Abstract
Echo intensity is the mean pixel intensity of a specific region of interest from an ultrasound image. This variable has been increasingly used in the literature as a physiological marker. Although there has been an increased interest in reporting changes in echo intensity in response to exercise, little consensus exists as to what a change in echo intensity represents physiologically. The purpose of this paper is to review some of the earliest, as well as the most up to date literature regarding the changes in echo intensity in response to exercise. Echo intensity has been used to measure muscle quality, muscle damage, acute swelling, and intramuscular glycogen. The changes in echo intensity, however, are not consistent throughout the literature and often times lead to conclusions that seem contrary to the physiologic effects of exercise. For example, echo intensity increases in conjunction with increases in strength, contrary to what would be expected if echo intensity was a marker of muscle quality/muscle damage. It is conceivable that a change in echo intensity represents a range of physiologic effects at different time points. We recommend that these effects should be determined experimentally in order to rule out what echo intensity might and might not represent. Until this is done, caution should be employed when interpreting changes in echo intensity with acute and chronic exercise.
Keywords: Muscle quality, Edema, Muscle damage, Glycogen content, Fluid shift, Muscle swelling, Ultrasound, Intracellular, Exercise
Introduction
A variety of imaging techniques are available for examining skeletal muscle components. Although not the same, the most popular methods include magnetic resonance imaging (considered the gold standard) [1], computed tomography [2], and ultrasonography [3, 4]. Among these, ultrasonography is reported to be the most accessible, noninvasive, and practical method for imaging changes in muscle size [5, 6]. Given this, there has been an increased use of ultrasound (i.e. brightness mode [B-mode] ultrasonography) in resistance exercise studies to quantify muscle size [3–10]. Ultrasound has also been used to quantify echo intensity [11–13], which is a variable that can be obtained from the same image used to assess skeletal muscle size.
Changes in echo intensity have been investigated in response to resistance exercise in both acute [4, 14–18] and chronic [3, 7–10, 12, 19–56] studies involving skeletal muscle. Echo intensity relates to the pixel density of the image and was initially quantified by visual scoring (arbitrarily depicting if an image is darker or lighter) from ultrasound images [13]. Although a few techniques exist in order to extract an arbitrary unit for echo intensity, most researchers now use image-processing programs, such as ImageJ (National Institute of Health, Bethesda, MD, United States) to determine echo intensity based on quantifying the pixel intensity of an ultrasound image (Fig. 1). Echo intensity is determined by drawing a region of interest on the ultrasound image without including subcutaneous fat or bone. This region of interest may be a pre-specified sized box [3, 31, 33, 36, 40, 42, 48–51, 53, 54], a box containing as much of the muscle as possible [4, 7, 8, 10, 20, 23, 24, 27, 35, 37, 57, 58], or free hand tracings between the adipose tissue and bone [9, 15]. The majority of studies on echo intensity use a scale between 0 (black) and 255 (white) [4, 20, 24] or 0 (black) to 256 (white) [29, 31, 34]. However, other studies use a reverse scale ranging from 0 (white) to 100 (black) [14, 16, 19]. Interestingly, although there has been a heightened interest in reporting changes in echo intensity in response to exercise, little consensus exists as to what a change in echo intensity represents physiologically. Although not currently known, many hypotheses exist regarding what changes in echo intensity might represent. The purpose of this paper is to review the past literature regarding changes in echo intensity in response to exercise and future considerations towards the usefulness of this measurement technique along with what echo intensity may or may not represent.
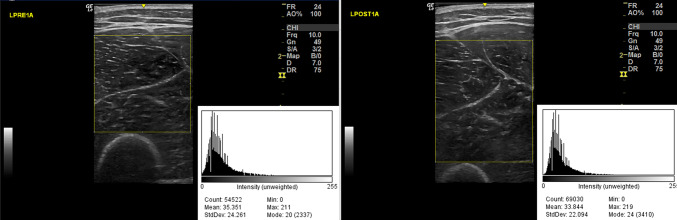
Fig. 1.
Comparison of echo intensity from pre and post resistance exercise. The settings are the same from pre to post ultrasound imaging. The image on the left depicts the left anterior thigh before exercise and the figure on the right depicts the left anterior thigh immediately after exercise. The yellow box represents the region of interest. The histograms display quantification of the echo intensity for each image
Methods
Literature search and inclusion criteria
Different available databases were searched to find studies on the use of ultrasonography and the changes in echo intensity in response to exercise. The databases used included PubMed (Public/Publisher Medline), Google Scholar, Scopus, Embase (Elsevier), and OVID (Offshore Vessel Inspection Database). The time frame of the search was from May to August 2019. Search terms that were used to locate these studies were: “echo intensity and muscle damage”, “echo intensity and muscle quality”, “echo intensity and muscle quality and exercise”, “echo intensity and edema and exercise”, “echo intensity and edema”, “changes in echo intensity”, “echo intensity and exercise”, “MuscleSound glycogen”, and “echo intensity skeletal muscle ultrasound”. Other studies were then located within the studies that we were reviewing. Studies were included in this review if changes in echo intensity caused by exercise were reported. The focus of this review was on human data. Studies using animals were only included to provide the origin of specific ideas from later studies. Studies were excluded if they were case studies, did not include exercise, if they did not look at the changes in echo intensity, and if the studies were not written in English. Studies utilizing animals and/or not investigating changes in response to exercise were excluded from our tables, but we did provide discussion from these studies where we felt pertinent.
Results
Muscle quality
Muscle quality is an umbrella term used to describe the relationship between muscle function and the intramuscular structures. Traditionally, muscle quality has been defined as muscle strength or power per unit of muscle mass [59, 60]. With inactivity and aging, there has been some suggestion that the contractile tissue might be replaced by fibrous and adipose tissue, thus decreasing the quality of muscle [47, 61–63]. This has been determined in humans by quantifying changes in echo intensity [7–10, 20–27, 45, 47, 57, 64] (Table 1). It has been stated that an increase of echo intensity represents changes caused by increased fibrous and adipose tissue [62, 65]. The lower (darker) the echo intensity, the better the quality of muscle [7–10, 20–27, 45, 47, 57, 64]. This hypothesis is based on past literature observing older adults with muscle disease [62, 66] and observations in dogs with muscular dystrophy that reported that animals with higher echo intensities also had higher interstitial fibrous tissue content [67].
Table 1.
