Abstract
Objective
This study evaluated the effect of smoking on patient-reported postoperative complications after minor oral surgical procedures by comparing the post-extraction symptoms between smokers and nonsmokers.
Materials and methods
Patients undergoing minor oral surgical procedures were recruited and followed up prospectively on the first, second, seventh, and twenty-first days after simple dental extractions.
Results
A total of 85 patients completed the study. Postoperative pain, measured with a visual analog scale, was consistently higher among smokers than nonsmokers (P < 0.0001). Patient-reported experience of bleeding events was significantly less among nonsmokers (P = 0.009) only on the first postoperative day. Facial swelling was more common in smokers than in nonsmokers (P = 0.04) on the second postoperative day. Postoperative infection was reported more by smokers than nonsmokers (P > 0.05). Trismus did not vary with time according to smoking status. On the 21st postoperative day, there were no statistically significant differences in postoperative complications between the groups.
Conclusions
The patient-reported pain score was consistently higher among smokers. The study’s findings suggested that initial differences in patient-reported complications between smokers and nonsmokers undergoing minor oral surgical procedures diminished after a week.
Keywords: Smoking, Tooth extraction, Complications, Postoperative, Patient-reported, Pain
1. Introduction
According to the World Health Organization (WHO), smoking is a leading cause of early death worldwide (Jha et al., 2013). Around 6 million deaths are attributed to tobacco consumption annually. Moreover, it has been estimated that more than 600,000 people die as a result of second-hand smoking each year (U.S. National Cancer Institute and the World Health Organization, 2016). Like other undesirable behaviors, smoking is an issue that affects countries worldwide (Kasat and Ladda, 2012). The Kingdom of Saudi Arabia, with a population of approximately 20 million, was found to be fourth in terms of the highest tobacco sales globally (Salama, 2012). The 2015 Saudi Health Interview Survey estimated the prevalence of smoking at 12.2%. Smoking was more common among males than females by 21.5% (Moradi-Lakeh et al., 2015). A recent study claimed that male school-age students in the eastern region of the Kingdom with an increased awareness of the negative effects of smoking on oral health were less likely to report being smokers (Nazir and Almas, 2017).
Smoking is a well-known risk factor for morbidities, including heart attacks, strokes, and cancer (Nazir and Almas, 2017, Warnakulasuriya et al., 2010). In addition to the deleterious effects on systemic health, smoking negatively impacts the oral health of an individual (Sheiham, 2005). Studies have shown that smoking delays wound healing, affects bone remodeling and impairs healing response (Giorgetti et al., 2012, Singh Soodan et al., 2015). Moreover, it has harmful effects on periodontal health, tooth loss, and salivary flow rate (Albandar et al., 2000, Joshi et al., 2010, Rad et al., 2011, Yanagisawa et al., 2010).
Immediately after tooth extraction, the body responds by forming a blood clot in the alveolar socket. Patients should be advised to discontinue smoking as it can disrupt clot formation and interfere with the healing process. Tobacco adversely affects oral health outcomes of almost all routine dental procedures. After dental extractions, the fibrinolytic activity induced by smoking decreases the alveolar blood supply and leads to a painful condition called dry socket, commonly seen in smokers (Kasat and Ladda, 2012). However, patient-reported outcomes that capture the patient’s perspective are as important as understanding the biological effects of smoking on wound-healing outcomes. The focus of our clinical practice should be on patient-centered care, which is “to improve the health outcomes for individual patients, within the context of everyday clinical practice, taking into account the objectives, preferences, and values of each patient, as well as the available economic resources.” (Sacristán, 2013) Several studies have assessed patient-reported complications following third molar surgical extractions (Al-Delayme, 2013, Larrazábal et al., 2010, Malkawi et al., 2011), dental implants (Nagahisa et al., 2018), periapical surgery (Garcia et al., 2007), and restorative procedures in pediatric dentistry (Ladewig and Tedesco, 2018). Larrazábal et al. analyzed the effect of oral hygiene and smoking on postoperative complications following surgical extraction of impacted third molars. However, their follow-up was limited to one week only (Larrazábal et al., 2010). The present study evaluated the effect of smoking on patient-reported complications following minor oral surgical procedures. Post-extraction symptoms including pain, bleeding, swelling, trismus, and infection were assessed on the first, second, seventh, and twenty-first day after dental extractions and compared between smokers and nonsmokers. We tested the hypothesis that there will be an increased incidence of postoperative complications among smokers than in non-smokers.
