Abstract
Objective:
To evaluate the effects of laser monotherapy on quality of life in breast cancer patients with chronic radiation dermatitis.
Study Design:
A prospective, IRB-approved study was conducted at Memorial Sloan Kettering Cancer Center. Breast cancer patients with chronic radiation dermatitis completed health-related quality of life (HR-QOL) questionnaires before and after laser monotherapy for radiation-induced breast telangiectasias (RIBT).
Methods:
After informed consent, all patients were issued theSkindex-16 and Breast-QAdverse Effects of Radiation HR-QOL questionnaires prior to receiving laser treatment. Patients were treated with a 595 nm pulsed dye laser at 4- to 6-week intervals, with percent telangiectasia clearance and adverse events recorded at each visit. Post-treatment HR-QOL questionnaires were collected after clinician-assessed telangiectasia clearance of >50%. Median HR-QOL scores before and after therapy were reported for individual HR-QOL domains (Skindex-16) and HR-QOL totals (Skindex-16 and Breast-Q Adverse Effects of Radiation). Before- and after-differences were calculated using the Wilcoxon Signed-Rank Test.
Results:
Twenty-two female patients (average age 56 years) enrolled in this study. A majority (13/22, 59%) exhibited telangiectasias across the décolletage and axilla in addition to the breast. Sixteen patients reached the 50% RIBT clearance threshold during the study period, and 11 of these patients (69%) completed follow-up HR-QOL questionnaires. Patients showed statistically significant improvements in emotional and functional Skindex-16 HR-QOL domains and in overall Skindex-16 HR-QOL score. Breast-Q scores also improved significantly, illustrating a decrease in specific physical and cosmetic concerns common to radiated breast skin. Common adverse events were transient post-treatment pain and redness.
Conclusion:
Breast cancer patients with RIBT presented with substantial deficits in several HR-QOL arenas. Laser monotherapy effectively treated the appearance of radiation dermatitis in these patients and also significantly improved HR-QOL.
Keywords: breast cancer, health related quality of life, pulsed dye laser, radiation dermatitis, telangiectasias
INTRODUCTION
Breast cancer is predicted to account for 30% of all malignancies that will be diagnosed in women in 2017, excluding non-melanoma skin cancers [1]. Because adjuvant radiation therapy (RT) is standard of care for locally advanced breast carcinoma following lumpectomy or total mastectomy, many breast cancer survivors experience treatment sequelae such as radiation dermatitis long after tumor extirpation.
Chronic radiation dermatitis may arise from months to several years after treatment. Common clinical manifestations include hypo- or hyperpigmentation, skin atrophy, fibrosis, breast retraction, and telangiectasias. Radiation-induced breast telangiectasias (RIBT) arise secondary to reduced or poorly supported vasculature in radiated breast skin, and have been reported to occur in 7.8–31.4% of radiated breast cancer patients [2–4]. The isolated or diffuse telangiectasias that appear across the breast cancer patient’s radiated skin field can affect health-related quality of life (HR-QOL)s through physical discomfort, perceived disfigurement, and cosmetic dissatisfaction. RIBT may further promote emotional distress by serving as a constant and tangible reminder of the patient’s breast cancer.
The efficacy and safety of the pulsed dye laser (PDL) in RIBT treatment has been previously described [5,6]. While improved psychosocial health following treatment has been illustrated qualitatively [5], HR-QOL has not been assessed with validated patient reported outcome (PRO) instruments. This study aimed to quantify patient HR-QOL before and after vascular laser therapy in order to evaluate the effect of RIBT and treatment on physical and psychosocial well-being.
MATERIALS AND METHODS
Study Design
For this prospective, single-center study, subjects completed HR-QOL questionnaires before and after PDL therapy for RIBT. The Institutional Review Board of Memorial Sloan-Kettering Cancer Center approved the study, and all patients provided written informed consent prior to questionnaire administration and laser treatment.
Inclusion and Exclusion Criteria
Inclusion criteria were oral and written informed consent, verbal and written English-language fluency, age greater than 18 years, Fitzpatrick skin type I–IV, history of breast cancer treated with surgery and adjuvant radiation, presence of telangiectasias in the radiation field of the treated breast, and request for PDL treatment of RIBT. Exclusion criteria were current oral steroid use, daily therapeutic anticoagulation, pregnancy or lactation, prior laser therapy for RIBT, and presence of suntan in area to be treated.