Changes in echo intensity used as a marker of muscle quality
| References | Participants (age in years) | Exercise | Measurement site | Measurement time points | Posture of measurement | Region of interest | Results | Notes |
|---|---|---|---|---|---|---|---|---|
| Jajtner et al. [22] |
28 women (20.5 ± 1.2) |
8 exercises RT program 2/week |
50% of VL and RF | Pre and 12 weeks | Supine | N/A | Decreased | Scale was 0–256 |
| Scanlon et al. [64] | 13 women and 13 men (> 60) |
RT 2/week for 6 weeks (2–4 sets of 8–12 repetitions of 6–10 exercises) |
RF and VL | Pre and 6 weeks | Supine | Tracing of as much of muscles as possible | No changes in |
Scale was 0–255 Contained a non-exercise control group |
| Radaelli et al. [23] |
20 women (60–74) |
1 or 3 sets of 10 exercises movements 2/week |
Not specified region of RF | Pre and 13 weeks | Supine | As much of muscle with a box b/w fat and bone | Decreased | Scale was 0–255 |
| Radaelli et al. [24] |
24 women (60–74) |
1–3 sets of 9 exercise (total body) 2/week |
Quadriceps | Pre, 6, 13, and 20 weeks | Supine | As much of muscle with a box b/w fat and bone | Decreased | Scale was 0–255 |
| Cadore et al. [20] | 14 women and 8 men (22.9 ± 7.8 and 21.3 ± 3.3) |
2–5 × 8–12 isokinetic (60°/s) knee flexions 2/week |
Vastus lateralis | Pre and 6 weeks | Supine | As much of muscle with a box b/w fat and bone | Decreased | Compared changes between a concentric and eccentric group |
| Fukumoto et al. [46] |
39 women High-velocity: 52.4 ± 9.2 Low-velocity: 52.5 ± 10.1 |
Daily RT with elastic band for 8 weeks | Gluteus maximus, gluteus medius and QF | Pre and 8 weeks | N/A | N/A | Gluteus maximus decreased and no changes in gluteus medius and QF | Scale was 0–255 and used Adobe Photoshop Elements |
| Yoshiko et al. [26] | 10 women and 7 men (78 ± 8) | Physical training 1–2/week | RF, BF, and thigh | Pre, 6, and 12 months | Supine | Tracing of muscles; thigh EI estimated [(RF in EI + BF in EI)/2] | RF and thigh decreased after 6 months; BF and thigh increased from 6 to 12 months | Control group had higher EI than training group after 6 months |
| Blue et al. [9] | 44 overweight or obese women and men (35.4 ± 12.3) | HIIT training (9 sessions) | Panoramic scan of the VL | Pre and 3 weeks | Supine | As much of muscle as possible | No changes | |
| Yoshiko et al. [7] | 64 men and women (≤ 65) |
Walking (2/week) and walking + RT (3/week) |
VL, RF and QF | Pre and 10 weeks | Supine | As much of muscle with a rectangle b/w fat and bone | Decreased | RF (Walking) decreased muscle thickness as RF (Walking + RT) increased but both EI decreased |
| Mangine et al. [25] |
15 men (24.0 ± 3.0) |
4 × 3–5 LB RT 2/week |
RF and VL (30, 50, and 70%) | Pre and 8 weeks | Supine | N/A | Increase only in RF (70%) | Average out of 2 images |
| Santos et al. [27] | 28 men (20.0 ± 3.3) |
Concentric and Eccentric RT 3/week |
3 different muscle belly sites each: VL, VM, VI, and RF |
Pre, 6, 15 weeks | Seated with leg held at 10° flexion | As much of muscle with a rectangle b/w fat and bone |
Lower VL: increased Middle VL: decreased VM: no change VI: decreased RF: no change |
|
| Yoshiko et al. [8] |
11 women and 9 men Long-term care (76.7 ± 5.6) versus non-long-term care (72.9 ± 6.6) |
Physical training 1–2/week | RF, BF, and thigh | Pre and 24 months | Supine for anterior regions and prone with full extension of posterior regions | As much of muscle with a rectangle b/w fat and bone | No changes | Strength did not change in training group but decreased in control group. Muscle thickness increased in BF and thigh |
| Bassan et al. [10] |
16 men 25.1 ± 4.1 |
3 × 10 maximal voluntary contractions of 4 s for unilateral knee extensor | RF and VI | Pre and 3 weeks | Supine | As much of muscle with a rectangle b/w fat and bone | No changes |
0–255 scale Strength and muscle thickness increased |
| Rowe et al. [57] |
17 men (24 ± 4) |
Bout of unilateral biceps curls on preacher bench | Biceps | Pre, 24, 48, and 72 h | Supine with arm abducted | Positioned ~ 3 mm from both the humerus and the superficial biceps brachii fascia and ~ 5 mm from the sides of the images | Increased | |
| Yamada et al. [21] | 112 women and men ≥ 65 years |
3 × 20 lower body weight exercise (7 total) and added nutrition 2/week |
RF and VI | Pre and 12 weeks | Supine | n/a |
RF: decreased VI: no change |
Used Adobe Photoshop Elements |
| Botton et al. [45] |
18 women and 26 men (69.7 ± 6.9) |
Linear periodization model of RT 3/week | RF | Pre | Supine | As much of muscle b/w fat and bone | No changes | Scale was 0–255 |
Measurement timepoints were measured based from exercise, thus 0 h indicates immediately after exercise. The decrease of echo intensity indicates the increase in muscle quality
N/A not available, b/w between, VL vastus lateralis, VI vastus intermedius, VM vastus medialis, RF rectus femoris, BF biceps femoris, QF quadriceps femoris, RT resistance training
Although echo intensity is used as a marker for changes in muscle quality [7–10, 20–27], studies using changes in echo intensity as a proxy have produced inconsistent results following resistance training (Table 1). Echo intensity has been reported to decrease [7, 20–24, 26, 27, 46], increase [25, 27, 57], or remain unchanged [8–10, 21, 27, 44–46, 64] following repeated bouts of resistance exercise. Using the traditional definition, a decrease in echo intensity should correspond to an increase in muscle strength per unit of muscle mass [9, 20]. The use of echo intensity is based on the assumption that a change in intramuscular content will impact performance. An increase in echo intensity should represent a reduction in performance as that would indicate lower muscle quality. In contrast, a decrease in echo intensity should occur with an improvement in performance. Scanlon and colleagues implemented a 6-week resistance training program with a non-exercise time matched control group [64]. There were group × time interactions for muscle strength and cross-sectional area, indicating that the muscle size and strength increased across time. However, there was no interaction with echo intensity, suggesting that echo intensity did not change with resistance training [64]. A study by Yoshiko et al. [26] observed a decrease in echo intensity (indication of improvement in muscle quality) following 6 months of resistance training but echo intensity returned back to baseline in the next 6 months. This return to baseline occurred despite continued training with resultant strength increases [26]. Although changes in muscle quality are predicted based on changes in echo intensity, it seems unlikely that there were exercise induced decreases followed by increases in intramuscular fibrotic/adipose tissue. Based on these inconsistent findings, the use of exercise induced changes in echo intensity for inferring changes in muscle quality should be made with caution.