2. Materials and methods
Ethical approval for this study was obtained from the Research Ethics Committee, King Abdulaziz University, Faculty of Dentistry. This prospective study recruited patients from the dental school oral surgery clinics. Patients scheduled for simple dental extraction under local anesthesia were enrolled in the study. Inclusion criteria were patients with permanent dentition, aged over 15 years, and undergoing minor oral surgical procedures. Exclusion criteria were pregnancy, alcohol/drug abuse, deciduous teeth extraction, surgical extractions, and any systemic disease with known drug therapy that could jeopardize healing. Patients who met the eligibility criteria were invited to participate in the study and informed about all its aspects, and if the patient agreed, written informed consent was obtained. No form of compensation was provided to the patients who agreed to participate. There were two cohorts: smokers (the exposed group) and nonsmokers (the unexposed group). Smokers were asked to identify the type of tobacco consumption they engaged in, including cigarette smoking, hookah/waterpipe (known as “shisha”) smoking, and cigar smoking.
On the day of the minor oral surgical procedures, patients’ data, including demographics, medical history, type of tobacco used, and frequency of smoking, were collected. A follow-up protocol was explained to each patient. A self-reported evaluation of postoperative symptoms was obtained on the first and second postoperative days by a follow-up phone call. Patients were recalled on the 7th and 21st postoperative days for a clinical examination. Complications such as pain, bleeding, swelling, trismus, and infection were recorded. Patients with persistent symptoms for more than 48 h were advised to come to the clinic for further assessment.
The patient’s level of pain intensity was assessed using the visual analog scale (VAS); a scale of 0 to 10 was used, where 0 indicated the absence of pain and 10 denoted the worst pain possible (McCormack et al., 1988). The pain VAS scale was explained to the patients at the initial visit. Post-extraction bleeding was categorized as no bleeding, bleeding persists for up to half an hour, 1–2 h, 2–3 h, or more than 3 h following an extraction. The method to assess postoperative edema was explained to the patient, and the perceived severity of the swelling was classified as mild, moderate, and severe, compared with no swelling. Trismus was determined by recording the maximum interincisal distance on the day of surgery (baseline value) and comparing the difference between the baseline value and each postoperative measurement. The readings were recorded in the clinic on day 7 and day 21. For postoperative days 1 and 2, the patients were trained to assess trismus using the three-finger test (Zawawi et al., 2003). The patients were instructed to insert three fingers between the maxillary and mandibular central incisors and report to the clinic if trismus was present.
Statistical analysis was conducted with the Statistical Package for Social Sciences (IBM® SPSS® version 24.0). Statistical analysis was performed using Chi-square test or, if appropriate, Fisher Exact test, Mann-Whitney test, and generalized model for repeated measures at alpha of 0.05.
