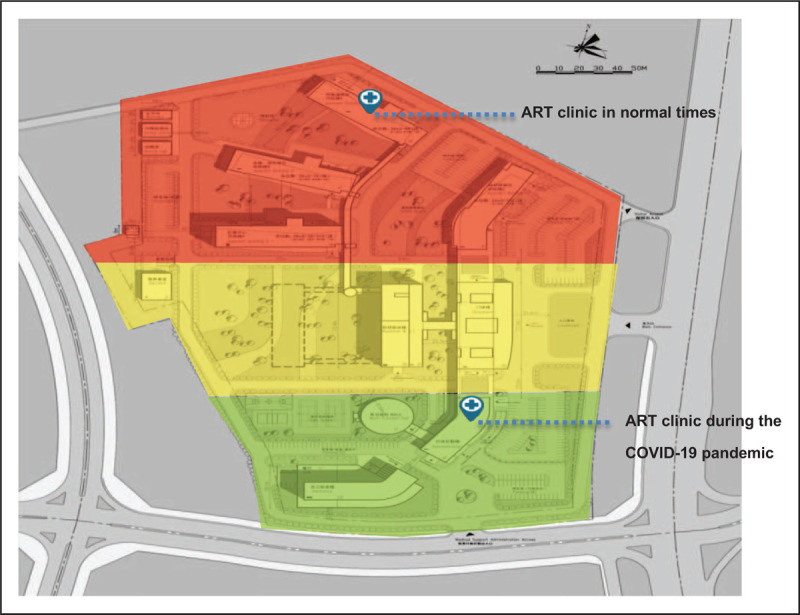
The general layout of the hospital during the corona virus disease 2019 pandemic. Red, contaminated zone; yellow, potentially contaminated zone; green, clean zone.
Minimize the number of follow-up visits to the hospital for antiretroviral therapy
As there is currently no effective vaccine against HIV, PLWH have to receive lifelong antiretroviral therapy (ART) to improve the quality of life and extend their lifespan. Our focus during and after the COVID-19 outbreak is to minimize the visits of patients who have been receiving ART in Shenzhen and to provide their medications and care needed in time. The measures we take are as follows:
-
(1)
Patients who insist on coming to the hospital are given 3 months’ refill of medications. For the individuals with other comorbidities, we prescribe a 3-month supply of those medications as well. Patients are advised to take their medicine at home, to avoid going out or gatherings, and to wear masks when necessary.
-
(2)
For patients who are concerned about being infected with COVID-19 and do not dare to come to the hospital, we use express delivery of the medicine, which effectively guarantees their treatment uninterrupted during the pandemic.
-
(3)
A hotline is established to provide counseling and consultation. Thus, the safety of the patients taking the medications can be ensured.
-
(4)
For those who are affected by the lockdown outside Shenzhen, we will issue a referral letter for them online and contact the local HIV doctors by phone to ensure that the patients can get care and medications as needed.
Ensure delivery of preexposure and postexposure prophylaxis services to stop new HIV infections during the coronavirus disease 2019 pandemic
As our hospital is one of the clinical sites for ‘China Real-world Orally intake PrEP (CROPrEP)’ cohort, we need to maintain regular follow-up for the participants when COVID-19 occurred. To avoid cross-infection and save medical resources, we work together with nongovernmental organizations (NGOs) to provide HIV self-testing package and 3-month refill by express delivery; moreover, NGOs also help to collect the test results that are uploaded on the digital platform.
On the other hand, before COVID-19, the average amount of PEP reached as high as 200–250 cases per month in our hospital, which has reduced above 50% during the COVID-19 pandemic. In order to provide emergent PEP service to reduce new HIV infections, we utilized Tel-medication system to enable remote consultation, prescription, and drug delivery. To provide real-time counseling for HIV prevention, we also establish a hotline to answer questions from the high-risk groups.
Test for SARS-CoV-2 and HIV in patients who present with respiratory symptoms and pneumonia
Fever and cough are the main symptoms of COVID-19, which are challenging to differentiate from the pulmonary infections of PLWH who present late for HIV care. Therefore, many newly diagnosed PLWH during this period were misdiagnosed with COVID-19 when they present with fever and cough and interstitial pneumonia on chest imaging. In this regard, medical staff should consider HIV infection when the patients test negative for Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). Newly diagnosed PLWH during the pandemic are required to undergo nucleic-acid amplification testing as well as antibody testing for COVID-19 at the specialized hospitals within 3 days before seeking HIV care at this hospital. People who come to the hospital in person directly are allowed to be in contact with other people only after they test negative for SARS-CoV-2 with the use of nucleic-acid amplification and antibody testing in an isolated room.