Muscle damage
Resistance exercise, particularly unaccustomed exercise, can lead to muscle damage in the days following the bout of exercise. Exercise induced muscle damage is often determined based on changes in indirect markers such as strength, blood proteins (i.e. myoglobin and creatine kinase activity), soreness, and swelling. More recently, the change in echo intensity as measured via ultrasound has been used as a marker for muscle damage [3, 12, 19, 28–44, 48–56, 68, 69] (Table 2). An increase in echo intensity has also been used prevalently in the literature to represent tissue (connective and muscle) damage, and inflammation. This increase of echo intensity (i.e. brighter image) has been suggested to represent the accumulation of inflammatory cells between muscle fibers [12, 31, 70]. Since the infiltration of inflammatory cells is known to peak 3–4 days after a muscle damaging event, various studies have concluded that the increase in echo intensity during that time period allowed them to infer that echo intensity is a measurement of exercise-induced edema and inflammation [3, 33, 39, 40].
Table 2.
Changes in echo intensity used as a marker of muscle damage
| References | Participants (age in years) | Exercise | Measurement site | Measurement time points | Posture of measurement | Region of interest | Results | Notes |
|---|---|---|---|---|---|---|---|---|
| Nosaka and Clarkson [12] |
14 men (21.9 ± 1.9) |
24 maximal eccentric actions from 50° to 100° on a modified arm curl machine (non-dominant arm) | Anterior arm (biceps brachialis and biceps brachii) | Pre, 0, 1, 2, 3, 4, and 5 days | Arm relaxed in a palm-up position on a table | N/A | Authors report 8 out of 14 increase | Results predominantly in the brachialis 3–5 days after exercise |
| Nosaka and Sakamoto [52] |
10 men (19.8 ± 1.9) |
24 maximal eccentric actions from 50° to 130° or 100° to 180° on a modified arm curl machine | 7 cm above elbow joint (biceps brachialis and biceps brachii) | Pre, 0, 1, 2, 3, 4, and 5 days | N/A | N/A | Increased | |
| Nosaka et al. [51] | 22 men (20.3 ± 1.6) | 24 maximal eccentric actions from 130° to 180° or 50° to 100° on a modified arm curl machine (non-dominant arm) | Biceps brachialis and biceps brachii | Pre, 0, 1, 2, 3, and 4 days | Sitting with forearm on armrest | 1 cm × 1 cm × 1 cm2 | Increased | |
| Chen and Nosaka [19] | 41 men and 10 women (20.5 ± 2.1) | 30 eccentric elbow flexors dumbbell (100% maximal isometric force at the elbow joint angle of 90° | Anterior Arm (4 and 8 cm from elbow) | Pre, 2, 4, and 9 days | Sitting | 2 × 2 = 4 cm2 | Increased | Scale was 0–100 |
| Chen et al. [28] | 15 men (21.8 ± 1.9) | 4 × 30 max isokinetic eccentric contractions of the elbow flexors every 4 weeks | Anterior arm (4–8 cm from elbow) | Pre, 48, and 120 h following each ex bout | Sitting | 2 × 2 = 4 cm2 | Increased | Scale was 0–256 |
| Chen et al. [29] | 30 men (22.2 ± 2) | 4 bouts of eccentric preacher curls | Anterior arm (4–8 cm from elbow) | Pre, 2, and 5 day | Sitting | 2 × 2 = 4 cm2 | Increased | Scale was 0–256 |
| Chen et al. [30] | 17 men (21.1 ± 2.1) | 5 × 6 maximal isokinetic eccentric contraction of knee/elbow extension/flexion | Mid-portion of the biceps brachii, long head of the triceps brachii, RF and BF | Pre, 1, 2, 3, 4, and 5 days |
EF: Sitting EE: Prone KE: Supine KF: Prone |
2 × 2 = 4 cm2 | Increased | Increased muscle damage |
| Chen et al. [55] | 65 men (21.3 ± 1.6) | 5 × 6 maximal eccentric contractions of elbow flexors at 30°/s | Mid-portion of the biceps brachii | Pre, 2, and 5 days | Sitting | 2 × 2 = 4 cm2 | Increased |
Scale was 0–256 5 different groups (30 reps of 10% 1RM at different time points) |
| Radaelli et al. [31] |
10 women (22.7 ± 3.2) |
4 × 10 Unilateral biceps Curls at 80% 1RM |
8 cm above elbow joint | Pre, 0, 24, 48, 72 h | Supine | 1 cm2 region | Increased | Scale was 0–256 |
| Pereira et al. [54] |
22 men (24.6 ± 5.1) |
4 × 10 isokinetic eccentric/concentric elbow flexion | Biceps brachii | Pre, 0, 24, 48, 72, and 96 h | Supine | 1 cm2 region | Increased from Pre to 0 but was significantly less from 24 to 96 h compared to 0 | Scale was 0–256 |
| Radaelli et al. [53] | 10 women (22.7 ± 1.7) and 10 men (23.1 ± 1.9) | 4 × 10 unilateral biceps curls at 80% 1RM | Mid-portion of biceps | Pre, 0, 24, 48, and 72 h | Supine with arm by their side | 1 cm2 region | Increased |
Scale was 0–255 Compared sex differences (no difference) |
| Chen et al. [68] |
65 men (21.8 ± 2.3) |
5 × 6 maximal voluntary eccentric contractions of elbow flexors | Mid-portion of biceps brachii | Pre, and 1, 2, 3, 4, 5, 6, 7, 8, 9, and 10 days | N/A | 2 × 2 = 4 cm2 | Increased |
Scale was 0–256 Total of 5 groups differing in time of maximal voluntary contractions (2) from exercise protocol |
| Chen et al. [32] |
26 men (66.4 ± 4.6) |
6 × 10 maximal eccentric knee flexion at 30° s−1 | Mid RF | Pre, 1, 2, 3, 4, and 5 days | Supine | 2 × 2 = 4 cm2 | Increased | Scale was 0–256 |
| Gonzalez-Izal et al. [33] | 16 men and women (21.5 ± 6.9) | 4 × 20 max contractions (CON or ECC, depending the session) of flexors and extensors of knee (0–90) at 60°/s | Mid portion of VL | Pre and 48 h | Supine | 2 cm2 region | Increased |
Scale was 0–256 Change of EI in exercise leg > control leg |
| Lau et al. [50] | 10 men | 2 bouts (7-day separation) 10 × 6 maximal isokinetic (60°/s) eccentric contractions of elbow flexors | Biceps brachii midbelly at 9 cm above the elbow crease | Pre, 0, 1, 2, 3, 4, 5, 6, and 7 days | N/A | 1 × 1 cm | Increased after Bout 1 but no changes after bout 2 | Scale was 0–255 |
| Chen et al. [49] |
104 men (22.0 ± 1.8) |
5 × 6 maximal voluntary isokinetic eccentric contractions of elbow flexors 30°/s starting at 90° flexion | Mid portion of biceps brachii | Pre, 0, 1, 2, 3, 4, and 5 days after the first and second exercise | N/A | 2 × 2 = 4 cm2 | Increased |
Scale was 0–256 Observing contralateral repeated bout effects |
| Damas et al. [34] | 10 men (27 ± 3) |
Isoinertial concentric-eccentric bilateral 45° leg press and extensions (2/week) |
