Abstract
Background
Ethiopia has taken strict preventive measures against COVID-19 to control its spread, to protect citizens, and ensure their wellbeing. Employee’s adherence to preventive measures is influenced by their knowledge, perceived susceptibility, severity, benefit, barrier, cues to action, and self-efficacy. Therefore, this study investigated the predictors of COVID-19 prevention practice using the Health Belief Model among employees in Addis Ababa, Ethiopia, 2020.
Methods
Multicentre cross-sectional study design was used. A total of 628 employees selected by systematic sampling method were included in this study. Data were collected using a pretested self-administered questionnaire. Summary statistics of a given data for each variable were calculated. Logistic regression model was used to measure the association between the outcome and the predictor variable. Statistical significance was declared at p-value<0.05. Direction and strength of association were expressed using OR and 95% CI.
Results
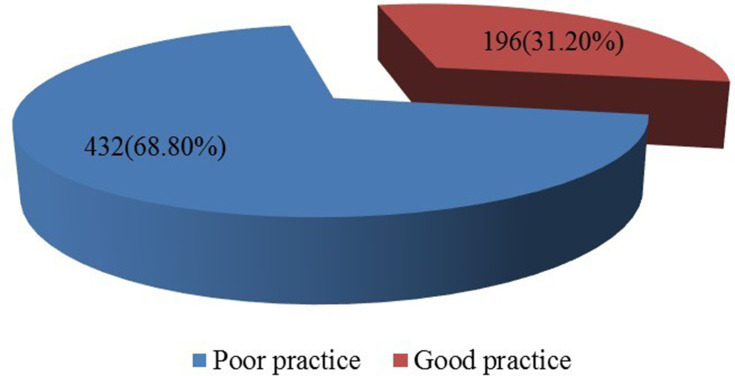
From a total of 628 respondents, 432 (68.8%) of them had poor COVID-19 prevention practice. Three hundred ninety-one (62.3%), 337 (53.7%), 312 (49.7), 497 (79.1%), 303 (48.2%) and 299 (52.4%) of the respondents had high perceived susceptibility, severity, benefit, barrier, cues to action and self-efficacy to COVID-19 prevention practice, respectively. Employees with a low level of perceived barriers were less likely to have a poor practice of COVID-19 prevention compared to employees with a high level of perceived barrier [AOR = 0.03, 95% CI (0.01,0.05)]. Similarly, employees with low cues to action and employees with a low level of self-efficacy were practiced COVID prevention measures to a lesser extent compared those with high cues to action and high level of self-efficacy [AOR = 0.05, 95% CI (0.026,0.10)] and [AOR = 0.08, 95% CI (0.04,0.14)], respectively.
Conclusion
The proportion of employees with poor COVID-19 prevention was high. Income, perceived barrier, cues to action, and self-efficacy were significantly associated with COVID-19 prevention practice.
Keywords: predictor, COVID-19, Health Belief Model, employees
Introduction
The globe is facing an extremely bizarre time struggling to fight an enemy it never saw before; the novel coronavirus disease (COVID)-19. SARS-CoV-2 or COVID-19 was first reported in December 2019, as a cluster of acute respiratory illness in Wuhan (pneumonia of unknown cause), Hubei Province, China, from where it spread rapidly around the globe involving more than 190 countries. The World Health Organization (WHO) declared the outbreak a Public Health Emergency of International Concern (PHEIC) on 30 January 2020 and a global pandemic on 11 March 2020.1,2
As of 22 April 2020, more than 2.57 million cases have been reported across 185 countries and territories, resulting in more than 178,558 deaths. About three-fourth (701,838) the people with COVID-19 have recovered while about 52, 262 of them are in a serious or critical condition.3,4
There are now more than 24,600 confirmed cases of coronavirus infection across the continent Africa, resulting in more than 1190 mortalities. Similarly, about 116 cases and 3 death of COVID-19 are reported in Ethiopia as of 22 April 2020.5
COVID-19 causes a range of respiratory symptoms including fever, fatigue, dry cough, and difficulty of breathing. It may result in serious complications like ARDS and death especially among elderly patients and patients with underlying medical conditions like heart disease, diabetes, hypertension, and asthma. A study done in China shows those patients with a severe form of COVID 9 developed ARDS and required ICU admission and oxygen therapy. At this stage of the diseases, the mortality rate is high (15%).6,7
For five decades, the Health Belief Model (HBM) has been one of the most widely used conceptual frameworks in health behavior. The HBM has been used both to explain change and maintenance of health-related behaviors and as a guiding framework for health behavior intervention.8
It is now believed that people will take action to prevent or control ill-health conditions like COVID-19 if they regard themselves as susceptible to the COVID-19; if they believe it would have potentially serious consequences; if they believe that a course of action like stay home, keep social distance, wear face mask, etc available to them would help reduce either their susceptibility to the disease or the severity of the condition; and if they think that the likely barriers (or cost) of taking the actions outweighed by its benefits.9
Given that health motivation is it’s a central focus, the Health Belief Model is an ideal option for addressing behavioral problems that evoke health concerns. The model has been tested repeatedly in western countries that it fits best for health behavior change studies as well as a planning model together with other health education and planning models, such as the PRECEDE–PROCEDE model. To date, a vaccine and effective treatment are not available for COVID-19. In a situation like this, basic hygiene principles and aggressive public health measures are virtually important for preventing the spread of the disease and hence reducing its impact in the community. Therefore, this study was aimed at assessing predictors of COVID-19 prevention practice among Higher Education employees in Addis Ababa Ethiopia using a Health Belief Model.