Data Collection
Data collected from each patient were age, type of breast cancer surgery, date of RT completion, presence and grade of any acute radiation dermatitis, time between RT and RIBT appearance, and RIBT locations. Specific RT information included type, dose, and number of fractions and was obtained from records supplied by the patient’s treating radiation oncologist. Finally, treating clinicians (AR, EL, KN) assigned numerical scores to three clinical telangiectasia parameters for each patient, with increasing score corresponding to increasing clinical severity. Parameters and scales were as follows: telangiectasia distribution, 1 (patchy) to 4 (diffuse); telangiectasia color, 1 (pink) to 7 (purple); telangiectasia diameter, 1 (thin, <1 mm), 2 (medium, 1 mm), and 3 (thick, >1 mm). Minimum and maximum possible clinical RIBT severity scores were, therefore, 3 and 14, respectively.
PRO Instruments
Following informed consent and prior to PDL treatment, all patients were given two validated PRO instruments intended to measure HR-QOL.
The Skindex-16 is an instrument developed to study the effects on HR-QOL of a wide variety of dermatologic diseases [7,8]. The 16-item questionnaire inquires about effects of the skin condition on three HR-QOL domains: physical skin symptoms (4 items; e.g., itching, hurting), emotions (7 items, e.g., worry, embarrassment), and social or physical functioning (5 items; e.g., social interactions, work). Patients report how often they are bothered by each item using a 7-box bipolar scale anchored by the phrases “never bothered” to “always bothered.” Individual item, domain, and total scores are transformed to a linear scale ranging from 0 to 100, with a higher score indicating worse HR-QOL.
The Breast-Q is a multi-module PRO instrument developed at Memorial Sloan-Kettering Cancer Center to evaluate concerns unique to breast cancer patients [9,10]. The Breast-Q Adverse Effects of Radiation module asks the patient to quantify how often she is bothered by six physical and cosmetic concerns (appearance of pigmentation and telangiectasias, xerosis, sensitivity to touch, skin thickness, skin irritation) specific to radiated breast skin. Patients report how often they are bothered by each item on a scale from 1 to 3 (“a lot,” “a little,” “not at all”). Raw scores are then added to create total scale score. Using a Rasch Unidimensional Measurement model (RUMM) Conversion Table, each raw scale total score is converted to a value from 0 (worst) to 100 (best).
Intervention
Patients were treated with a 595 nm pulsed dye laser at 4- to 6-week intervals. Laser settings were based on those delineated by Nymann et al. [11]. Given the fragile nature of radiated breast tissue, the lowest fluence needed to produce transient purpura and erythema was used during each treatment.
Clinical Evaluation
Participants were asked to provide a pain score on a scale from 0 (no pain) to 10 (highest pain imaginable) at every session. From the second treatment onward, patients reported any adverse events along with number of days of pain, redness, and crusting after the prior treatment. Also from the second treatment onward, clinicians recorded any pigment change and measured percent telangiectasia clearance in quartiles (0–25%, 25–50%, 50–75%, and 75–100% clearance from baseline).
In order to assess post-treatment HR-QOL, the Skindex-16 and Breast-Q Adverse Effects of Radiation were again administered once the clinician deemed RIBT clearance to have reached a threshold of at least 50%.
Statistical Analysis
Data collected for this study is presented using descriptive statistics. Median HR-QOL scores before and after PDL therapy are reported for individual HR-QOL domains (Skindex-16) and HR-QOL totals (Skindex-16 and Breast-Q Adverse Effects of Radiation). Before- and after-differences were calculated using the Wilcoxon Signed-Rank Test.
RESULTS
Patient Population
Twenty-two patients enrolled in this study between March 2013 and November 2016. Patient characteristics are illustrated in Table 1. All 22 patients had been treated surgically with mastectomies, and most patients (55%) did not undergo breast reconstruction following RT. A majority of patients (64%) experienced mild to moderate (grades 1 and 2) acute radiation dermatitis during RT. On average, patients presented for PDL therapy 7.7 years (SD 4.1) after RT, although most (73%) recalled their RIBT appearing within 1 year of RT completion. RIBT were found across the chest wall, axilla, and décolletage, with most patients (59%) exhibiting telangiectasias across all three sites at once.
TABLE 1.