Mid portion of VL | Pre, 3, and 10 weeks | Supine | N/A | Increased |
Scale was 0–256 Ultrasound pictures were opened on PowerPoint and each image was manually rotated to reconstruct vastus lateralis |
| Jenkins et al. [35] |
15 men (21.7 ± 2.4) |
Bicep curls to failure | 33% of anterior arm | Pre, 2, 4 weeks | Supine | As much of muscle with a box b/w fat and bone | No changes | |
| Fritsch et al. [36] | 24 men (18–35) | 10 × 10 counter-movement jump | Midpoint of RF | Pre, 24, 48, and 72 h | Supine | 1 cm2 positioned at midpoint of RF | Increased | Scale was 0–255 EI used to compare muscle damage between a treatment protocol versus placebo |
| Medeiros et al. [3] | 40 men (18–34) | 4 × 10 isokinetic biceps curls | Anterior arm (8 cm above elbow) | Pre, 0, 24, 48, 72, and 96 h | Supine | 1 × 1 = 1 cm2 | Increased | |
| Stock et al. [37] | 13 men (23 ± 4) | 8–12 (failure) unilateral concentric-only dumbbell curls and shoulder presses 2/week | 66% of anterior arm | Pre, 72 or 96 h each week (8 Total) | Supine | As much of muscle with a rectangle b/w fat and bone | No change | |
| Jenkins et al. [58] | 26 men (23.1 ± 4.7) |
Leg extensions High load: 3 × failure at 80% 1RM Low load: 3 × failure at 30% 1RM |
VL, VM, and RF | Pre, 2, and 6 weeks | Supine | As much of muscle with a rectangle b/w fat and bone | Both groups decreased at 6 weeks |
Settings: gain of 50 dB, frequency of 10 MHz, and depth of 8 cm p = .07 and .09 were recorded as significant in study |
| Brusco et al. [39] | 10 men (24.4 ± 4.1) | 6 × 10 maximal voluntary eccentric hamstring contraction | 50% BF and semitendinosus | Pre and 72 h | Prone | As much of muscle as possible | Increased only in semitendinosus | |
| Hill et al. [56] |
36 women Control (23.3 ± 1.7) Eccentric BFR (21.7 ± 1.0) Concentric BFR (22.1 ± 1.7) |
1 × 30, 3 × 15 of forearm flexors at 40% of arterial occlusion and 30% of 1RM | Biceps brachii (66% of distance from medial acromion of the scapula to fossa cubit) | Pre, 0, 2, and 4 weeks | Supine | Nonspecific (noted that it was the same area used for muscle thickness) | No changes |
10 MHz at a gain of 58 dB and analyzed by ImageJ Used 1–255 |
| Matta et al. [40] |
13 women (21.6 ± 2) |
2 × 10 elbow flexions eccentric contractions | Brachialis | Pre, immediately, 24, 48, 72, and 96 h | Supine | 25 × 25 pixels | Increased 72 and 96 h | |
| Tsuchiya et al. [39] |
16 men Placebo (20.9 ± 0.4) EPA (21.9 ± 1.4) |
6 × 10 maximal eccentric contraction of elbow flexors from 90° to extension | Biceps—3 different placement (70°, 110°, 150°) 9 cm from the elbow joint | Pre, post, 1, 2, 5 days | N/A | Average 20 × 20 mm | Placebo: 110°: increased on days 2 and 5 and 150°: increased post, day 2 and 5 | Used 0–100 scale but graphs are to 250 |
| Biazon et al. [43] |
30 men (22 ± 3) |
Leg-extension 2/week |
VL | Pre, 5, and 10 weeks | Supine | N/A | Increased after 5 weeks and decreased after 10 weeks from 5 weeks | Scale was 0–256 |
| Cadore et al. [44] | 14 women and 8 men (22.9 ± 7.8 and 21.3 ± 3.3) | 4 × 20 knee extension/flexion (fatigue exercise protocol) | Mid-point of VL | Pre and 48 h | Supine | As much of muscle with a box b/w fat and bone | No change |
Scale was 0–255; No changes may be due to muscle group regarding muscle damage |
| Grazioli et al. [38] |
26 men (22.3 ± 3.2) |
1 × 15 20-m sprints (straight versus 2 changes in direction) | RF and BF | Pre, 0, 24, 48 ad 72 h | Supine | Tracing of as much of muscle as possible | No changes | Scale was 0–255 |
| Orssatto et al. [48] |
16 judo athletes (gender N/A) (23.1 ± 3.8) |
10 × 10 maximal bilateral countermovement jumps | 50% RF and VL | Pre, 24, and 48 h | Supine | 1 cm2 box | RF and VL increased after 24 and 48 h compared to pre but there are no differences b/w 24 and 48 h | Scale was 0–255 |
Measurement timepoints were measured based from exercise, thus 0 h indicates immediately after exercise. The increase of echo intensity indicates the increase in muscle damage
N/A not available, b/w between, RM repetition max, VL vastus lateralis, RF rectus femoris, BF biceps femoris, RT resistance training, BFR blood flow restriction
Studies investigating echo intensity 72 h following resistance exercise (typical time course of exercise-induced muscle damage) seem to provide some evidence that changes in echo intensity could be detecting edema and inflammation associated with exercise-induced muscle damage [3, 12, 28, 30, 31, 49–54, 68, 71]. However, echo intensity has been shown to be elevated up to 10 weeks following the initiation of a traditional resistance training program [34]. Of note, muscle strength increased throughout the study which contrasts with the idea that the muscle was damaged. Another study also observed changes in echo intensity following the initial 5 weeks of a 10-week resistance training program. After the first 5 weeks, echo intensity decreased towards baseline [43]. Although the elevation in the first 5 weeks seems to corroborate that this was a detection of exercise-induced muscle damage, there are a few points of consideration. First, the high load exercise condition consisted of three sets of 10 repetitions at 80% of the participant’s concentric one-repetition maximum on a single exercise (i.e. leg extension). Given that this was performed twice a week, it is worth considering whether this was actually damaging. Second, the other exercise group was completed with low loads in combination with blood flow restriction, which is not commonly associated with exercise-induced muscle damage [72]. Third, and perhaps most important, all groups (traditional high load, high load with blood flow restriction, and low load with blood flow restriction) increased strength throughout the study. This is seemingly unexpected from a muscle that is damaged [43]. For example, a damaged muscle is not expected to be stronger than an undamaged muscle. This suggests that the ability of echo intensity to inform changes in edema/muscle damage may need to be reconsidered but perhaps not disregarded.