Methods and Materials
Study Area and Period
The study was conducted to determine the predictors of COVID-19 prevention practice among employees working in Addis, Ethiopia, May 2020. Addis Ababa is the capital city of Ethiopia with a population of around 4.7 million. Addis Ababa has 109 administrative sub-cities and a total of 99 Kebeles. The study was done among employees selected from four organizations in Addis Ababa (Ethiopian Airlines, Commercial Bank of Ethiopia, Black Lion Hospital, and Ethiopian Telecommunication Corporation). The study was done from May to June 2020.
Study Design
A multicentered cross-sectional study design was used to assess predictors of COVID-19 prevention practices using a Health Belief Model among employees in Addis Ababa, Ethiopia, 2020.
Inclusion and Exclusion Criteria
Employees from the four stated organizations and who are willing to participate were included in this study. Employees with hearing and visual impairment were excluded from this study.
Sample Size
The sample size for the study was calculated using a single proportion formula by assuming 95% CL, 4% marginal error, and 50% proportion of COVID-19 prevention practice. Therefore, by adding a 10% non-response rate, the final sample size for this study was 628.
Sampling Method
The sample size was proportionally allocated to each of the four organizations. Then, a systematic sampling method was used to select the study participants from each of the four organizations. According to the available data during the study period, a total of 4396 active workers were available in the four selected organizations in Addis Ababa. Hence, by dividing the total active employees during the study period (4396) with the total sample size (628), (N/n), the sampling interval (K) of 7 was obtained. The first employee was selected at random from each organization and consecutive participants were selected every seventh employee. Participants were approached in their working area.
Variables
COVID-19 prevention practice was the dependent variable. Demographic variables, knowledge about COVID-19, and the HBM constructs (perceived susceptibility, perceived severity, perceived benefit, perceived barrier, cues to action, and self-efficacy) were the independent variables.
Data Collection Method and Instrument
The questionnaire was developed by reviewing previous different literature conducted on prevention practice of COVID-19 and in consultation with experts from different fields to check the relevance and make necessary changes according to the study requirements. The questions were modified according to the suggestions received from the expert panel and output from the pre-test. Guidelines for layout, question design, formatting, and pretesting testing were followed.
The questionnaire was used to gather employees’ demographic data, knowledge about COVID-19 and its prevention, Health Belief Model constructs (perceived susceptibility, perceived severity, perceived benefit, perceived barrier, and cues to action self-efficacy), and practice of COVID-19 prevention.
Data Analysis
SPSS version 23 computer software package was used to analyze the data. The collected data were entered into SPSS and data cleaning was undertaken before data analysis. Summary statistics like frequency, percent, mean, and standard deviation of a given data for each variable were calculated. A logistic regression model was used to measure the association between the outcome (COVID-19 prevention practice) and the predictor variables (socio-demographic variables, knowledge, and the HBM constructs). Statistical significance was declared at p-value<0.05. Direction and strength of association was expressed using OR and 95% CI.
Data Quality Assurance
A preliminary phase was conducted to assess the validity and reliability of the questionnaire before its use. Initially, three Ethiopian experts in the field of epidemiology and research in Ethiopian universities were asked to assess the degree to which items in the questionnaires were relevant and can correctly measure predictors of COVID-19 prevention practice using the Health Belief Model, and a correction was made accordingly. Then, the questionnaire was pretested on 30 participants who were excluded later from the study sample. Data were used to assess internal consistency reliability using Cronbach’s alpha. The results showed adequate internal consistency reliability (with Cronbach’s alpha= 0.915 or perceived susceptibility, 0.773 for perceived severity, 0.954 for the perceived benefit, 0.869 for the perceived barrier, 0.806 for cues to action, and 0.986for self-efficacy questions).
Ethics Approval and Consent to Participants
Approval and ethical clearance was obtained from the Institution Review Board (IRB) of Universal Medical and Business College (UMBC) which was in accordance with the principles embodied in the Declaration of Helsinki. Official permission was also obtained from the principals of the four selected organizations before approaching the study participants. The objective and purpose of the study was clearly explained to the study subjects to obtain written informed consent before data collection. Participants were also informed that they can discontinue or decline to participate in the study at any time. Confidentiality of the information was maintained and the data were recorded anonymously throughout the study.
Operational Definition and Its Measurements
Knowledge of COVID-19: knowledge of COVID-19 was measured using 12 questions. Each correct response was scored 1, and each incorrect response was scored 0. A total score of ≥9 (≥80%) out of 12 was considered as having good knowledge whereas a score <9 (<80%) was considered as poor knowledge towards COVID-19 and its prevention.
