Abstract
A Best Evidence Topic in general surgery was written according to a structured protocol. The question addressed was ‘Appendiceal phlegmon in adults: Do we know how to manage it yet?‘. Altogether 217 papers were found on Ovid Embase and Medline, 334 on PubMed and 13 on the Cochrane database using the reported search. From the screened articles, 5 represented the best evidence to answer the clinical question. The authors, journal, date and country of publication, patient group studied, study type, relevant outcomes and results of these papers are tabulated. We conclude that the best management method is conservative only treatment without interval appendicectomy. These patients must be followed up, including colonoscopy and/or CT imaging as indicated, to investigate for conditions such as inflammatory bowel disease or malignancy masquerading as appendicitis.
Keywords: Appendiceal mass, Appendicular/appendix mass, Appendiceal phlegmon, Appendicular/appendix phlegmon, Early appendicectomy, Interval appendicectomy, Conservative management, Evidence-based medicine
Highlights
-
•
On-going controversy exists around the best management option for an appendiceal phlegmon.
-
•
Various articles advocate each of the following: early appendicectomy, interval appendicectomy and conservative management.
-
•
Therefore, we conducted a literature review in the format of a Best Evidence Topic to identify the best approach.
-
•
We conclude that the best management method is conservative only treatment without interval appendicectomy.
-
•
They must be followed up, including colonoscopy/imaging as indicated, to identify conditions masquerading as appendicitis.
-
•
Our suggestion is in direct contrast to the widely practiced method of interval appendicectomy.
1. Introduction
A Best Evidence Topic was constructed according to a structured protocol. This is fully described by the International Journal of Surgery [1].
2. Clinical scenario
A 29-year-old male patient presents with a 7-day history of migratory central to right lower quadrant abdominal pain. This is associated with nausea, anorexia and low-grade pyrexia. On examination, a mass like structure is palpated in the right lower quadrant. Ultrasound scanning confirms your diagnosis of an appendiceal mass. You recall the ongoing controversy around the best management options: early appendicectomy, interval appendicectomy and purely conservative management. Unsure which is in the best interest of the patient, you resolve to check the literature for evidence.
3. Three-part question
In [adult patients with an appendiceal phlegmon], what is the best management option out of [early appendicectomy, interval appendicectomy and purely conservative management] in terms of [length of admission, complications and other clinical outcomes]?
4. Search strategy
The search strategy outlined below was utilised and where possible the results were limited to English articles, human studies and adult population. In addition, the reference lists of the screened articles were reviewed.
Medline 1946 to May 2020 and Embase 1974 to May 2020 using the OVID interface:
[Appendiceal mass OR appendicular mass OR appendix mass OR Appendiceal phlegmon OR appendicular phlegmon OR appendix phlegmon] AND [appendicectomy OR appendectomy]
Medline using the PubMed interface:
[Appendiceal mass OR appendicular mass OR appendix mass OR Appendiceal phlegmon OR appendicular phlegmon OR appendix phlegmon] AND [appendicectomy OR appendectomy].
4.1. Search outcome
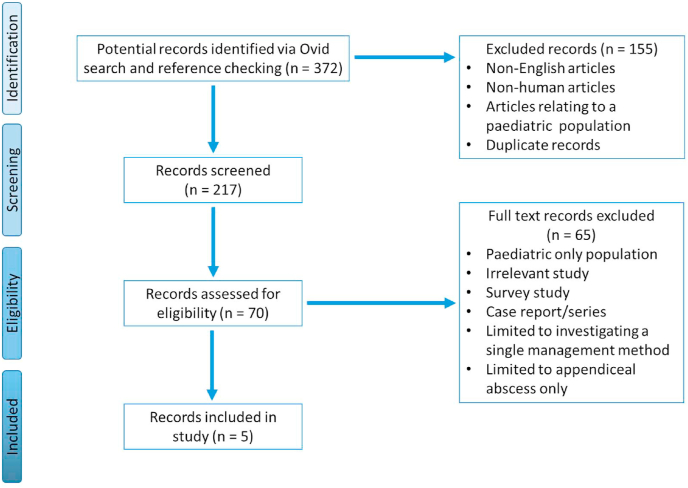
217 papers on Ovid Embase and Ovid Medline, 334 papers on PubMed and 13 papers on the Cochrane database were found using the reported search and screened. From these 5 papers were identified that provided the best evidence to answer the question of the optimal management method for an appendiceal phlegmon out of early appendicectomy (EA), interval appendicectomy (IA) and purely conservative management (CM). These are presented in Appendix 1. An example of the screening and eligibility assessment process for the search results obtained from the Ovid interface is detailed in Fig. 1.
Fig. 1.