3. Results
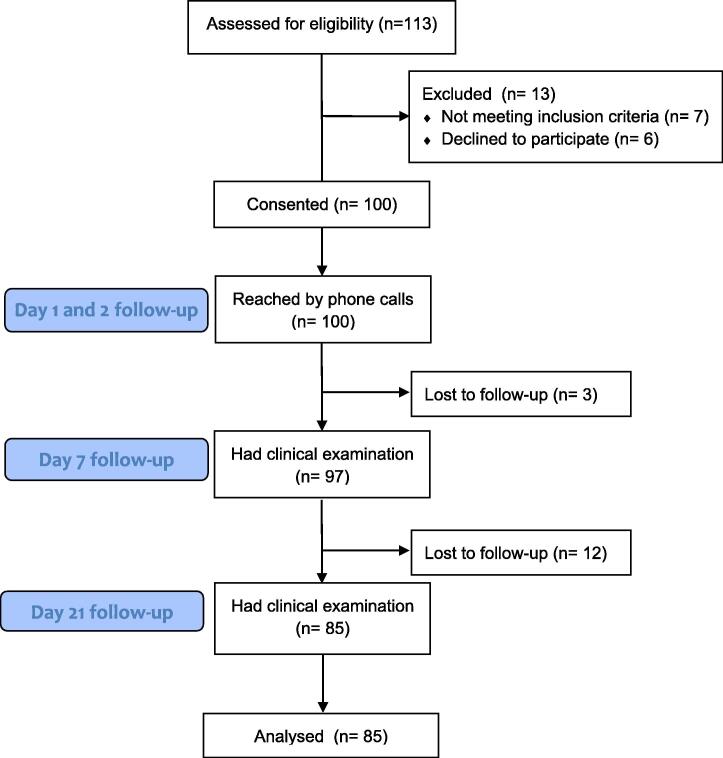
A total of 113 patients were invited to participate in the study. Seven patients did not meet the inclusion criteria as they were pregnant or less than 15 years of age. Six patients declined to participate. One hundred patients consented and enrolled in the study. Lost to follow-up rate was only 15%. Fig. 1 shows a flowchart of patient enrollment. Eighty-five patients complied with the entire study follow-up protocol. Approximately, one-third of the patients were smokers (30.6%). Table 1 shows the demographic characteristics of patients. Almost two-thirds of the patients were females; however, the majority of smokers were males (92%). The majority of smokers belonged to the 36–45 years age group, whereas most nonsmokers were between ages 15 and 35 years. The two groups did not differ in the proportion of patients with medical conditions.
Fig. 1.
Flowchart of study sample enrollment.
Table 1.
Demographic characteristics of all patients including smokers and nonsmokers.
| Variables | Total | Smokers | Nonsmokers | P value |
|---|---|---|---|---|
| (N = 85) | (n = 26) | (n = 59) | ||
| % (n) | % (n) | % (n) | ||
| Gender | <0.0001* | |||
| Male | 36.5% (31) | 92.3% (24) | 11.9% (7) | |
| Female | 63.5% (54) | 7.7% (2) | 88.1% (52) | |
| Age | <0.001* | |||
| 15–25 years | 20.2% (17) | 0 | 28.8% (17) | |
| 26–35 years | 28.2% (24) | 23.1% (6) | 30.5% (18) | |
| 36–45 years | 31.8% (27) | 53.8% (14) | 22.0% (13) | |
| >45 years | 20.0% (17) | 23.1% (6) | 18.6% (11) | |
| Medical conditions | ||||
| Yes | 15.3% (13) | 11.5% (3) | 16.9% (10) | 0.7 |
P value of Chi-square or Fisher’s exact tests.
: statistical significance.
Sixty-eight percent of patients reported compliance with postoperative instructions given by their dentists. Table 2 illustrates smoking-related behavior. Cigarette smoking was most dominant and approximately two-thirds of cigarette smokers reported smoking one pack daily. All the waterpipe smokers reported smoking only once daily. Interestingly, the majority of smokers admitted to smoking after extraction (96.2%).
Table 2.
Smoker patients’ behavior presented in percentages (n).
| Smoking behavior | % (n) | |
|---|---|---|
| Type of smoking | Cigarette smoking | 88.5% (23) |
| Hookah/water pipe | 3.8% (1) | |
| More than one | 7.7% (2) | |
| Number of cigarettes per day | One cigarette | 28% (7) |
| One pack | 68% (17) | |
| More than 1 pack | 4% (1) | |
| For waterpipe smokers, number of sessions in a day | Once | 100% (2) |
| Did you smoke after extraction? | Yes | 96.2% (25) |
Table 3 presents postoperative complications such as bleeding, swelling, trismus, and infection on the 1st, 2nd, 7th, and 21st postoperative days among smokers and nonsmokers. Smokers reported less severe bleeding initially, on day 1 (P = 0.009). After day 1, no differences in bleeding severity were reported. The severity of swelling significantly increased in smokers than in nonsmokers on day 2 (P = 0.04). However, there was no difference between the groups after the second postoperative day. Nonsmokers reported slightly higher rates of trismus on postoperative days 1 and 2, but they did not reach statistical significance. Throughout all postoperative follow-ups, the incidence of infection was only slightly higher among smokers than in nonsmokers (P > 0.05).
Table 3.