COVID-19 prevention practices: Practice of COVID-19 prevention was measured using eleven questions. Each correct response in the practice category was scored 1, and each incorrect response was scored 0. A total score of ≥8 (≥80%) out of eleven was considered as having good practice whereas a score <8 (<80%) was considered as having a poor practice of COVID-19 prevention.10
Perceived susceptibility: one’s belief regarding the chance of getting COVID-19. Respondents will be asked eight7 questions (eg I am not afraid of getting Coronavirus infection) to describe their level of agreement in a five-scale response format from “strongly disagree” to “strongly agree”. The 5-point Likert scale response options, scored from 1 to 5, were strongly disagree, disagree, neutral, agree, and strongly agree. Subscale scores were obtained by summing item scores and dividing by the total number of items. If it is above or equal to the average score, it was indicative of high perceived susceptibility.11
Perceived severity: one’s belief of how serious COVID-19 and its squeal are. Respondents were asked six6 questions (eg Becoming Corona virus-infected is the worst thing that could happen to me) to describe their level of agreement in a five scale response format from “strongly disagree” to “strongly agree”. The 5-point Likert scale response options, scored from 1 to 5, were strongly disagree, disagree, neutral, agree, and strongly agree. Subscale scores were obtained by summing item scores and dividing by the total number of items. If it is above or equal to the average score, it was indicative of high perceived severity.12
Perceived benefit: one’s beliefs in the efficacy of COVID-19 prevention practice like hand washing, social distancing, etc. to reduce the risk of getting COVID-19. Respondents were asked 109 questions (eg Washing hands frequently with soap and water or using alcohol-based hand rub kills the virus that causes COVID-19) to describe their level of agreement in a five-scale response format from “strongly disagree” to “strongly agree”. The 5-point Likert scale response options, scored from 1 to 5, were strongly disagree, disagree, neutral, agree, and strongly agree. Subscale scores were obtained by summing item scores and dividing by the total number of items. If it is above or equal to the average score, it was indicative of a high perceived benefit.13
Perceived barrier: one’s belief about the tangible and psychological costs of practicing COVID-19 prevention mechanisms like staying at home. Respondents were asked six6 questions (eg Face mask is hard to get) to describe their level of agreement in a five-scale response format from “strongly disagree” to “strongly agree”. The 5-point Likert scale response options, scored from 1 to 5, were strongly disagree, disagree, neutral, agree, and strongly agree. Subscale scores were obtained by summing item scores and dividing it by the total number of items. If it is above or equal to the average score, it was indicative of a low level of perceived barrier.14
Cues to action: strategies to activate one’s “readiness” to use COVID-19 prevention practices. Based on prior research (Wilson et al, 1991), a 6-item yes/no scale was used to assess participant’s exposure to cues that could influence them to engage in COVID-19 practice. The scale was developed. Typical items as follows: “Do you know someone with COVID-19?” The sum of the score ranged from 6 to 12; higher scores indicated exposure to more COVID-19 information. Scale score was obtained by summing item scores and dividing by the total number of items.15
Self-efficacy: one’s confidence in one’s ability to use or apply prevention of COVID-19 practices recommended by WHO in a different situation. Respondents were asked five5 questions (eg feel confident that I could talk to any person to using a face mask) to describe their level of agreement in a five-scale response format from “strongly disagree” to “strongly agree”. The 5-point Likert scale response options, scored from 1 to 5, were strongly disagree, disagree, neutral, agree, and strongly agree. Subscale scores were obtained by summing item scores and dividing by the total number of items. If it was above or equal to the average score, it was indicative of a high level of self-efficacy.16
Result
Socio-Demographic Characteristics of the Respondents
A total of 628 employees working in four organizations in Addis Ababa were included in this study. More than half of the study subjects 414 (65.9%) were in the age category of 24–28 years with a mean ± SD of 28.76 ± 5.10 years. The majority of the respondent 434 (69.1%) were males and more than half 361 (57.5%) of them were single. The majority 376 (59.9%) and 402 (64.0%) of them were degree holders by educational level and earn a monthly income of 2500–7499 birr, respectively. Most 247 (39.3%) of them were bank workers, while 131 (20.9%) of them were health workers (Table 1).
Table 1.
Socio-Demographic Characteristics of the Respondents, Employees in Addis Ababa, Ethiopia, May 2020
| Variables | Category | Number | Percent |
|---|---|---|---|
| Age (years) | 24–28 | 414 | 65.9 |
| ≥29 | 214 | 34.1 | |
| Sex | Male | 434 | 69.1 |
| Female | 194 | 30.9 | |
| Marital status | Single | 361 | 57.5 |
| Married | 267 | 42.5 | |
| Educational level | Certificate | 90 | 14.3 |
| Degree | 376 | 59.9 | |
| Masters | 141 | 22.5 | |
| PhD | 21 | 3.3 | |
| Occupation | Health workers | 131 | 20.9 |
| Airline workers | 82 | 13.1 | |
| Bank workers | 247 | 39.3 | |
| Telecommunication workers | 168 | 26.8 | |
| Income (birr) | 2500–7499 | 402 | 64.0 |
| 7500–12,499 | 85 | 13.5 | |
| ≥12,500 | 141 | 22.5 |
Knowledge of the Respondents About COVID-19
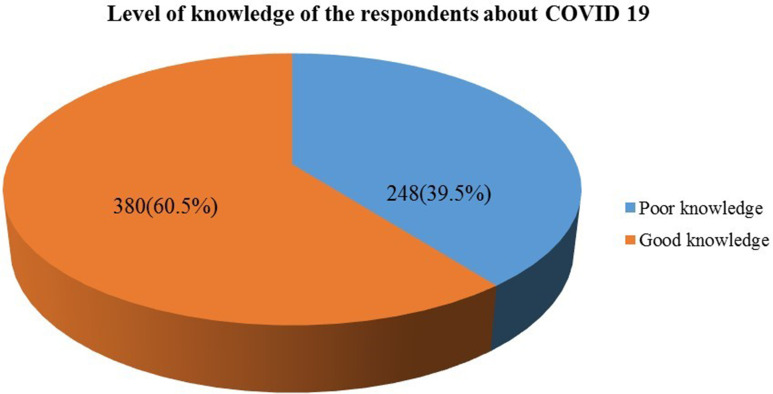
Of the total of 628 respondents, 248 (39.5%) of them had poor knowledge about COVID-19 (Figure 1). All of the respondents heard about the disease. More than half 337 (53.7%) of them were not aware of the call center service number to seek information about COVID-19 and half 309 (49.2%) of the employees were aware of the main symptoms of COVID-19 like fever, dry cough, and difficulty of breathing. Two hundred ninety-seven (47.3%) of them believed that persons infected with COVID-19, but has no symptoms cannot transmit the virus to others. Close to half 297 (47.3%) of them said children and young adults do not need to take measures to prevent COVID-19, and people who have contact with someone infected with the COVID-19 should be immediately quarantined. Only 261 (41.6%) of them said the length of quarantine of people who have contact with COVID-19 cases is 14 days (Table 2).