Acute swelling
The change in echo intensity has also been used to provide insights into the balance between extracellular and intracellular fluid in studies investigating acute changes in cell swelling [4, 15, 18] (Table 3). For example, some have hypothesized that short-term changes in intracellular swelling are important, mechanistically, for long-term changes in muscle size [73, 74]. This index of acute swelling was traditionally determined based on acute changes in muscle thickness and the resultant change in plasma volume estimated from hematocrit [73, 75]. Given the idea that echo intensity relates to edema, changes in this variable were recently used as a non-invasive way to determine whether the acute change in muscle thickness was due to an intracellular shift or rather due to the fluid accumulation around the fibers [4, 15, 18]. Wong and colleagues found inconsistent results for changes in echo intensity when implementing unilateral bicep curls in combination with blood flow restriction [4]. In their first experiment, four sets of exercise produced no change in echo intensity, but the same protocol produced a decrease in their second experiment. Other studies have found no changes [4, 15] or instead increases [18] following exercise. Although limitations exist with using acute changes in muscle thickness as a marker of intracellular fluid shifts, the ability to use echo intensity as a marker of fluid location does not seem to provide additional insights. It is not known why the same exercise protocol produced consistent acute changes in muscle thickness but different results for changes in echo intensity [4].
Table 3.
Changes in echo intensity used as a marker of acute swelling
| References | Participants (age in years) | Exercise | Measurement site | Measurement time points | Posture of measurement | Region of interest | Results | Notes |
|---|---|---|---|---|---|---|---|---|
| Wong et al. [4] |
96 men and women (18–35) |
4 × failure unilateral biceps curls at 40% 1RM | 70% of arm | Pre and post | Supine | As much of muscle with a box b/w fat and bone | No change and decrease | There were 2 experiments with the same exercise protocol yielding different EI results |
| Yitzchaki et al. [15] |
49 men and women (23 ± 3) |
4 × failure unilateral biceps curls at 70% 1RM | 70% of arm | Pre and post | Standing | Tracing of muscle b/w fat and bone | No changes | Probe tilt controlled with liquid level |
| Muddle et al. [18] |
22 men (22.7 ± 3.5) |
Isometric contractions to fatigue at 30 or 70% 1RM | 66% of VL and 50% of RF | Pre and post | Supine | As much of the muscle | Increased collapse across muscle | VL EI > RF EI |
Acute swelling was used to quantify the pixel intensity of the ultrasound image. The grayscale of 0–255 using ImageJ was quantified as the lower the echo intensity, the more swelling (from fluids) in or around the muscle
N/A not available, b/w between, VL vastus lateralis, RF rectus femoris, EI echo intensity
Glycogen content
Skeletal muscle utilizes glycogen to produce energy in response to exercise. Typically, the invasive biopsy technique is needed to quantify changes in muscle glycogen. Although, recently challenged [17], it has been proposed that changes in echo intensity may be able to non-invasively determine changes in muscle glycogen [14, 16]. Instead of using the echo intensity grayscale (0–255) where 0 is dark and 255 is white, the software used to determine glycogen is from 0 to 100 and the scale is reversed. In other words, 0 indicates a white image and 100 indicates a black image. Although the scale is different, the technology is based on changes in echogenicity. Echo intensity is thought to detect changes in water content. Glycogen is hydrophilic, which means it attracts water. Thus, when muscle glycogen content is high, the ultrasound image is hypoechoic (black). Conversely, when the ultrasound image is whiter, the muscle glycogen content is low. The scale (0–100) was likely reversed so that a drop in muscle glycogen would correspond to a drop in the echo intensity score (i.e. whiter image). Using the traditional scale, this would have corresponded to an increase in echo intensity score (i.e. 0–255 scale, whiter image).
Early work suggested that changes in echo intensity might correspond to changes in muscle glycogen following exercise [14, 16] (Table 4). However, recent work has found changes in muscle glycogen but no change in echo intensity after exercise [17]. This finding led Routledge and colleagues [17] to conclude that there was no relationship between changes in echo intensity and changes in muscle glycogen as measured via biopsy. Other work would seem to corroborate this [4], where echo intensity was suggested to decrease (i.e. darker) following exercise previously shown to decrease muscle glycogen [76]. If changes in echo intensity correspond to changes in glycogen, then this would have to be interpreted as an increase in glycogen following acute exercise. Taken together, it seems unlikely that changes in echo intensity correspond to changes in muscle glycogen following exercise.
Table 4.
Changes in echo intensity used as a marker of glycogen content
| References | Participants (age in years) | Exercise | Measurement site | Measurement time points | Posture of measurement | Region of interest | Results | Notes |
|---|---|---|---|---|---|---|---|---|
| Hill and San Millán [16] | 22 men (31.3 ± 5.1) | 90 min cycling | Mid-point of VL | Pre and post | N/A | Nonspecific (avoided skin and tissues below RF or VL) | Decreased after exercise | Men contracted quads for imaging |
| Nieman et al. [14] | 20 men (18–55) | 75-km cycling | VL | Pre and post | N/A | Nonspecific (avoided skin and bone) | Decreased after exercise | Averaged out of 3 images |
| Routledge et al. [17] | 14 men (18.2 ± 0.8) | 80 min rugby match | 50% of VL via ultrasound | Pre and post | Supine | N/A | No changes | Biopsies indicated glycogen decreases (40–50%) |
MuscleSound (0–100) was used to quantify the pixel intensity of the ultrasound image. 0 indicates low glycogen as 100 indicated high glycogen
N/A not available, VL vastus lateralis, RF rectus femoris
Future research and considerations
Manipulation of single variables
Measurements incorporating echo intensity requires further research in order to determine what echo intensity is actually representing. The manipulation of different variables to see what impact that manipulation has on changes in echo intensity would be a preferred method to better address what changes in echo intensity represent physiologically. For example, Dankel et al. [77] manipulated the acute swelling response to observe whether echo intensity tracked with this manipulated collection of fluid. Manipulations of other variables can be done in a similar fashion to see what effect this may or may not have on changes in echo intensity.