PRISMA flow chart for Ovid search (PubMed and Cochrane flow chart not included in this figure).
5. Results
The results of this article are tabulated in Appendix 1; this contains a review of the most relevant and highest quality evidence available assessing the optimal method of appendiceal mass management. This table is structured according to the guidance by the International Journal of Surgery [1] highlighting key results, statistical analysis outcomes and study limitations.
6. Discussion
The management of an appendiceal mass is an area of ongoing debate and controversy; a recent survey study by Sajid et al. displayed the immense disparity in the perceived optimal management method amongst general surgeons [2]. Considering this, we conducted a review of the Best Evidence Topic.
Demetrashvili et al. [3] performed a prospective study comparing EA, IA and CM. Their study favoured the approach of conservative treatment with antibiotics and image-guided drainage where indicated, without the need for IA unless there was a recurrence of appendicitis. Of interest was the finding that of the 3 patients in the CM group who developed recurrence of appendicitis, all had undergone percutaneous drainage as part of their conservative management. Following completion of conservative management, Colonoscopy and CT imaging was recommended within 4–6 weeks; this approach is justified in obviating the considerable risk of missing hidden pathologies associated with CM [4].
Aranda-Narváez et al. [5] conducted a retrospective study with a control group of EA matched to a CM/IA group. An initial conservative management was successful in all cases without requirement for urgent surgical intervention. Only 13.3% of the laparoscopic approach to the EA was completed without conversion to open, though it is important to note that the data sampling was done from 1997 to 2009 whereby advances in minimally invasive surgery were ongoing [6]. This study, similarly to that of Demetrashvili et al., concluded that the best method of management is that of a purely conservative management, only with the addition of IA in cases of symptomatic recurrence. The mean percentage of recurrence across the tabulated articles of Appendix 1 was 17%; this is comparable to the figures quoted by other studies, which range from 12% to 20% [[7], [8], [9]].
Cheng at al [10] conducted a Cochrane systematic review in 2017 of randomised controlled trials (RCT) comparing EA and IA, and identified only two suitable RCTs. It is important to note that the reviewers regarded both trials as very low quality trials. Further, this Cochrane review did not have a meta-analysis due to the fact that only one trial was identified for each outcome (appendiceal phlegmon and appendiceal abscess). In our article, it was decided to include only one of the two RCTs in the results table due to the fact that the other RCT's patient population consisted of only paediatric patients with appendiceal abscesses. The included RCT is that by Kumar et al. [11] who concluded that the best management modality was again of CM without appendicectomy. Of note is the fact that this trial does not investigate quality of life.
In 2014, Olsen et al. [12] conducted a systematic review of studies investigating treatment modalities of CM and EA, but not of IA. The results included in the table are specifically that of the adult population, but not of the paediatric or mixed population studies. In adults, it was identified that the frequency of complication in EA ranged between 0 and 57%: major complications occurred in up to 19% and the risk of intestinal resection was approximately 10%. On the other hand, this systematic review mentions that all of the patients with a phlegmon responded to antibiotics. Overall, Olsen et al. concluded that CM is the safest method of appendiceal mass management, with a low risk of treatment failure and complications.
Due to the fact that the aforementioned study did not investigate IA, it was decided to include the systematic review by Darwazeh et al. [13] comparing CM and IA. It is important to note that the number of CM studies included in this review were 21 which was considerably higher compared to the IA group which comprised of 5 studies. The commonest morbidity in the CM group was unresolved sepsis requiring surgery. The commonest morbidities in the IA group were infections and bowel obstruction. A particular weakness of the study to highlight is the fact that the cumulative days of hospital admission and morbidity were calculated using a simple addition of the values from the IA group to the CM group; this may provide an inaccurate number, particularly if the IA studies themselves had already included both initial admission and re-admission. Despite this, they concluded that IA is of minimal benefit, whereby the number needed to treat to prevent one case of recurrence is 8.
Overall, it is clear from the discussed articles that conservative management with appropriate follow up is the best management method. The average of data from the tabulated studies comparing EA to IA indicated that the operative time of EA was 22.8 min longer, the admission length of EA was 4.5 days longer and the complication rate of EA was 40.9% higher. Therefore, if surgery was indicated, IA is a superior option to EA.
7. Clinical bottom line
In the management of an appendiceal phlegmon in an adult, it is evident from the discussed articles that the best management method is conservative only treatment without interval appendicectomy. These patients must be followed up, including colonoscopy and/or CT imaging as indicated, to investigate for conditions such as inflammatory bowel disease or malignancy masquerading as appendicitis.
Our suggestion is in direct contrast to the widely practiced method of interval appendicectomy [14], popularised as the Ochsner-Sherren regimen. It is important to note that to this day there are no prospective, large-scale and well-designed clinical trials with blinding of outcome assessors directly comparing CM, EA and IA; this highlights an important area for future research.