Figure 1.
Level of knowledge of the respondents about COVID-19, employees in Addis Ababa, Ethiopia, May 2020.
Table 2.
Knowledge of the Respondents About COVID-19, Employees in Addis Ababa, Ethiopia, May 2020
| Variables | Category | Number | Percent |
|---|---|---|---|
| Know the call center service number to seek information about COVID-19 | Yes | 291 | 46.3 |
| No | 337 | 53.7 | |
| Know the main symptoms of COVID-19 (fever, dry cough, difficulty of breathing) | Yes | 309 | 49.2 |
| No | 319 | 50.8 | |
| Supportive treatment can help most patients recover from the COVID-19 infection | Yes | 132 | 21.0 |
| No | 496 | 79.0 | |
| Patients who have chronic illnesses, elderly and obese are more likely to develop a severe form of COVID-19 | Yes | 297 | 47.3 |
| No | 331 | 52.7 | |
| Persons infected with COVID-19, but has no symptoms cannot transmit the virus to others | Yes | 297 | 47.3 |
| No | 331 | 52.7 | |
| It is not necessary for children and young adults to take measures to prevent COVID-19 | Yes | 297 | 47.3 |
| No | 331 | 52.7 | |
| People who have contact with someone infected with the COVID-19 virus should be immediately quarantined | Yes | 297 | 47.3 |
| No | 331 | 52.7 | |
| Length (in days) of quarantine of people who have contact with COVID-19 cases | 5 | 171 | 27.2 |
| 10 | 112 | 17.8 | |
| 14 | 261 | 41.6 | |
| 21 | 84 | 13.4 |
Sources Information About COVID-19
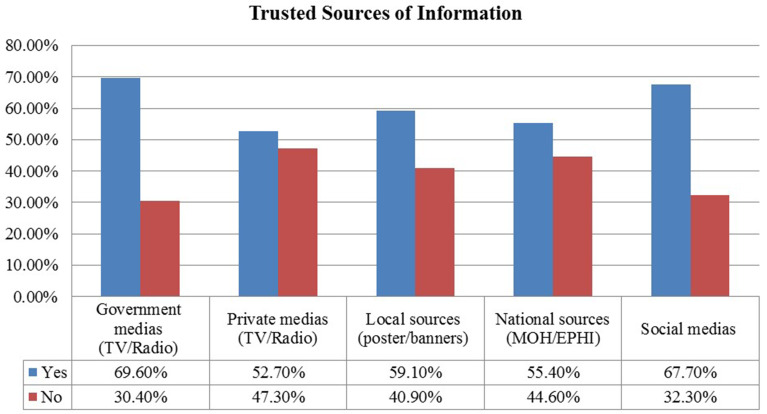
The major sources of information about COVID-19 for the study subjects were government media (TV/Radio) (69.6%), social media (67.7%), local sources like posters, banners (59.1%), national sources (MOH/EPHI) (55.4%) and private medias TV/Radio (52.7%) (Figure 2).
Figure 2.
Trusted sources information about COVID-19, employees in Addis Ababa, Ethiopia, May 2020.
Factors Affecting Knowledge of the Respondents About COVID-19
Bivariate and multivariate logistic regression models were carried out to determine the factors affecting the employees’ knowledge of COVID-19. Only variables with a p-value ≤0.2 (age, level of education, occupation, income) were included in the multivariate regression.
After adjusting for possible confounding factors with multivariate regression; age, level of education, and income were significantly associated with knowledge about COVID-19 with a p-value <0.05.
Employees in the age category of 24–28 years were 2.75 times [AOR = 2.75, 95% CI (1.72, 4.41)] more likely to have a poor level of knowledge about COVID-19 compared to employees whose age was greater than 28 years. Similarly, employees with an educational level of the certificate were 10.02 times [AOR = 10.02, 95% CI (5.02, 19.99)] more likely to have a poor level of knowledge about COVID-19 than employees with an educational level of degree an above. Employees with a monthly income of 7500–12,499 birr were less likely to have a poor level of knowledge about COVID-19 (Table 3).
Table 3.
Factors Affecting Knowledge of the Respondents About COVID-19, Employees in Addis Ababa, Ethiopia, May 2020
| Variables | Category | Knowledge of COVID-19 | COR (95% CI) | AOR (95% CI) | P-value | |
|---|---|---|---|---|---|---|
| Poor, N%) | Good, N(%) | |||||
| Age (years) | 24–28 | 150(60.5) | 264(69.5) | 1.49(1.06, 2.08)* | 2.75(1.72, 4.41) | 0.000 |
| ≥28 | 98(39.5) | 116(30.5) | 1 | 1 | ||
| Level of education | Certificate | 21(8.5) | 110(28.9) | 4.09(2.47, 6.78)* | 10.02(5.02, 19.99) | 0.000 |
| Degree | 45(18.1) | 37(9.7) | 0.64(0.40,1.03) | 1.41(0.78, 2.53) | 0.255 | |
| Master and above | 182(73.4) | 233(61.3) | 1 | 1 | ||
| Occupation | Non-health workers | 227(91.5%) | 270(71.1) | 0.23(0.14, 0.37)* | 0.85(0.48, 1.51) | 0.581 |
| Health workers | 21(8.5%) | 110(28.9) | 1 | 1 | ||
| Income (birr) | 2500–7499 | 139(56.0) | 263(69.2) | 0.89(0.59, 1.34) | 0.70(0.46, 1.08) | 0.106 |
| 7500–12,499 | 64(25.8) | 21(5.5) | 0.15(0.08, 028)* | 0.10(0.05, 0.20) | 0.000 | |
| ≥12,500 | 45(18.1) | 96(25.3) | 1 | 1 | ||
Note: *p-value < 0.05.