Enrolled Patient Characteristics
| Enrolled patients (N = 22) | |
|---|---|
| Age (years) | |
| Mean (SD) | 56.0 (8.8) |
| Range | 39–69 |
| Reconstruction, n (%) | |
| None | 12 (54.5) |
| Saline implant | 1 (4.5) |
| Silicone implant | 8 (36.4) |
| Flap | 1 (4.5) |
| Radiation dose to chest wall, n (%) | |
| 4,800 cGY, 24 fractions | 1 (4.5) |
| 5,000 cGY, 25 fractions | 11 (50.0) |
| 5,040 cGY, 28 fractions | 7 (31.8) |
| Information not available | 3 (13.6) |
| Acute radiation dermatitis grade, n (%)a | |
| Grade 1 | 4 (18.2) |
| Grade 2 | 10 (45.5) |
| Grade 3 | 5 (22.7) |
| Grade 4 | 2 (9.1) |
| No acute radiation dermatitis reported | 1 (4.5) |
| Time between RT and RIBT appearance n (%) | |
| < 6 months | 8 (36.4) |
| 6–12 months | 8 (36.4) |
| >1–2 years | 2 (9.1) |
| > 2 years | 3 (13.6) |
| Not reported | 1 (4.5) |
| Years since RT | |
| Mean (SD) | 7.7 (4.1) |
| Range | 2–17 |
| Clinical RIBT severity score | |
| Mean (SD) | 7.0 (1.6) |
| Range | 3–10 |
| Telangiectasia location, n (%) | |
| Chest wall/breast | 2 (9.1) |
| Chest wall/breast and axilla | 3 (13.6) |
| Chest wall/breast and décolletage | 4 (18.2) |
| Chest wall/breast, axilla, and décolletage | 13 (59.1) |
SD, standard deviation; RT, radiation therapy; RIBT, radiation-induced breast telangiectasias.
Grade 1, faint erythema or dry desquamation; Grade 2, moderate to brisk erythema, patchy moist desquamation, mostly confined to skin folds and creases, moderate edema; Grade 3, moist desquamation other than skin folds and creases, bleeding induced by minor trauma or abrasion; Grade 4, skin necrosis or ulceration of full thickness dermis, spontaneous bleeding from involved site.
RIBT Clearance With PDL
Three patients were lost to follow-up after their first treatment and could not be assessed for telangiectasia clearance. Two patients who returned for second treatments and one patient who returned for third and fourth treatments were subsequently lost to follow-up before reaching the 50% RIBT clearance threshold. Treatment parameters for the 16 patients in whom >50% RIBT clearance was achieved are reported in Table 2. Ninety-one percent of treatments used 10 mm spot size, with typical pulse durations of 6 and 3 milliseconds (41% and 52%, respectively) and fluences of 7 and 8 J/cm2 (50% and 46%, respectively). Although the PDL was able to clear at least 50% of a majority (69%) of patients’ RIBT after one session (Fig. 1), many patients went on to receive further treatments until they reached the 75–100% clearance quartile (Figs. 2 and 3). Of note, treatment parameters were recorded across 10 of the 11 treatments in the six patients who were lost to follow-up before reaching >50% clearance. These parameters did not differ substantially from those of the rest of the study population (90% used 10 mm spot size, 60% used 6 milliseconds and 40% used 3 milliseconds pulse duration, 60% used 7 J/cm2, and 40% used 8 J/cm2 fluence).
TABLE 2.
Treatment Parameters (N = 44 Treatments in 16 Patients)
| 595 nm pulsed dye laser | |
|---|---|
| Spot size, n (%)a | |
| 10 mm | 40 (90.9) |
| 7 mm | 3 (6.8) |
| NR | 1 (2.3) |
| Pulse duration, n (%)a | |
| 6 ms | 18 (40.9) |
| 3 ms | 23 (52.3) |
| 1.5ms | 2 (4.5) |
| NR | 1 (2.3) |
| Fluence, n (%)a | |
| 7 J/cm2 | 22 (50.0) |
| 8 J/cm2 | 20 (45.5) |
| 9 J/cm2 | 2 (4.5) |
| No. treatments to >50% RIBT clearance, n (%)b | |
| 1 | 11 (68.8) |
| 2 | 2 (12.5) |
| 3 | 2 (12.5) |
| 4 | 1 (6.2) |
| Average no. treatments to >50% RIBT clearance | 1.6 |
RIBT, radiation-induced breast telangiectasias.
N = 44 treatments.
N = 16 patients.
Fig. 1.