Declaration of competing interest
None to declare.
Appendix 1.
| Article | Author, date, journal, country and study type (Level of Evidence) | Patient group | Outcomes | Key results | Comments |
|---|---|---|---|---|---|
| Comparison of treatment methods of appendiceal mass and abscess: A prospective Cohort Study [3] | Demetrashvili et al. (2019), Annals of Medicine and Surgery, Georgia | N = 74 patients | Operative time | EA (117.7 min) vs IA (87.1 min) [P = 0.008] | Does not differentiate between phlegmon and abscess. Small Sample size. Not randomised. Excluded immunocompromised and ASA 4–5 patients. |
| Total length of admission | EA (10.4 days) vs IA (8.1 days) [P = 0.009] | ||||
| Prospective cohort study (Level III) | Complications | EA (22.2%) vs IA (0%) [P = 0.02] | |||
| Other | In EA group, ileocecectomy/right hemicolectomy performed in 25.9% of cases compared with 8.33% in IA group. Appendicitis recurred in 13% of the CM group who proceeded with appendicectomy with no complications post-operatively. In this group, both operative time (51.4 min) and hospital stay (4.3 days) was significantly shorter compared to IA group. 3 patients (4.05%) had hidden pathologies of malignancy and Crohn's disease. |
||||
| Conservative approach versus urgent appendectomy in surgical management of acute appendicitis with abscess or phlegmon [5] | Aranda-Narváez et al. (2010), Revista Española de Enfermedades Digestivas, Spain | N = 30 patients | Operative time | No statistically significant difference between EA and IA. | Retrospective study. Small sample size. Patients with severe sepsis excluded. |
| Total length of admission | No statistically significant difference. | ||||
| Retrospective cohort study (Level III) | Complications | Contaminated surgery: EA (100%) vs IA (28.6%) [P < 0.001]. Surgical site infection: EA (40%) vs IA (0%) [P < 0.001] |
|||
| Other | Appendicitis recurred in 33.3% of the CM group who proceeded with appendicectomy with no complications post-operatively. 1 patient (3.33%) had hidden pathology of caecal adenocarcinoma. |
||||
| Early versus delayed appendicecto-my for appendiceal phlegmon or abscess (Review) [10] | Cheng et al. (2017), Cochrane Database of Systematic Reviews, China | N = 40 patients (Only one of the two studied RCTs included here as the other RCT was purely based on appendiceal abscesses in a paediatric population) | Operative time | EA (53 min) vs IA (38 min) [Extracted from original RCT article rather than Cochrane review. P < 0.05] | No pooling of data/meta-analysis. No power calculation, small sample size and recruitment of a mixture of both paediatric and adult patients in the included RCT. Included RCT at high risk of performance and reporting bias, and unclear risk of selection bias (No blinding, unclear method of randomisation and allocation concealment). Sampling done between 1998 and 2001 consisting of only open appendicecto-my. |
| Total length of admission | EA (21.4 days) vs IA (14.7 days) [P < 0.001]. NB original article indicates 4.9 days length of admission in CM group. | ||||
| Systematic review of 2 RCTs (Level I) | Complications | Complication rate (Wound infection and faecal fistula): EA (30%) vs IA (0%) [Risk Ratio 13, P = 0.07] | |||
| Other | Time away from normal activities: EA (25 days) vs IA (20 days) [P = 0.005) No cross over from IA group to EA group. 2/20 (10%) patients in CM group had recurrent appendicitis requiring appendicectomy. |
||||
| Treatment of appendiceal mass – a qualitative systematic review [12] | Olsen et al. (2014), Danish Medical Journal, Denmark | N = 48 studies (Only data for adult population studies included here) | Total length of admission | Noted but not assessed | Does not investigate IA. Includes both phlegmon and abscess. No meta-analysis. Studies ranged from 1969 to 2013. |
| Treatment failure | CM (0–22%) | ||||
| Systematic review (Level I) | Complications | EA (Range of 0–57%) | |||
| Other | Studies on recurrent appendicitis excluded. | ||||
| A Systematic Review of Perforated Appendicitis and Phlegmon: Interval Appendectomy or Wait-and-See? [13] | Darwazeh et al. (2016), The American Surgeon, United States | N = 1943 patients (26 studies) | Operative time | Not assessed. | Does not investigate EA. Includes both phlegmon and abscess. Mixture of paediatric and adult patients. No meta-analysis. |
| Total length of admission | CM group (9.6 days) vs IA (14.6 days - Cumulative estimate including initial admission) [Significance not assessed] | ||||
| Systematic review (Level I) | Complications | CM group (13.3%) vs IA (23.7% - Cumulative estimate including initial admission) [Significance not assessed] | |||
| Other | 12.4% recurrence of appendicitis in CM group. |
Author contribution
Pedram Panahi, MBBS, MRes (Distinction): Generated research proposal, conducted literature search and wrote manuscript. Rashid Ibrahim, MD, MRCS: Reviewed literature search methodology and assisted in writing paper. Pushpa Veeralakshmanan, MBChB: Assisted in writing paper. James Ackah, MPharm, BMBS, MRCS: Assisted in writing paper. Professor Mark Coleman, MBChB, FRCS (Gen Surg), FRCPSG (Hons), MD: Supervising Consultant.