Constructs of the HBM About COVID-19 Prevention Practice
Three hundred ninety-one (62.3%) of the respondents had high perceived susceptibility to COVID-19 while the rest 237 (37.7%) had low perceived susceptibility to Coronavirus infection with a mean score ± SD of 14.65±8.5 and a median value of 11. Concerning the perceived severity of the disease, 337 (53.7%) of the respondents had high perceived severity to coronavirus infection while the rest 291 (46.3%) had low perceived severity and the mean score for perceived severity was 22.34 with a standard deviation ±7.8 and median value 24. Concerning the third component of the Health Belief Model, half 316 (50.3%) of the respondents had low perceptions about the benefit of coronavirus infection prevention practice. But 312 (49.7%) of the participants had high perceived benefit with a mean ± SD score of 34.0± 12.7 with a median value of 39. Three hundred twenty-five (51.8%) of the respondents were exposed to low triggering factors for coronavirus infection prevention with a mean ± SD score of 8.9±2.3 and median value 8. Four hundred ninety-seven (79.1%) of the respondents had a high perceived barrier and the rest 131 (20.9%) of the participants had low perceived barrier with a mean ± SD score of 18.02 ± 7.3 with a median value of 21. About 329 (52.4%) had low self-efficacy towards coronavirus infection prevention with a mean ± SD score of 15.6 ± 7.5 with and a median value of 15 (Table 4).
Table 4.
Opinions of the Constructs of Health Belief Model About COVID-19 Prevention Practice, Employees in Addis Ababa, Ethiopia, May 2020 (N=628)
| Items | Frequency | Percent |
|---|---|---|
| Perceived susceptibility | ||
| High | 391 | 62.3 |
| Low | 237 | 37.7 |
| Perceived severity | ||
| High | 291 | 46.3 |
| Low | 337 | 53.7 |
| Perceived benefit | ||
| High | 312 | 49.7 |
| Low | 316 | 50.3 |
| Perceived barrier | ||
| High | 497 | 79.1 |
| Low | 131 | 20.9 |
| Cues to action | ||
| High | 303 | 48.2 |
| Low | 325 | 51.8 |
| Self-efficacy | ||
| High | 299 | 52.4 |
| Low | 329 | 47.6 |
Practice of COVID-19 Prevention
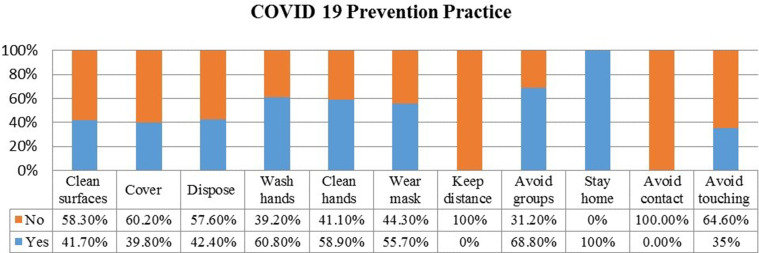
Of the total of 628 respondents, 432 (68.8%) of them had a poor practice of COVID-19 prevention. More than half 58.3% of them did not clean surfaces. Only 39.8% of them cover their mouth and nose while sneezing and coughing while 42.4% of them disposed used tissues properly after coughing and sneezing. The majority of 60.8% of them washed their hands frequently with soap and water for 20 seconds and 58.9% of them cleaned their hands with alcohol-based sanitizer if water is not available. More than half 55.7% of them wear masks in public areas and none of them kept their distance. More than two-thirds of 68.85% of them avoided groups and all of them stayed at home if they feel sick (Figures 3 and 4).
Figure 3.
Overall practice of COVID-19 prevention, employees in Addis Ababa, Ethiopia, May 2020.
Figure 4.
Practice of COVID-19 prevention, employees in Addis Ababa, Ethiopia, May 2020.
Factors Associated with COVID-19 Prevention Practice
A bivariate and a multivariate logistic regression model was carried out to determine the factors affecting the employees’ knowledge of COVID-19. Only variables with a p-value ≤0.2 (sex, knowledge, perceived severity) were included in the multivariate regression.
After adjusting for possible confounding factors with multivariate regression; income, perceived barrier, cues to action, and self-efficacy were significantly associated with prevention practice of COVID-19 with a p-value <0.05.
Employees with a monthly income of 7500–12,499 birr and 7500–12,499 birr were more likely to practice the prevention of COVID-19 compared to employees with a monthly income of ≥12,500 birr [AOR = 3.67, 95% CI (1.09,12.42)] and [AOR = 4.25, 955CI (1.23,14.65)], respectively. Employees with low level of perceived barriers were less likely to have a poor practice of COVID-19 prevention compared to employees with a high level of perceived barrier [AOR = 0.03, 95% CI (0.01,0.05)]. Similarly, employees with low cues to action and employees with a low level of self-efficacy were practiced COVID prevention measures to a lesser extent compared those with high cues to action and high level of self-efficacy [AOR = 0.05, 95% CI (0.026, 0.10)] and [AOR = 0.08, 95% CI (0.04, 0.14)], respectively (Table 5).
Table 5.