Mechanical considerations
One consideration to make when assessing changes in echo intensity is the control for the probe tilt of the ultrasound transducer. Electrical levels with digital readers [4, 77, 78] and liquid levels [15] has been implemented in research evaluating the change of echo intensity. Although muscle size measurements have been observed to not be highly influenced by the ultrasound probe tilt (probe was tilted ranging within 6° perpendicular to the muscle), there are significant changes in echo intensity [78]. When looking at changes in echo intensity (the focus of this review), the tilt can be partially accounted for without a level by using a single tester. This is because it would be expected that the technique used at pre would be a similar technique used at post. Of course, a non-exercise time matched control group would also help give confidence to the results. Ultrasonography settings (particularly gain) can modify the intensity of the measurement (Fig. 2). Thus, these settings should also be noted in future literature to ensure that the same settings were used for all testing (especially at pre and post). If the gain is not all the way up or all the way down and is the same setting both at pre and post, the direction of change should be consistent. Importantly, although the direction of change will likely be the same across a range of settings, the magnitude of change will likely be different. Probe sites should also be considered, as measurements from different muscle regions might result in different responses [79]. However, with respect to the impact of exercise, the important question would be “do different regions of the muscle result in different changes?” rather than “does echo intensity differ along the length of the limb?”. It is also likely important to ensure that the skin is not being depressed by the probe. Using a generous amount of gel may help prevent this but may also in and of itself contribute to changes in echo intensity.
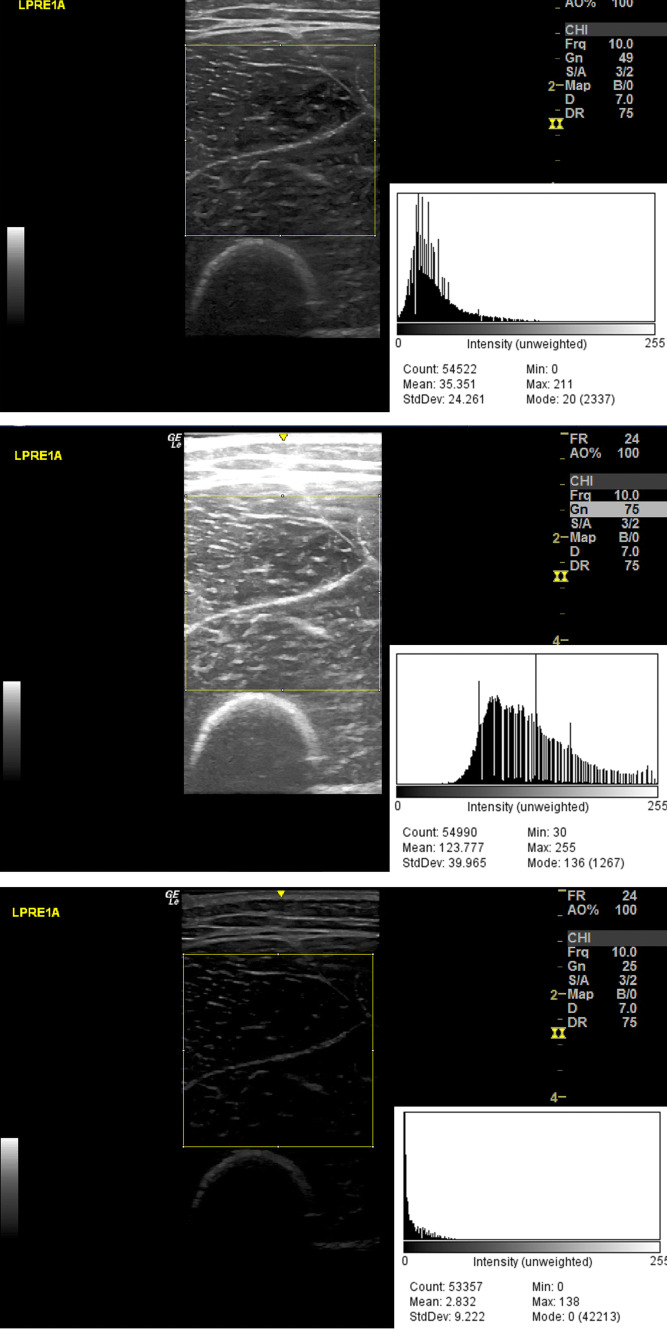
Fig. 2.
Comparisons of echo intensity using the same image but with different settings for gain. The top image represents an image with the gain at 49, which is commonly used in the previous literature. The histogram connected to this figure also provides the mean echo intensity as 35.35 AU. The middle figure represents the same image with the gain set at 75. The echo intensity is 123.77 AU with a higher gain setting. The bottom figure represents the same image with a low gain setting of 25. This brings the mean echo intensity down to 2.83 AU. The yellow box represents the region of interest
Physiological state after resistance exercise considerations
An acute swelling response has been evident after resistance exercise, especially when using blood flow restriction [4, 74]. It is possible that the state of the muscle immediately after exercise is different than the state of the muscle after a chronic training period. For example, the acute swelling response may produce differential effects depending on the muscles architecture. In a pennated muscle [80], the acute change in the orientation of fibers following exercise may have a greater impact on the ultrasound echo than a non-pennate muscle. In addition, the impact of muscle temperature may need to be considered. Muscle temperature has been shown to be elevated during and immediately after resistance exercise (around 2 °C) with a gradual reduction of temperature during the initial minutes following exercise [81]. Thus, if an ultrasound image of a muscle is to be taken immediately after exercise, it would be at a slightly higher temperature than before exercise. For example, all of the acute studies included in this review [4, 14–18] were measured when the muscle was likely at an elevated temperature. Nevertheless, one paper by Wong et al. [4] found differential responses to the same exercise bout. It is unlikely that temperature was elevated following one bout of exercise and not the other. Although muscle temperature is an interesting variable to consider with changes in echo intensity, it may not be able to explain the changes observed following exercise.
Reliability
The reliability of a measurement will ultimately determine the ability to determine a change in any given variable. With echo intensity, many studies report intra-class correlations [23, 24, 35] and some report correlation (r value) coefficients [14, 16]. However, both of these are highly influenced by the variance of echo intensity in the sample. Providing the standard deviation of the difference score (Test 2–Test 1) multiplied by 1.96 may provide a better indicator or reliability in the units to which they were measured. Others may choose to report a % coefficient of variation. The reliability of echo intensity appears to be relatively poor. For example, when echo intensity was measured twice within the span of a minute, the coefficient of variation was 3.3% for echo intensity and 0.7% for muscle thickness [77]. Therefore, it is important to understand that echo intensity can differ between two images taken within a minute in a scenario where the probe never left the surface of the skin. Once more, the use of a non-exercise time matched control condition (group) may be important to ensure that any change observed from the intervention exceeds that of random noise.