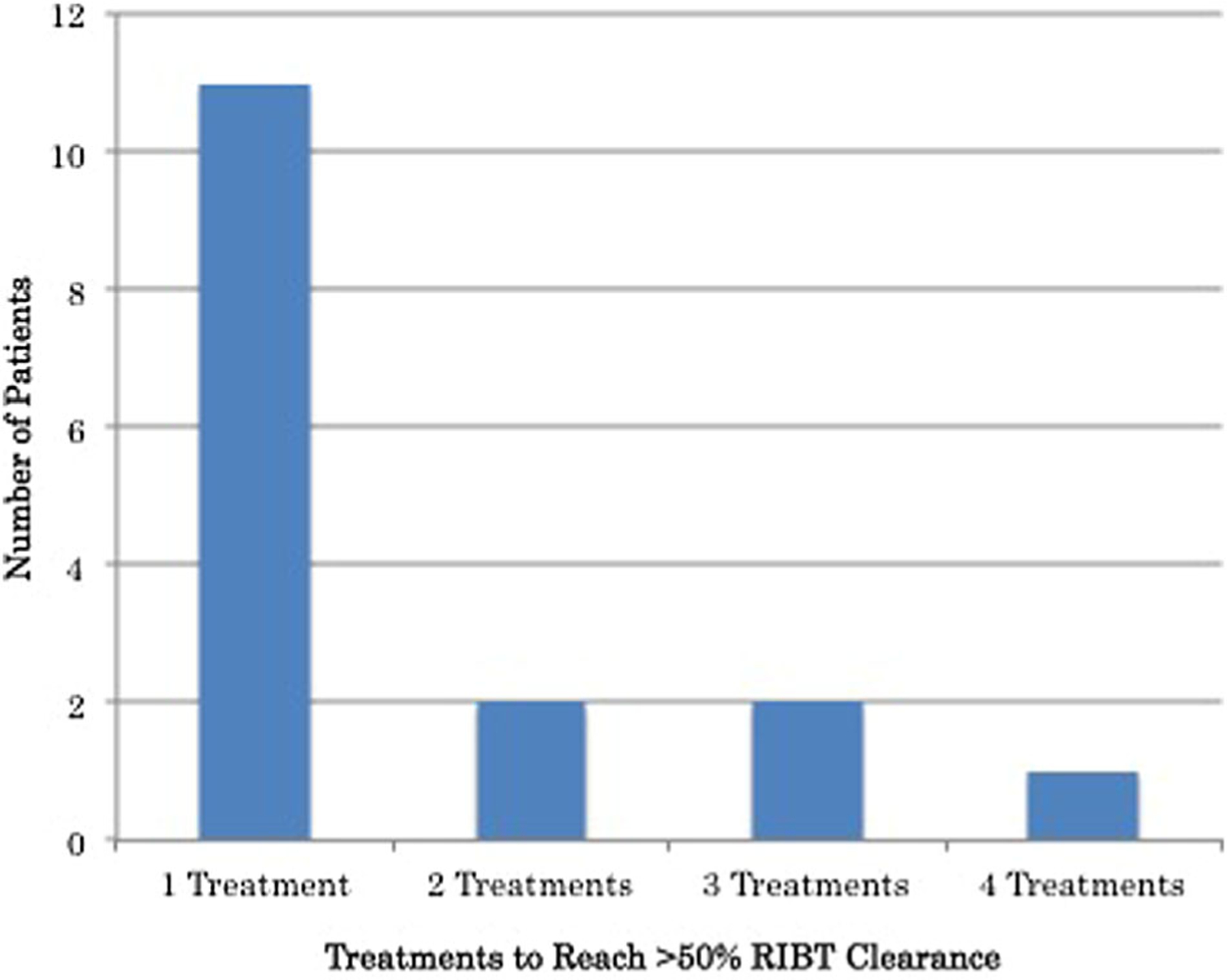
Number of treatments needed to reach >50% RIBT clearance. RIBT, radiation-induced breast telangiectasias.
Fig. 2.
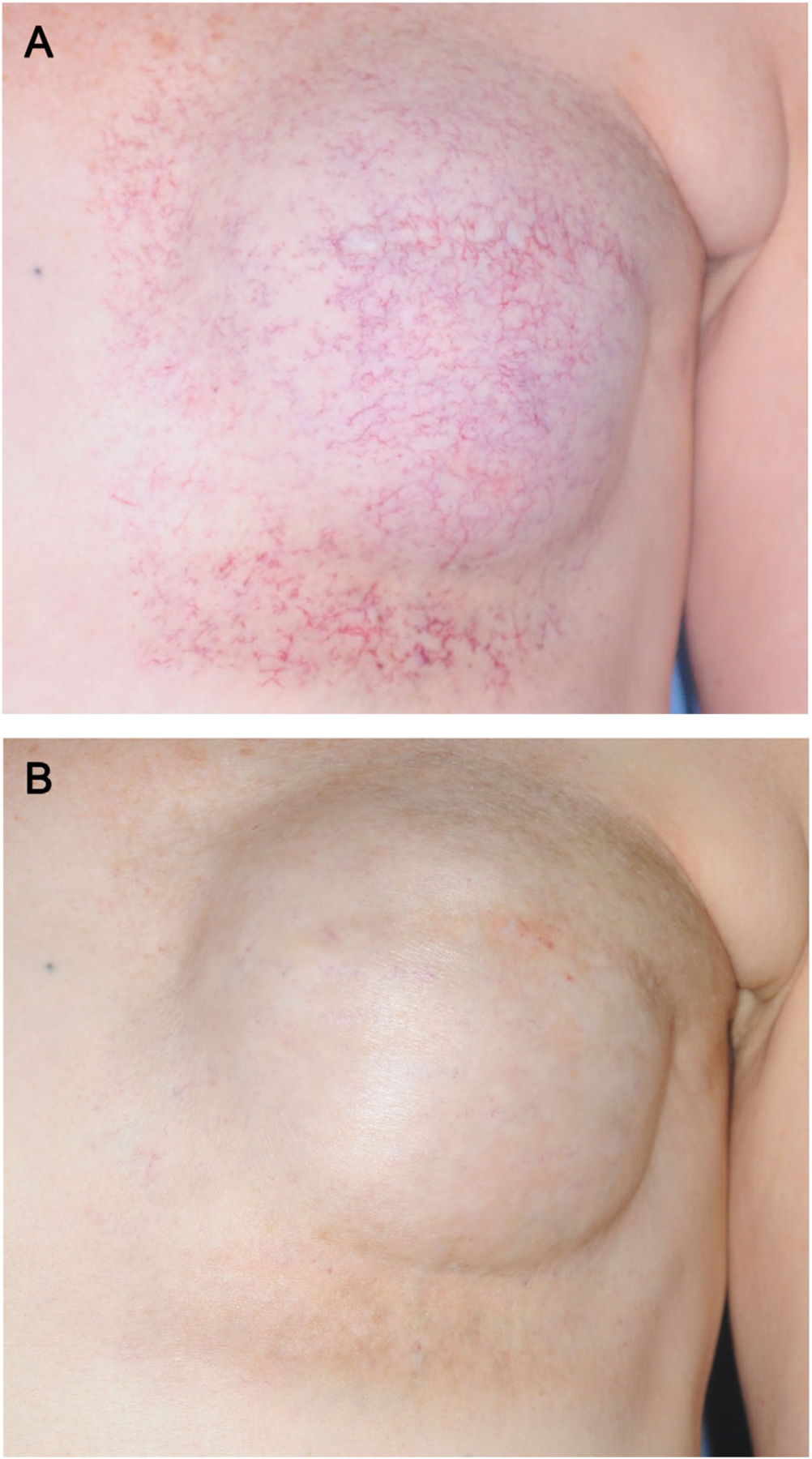
Clinical improvement in RIBT following treatment with the 595 nm PDL. (A) RIBT, reported to have arisen within 6 months of radiation therapy 10 years prior, distributed across the chest wall and breast. (B) 75–100% reduction in RIBT burden 4 weeks after the last of three laser treatments (10 mm spot size, average fluence 7 J/cm2, 1.5–3 milliseconds pulse duration). RIBT, radiation-induced breast telangiectasias; PDL, pulsed-dye laser.
Fig. 3.
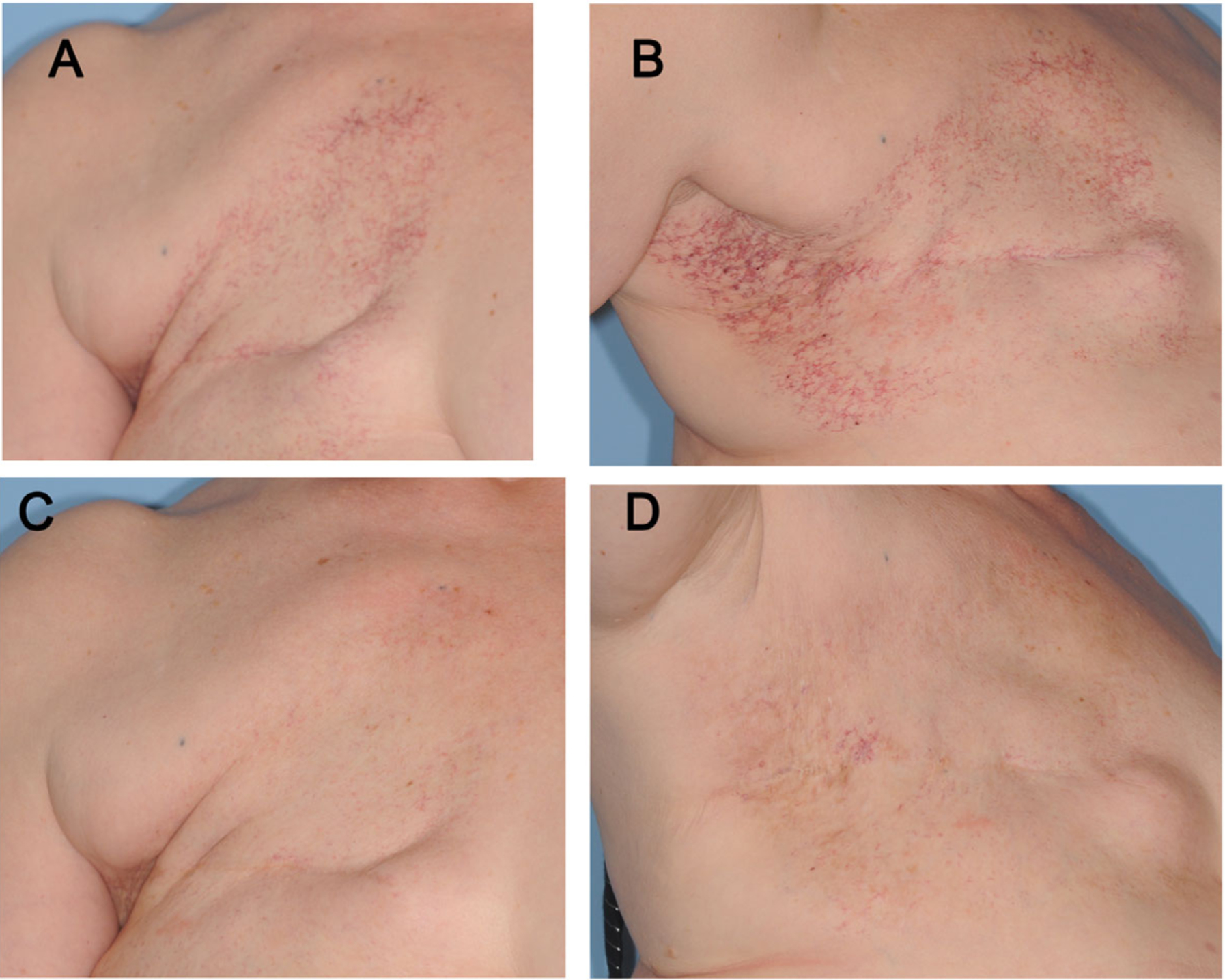
Clinical improvement in RIBT following treatment with the 595 nm PDL. (A) Pre-treatment RIBT across the chest wall and décolletage. (B) This patient’s RIBT also extended up into her axilla. (C) Frontal and (D) axillary views 4 weeks after treatment number two, with 75–100% clearance (10 mm spot size, average fluence 7 J/cm2, 3 milliseconds pulse duration). RIBT, radiation-induced breast telangiectasias; PDL, pulsed dye laser.
HR-QOL Improvement