Factors Associated with COVID-19 Prevention Practice, Employees in Addis Ababa, Ethiopia, May 2020 (N=628)
| Variables | Category | Practice | COR, 95% CI | AOR, 95% CI | P-value | |
|---|---|---|---|---|---|---|
| Poor | Good | |||||
| Sex | Male | 308 | 126 | 0.73(0.51,1.04) | ||
| Female | 124 | 70 | 1 | |||
| Age (years) | 24–28 | 298 | 116 | 0.65(0.46,0.93)* | 1.53(0.79,0.299) | 0.210 |
| >28 | 134 | 80 | 1 | 1 | ||
| Marital status | Single | 219 | 142 | 2.56(1.77,3.69)* | 1.96(0.93,4.13) | 0.770 |
| Married | 213 | 54 | 1 | 1 | ||
| Educational status | Certificate | 46 | 142 | 5.50(3.02,10.01)* | 2.91(0.86,9.79) | 0.085 |
| Degree | 248 | 54 | 2.97(1.83,4.81)* | 1.43(0.55,3.69) | 0.463 | |
| Masters and above | 138 | 196 | 1 | 1 | ||
| Occupational status | Non-health workers | 363 | 134 | 0.41(0.28,0.61)* | 0.56(0.267,1.19) | 0.563 |
| Health workers | 69 | 62 | 1 | 1 | ||
| Income (birr) | 2500–7499 | 248 | 154 | 4.85(2.78,8.48)* | 3.67(1.09,12.42) | 0.036 |
| 7500–12,499 | 59 | 26 | 3.44(1.72,6.90)* | 4.25(1.23,14.65) | 0.022 | |
| ≥12,500 | 125 | 16 | 1 | 1 | ||
| Knowledge | Poor knowledge | 180 | 68 | 0.74(0.52,1.06) | ||
| Good knowledge | 252 | 128 | 1 | |||
| Perceived susceptibility | Low | 281 | 110 | 0.69(0.49,0.97)* | 1.24(0.68,2.24) | 0.482 |
| High | 151 | 86 | 1 | 1 | ||
| Perceived severity | Low | 236 | 101 | 0.88(0.63,1.24) | ||
| High | 196 | 95 | 1 | |||
| Perceived benefit | Low | 231 | 85 | 0.67(0.47,0.94)* | 1.34(0.75,2.39) | 0.324 |
| High | 201 | 111 | 1 | 1 | ||
| Perceived barrier | Low | 406 | 91 | 0.06(0.03,0.09)* | 0.03(0.01,0.05) | 0.000 |
| High | 26 | 105 | 1 | |||
| Cues to action | Low | 280 | 45 | 0.16(0.11,0.24)* | 0.05(0.026,0.10) | 0.000 |
| High | 152 | 151 | 1 | 1 | ||
| Self-efficacy | Low | 280 | 49 | 0.18(0.12,0.26)* | 0.08(0.04,0.14) | 0.000 |
| High | 152 | 147 | 1 | 1 | ||
Note: *P-value < 0.05.
Discussion
COVID-19 is an emerging infectious disease that poses a significant threat to public health.17 Given the severe threats imposed by COVID-19 and the lack of a COVID-19 vaccine, preventive measures play a vital role in decreasing infection rates and halting the spread of the disease.18 This indicates the necessity of employees to practice the preventive and control measures, which is affected by socio-demographic characteristics, level of knowledge, perceived susceptibility, severity, benefit, barrier, cues to action, and self-efficacy. Therefore, this study was the first study to assess the predictors of coronavirus infection prevention practice among employees of Addis Ababa, Ethiopia using the Health Belief Model.
In this study, the level of COVID-19 prevention practice was 196 (31.2%). This was similar to a study conducted in residents of Ethiopia.19 However, this was lower when compared to the previous study done among health professionals in Ethiopia which were 63%,20,21 and with the study conducted among the high-risk group of Addis Ababa Ethiopia which was 49%22 with the study conducted in the Kingdom of Saudi Arabia.23 And with the study conducted in Hong Kong which was 77% of the participants reported good health performance for COVID–19.24 This discrepancy might be due to the difference in the study population.
A perceived barrier is one of the components of HBM that deals with the perception of barriers that do not allow the performance of coronavirus infection prevention (ie availability and accessibility of water, home environment, and the availability of electricity and internet connection).25 The present study finds out that employees with low level of perceived barriers were less likely to have a poor practice of COVID-19 prevention compared to employees with a high level of perceived barrier [AOR = 0.03, 95% CI (0.01,0.05)]. This might be due to the finding proportion of households with soap and water for hand-washing was 13% and current levels of access to water and hand-washing facilities, and characteristics of the home environment are not conducive for effective implementation of basic prevention measures, including social distancing26 and limited access to electricity and internet connection discourages work from home.27
Self-efficacy is one of the components of HBM that refers to the level of a person’s confidence in his or her ability to successfully perform the prevention mechanism of COVID-19.8 The current study identified that employees with low cues to action and employees with a low level of self-efficacy were practice COVID prevention measures to a lesser extent compared with those with high cues to action and high level of cues to action [AOR = 0.05, 95% CI (0.026,0.10)] and [AOR = 0.08, 95% CI (0.04,0.14)], respectively. This was in line with the study conducted in Turkish adults28 and with the study conducted in Iran among hospital staff.29 Individuals who believe they are at low risk of developing a COVID-19 are more likely to engage in unhealthy, or risky, behaviors like not wearing a face mask, unable to keep social distancing, etc.,30 and the combination of Perceived severity and Perceived susceptibility is referred to as perceived threat31 which depend on knowledge about the COVID-19 situation.32
The HBM predicts that higher perceived threat leads to a higher likelihood of engagement in health-promoting behaviors like keeping social distancing, properly wearing a face mask, hand hygiene, etc. But the current study failed to show the significant association between COVID-19 prevention practice and perceived severity and perceived susceptibility. This might be due to the knowledge gap that was found among the employees towards the COVID-19 situation was 40%. A study conducted in Sudan to determine the Sudanese perceptions of COVID-19 using the Health Belief Model showed that low perceived susceptibility (beliefs about the likelihood of getting COVID-19) and severity (beliefs about the seriousness of contracting COVID-19, including consequences) was 45% and 40%, respectively.33 This is slightly higher compared to the current study, which was 37.7% of the employee had low perceived susceptibility. But the perceived severity was slightly lower which 53.7% of the employees had low perceived severity. This difference might be due to the difference in the study area.and the source of the population.
