Corresponding Author

Key Words: COVID-19, echocardiography, inflammation, myocaardial injury, SARS-CoV-2, troponin
Since the first case of coronavirus disease-2019 (COVID-19) that was reported in Wuhan (China) in late 2019, this infectious pathology has reached pandemic status, affecting many millions of patients worldwide and causing a very large number of deaths. A critical progression of disease in around 5% to 10% of infected individuals, who need intensive care, imposes the adoption of an efficient prognostication, aimed at delivering more appropriate treatments and optimizing the usage of health care in a world with limited resources. The clinical evolution of COVID-19, which can often progress from mild respiratory symptoms to severe lung involvement and multiple organ injury, is a paradigmatic example of disease needing accurate risk stratification for preventing rapid and sustained clinical deterioration.
An increase in the circulating values of cardiac troponins has long been used for diagnosing myocardial injury, irrespective of its ischemic, toxic, immune-mediated, traumatic, and even infectious (i.e., both viral and bacterial) origin (1,2). Evidence has been provided that cardiac troponin elevations are associated with disease severity in patients with severe acute respiratory syndrome-coronavirus (SARS-CoV) infection, the virus causing SARS nearly 20 years ago and which is genetically homologous to SARS-CoV-2, the underlying pathogen of COVID-19 (3). Data are also progressively accumulating, attesting to the possible prognostic role of cardiac troponins in patients with COVID-19 (4, 5, 6). Some meta-analyses and reviews have also confirmed that higher values of cardiac troponin I in COVID-19 are significant predictors of severe COVID-19 illness (7, 8, 9), thus providing clear evidence that SARS-CoV-2 infection may be associated with various degrees of cardiac injury and dysfunction (10). Puntmann et al. (11) recently assessed the occurrence of myocardial injury in 100 patients hospitalized for COVID-19. Cardiac magnetic resonance (CMR) revealed the presence of abnormal CMR findings (i.e., raised myocardial native T1, raised myocardial native T2, myocardial late gadolinium enhancement, and pericardial enhancement) in 78% of cases and myocardial inflammation in 60%. During hospitalization, high-sensitivity cardiac troponin T (hs-cTnT) levels were found to be significantly increased (13.9 ng/l or even higher) in 15 patients (15%) whereas, at the time of performing CMR, detectable levels of hs-cTnT (i.e., ≥3 ng/l) were found in the vast majority of patients (i.e., 71%) recently recovered from COVID-19, with some of them displaying even values of ≥13.9 ng/l. Importantly, hs-cTnT values were predictive of some CMR abnormalities.
In the paper published by Giustino et al. (12) in this issue of the Journal, cTn values were measured at hospital admission or during hospitalization, for diagnosing myocardial injury and predicting the outcome of COVID-19 patients (12). Notably, patients with elevated values of this cardiac injury biomarker had more electrocardiographic abnormalities, higher values of inflammatory biomarkers, and increased prevalence of significant echocardiographic abnormalities. Cardiac structural abnormalities were detected in around 65% of COVID-19 patients with myocardial injury undergoing transthoracic echocardiography (TTE), and in-hospital mortality increased among those patients in parallel with increasing levels of cTnI, especially in those with echocardiographic abnormalities. Importantly, although failing to reach statistical significance, Giustino et al. (12) reported that the body mass index was higher in the group of patients with myocardial injury than in those without (29.1 vs. 26.5 kg/m2). This is a substantial aspect because obese patients tend to experience worse outcomes and more critical illness in COVID-19 and are known to have more cardiac structural and functional abnormalities on TTE or other cardiac imaging, as well as more comorbidities associated with worse outcomes (13,14). Current statistics indicate that 75% of the U.S. population is either overweight or obese, whereas over 42% meet obesity criteria by a body mass index of 30 kg/m2 or higher and over 9% have body mass index of 40 kg/m2 or higher, indicating Class III, severe, or morbid obesity (15). Interestingly, the cohort in these New York City and Milan hospitals were leaner than in most major U.S. cities.