CONCLUSION
In summary, our HIV care delivery focuses on protecting PLWH who are immunosuppressed from contracting COVID-19, especially those with CD4 cells below 200 cells/μl and those with other chronic diseases. During this pandemic, the Chinese National Center for AIDS/STD Control and Prevention issued a notice guaranteeing a free, uninterrupted antiretroviral drug supply and released a list of ART clinics for PLWH to refill ART in China [4]. With that guarantee, we have adopted the above-mentioned interventions and measures to effectively continue HIV care to protect the health of PLWH in Shenzhen. None of the 15000 PLWH seeking HIV care at this hospital were diagnosed with COVID-19 during this pandemic. However, the current pandemic is not yet over, and the characteristics of COVID-19 remain to be further studied. More investigations are warranted to identify the most efficient mode of sustainable delivery of HIV care and prevention in ensuring that HIV control is not stalled by the COVID-19 pandemic [5▪,7▪,8▪,9▪,10▪].
Acknowledgements
I would like to thank Drs. Zhiwei Chen and Linqi Zhang for giving this opportunity to share our experience.
Financial support and sponsorship
This work was supported by The Shenzhen Sanming Project of Medicine (SZSM201512029) from 2015 to 2020 to H.W. and Zhiwei Chen.
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). Gisanddata.maps.arcgis.com. (2020). Retrieved 25 June 2020. Available at: https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740f.
- 2▪▪.Jiang H, Zhou Y, Tang W. Maintaining HIV care during the COVID-19 pandemic. Lancet HIV 2020; 7:e308–e309. [DOI] [PMC free article] [PubMed] [Google Scholar]; Many locations are facing the risk of SARS-CoV-2 infection and barriers and challenges for maintaining the HIV care continuum during the COVID-19 pandemic.
- 3▪.Wei G, Huiling W, Hua B, et al. Quick community survey on the impact of COVID-19 outbreak for the healthcare of people living with HIV. Chin J Epidemiol 2020; 41:662–666. [DOI] [PubMed] [Google Scholar]
- 4.UNAIDS and China working together during the COVID-19 outbreak to ensure that people living with HIV continue to get treatment. Unaids.org. (2020). Retrieved 1 April 2020. Available at: https://www.unaids.org/en/resources/presscentre/pressreleaseandstatementarchive/2020/february/20200218_china_covid19.
- 5▪.Q&A: HIV, antiretrovirals and COVID-19. Who.int. (2020). Available at: https://hivgaps.org/wpcontent/uploads/2020/03/WHO-QA-on-COVID-19-HIV-and-ARVs.pdf.; This interim guidance reviews special considerations for persons with HIV and their heath care in USA during the COVID-19 pandemic.
- 6.Huang T, Guo Y, Li S, et al. Application and effects of fever screening system in the prevention of nosocomial infection in the only designated hospital of coronavirus disease 2019 (COVID-19) in Shenzhen, China. Infect Control Hosp Epidemiol 2020; 1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7▪.Zhao S, Cao P, Chong M, et al. COVID-19 and gender-specific difference: Analysis of public surveillance data in Hong Kong and Shenzhen, China, from January 10 to February 15, 2020. Infect Control Hosp Epidemiol 2020; 41:750–751. [DOI] [PMC free article] [PubMed] [Google Scholar]; This paper shared the experience of maintaining HIV care in Thailand during the COVID-19 pandemic.
- 8▪.Thai hospitals to provide three- to six-month supplies of antiretroviral therapy. Unaids.org. (2020). 25 March 2020. Available at: https://www.unaids.org/en/resources/presscentre/featurestories/2020/march/20200325_thailand.
- 9▪.Interim guidance for COVID-19 and persons with HIV (Interim Guidance). AIDSinfo. (2020). Last Updated: June 19, 2020. Available at: https://aidsinfo.nih.gov/guidelines/html/8/covid-19-and-persons-with-hiv--interim-guidance-/554/interim-guidance-for-covid-19-and-persons-with-hiv; UNAIDS is working to ensure continued provision of HIV prevention and treatment service during the COVID-19 pandemic.
- 10▪.WHAT PEOPLE LIVING WITH HIV NEED TO KNOW ABOUT HIV AND COVID-19. Unaids.org. (2020). Retrieved 1 April 2020. Available at: https://www.unaids.org/en/resources/documents/2020/HIV_COVID-19_brochure.; This paper offer the experience regarding the fever screening system in the prevention of nosocomial infection at designated hospital of COVID-19 in Shenzhen, China.