Comparison of postoperative complications follow-up (bleeding, swelling, trismus and infection) between smokers and nonsmokers.
| Postoperative Complications | Overall % (n) | Smokers % (n) | Nonsmokers % (N) | P value Chi square or Fisher Exact test | P value for repeated GM model | ||
|---|---|---|---|---|---|---|---|
| Bleeding | Day 1 | No | 2.4% (2) | 0.0% (0) | 3.4% (2) | <0.009* | 0.1 |
| <1 h | 20% (17) | 34.6% (9) | 13.6% (8) | ||||
| 1–2 h | 24.7% (21) | 34.6% (9) | 20.3% (12) | ||||
| 2–3 h | 14.1% (12) | 0.0% (0) | 20.3% (12) | ||||
| More than 3 h | 38.8% (33) | 30.8% (8) | 42.4% (25) | ||||
| Day 2 | No | 89.4% (76) | 92.3% (24) | 88.1% (52) | 1.0 | ||
| <1 h | 1.2% (1) | 0.0% (0) | 1.7% (1) | ||||
| 1–2 h | 2.4% (2) | 3.4% (2) | 0.0% (0) | ||||
| More than 3 h | 7% (6) | 7.7% (2) | 6.8% (4) | ||||
| Day 7 | No | 98.8% (84) | 100.0% (26) | 98.3% (58) | 1.0 | ||
| More than 3 h | 1.2% (1) | 0.0% (0) | 1.7% (1) | ||||
| Day 21 | No | 100% (85) | 100.0% (26) | 100.0% (59) | – | ||
| Swelling | Day 1 | No | 56.5% (48) | 46.2% (12) | 61.0% (36) | 0.6 | 0.2 |
| Mild | 36.5% (31) | 46.2% (12) | 32.2% (19) | ||||
| Moderate | 5.9% (5) | 7.7% (2) | 5.1% (3) | ||||
| Day 2 | No | 70.6% (60) | 53.8% (14) | 78.0% (46) | <0.04* | ||
| Mild | 24.7% (21) | 42.3% (11) | 16.9% (10) | ||||
| Moderate | 4.7% (4) | 3.8% (1) | 5.1% (3) | ||||
| Day 7 | No | 92.9% (79) | 92.3% (24) | 93.2% (55) | 1.0 | ||
| Mild | 6% (7.1) | 7.7% (2) | 6.8% (4) | ||||
| Day 21 | No | 100% (85) | 100.0% (26) | 100.0% (59) | – | ||
| Trismus | Day 1 | No | 88.2% (75) | 96.2% (25) | 84.7% (50) | 0.2 | 0.2 |
| Yes | 11.8% (10) | 3.8% (1) | 15.3% (9) | ||||
| Day 2 | No | 95.3% (81) | 96.2% (25) | 94.9% (56) | 1.0 | ||
| Yes | 4.7% (4) | 3.8% (1) | 5.1% (3) | ||||
| Day 7 | No | 100% (85) | 100.0% (26) | 100.0% (59) | – | ||
| Day 21 | No | 100% (85) | 100.0% (26) | 100.0% (59) | – | ||
| Infection | Day 1 | No | 76.5% (65) | 73.1% (19) | 78.0% (46) | 0.8 | 0.5 |
| Yes | 23.5% (20) | 26.9% (7) | 22.0% (13) | ||||
| Day 2 | No | 95.3% (81) | 92.3% (24) | 96.6% (57) | 0.6 | ||
| Yes | 4.7% (4) | 7.7% (2) | 3.4% (2) | ||||
| Day 7 | No | 95.3% (81) | 92.3% (24) | 96.6% (57) | 0.6 | ||
| Yes | 4.7% (4) | 7.7% (2) | 3.4% (2) | ||||
| Day 21 | No | 98.8% (84) | 100.0% (26) | 98.3% (58) | 1.0 | ||
| Yes | 1.2% (1) | 1.7% (1) | 0.0% (0) | ||||
: statistical significance.