In the current study of a total of 628 respondents, 380 (60.5%) of them had good knowledge about COVID-19. This was higher when it compared with the study that was done in Ethiopia which was 52% of the participants had good knowledge on transmission of COVID-1922 and with the study conducted in India which was 39% of the participants have good perceived knowledge for preventive measures.34
Limitation
This study has some limitations. One of the limitations is bias occurred as a result of the study design (cross-sectional) since the study took the information at specified time-points and cause and effect association cannot be studied. Different mechanisms were used to reduce potential bias in the study. In addition to this, a lack of sufficient similar study limited comparison to this study finding with other studies. However, identifying knowledge gaps, perceived susceptibility, severity, benefit, barrier, cues to action, self-efficacy, and practice can be used to develop effective interventions and establish baseline levels to set priorities for program managers.
Conclusions
This study examined the predictors of COVID-19 prevention practice using the Health Belief Model among employees of Addis Ababa, Ethiopia. A significant number of employees had poor knowledge about COVID-19 and its prevention. The proportion of poor prevention practice of COVID-19 was also high. Income, perceived barrier, cues to action, and self-efficacy were significantly associated with the prevention practice of COVID-19 with a p-value<0.05. Hence, policymakers and other concerned bodies should focus on those areas to improve the prevention practice of COVID-19.
Acknowledgments
Our heartfelt thanks go to Universal Medical and Business College for funding the study. The researchers also wish to express their gratitude to the study subjects and to all those who lent their hands for the successful completion of this research.
Funding Statement
This research was funded by Universal Medical College but has no other role in the manuscript.
Permission for Publication
Consent to publish is not applicable for this manuscript because there are no individual data details like images or videos.
Accessibility of Data and Materials
The result of this research was extracted from the data gathered and analyzed based on the stated methods and materials. There are no supplementary files. The original data supporting this finding will be available at any time upon request.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors affirm that there is no conflict of interest concerning the publication of this manuscript.
References
- 1.Wuhan City Health Committee (WCHC). Wuhan Municipal Health and Health Commission’s briefing on the current pneumonia epidemic situation in our city 2019 [updated 31 December 2019, 14 January 2020]. Med Virol. 2020;92(4):441–447. doi: 10.1002/jmv.25689 [DOI]
- 2.European Centre for Disease Prevention and Control (ECDC). Risk Assessment: Outbreak of Acute Respiratory Syndrome Associated with a Novel Coronavirus, Wuhan, China; First Update 2020 [Updated 22 January 2020]. Stockholm: ECDC; 2020. [Google Scholar]
- 3.World Health Organization (WHO). Coronavirus disease 2019 (COVID-19) Situation Report – 93. Data as received by WHO from national authorities by 10:00 CEST, 22 April 2020. Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200422-sitrep-93-covid-19.pdf?sfvrsn=35cf80d7_4.
- 4.Center for Disease Control and Prevention (CDC). COVID View Summary ending on April 18, 2020. CDC 24/7: Saving Lives, Protecting People. Available From: https://www.cdc.gov/coronavirus/2019-ncov/covid-data/covidview/past-reports/04242020.html.
- 5.WHO. COVID-19 Situation update for the WHO African Region, External Situation Report. World Health Organization (WHO) 2020 [Google Scholar]
- 6.She J, Jiang J, Ye L, Hu L, Bai C, Song Y. 2019 novel coronavirus of pneumonia in Wuhan, China: emerging attack and management strategies. Clin Transl Med. 2020;9(1):19. doi: 10.1186/s40169-020-00271-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China [published correction appears in Lancet]. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jones CL, Jensen JD, Scherr CL, Brown NR, Christy K, Weaver J. The Health Belief Model as an explanatory framework in communication research: exploring parallel, serial, and moderated mediation. Health Commun. 2015;30(6):566–576. doi: 10.1080/10410236.2013.873363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Raffy L, Weston K. Applying the Health Belief Model to assess prevention services among young adults. Int J Health Prom Educ. 2018;1–11. doi: 10.1080/14635240.2018.1549958. [DOI] [Google Scholar]
- 10.UNICEF, WHO & CIFRC. Key messages and actions for COVID-19 prevention and control in schools. 2020.