Of 16 patients treated to or beyond the 50% RIBT clearance threshold, 11 (69%) completed follow-up HR-QOL questionnaires. Median HR-QOL scores across these 11 patients demonstrated statistically significant improvement as measured by both the Skindex-16 and the Breast-Q. Upon evaluation of individual Skindex-16 domains, patients reported statistically significant improvements in both emotional and functional realms (Fig. 4). Prior to treatment, patients sustained greatest HR-QOL deficit in the emotional Skindex-16 domain. Individual question review indicated that items referring to “embarrassment about your skin condition” and “appearance of your skin condition” were the most negatively scored. Assessment of individual Breast-Q items illustrated worst baseline HR-QOL scores for the question specifically asking about visible RIBT marks.
Fig. 4.

HR-QOL scores before (blue bars) and after (red bars) PDL treatment to >50% RIBT clearance. HR-QOL, health-related quality of life; PDL, pulsed-dye laser; RIBT, radiation-induced breast telangiectasias. *P < 0.05.
To assess whether improvement in HR-QOL paralleled degree of clinical improvement, the change in HR-QOL before and after PDL treatment was analyzed separately in the group who completed post-treatment HR-QOL questionnaires after reaching 50–75% clearance (7 patients) and in the group who completed post-treatment HR-QOL questionnaires after reaching 75–100% clearance (4 patients). Though the 75–100% group had a 1.9-point greater improvement in Skindex-16 score (1.9; 95%CI: −22.3 to 31.3, P = 0.68) and 6.4-point greater improvement in Breast-Q score (6.4; 95%CI: −14.6 to 27.5, P = ¼ 0.55) after treatment, these were not statistically significant differences.
Adverse and Patient/Clinician-Reported Treatment Events
PDL therapy was generally well tolerated by patients, with post-procedure pain, redness, and crusting rarely lasting more than 1 week after treatment. This data is recorded for the 16 patients in whom >50% RIBT clearance was achieved in Table 3. Of note, patient- and clinician-reported treatment events across the six patients lost to follow-up before reaching 50% did not differ from the rest of the study population. Average pain score, recorded for six of 11 total sessions, was 6/10. For the three of these patients who returned after their first treatments, average number of days of post-procedure redness, pain, and crusting were 6, 1.5, and 1.1, respectively.
TABLE 3.