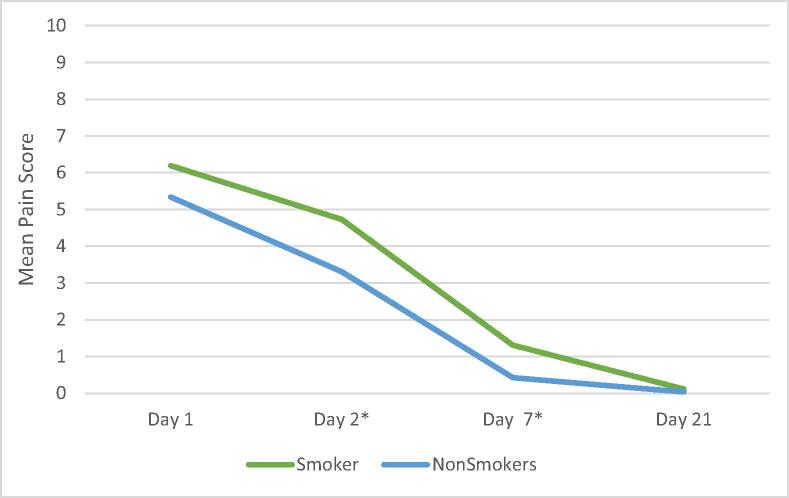
Overall, smokers consistently reported more postoperative pain than nonsmokers at all points (Fig. 2). Moreover, this relationship reached statistical significance on the second and seventh post-operative days.
Fig. 2.
Mean Pain Score of smokers and nonsmokers.
Generalized models for repeated measures indicated no statistically significant interaction between smoking status and any of the postoperative complications. The main effect of one’s smoking status showed a statistically significant difference in terms of only one of the postoperative complications i.e. pain, which was assessed by the mean pain score on different postoperative days (P < 0.0001, partial η2 = 0.76). A Bonferroni pairwise comparison showed that the mean pain score was significantly different between all pairs of postoperative days.
When assessing the effect of time for each of the postoperative complications regardless of the smoking status, generalized models for repeated measures demonstrated a significant reduction in postoperative complications with time, except for that in trismus. Patient-reported bleeding significantly increased in smokers on day 1, compared to the other postoperative days. Facial swelling was comparable on postoperative days 1 and 2 and significantly decreased after the second postoperative day (P < 0.0001). Reported infection significantly reduced over time (P < 0.0001), except on days 2 and 7, when there was no observable change.
4. Discussion
The purpose of this study was to evaluate postoperative complications in smokers compared with nonsmokers on days 1, 2, 7, and 21 after minor oral surgical procedures. We observed that patient-reported pain was the only complication that was significantly greater in smokers than in nonsmokers. Our results are in agreement with the studies conducted by Grossi et al. and Larrazábal et al., who showed that smoking was associated with higher pain perception and discomfort following surgical extraction of lower third molars (Grossi et al., 2007, Larrazábal et al., 2010). In contrast, Al-Delayme demonstrated that cigarette smoking did not affect the severity of pain, swelling, or trismus after lower third molar surgical extractions (Al-Delayme, 2013). In this study, the highest intensity of pain was reported on the first day. This finding supports the observations of López-Carriches et al., who stated that pain levels peak 12 to 24 h after surgical extraction of lower third molars (López-Carriches et al., 2006). In this study, differences in the severity of pain disappeared after the 7th postoperative day. The results are in agreement with previous reports that a return to preoperative quality of life is expected after the end of the first postoperative week (López-Carriches et al., 2006, Pandurić et al., 2009).
In our study, the most frequent patient-reported complications following routine dental extractions were bleeding (97.6%), pain (89.4%), and swelling (42.4%), in order of frequency. However, Malkawi et al. showed that the most frequent complications after surgical extraction of mandibular third molars were mild pain, swelling, and trismus. These differences could be attributed to the challenges associated with surgical extractions that increased the risk of immediate and delayed postoperative complications such as trismus (Malkawi et al., 2011). In this study, smokers exhibited less bleeding on day 1. The findings are supported by Feldman et al. who showed that smokers had less clinical signs of inflammation and gingival bleeding compared to nonsmokers. This observation may be attributed to the effect of nicotine that contributes to local vasoconstriction, reduced blood flow, and edema (Feldman et al., 1983). The differences in swelling on the second postoperative day could be attributed to smoking-induced endothelial dysfunction and an increase in the intercellular adhesion molecule-1 (ICAM-1) level (Fraser et al., 2001, Koundouros et al., 1996).