The current recommendations of the American College of Cardiology (ACC) endorse the measurement of cTn levels when a diagnosis of acute myocardial infarction is being considered in patients with SARS-CoV-2 infection. This indication seems somehow inadequate according to the information collected by Giustino et al. (12), whereby there is now evidence that Tn-positive COVID-19 patients may benefit from routine TTE, which would allow practitioners to garner useful prognostic information and to establish specific therapeutic options in patients with cardiac injury. In keeping with this suggestion, ACC criteria shall also be expanded in all patients infected with COVID-19, not only those with a clinical suspicion of cardiac ischemia. Several lines of evidence now attest that cardiac injury in COVID-19 patients may be triggered by a multitude of different but convergent causes, encompassing certainly thrombosis in cardiac arteries and subsequent myocardial ischemia, but also encompassing direct cytopathic damage of cardiomyocytes and endothelial cells directly caused by SARS-CoV-2, along with inflammatory and immune injuries (16). A severe myocardial involvement can then be associated with pump failure and cardiac dysfunction, leading to hypoxia and increased systemic inflammatory responses (5). Because cTn elevations are commonplace due to many of these pathogenetic pathways, the clinical usefulness of routinely measuring these biomarkers in all patients hospitalized for COVID-19 seems straightforward.
Due to the increased number of patients with COVID-19, hospitals are facing an unprecedented burden on available resources, so that clinicians increasingly need prognostic tools that may enable targeted and tailored treatments (17). Normal or nonevolving cTn levels, along with normal values of other biomarkers of inflammation (e.g., C-reactive protein, ferritin) or cardiac dysfunction (e.g., natriuretic peptides), may safely reduce the need to perform routine tests such as TTE and stress testing in patients admitted with dyspnea and chest pain related to COVID-19 (18). Khanji et al. (18) have recently reviewed the potential for handheld ultrasound as a potential fast, efficient, and cost-effective echocardiographic screening modality in COVID-19 and other pandemics and clinical situations. Higher values of these biomarkers, even with normal liver and renal function tests, may instead reflect the presence of cardiac and/or initial multiple organ injury, thus reflecting unfavorable disease progression. Finally, coronary angiography may be advisable in patients with cTn elevations and clinical symptoms suggestive of acute coronary syndrome/acute myocardial infarction.
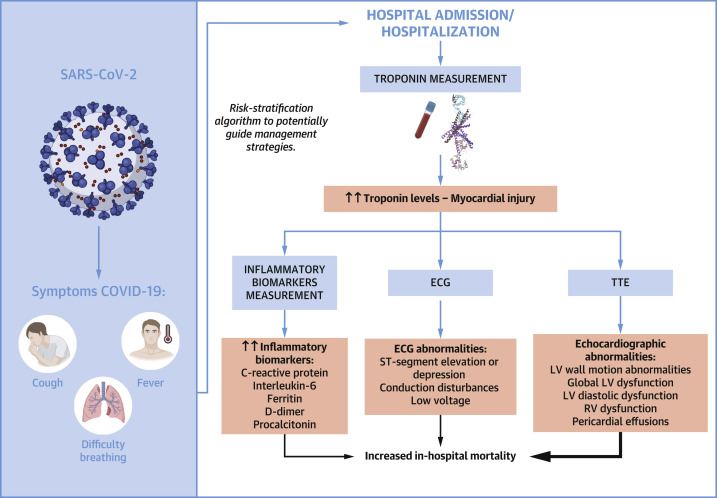
cTns play an important role in evaluating disease severity and/or mortality in SARS-CoV-2 infection. Hence, we endorse routine serial measurement of these biomarkers in patients hospitalized for COVID-19 with TTE, at least handheld or full, for most of those with high values (Figure 1 ). We congratulate the esteemed investigator group from the United States and Italy for this excellent data in this issue of the Journal (12). Despite the limitations of a relatively small number of participants (n = 305) and selection bias for who specifically received assessment with Tn, electrocardiography, and TTE, this study provides very practical evidence to improve current clinical practice during this and possibly other such pandemics. Because of the potential for myocarditis and the cardiac abnormalities that Puntmann et al. (11) noted following COVID-19 with CMR, the professional sports leagues are currently performing routine TTE in all their players who have recovered from COVID-19 and now have positive antibodies. Although this approach may be ideal considering the exercise intensities and costs involved with high-level professional athletes, this is likely not practical for all people, even athletes and heavy exercisers who have recovered fully from this illness and who are without worrisome cardiovascular symptoms or signs. Long-term follow-up of patients who have recovered from COVID-19 will be required to further influence routine clinical practices.
Figure 1.