Conclusion
Echo intensity, quantified from the pixel intensity of an ultrasound image, is purported to represent several different physiological effects as noted in literature. However, in response to exercise, the change in echo intensity seems to respond in a multitude of different ways. For example, the increase in echo intensity could be interpreted as a decrease in muscle quality, an increase in edema/inflammation, and a decrease in muscle glycogen. A decrease in echo intensity, which is also observed, would indicate the exact opposite. It is conceivable that a change in echo intensity represents all of these purported physiologic effects at different time points. We recommend that these effects be determined experimentally to rule out what echo intensity might and might not represent. Until this is done, caution should be employed when interpreting changes in echo intensity as a main marker for physiological changes after acute and chronic exercise.
Compliance with ethical standards
Conflict of interest
The authors declare they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Yasuda T, Loenneke JP, Thiebaud RS, Abe T. Effects of blood flow restricted low-intensity concentric or eccentric training on muscle size and strength. PLoS ONE. 2012;7:e52843. doi: 10.1371/journal.pone.0052843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schedel H, Reimers CD, Nägele M, et al. Imaging techniques in myotonic dystrophy. A comparative study of ultrasound, computed tomography and magnetic resonance imaging of skeletal muscles. Eur J Radiol. 1992;15:230–238. doi: 10.1016/0720-048X(92)90113-N. [DOI] [PubMed] [Google Scholar]
- 3.Medeiros DM, Mantovani RF, Lima CS. Effects of low-intensity pulsed ultrasound on muscle thickness and echo intensity of the elbow flexors following exercise-induced muscle damage. Sport Sci Health. 2017;13:365–371. doi: 10.1007/s11332-017-0366-5. [DOI] [Google Scholar]
- 4.Wong V, Abe T, Chatakondi RN, et al. The influence of biological sex and cuff width on muscle swelling, echo intensity, and the fatigue response to blood flow restricted exercise. J Sports Sci. 2019;37:1865–1873. doi: 10.1080/02640414.2019.1599316. [DOI] [PubMed] [Google Scholar]
- 5.Franchi MV, Longo S, Mallinson J, et al. Muscle thickness correlates to muscle cross-sectional area in the assessment of strength training-induced hypertrophy. Scand J Med Sci Sports. 2018;28:846–853. doi: 10.1111/sms.12961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Loenneke JP, Dankel SJ, Bell ZW, et al. Ultrasound and MRI measured changes in muscle mass gives different estimates but similar conclusions: a Bayesian approach. Eur J Clin Nutr. 2019 doi: 10.1038/s41430-019-0431-z. [DOI] [PubMed] [Google Scholar]
- 7.Yoshiko A, Tomita A, Ando R, et al. Effects of 10-week walking and walking with home-based resistance training on muscle quality, muscle size, and physical functional tests in healthy older individuals. Eur Rev Aging Phys Act. 2018;15:13. doi: 10.1186/s11556-018-0201-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yoshiko A, Kaji T, Sugiyama H, et al. Twenty-four months’ resistance and endurance training improves muscle size and physical functions but not muscle quality in older adults requiring long-term care. J Nutr Health Aging. 2019;23:564–570. doi: 10.1007/s12603-019-1208-8. [DOI] [PubMed] [Google Scholar]
- 9.Blue MNM, Smith-Ryan AE, Trexler ET, Hirsch KR. The effects of high intensity interval training on muscle size and quality in overweight and obese adults. J Sci Med Sport. 2018;21:207–212. doi: 10.1016/j.jsams.2017.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.de Bassan N, Denadai BS, de Lima LCR, et al. Effects of resistance training on impulse above end-test torque and muscle fatigue. Exp Physiol. 2019;104:1115–1125. doi: 10.1113/EP087204. [DOI] [PubMed] [Google Scholar]
- 11.Varghese A, Bianchi S. Ultrasound of tibialis anterior muscle and tendon: anatomy, technique of examination, normal and pathologic appearance. J Ultrasound. 2014;17:113–123. doi: 10.1007/s40477-013-0060-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nosaka K, Clarkson PM. Changes in indicators of inflammation after eccentric exercise of the elbow flexors. Med Sci Sports Exerc. 1996;28:953–961. doi: 10.1097/00005768-199608000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Sipila S, Suominen H. Ultrasound imaging of the quadriceps muscle in elderly athletes and untrained men. Muscle Nerve. 1991;14:527–533. doi: 10.1002/mus.880140607. [DOI] [PubMed] [Google Scholar]
- 14.Nieman DC, Shanely RA, Zwetsloot KA, et al. Ultrasonic assessment of exercise-induced change in skeletal muscle glycogen content. BMC Sports Sci Med Rehabil. 2015;7:9. doi: 10.1186/s13102-015-0003-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yitzchaki N, Kuehne TE, Mouser JG, Buckner SL. Can changes in echo intensity be used to detect the presence of acute muscle swelling? Physiol Meas. 2019;40:045002. doi: 10.1088/1361-6579/ab122a. [DOI] [PubMed] [Google Scholar]
- 16.Hill J, San Millán I. Validation of musculoskeletal ultrasound to assess and quantify muscle glycogen content. A novel approach. Physician Sportsmed. 2014;42:45–52. doi: 10.3810/psm.2014.09.2075. [DOI] [PubMed] [Google Scholar]
- 17.Routledge HE, Bradley WJ, Shepherd SO, et al. Ultrasound does not detect acute changes in glycogen in vastus lateralis of man. Med Sci Sports Exerc. 2019 doi: 10.1249/MSS.0000000000002052. [DOI] [PubMed] [Google Scholar]
- 18.Muddle TWD, Magrini MA, Colquhoun RJ, et al. Impact of fatiguing, submaximal high-vs. low-torque isometric exercise on acute muscle swelling, and echo intensity in resistance-trained men. J Strength. 2019;33:1007–1019. doi: 10.1519/JSC.0000000000003033. [DOI] [PubMed] [Google Scholar]