Although Grossi et al. affirmed that trismus was the most significant predictor of patient discomfort (Grossi et al., 2007), we found that only 11.8% of patients reported postoperative trismus. Infection was more common among smokers than in nonsmokers, but it did not reach statistical significance. The results are consistent with previous findings (Rodriguez-Argueta et al., 2011). The association between smoking and dry socket is controversial in the literature. A community-based research in Australia showed no significant association between smoking and dry socket (Parthasarathi et al., 2011). However, studies conducted by Khan et al. concluded that smoking increased dry socket incidence by 4.2%. They observed that dry socket was significantly more prevalent in mandibular extractions compared to maxillary extraction cases (Khan et al., 2017).
Our study sample included more females (63.5%) than male patients. The sex distribution of patients was similar to that in the study conducted by Malkawi et al. The similarity could be justified by the fact that both samples were derived from a pool of dental school oral surgery patients. Nearly 30% of the sample comprised of smokers, slightly above the national smoking average in the Kingdom of Saudi Arabia (12.2%). The predominance of male smokers in this study sample is in agreement with the national figures (Moradi-Lakeh et al., 2015). While 68.4% of our patients complied with post-operative instructions, the majority (96%) admitted to smoking after dental extraction. The patient compliance rate concurred with that in Alsaleh et al.’s study, which reported compliance of 73% (Alsaleh et al., 2018). It was interesting that 28% did not consider smoking cessation as a part of their postoperative extraction instructions, which suggests that more emphasis needs to be placed on smoking cessation to reduce post-operative complications. It has been documented that while most smokers want to quit, the majority reported never being advised by their physicians to discontinue smoking (Joshi et al., 2010). The study highlights the social responsibility of the dental profession towards patients who smoke.
The main strengths of this study were the prospective design and the extensive follow-up period of 21 days, which reduced the likelihood of recall bias and supported the study’s validity. Moreover, this study focused on patient-reported outcomes rather than immunohistochemistry findings, which are more relevant to patient-centered care. A limitation of this study was that the study sample was recruited from a dental school, which may limit the generalizability to different healthcare settings, such as private practice. Other limitations were the uneven recruitment according to smoking status and limited sample size. Future studies should analyze the differences in postoperative complications according to the type of smoking and examine postoperative complications associated with electronic cigarettes.
5. Conclusions
The patient-reported pain score was consistently higher among smokers than in nonsmokers for the first 7 days. The findings suggested that the initial differences in patient-reported complications (pain, bleeding, and swelling) between smokers and nonsmokers undergoing minor oral surgical procedures disappeared after a week. Trismus and infection showed no significant differences according to smoking status.
Financial support and sponsorship
Nil.
Declaration of Competing Interest
The authors have no conflicts of interest to declare.
Footnotes
Peer review under responsibility of King Saud University.
Contributor Information
Alaa A. Sanari, Email: dr.a.sanari@gmail.com.
Bushra A. Alsolami, Email: bushra.alsolami@hotmail.com.
Hala M. Abdel-Alim, Email: habdelalim@kau.edu.sa.
Mohammed Y. Al-Ghamdi, Email: Myalghamdi@kau.edu.sa.
Dalia E. Meisha, Email: dmeisha@kau.edu.sa.