Patient- and Clinician-Reported Treatment Events (N = 44 Treatments in 16 Patients)
| 595 nm pulsed dye laser | |
|---|---|
| Intra-procedure pain scorea,b | |
| Mean (SD) | 6.0 (2.2) |
| Range | 1–10 |
| Post-procedure redness (days)c | |
| Mean (SD) | 5.9 (4.5) |
| Range | 0–17 |
| Post-procedure pain (days)d | |
| Mean (SD) | 1.5 (2.5) |
| Range | 0–9 |
| Post-procedure crusting (days)c | |
| Mean (SD) | 1.2 (3.0) |
| Range | 0–12 |
| Pigment change, n (%)e | |
| None | 10 (66.7) |
| Hypopigmentation | 1 (6.7) |
| Hyperpigmentation | 4 (26.7) |
SD, standard deviation.
Patients asked to report pain on a scale from 0 (no pain) to 10 (worst imaginable pain) during treatment.
Data available for 34 visits.
Data available for 30 visits.
Data available for 31 visits.
N = 15 patients.
There was one incident of cutaneous ulceration of the inframammary fold with resulting breast implant compromise secondary to PDL therapy. The patient had undergone two treatments spaced 4 weeks apart using 10 mm spot size, 7 J/cm2 fluence, and 3 milliseconds pulse duration to the upper breast, décolletage, and inframammary fold. She completed a post-treatment HR-QOL questionnaire, having reached >50% RIBT clearance, and received no further treatment thereafter.
DISCUSSION
Though breast cancer has become increasingly prevalent, there is a paucity of literature regarding chronic radiation dermatitis and its treatment. Life saving measures such as surgery and radiation may have unintended sequelae that lead to declines in functional or emotional quality of life. Patients uninformed about potential long-term effects of cancer treatments may be ill-equipped to cope with the concomitant quality of life impairments. Breast telangiectasias are one sequela of radiation therapy that may be physically and emotionally distressing in addition to being cosmetically concerning. Whelan et al. reported that over 20% of patients had at least grade 1 skin toxicity at 5- and 10-year follow-up after standard or hypofractionated radiotherapy [12]. HR-QOL is an important consideration when assessing patients for treatment of this common sequela of RT as well as for post-treatment follow-up.
Compared to baseline, all but one patient in this study had improvement in both Breast-Q and Skindex-16 HR-QOL scores after laser therapy for RIBT. Breast-Q score improvement illustrates that specific physical and cosmetic concerns common to radiated breast skin bothered patients less after laser therapy. Across patients, all three Skindex-16 domains—functional, emotional, and physical—demonstrated improvement, with the emotional domain score showing the greatest change over time. This underscores that while chronic radiation dermatitis may have a physically disfiguring effect, it can also carry with it a significant emotional burden. Patients treated in this study discussed several psychosocial effects of RIBT, including embarrassment by its physical appearance and distress induced by the tangible reminder of their breast cancer. Throughout therapy, multiple patients commented that treating the areas helped to improve self-esteem, intimate interactions, and daily activities.
Our data did not show a significant difference in HR-QOL improvement in patients who reached 75–100% clearance compared with those who completed post-treatment QOL questionnaires after 50–75% clearance. That HR-QOL improvement does not necessarily parallel degree of clinical RIBT clearance may suggest that the process of undergoing laser therapy at all is enough to yield substantial HR-QOL improvement. This said, the sample sizes for these calculations are small and warrant future study.
The PDL showed good efficacy in treating RIBT in this study, with at least 50% clearance achieved through a range of one to four treatment sessions. The most common treatment reactions were post-laser pain, purpura, and erythema, events that were all transient and expected. While this laser is relatively non-invasive, we did experience one episode of cutaneous ulceration in radiated inframammary skin after PDL treatment prompting breast implant exchange. This event, reported previously [13], was thought to occur secondary to increased radiation exposure in the inframammary fold and poor muscle coverage over the silicone implant predisposing the tissue to breakdown. The event highlights the importance of treating radiated skin conservatively, given its delicate nature and poorer wound healing. Specifically, it is prudent to avoid compromised skin and atrophied areas without muscle coverage such as the inframammary fold.
In order to minimize confounders such as different lasers or laser operators, this study was carried out at a single site, which limited the study’s sample size. Another limitation of this study is relatively short follow-up time. Future studies might include several centers using identical lasers and laser parameters and might also follow patients for longer time periods in order to determine whether RIBT recur after PDL treatment and at what rate. PDL adjuvants such as topical rapamycin and longer-wavelength PDL alternatives such as the Alexandrite laser, which have been used in the port-wine stain population with mixed results [14–16], may also be of interest for future study in RIBT treatment.