References
- 1.Khan O.A., Dunning J., Parvaiz A.C., Agha R., Rosin D., Mackway-Jones K. Towards evidence-based medicine in surgical practice: best BETs. Int. J. Surg. 2011;9:585–588. doi: 10.1016/j.ijsu.2011.08.001. [DOI] [PubMed] [Google Scholar]
- 2.Sajid M.S., Ray K., Hebbar M., Riaz W., Baig M.K., Sains P. South Coast appendicular mass management (SCAM) survey. Translational Gastroenterology and Hepatology. 2020;5 doi: 10.21037/tgh.2019.11.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Demetrashvili Z., Kenchadze G., Pipia I., Khutsishvili K., Loladze D., Ekaladze E. Comparison of treatment methods of appendiceal mass and abscess: a prospective Cohort Study. Annals of Medicine and Surgery. 2019;48:48–52. doi: 10.1016/j.amsu.2019.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tannoury J., Abboud B. Treatment options of inflammatory appendiceal masses in adults. World J. Gastroenterol.: WJG. 2013;19(25):3942. doi: 10.3748/wjg.v19.i25.3942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aranda-Narváez J.M., González-Sánchez A.J., Marín-Camero N., Montiel-Casado C., López-Ruiz P., Sánchez-Pérez B. Conservative approach versus urgent appendectomy in surgical management of acute appendicitis with abscess or phlegmon. Rev. Esp. Enferm. Dig. 2010;102(11):648. doi: 10.4321/s1130-01082010001100005. [DOI] [PubMed] [Google Scholar]
- 6.Cash C., Frazee R. Improvements in laparoscopic treatment for complicated appendicitis. J. Laparoendosc. Adv. Surg. Tech. 2012;22(6):581–583. doi: 10.1089/lap.2011.0419. [DOI] [PubMed] [Google Scholar]
- 7.Eryilmaz R., Sahin M., Savaş M.R. Is interval appendectomy necessary after conservative treatment of appendiceal masses? Ulusal travma ve acil cerrahi dergisi= Turkish journal of trauma & emergency surgery: TJTES. 2004;10(3):185–188. [PubMed] [Google Scholar]
- 8.Tekin A., Kurtoğlu H.C., Can I., Öztan S. Routine interval appendectomy is unnecessary after conservative treatment of appendiceal mass. Colorectal Dis. 2008;10(5):465–468. doi: 10.1111/j.1463-1318.2007.01377.x. [DOI] [PubMed] [Google Scholar]
- 9.Hoffmann J., Lindhard A., Jensen H.E. Appendix mass: conservative management without interval appendectomy. Am. J. Surg. 1984;148(3):379–382. doi: 10.1016/0002-9610(84)90476-8. [DOI] [PubMed] [Google Scholar]
- 10.Cheng Y., Xiong X., Lu J., Wu S., Zhou R., Cheng N. Early versus delayed appendicectomy for appendiceal phlegmon or abscess. Cochrane Database Syst. Rev. 2017;(6) doi: 10.1002/14651858.CD011670.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kumar S., Jain S. Treatment of appendiceal mass: prospective, randomized clinical trial. Indian J. Gastroenterol. 2004;23:165–167. [PubMed] [Google Scholar]
- 12.Olsen J., Skovdal J., Qvist N., Bisgaard T. Treatment of appendiceal mass–a qualitative systematic review. Danish Medical Journal. 2014;61(8):A4881. [PubMed] [Google Scholar]
- 13.Darwazeh G., Cunningham S.C., Kowdley G.C. A systematic review of perforated appendicitis and phlegmon: interval appendectomy or wait-and-see? Am. Surg. 2016;82(1):11–15. [PubMed] [Google Scholar]
- 14.Chen C., Botelho C., Cooper A., Hibberd P., Parsons S.K. Current practice patterns in the treatment of perforated appendicitis in children. J. Am. Coll. Surg. 2003;196(2):212–221. doi: 10.1016/S1072-7515(02)01666-6. [DOI] [PubMed] [Google Scholar]