References
- Al-Delayme R.M. The effect of cigarette smoking on the severity of pain, swelling and trismus after the surgical extraction of impacted mandibular third molar. J. Clin. Exp. Dent. 2013;5(3):117–121. doi: 10.4317/jced.50979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albandar J.M., Streckfus C.F., Adesanya M.R., Winn D.M. Cigar, pipe, and cigarette smoking as risk factors for periodontal disease and tooth loss. J. Periodontol. 2000;71(12):1874–1881. doi: 10.1902/jop.2000.71.12.1874. [DOI] [PubMed] [Google Scholar]
- Alsaleh M.K., Alajlan S.S., Alateeq N.F., Alamer N.S., Alshammary F., Alhobeira H.A., Khan S., Siddiqui A.A. Alveolar osteitis: patient’s compliance with post-extraction instructions following permanent teeth extraction. J. Contemp. Dent. Pract. 2018;19(12):1517–1524. [PubMed] [Google Scholar]
- Fraser H.S., Palmer R.M., Wilson R.F., Coward P.Y., Scott D.A. Elevated systemic concentrations of soluble ICAM-1 (sICAM) are not reflected in the gingival crevicular fluid of smokers with periodontitis. J. Dent. Res. 2001;80(7):1643–1647. doi: 10.1177/00220345010800070901. [DOI] [PubMed] [Google Scholar]
- Feldman R.S., Bravacos J.S., Rose C.L. Associations between smoking, different tobacco products and periodontal disease indexes. J. Periodontol. 1983;54(8):481–487. doi: 10.1902/jop.1983.54.8.481. [DOI] [PubMed] [Google Scholar]
- Garcia B., Penarrocha M., Marti E., Gay-Escodad C., von Arx T. Pain and swelling after periapical surgery related to oral hygiene and smoking. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2007;104(2):271–276. doi: 10.1016/j.tripleo.2007.01.025. [DOI] [PubMed] [Google Scholar]
- Giorgetti A.P.O., César Neto J.B., Casati M.Z., Sallum E.A., Nociti Júnior F.H. Cigarette smoke inhalation influences bone healing of post-extraction tooth socket: a histometric study in rats. Braz. Dent. J. 2012;23(3):228–234. doi: 10.1590/s0103-64402012000300008. [DOI] [PubMed] [Google Scholar]
- Grossi G.B., Maiorana C., Garramone R.A., Borgonovo A., Creminelli L., Santoro F. Assessing postoperative discomfort after third molar surgery: a prospective study. J. Oral Maxillofac. Surg. 2007;65(5):901–917. doi: 10.1016/j.joms.2005.12.046. [DOI] [PubMed] [Google Scholar]
- Jha P., Ramasundarahettige C., Landsman V., Rostron B., Thun M., Anderson R.N., McAfee T., Peto R. 21st-century hazards of smoking and benefits of cessation in the United States. N. Engl. J. Med. 2013;368(4):341–350. doi: 10.1056/NEJMsa1211128. [DOI] [PubMed] [Google Scholar]
- Joshi V., Suchin V., Lim J., Edin M. Smoking cessation: barriers, motivators and the role of physicians — a survey of physicians and patients. Proc. Singapore Healthc. 2010;19(2):145–153. [Google Scholar]
- Kasat V., Ladda R. Smoking and dental implants. J. Int. Soc. Prev. Commun. Dent. 2012;2(2):38–41. doi: 10.4103/2231-0762.109358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan A.H. Prevalence and association of dry socket in oral health and dental management. Int. J. Oral Surg. 2017;16(4):1–6. [Google Scholar]
- Koundouros E., Odell E., Coward P., Wilson R., Palmer R.M. Soluble adhesion molecules in serum of smokers and non-smokers, with and without periodontitis. J. Periodontal Res. 1996;31(8):596–599. doi: 10.1111/j.1600-0765.1996.tb00525.x. [DOI] [PubMed] [Google Scholar]
- Ladewig N.M., Tedesco T.K. Patient-reported outcomes associated with different restorative techniques in pediatric dentistry : a systematic review and MTC meta- analysis. PLoS ONE. 2018;13(12):e0208437. doi: 10.1371/journal.pone.0208437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larrazábal C., García B., Peñarrocha M., Peñarrocha M. Influence of oral hygiene and smoking on pain and swelling after surgical extraction of impacted mandibular third molars. J. Oral Maxillofac. Surg. 2010;68(1):43–46. doi: 10.1016/j.joms.2009.07.061. [DOI] [PubMed] [Google Scholar]
- López-Carriches C., Gómez-Font R., Martínez-González J.M., Donado-Rodríguez M. Influence of smoking upon the postoperative course of lower third molar surgery. Med. Oral Patol Oral Cir Bucal. 2006;11(1):E56–E60. [PubMed] [Google Scholar]