- 11.Bavel JJV, Baicker K, Boggio PS, et al. Using social and behavioural science to support COVID-19 pandemic response. Nat Hum Behav. 2020;4:460–471. doi: 10.1038/s41562-020-0884-z [DOI] [PubMed] [Google Scholar]
- 12.Burro R, Savardi U, Annunziata MA, De Paoli P, Bianchi I. The perceived severity of a disease and the impact of the vocabulary used to convey information: using Rasch scaling in a simulated oncological scenario. Patient Prefer Adherence. 2018;12:2553–2573. doi: 10.2147/PPA.S175957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tingchi Liu M, Brock JL, Cheng Shi G, Chu R, Tseng T. Perceived benefits, perceived risk, and trust: influences on consumers’ group buying behavior. Asia Pacific J Market Logist. 2013;25(2):225–248. doi: 10.1108/13555851311314031 [DOI] [Google Scholar]
- 14.Mukhtar S. Mental health and emotional impact of COVID-19: applying Health Belief Model for medical staff to general public of Pakistan. Brain Behav Immun. 2020;87:28–29. doi: 10.1016/j.bbi.2020.04.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Halligan P, Cockburn J, Wilson BA. The behavioral assessment of visual neglect. Neuropsychol Rehabil Int J. 1991;1:1. [Google Scholar]
- 16.Joseph G, Burke NJ, Tuason N, Barker JC, Pasick RJ. Perceived susceptibility to illness and perceived benefits of preventive care: an exploration of behavioral theory constructs in a transcultural context. Health Educ Behav. 2009;36(5 Suppl):71S–90S. doi: 10.1177/1090198109338915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Egeru A, Dejene SW, Siya A. Short report on implications of Covid-19 and emerging zoonotic infectious diseases for pastoralists and Africa. Res Policy Pract. 2020;10:12. doi: 10.1186/s13570-020-00173-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Prem K, Liu Y, Russell TW, et al. The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: a modelling study. Lancet Public Health. 2020;5:e261–70. doi: 10.1016/S2468-2667(20)30073-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bekele D, Tolossa T, Tsegaye R, Teshome W. The knowledge and practice towards COVID-19 pandemic prevention among residents of Ethiopia: an online cross-sectional study. bioRxiv. 2020. doi: 10.1101/2020.06.01.127381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bedru J, Zemedu A, Simeneh M, et al. Knowledge, attitude and practice of healthcare workers towards COVID-19 and its prevention in Ethiopia: a multicentre study. Int J Risk Safe Med. 2020. doi: 10.21203/rs.3.rs-29437/v1 [DOI] [Google Scholar]
- 21.Kebede Y, Yitayih Y, Birhanu Z, Mekonen S, Ambelu A, Tu W-J. Knowledge, perceptions and preventive practices towards COVID-19 early in the outbreak among Jimma university medical center visitors, Southwest Ethiopia. PLoS One. 2020;15(5):e0233744. doi: 10.1371/journal.pone.0233744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Defar A, Molla G, Abdella S, et al. Knowledge, practice and associated factors towards the prevention of COVID-19 among high-risk groups: a cross-sectional study in Addis Ababa, Ethiopia. medRxiv. 2020. doi: 10.1101/2020.08.14.20172429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Al-Hanawi Mohammed K, Angawi K, Alshareef Noor QAM, et al. Knowledge, attitude and practice toward COVID-19 among the public in the Kingdom of Saudi Arabia: a cross-sectional study. Front Public Health. 2020;(8). doi: 10.3389/fpubh.2020.00217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kwok KO, Li KK, Chan HH, et al. Community responses during the early phase of the COVID-19 epidemic in Hong Kong: risk perception, information exposure and preventive measures. medRxiv. 2020. [Google Scholar]
- 25.Yoon HJ, Kim Y. Understanding green advertising attitude and behavioral intention: an application of the health belief model. J Promo Manage. 2016;22:49–70. doi: 10.1080/10496491.2015.1107006. [DOI] [Google Scholar]
- 26.Kaleab B. COVID-19 prevention measures in Ethiopia Current realities and prospects. STRATEGY SUPPORT PROGRAM | WORKING PAPER 142.IFPRI Ethiopia 2020.
- 27.Masters GN, Taylor-Guy P, Fraillon J, Chase A-M. Ministerial briefing paper on evidence of the likely impact on educational outcomes of vulnerable children learning at home during COVID-19. Canberra: Australian government, department of education, skills and employment; 2020. Available from: https://research.acer.edu.au/learning_processes/24/.
- 28.Murat Y, Abdurrahim G. COVID-19 severity, self-efficacy, knowledge, preventive behaviors, and mental health in Turkey. Death Stud. 2020. doi: 10.1080/07481187.2020.1793434 [DOI] [PubMed] [Google Scholar]
- 29.Barati M, Bashirian S, Jenabi E, et al. Factors associated with preventive behaviours of COVID-19 among hospital staff in Iran in 2020: an application of the protection motivation theory [published online ahead of print, 2020 Apr 28]. J Hosp Infect. 2020;105(3):430–433. doi: 10.1016/j.jhin.2020.04.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Teh CH, Teh MW, Lim KH, et al. Clustering of lifestyle risk behaviours and its determinants among school-going adolescents in a middle-income country: a cross-sectional study. BMC Public Health. 2019;19(1). doi: 10.1186/s12889-019-7516-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sukeri S, Zahiruddin WM, Shafei MN, et al. Perceived severity and susceptibility towards leptospirosis infection in Malaysia. Int J Environ Res Public Health. 2020;17:6362. doi: 10.3390/ijerph17176362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Orji R, Julita Vassileva J, Mandryk R. Towards an effective health interventions design: an extension of the Health Belief Model. Online J Public Health Inform. 2012;4(3):e9. doi: 10.5210/ojphi.v4i3.4321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nasir EF, Yagoub HMA, Alhag AK. Study of the Sudanese perceptions of COVID-19: 2020. Applying the Health Belief Model. BMJ. 2020. doi: 10.1101/2020.05.28.20115477 [DOI] [Google Scholar]
- 34.Jose R, Narendran M, Bindu A, Beevi N, Manju L, Benny PV. Public perception and preparedness for the pandemic COVID 19: a Health Belief Model approach clinical. Epidemiol Glob Health. 2020. doi: 10.1016/j.cegh.2020.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]