Within our patient population, RIBT were reported to arise roughly 1 year after radiation. While this finding is subject to recall bias, it might be used to prompt earlier discussions about chronic radiation-induced skin changes after breast cancer treatment. This could lead to earlier intervention, and, subsequently, earlier alleviation of associated impairments in HR-QOL.
CONCLUSION
The psychosocial impact of an illness and its treatment is particularly salient in oncology, as life-saving interventions may have unanticipated and distressing sequelae. We demonstrated that RIBT causes HR-QOL impairment in afflicted patients and that RIBT treatment can yield substantial improvement in multiple HR-QOL spheres. As breast cancer survivorship increases, it is of paramount importance to identify chronic treatment sequelae and their effects on HR-QOL in order to optimize physical and psychosocial health for this population in the long term.
ACKNOWLEDGMENT
This research was funded in part through the NIH/NCI Cancer Center Support Grant P30 CA008748.
Footnotes
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported.
REFERENCES
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2017. CA Cancer J Clin 2017;67(1):7–30. [DOI] [PubMed] [Google Scholar]
- 2.Spalek M Chronic radiation-induced dermatitis: Challenges and solutions. Clin Cosmet Investig Dermatol 2016;9: 473–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lilla C, Ambrosone CB, Kropp S, et al. Predictive factors for late normal tissue complications following radiotherapy for breast cancer. Breast Cancer Res Treat 2007;106(1):143–150. [DOI] [PubMed] [Google Scholar]
- 4.Pignol JP, Truong P, Rakovitch E, Sattler MG, Whelan TJ, Olivotto IA. Ten years results of the Canadian breast intensity modulated radiation therapy (IMRT) randomized controlled trial. Radiother Oncol 2016;121(3):414–419. [DOI] [PubMed] [Google Scholar]
- 5.Rossi AM, Nehal KS, Lee EH. Radiation-induced breast telangiectasias treated with the pulsed dye laser. J Clin Aesthet Dermatol 2014;7(12):34–37. [PMC free article] [PubMed] [Google Scholar]
- 6.Ahmad M, Mirza S, Foo IT. Pulsed dye laser treatment of telangiectasia after radiotherapy for breast carcinoma. Br J Plast Surg 1999;52(3):236–237. [DOI] [PubMed] [Google Scholar]
- 7.Chren MM. The Skindex instruments to measure the effects of skin disease on quality of life. Dermatol Clin 2012;30(2): 231–236, xiii. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chren MM, Lasek RJ, Quinn LM, Mostow EN, Zyzanski SJ. Skindex, a quality-of-life measure for patients with skin disease: Reliability, validity, and responsiveness. J Invest Dermatol 1996;107(5):707–713. [DOI] [PubMed] [Google Scholar]
- 9.Cano SJ, Klassen AF, Scott AM, Cordeiro PG, Pusic AL. The BREAST-Q: Further validation in independent clinical samples. Plast Reconstr Surg 2012;129(2):293–302. [DOI] [PubMed] [Google Scholar]
- 10.Fuzesi S, Cano SJ, Klassen AF, Atisha D, Pusic AL. Validation of the electronic version of the BREAST-Q in the army of women study. Breast 2017;33:44–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nymann P, Hedelund L, Haedersdal M. Intense pulsed light vs. long-pulsed dye laser treatment of telangiectasia after radiotherapy for breast cancer: A randomized split-lesion trial of two different treatments. Br J Dermatol 2009;160(6):1237–1241. [DOI] [PubMed] [Google Scholar]
- 12.Whelan TJ, Pignol JP, Levine MN, et al. Long-term results of hypofractionated radiation therapy for breast cancer. N Engl J Med 2010;362(6):513–520. [DOI] [PubMed] [Google Scholar]
- 13.Rossi AM, Nehal KS, Mehrara B, Lee E. Cutaneous ulceration and breast implant compromise after pulse dye laser for radiation-induced telangiectasias. JAAD Case Rep 2017; 3(3):180–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Greveling K, Prens EP, van Doorn MB. Treatment of port wine stains using pulsed dye laser, erbium YAG laser, and topical rapamycin (sirolimus)—A randomized controlled trial. Lasers Surg Med 2017;49(1):104–109. [DOI] [PubMed] [Google Scholar]
- 15.Griffin TD Jr., Foshee JP, Finney R, Saedi N. Port wine stain treated with a combination of pulsed dye laser and topical rapamycin ointment. Lasers Surg Med 2016;48(2):193–196. [DOI] [PubMed] [Google Scholar]
- 16.Carlsen BC, Wenande E, Erlendsson AM, Faurschou A, Dierickx C, Haedersdal M. A randomized side-by-side study comparing alexandrite laser at different pulse durations for port wine stains. Lasers Surg Med 2017;49(1):97–103. [DOI] [PubMed] [Google Scholar]