- Malkawi Z., Al-Omiri M.K., Khraisat A. Risk indicators of postoperative complications following surgical extraction of lower third molars. Med. Princ. Pract. 2011;20(4):321–325. doi: 10.1159/000324550. [DOI] [PubMed] [Google Scholar]
- McCormack H.M., Horne D.J., Sheather S. Clinical applications of visual analogue scales: a critical review. Psychol. Med. 1988;18(4):1007–1019. doi: 10.1017/s0033291700009934. [DOI] [PubMed] [Google Scholar]
- Moradi-Lakeh M., El Bcheraoui C., Tuffaha M., Daoud F., Al Saeedi M., Basulaiman M., Memish Z.A., AlMazroa M.A., Al Rabeeah A.A., Mokdad A.H. Tobacco consumption in the Kingdom of Saudi Arabia, 2013: findings from a national survey. BMC Public Health. 2015;15:611. doi: 10.1186/s12889-015-1902-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagahisa K., Arai K., Baba S. Study on oral health-related quality of life in patients after dental implant treatment with patient-reported outcome. Int. J. Oral Maxillofac. Impl. 2018;33(5):1141–1148. doi: 10.11607/jomi.6496. [DOI] [PubMed] [Google Scholar]
- Nazir M.A., Almas K. Awareness about the effects of tobacco consumption on oral health and the possibility of smoking behavior among male Saudi schoolchildren. Eur. J. Dent. 2017;11(1):29–35. doi: 10.4103/ejd.ejd_300_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pandurić D.G., Brozović J., Susić M., Katanec D., Bego K., Kobler P. Assessing health-related quality of life outcomes after the surgical removal of a mandibular third molar. Coll. Antropol. 2009;33(2):437–447. [PubMed] [Google Scholar]
- Rad M., Kakoie S., Brojeni F.N., Pourdamghan N. Effect of long-term smoking on whole-mouth salivary flow rate and oral health. J. Dent. Res. Dent. Clin. Dent Prosp. 2011;4(4):110–114. doi: 10.5681/joddd.2010.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez-Argueta O.F., Figueiredo R., Valmaseda-Castellon E., Gay-Escoda C. Postoperative complications in smoking patients treated with implants: a retrospective study. J. Oral Maxillofac. Surg. 2011;69(8):2152–2157. doi: 10.1016/j.joms.2011.02.082. [DOI] [PubMed] [Google Scholar]
- Sacristán J.A. Patient-centered medicine and patient-oriented research : improving health outcomes for individual patients. BMC Med. Inform. Decis. Mak. 2013;13:6. doi: 10.1186/1472-6947-13-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salama R. Challenges facing smokers in Saudi Arabia. Int. J. Heal. Sci. 6. 2012;2:V-VI. doi: 10.12816/0005986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheiham A. Oral health, general health and quality of life. Bull World Health Organ. 2005;83(9):644. [PMC free article] [PubMed] [Google Scholar]
- Singh Soodan K., Priyadarshni P., Kaur K. An effect of smoking on wound healing following extraction: a critical study. IOSR J. Dent. Med. Sci. 2015;14(9):66–70. [Google Scholar]
- Parthasarathi K., Smith A., Chandu A. Factors affecting incidence of dry socket: a prospective community-based study. J. Oral Maxillofac. Surg. 2011;69(7):1880–1884. doi: 10.1016/j.joms.2010.11.006. [DOI] [PubMed] [Google Scholar]
- U.S. National Cancer Institute and World Health Organaization, 2016. The economics of tobacoo and tobacco control. Bethseda, MD: U.S. Department of Health and Human services, National Institutes of Health, National Cancer Instutute; Geneva, CH: World Health Organization. National cancer institute tobacco control monograph 21. NIH publication No. 16-CA-8029A.
- Warnakulasuriya S., Dietrich T., Bornstein M.M., Casals Peidró E., Preshaw P.M., Walter C., Wennström J.L., Bergström J. Oral health risks of tobacco use and effects of cessation. Int. Dent. J. 2010;60(1):7–30. [PubMed] [Google Scholar]
- Yanagisawa T., Ueno M., Shinada K., Ohara S., Wright F.A.C., Kawaguchi Y. Relationship of smoking and smoking cessation with oral health status in Japanese men. J. Periodontal Res. 2010;45(2):277–283. doi: 10.1111/j.1600-0765.2009.01233.x. [DOI] [PubMed] [Google Scholar]
- Zawawi K.H., Al-Badawi E.A., Lobo S.L., Melis M., Mehta N.R. An index for the measurement of normal maximum mouth opening. J. Can. Dent. Assoc. 2003;69(11):737–741. [PubMed] [Google Scholar]