Myocardial Injury Evaluation Scheme in COVID-19 Patients
This chart illustrates the clinical evolution and the specific assessment of myocardial injury performed by Giustino et al. (12) in patients with coronavirus disease-2019 (COVID-19). ECG = electrocardiogram; LV = left ventricle; RV = right ventricle; SARS-CoV-2 = severe acute respiratory syndrome coronavirus 2; TTE = transthoracic echocardiographic.
Footnotes
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the JACCauthor instructions page.
References
- 1.Musher D.M., Abers M.S., Corrales-Medina V.F. Acute infection and myocardial infarction. N Engl J Med. 2019;380:171–176. doi: 10.1056/NEJMra1808137. [DOI] [PubMed] [Google Scholar]
- 2.Pizzini A., Burkert F., Theurl I., Weiss G., Bellmann-Weiler R. Prognostic impact of high sensitive troponin T in patients with influenza virus infection: a retrospective analysis. Heart Lung. 2020;49:105–109. doi: 10.1016/j.hrtlng.2019.05.009. [DOI] [PubMed] [Google Scholar]
- 3.Zhu N., Zhang D., Wang W. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lala A., Johnson K.W., Januzzi J.L. for the Mount Sinai COVID Informatics Center. Prevalence and impact of myocardial injury in patients hospitalized with COVID-19 infection. J Am Coll Cardiol. 2020;76:533–546. doi: 10.1016/j.jacc.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guo T., Fan Y., Chen M. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5:811–818. doi: 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang D., Hu B., Hu C. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lippi G., Lavie C.J., Sanchis-Gomar F. Cardiac troponin I in patients with coronavirus disease 2019 (COVID-19): evidence from a meta-analysis. Prog Cardiovasc Dis. 2020;63:390–391. doi: 10.1016/j.pcad.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li J.W., Han T.W., Woodward M. The impact of 2019 novel coronavirus on heart injury: a systematic review and meta-analysis. Prog Cardiovasc Dis. 2020 Apr 16 doi: 10.1016/j.pcad.2020.04.008. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bavishi C., Bonow R.O., Trivedi V., Abbott J.D., Messerli F.H., Bhatt D.L. Acute myocardial injury in patients hospitalized with COVID-19 infection: a review. Prog Cardiovasc Dis. 2020 Jun 6 doi: 10.1016/j.pcad.2020.05.013. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aggarwal G., Cheruiyot I., Aggarwal S. Association of cardiovascular disease with coronavirus disease 2019 (COVID-19) severity: a meta-analysis. Curr Probl Cardiol. 2020;45:100617. doi: 10.1016/j.cpcardiol.2020.100617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Puntmann V.O., Carerj M.L., Wieters I. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020 Jul 27 doi: 10.1001/jamacardio.2020.3557. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Giustino G., Croft L.B., Stefanini G.G. Characterization of myocardial injury in patients with COVID-19. J Am Coll Cardiol. 2020;76:2043–2055. doi: 10.1016/j.jacc.2020.08.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lavie C.J., Laddu D., Arena R., Ortega F.B., Alpert M.A., Kushner R.F. Healthy weight and obesity prevention: JACC Health Promotion Series. J Am Coll Cardiol. 2018;72:1506–1531. doi: 10.1016/j.jacc.2018.08.1037. [DOI] [PubMed] [Google Scholar]
- 14.Sanchis-Gomar F., Lavie C.J., Mehra M.R., Henry B.M., Lippi G. Obesity and outcomes in COVID-19: when an epidemic and pandemic collide. Mayo Clin Proc. 2020;95:1445–1453. doi: 10.1016/j.mayocp.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sharma A., Garg A., Rout A., Lavie C.J. Obesity is associated with more critical illness in COVID-19. Mayo Clin Proc. 2020;95:2040–2042. doi: 10.1016/j.mayocp.2020.06.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Knowlton K.U. Pathogenesis of SARS-CoV-2 induced cardiac injury from the perspective of the virus. J Mol Cell Cardiol. 2020;147:12–17. doi: 10.1016/j.yjmcc.2020.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chapman A.R., Bularga A., Mills N.L. High-sensitivity cardiac troponin can be an ally in the fight against COVID-19. Circulation. 2020;141:1733–1735. doi: 10.1161/CIRCULATIONAHA.120.047008. [DOI] [PubMed] [Google Scholar]
- 18.Khanji M.Y., Ricci F., Patel R.S. The role of hand-held ultrasound for cardiopulmonary assessment during a pandemic. Prog Cardiovasc Dis. 2020 Jul 10 doi: 10.1016/j.pcad.2020.07.003. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]