- 19.Chen TC, Nosaka K. Responses of elbow flexors to two strenuous eccentric exercise bouts separated by three days. J Strength Cond Res. 2006;20:108. doi: 10.1519/R-16634.1. [DOI] [PubMed] [Google Scholar]
- 20.Cadore EL, González-Izal M, Pallarés JG, et al. Muscle conduction velocity, strength, neural activity, and morphological changes after eccentric and concentric training. Scand J Med Sci Sports. 2014;24:e343–e352. doi: 10.1111/sms.12186. [DOI] [PubMed] [Google Scholar]
- 21.Yamada M, Kimura Y, Ishiyama D, et al. Synergistic effect of bodyweight resistance exercise and protein supplementation on skeletal muscle in sarcopenic or dynapenic older adults. Geriatr Gerontol Int. 2019;19:429–437. doi: 10.1111/ggi.13643. [DOI] [PubMed] [Google Scholar]
- 22.Jajtner A, Hoffman J, Scanlon T, et al. Performance and muscle architecture comparisons between starters and nonstarters in National Collegiate Athletic Association Division I women’s soccer. J Strength Cond Res. 2013;27:2355–2365. doi: 10.1519/JSC.0b013e31829bd7c5. [DOI] [PubMed] [Google Scholar]
- 23.Radaelli R, Botton CE, Wilhelm EN, et al. Low- and high-volume strength training induces similar neuromuscular improvements in muscle quality in elderly women. Exp Gerontol. 2013;48:710–716. doi: 10.1016/j.exger.2013.04.003. [DOI] [PubMed] [Google Scholar]
- 24.Radaelli R, Botton CE, Wilhelm EN, et al. Time course of low- and high-volume strength training on neuromuscular adaptations and muscle quality in older women. Age. 2014;36:881–892. doi: 10.1007/s11357-013-9611-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mangine G, Redd MJ, Gonzalez AM, et al. Resistance training does not induce uniform adaptations to quadriceps muscles. Cold Spring Harbor. 2018 doi: 10.1101/325860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yoshiko A, Kaji T, Sugiyama H, et al. Effect of 12-month resistance and endurance training on quality, quantity, and function of skeletal muscle in older adults requiring long-term care. Exp Gerontol. 2017;98:230–237. doi: 10.1016/j.exger.2017.08.036. [DOI] [PubMed] [Google Scholar]
- 27.Santos R, Valamatos MJ, Mil-Homens P, Armada-da-Silva PAS. Muscle thickness and echo-intensity changes of the quadriceps femoris muscle during a strength training program. Radiography. 2018;24:e75–e84. doi: 10.1016/j.radi.2018.03.010. [DOI] [PubMed] [Google Scholar]
- 28.Chen TC, Chen H-L, Lin M-J, et al. Muscle damage responses of the elbow flexors to four maximal eccentric exercise bouts performed every 4 weeks. Eur J Appl Physiol. 2009;106:267–275. doi: 10.1007/s00421-009-1016-7. [DOI] [PubMed] [Google Scholar]
- 29.Chen T, Chen H-L, Lin M-J, et al. Potent protective effect conferred by four bouts of low-intensity eccentric exercise. Med Sci Sports Exerc. 2010;42:1004–1012. doi: 10.1249/MSS.0b013e3181c0a818. [DOI] [PubMed] [Google Scholar]
- 30.Chen TC, Lin K-Y, Chen H-L, et al. Comparison in eccentric exercise-induced muscle damage among four limb muscles. Eur J Appl Physiol. 2011;111:211–223. doi: 10.1007/s00421-010-1648-7. [DOI] [PubMed] [Google Scholar]
- 31.Radaelli R, Bottaro M, Wilhelm E, et al. Time course of strength and echo intensity recovery after resistance exercise in women. J Strength Cond Res. 2012;26:2577–2584. doi: 10.1519/JSC.0b013e31823dae96. [DOI] [PubMed] [Google Scholar]
- 32.Chen TC, Tseng W-C, Huang G-L, et al. Low-intensity eccentric contractions attenuate muscle damage induced by subsequent maximal eccentric exercise of the knee extensors in the elderly. Eur J Appl Physiol. 2013;113:1005–1015. doi: 10.1007/s00421-012-2517-3. [DOI] [PubMed] [Google Scholar]
- 33.Gonzalez-Izal M, Cadore EL, Izquierdo M. Muscle conduction velocity, surface electromyography variables, and echo intensity during concentric and eccentric fatigue. Muscle Nerve. 2014;49:389–397. doi: 10.1002/mus.23926. [DOI] [PubMed] [Google Scholar]
- 34.Damas F, Phillips SM, Lixandrão ME, et al. Early resistance training-induced increases in muscle cross-sectional area are concomitant with edema-induced muscle swelling. Eur J Appl Physiol. 2016;116:49–56. doi: 10.1007/s00421-015-3243-4. [DOI] [PubMed] [Google Scholar]
- 35.Jenkins NDM, Housh TJ, Buckner SL, et al. Neuromuscular adaptations after 2 and 4 weeks of 80% versus 30% 1 repetition maximum resistance training to failure. J Strength Cond Res. 2016;30:2174–2185. doi: 10.1519/JSC.0000000000001308. [DOI] [PubMed] [Google Scholar]
- 36.Fritsch CG, Dornelles MP, Severo-Silveira L, et al. Effects of low-level laser therapy applied before or after plyometric exercise on muscle damage markers: randomized, double-blind, placebo-controlled trial. Lasers Med Sci. 2016;31:1935–1942. doi: 10.1007/s10103-016-2072-y. [DOI] [PubMed] [Google Scholar]
- 37.Stock MS, Mota JA, DeFranco RN, et al. The time course of short-term hypertrophy in the absence of eccentric muscle damage. Eur J Appl Physiol. 2017;117:989–1004. doi: 10.1007/s00421-017-3587-z. [DOI] [PubMed] [Google Scholar]
- 38.Grazioli R, Lopez P, Machado CLF, et al. Moderate volume of sprint bouts does not induce muscle damage in well-trained athletes. J Bodyw Mov Ther. 2019 doi: 10.1016/j.jbmt.2019.05.019. [DOI] [PubMed] [Google Scholar]
- 39.Brusco CM, Blazevich AJ, Radaelli R, et al. The effects of flexibility training on exercise-induced muscle damage in young men with limited hamstrings flexibility. Scand J Med Sci Sports. 2018;28:1671–1680. doi: 10.1111/sms.13068. [DOI] [PubMed] [Google Scholar]
- 40.da Matta TT, de Pereira WCA, Radaelli R, et al. Texture analysis of ultrasound images is a sensitive method to follow-up muscle damage induced by eccentric exercise. Clin Physiol Funct Imaging. 2018;38:477–482. doi: 10.1111/cpf.12441. [DOI] [PubMed] [Google Scholar]
- 41.Matta TT, Pinto RO, Leitão BFM, Oliveira LF. Non-uniformity of elbow flexors damage induced by an eccentric protocol in untrained men. J Sports Sci Med. 2019;18:223–228. [PMC free article] [PubMed] [Google Scholar]
- 42.Tsuchiya Y, Yanagimoto K, Ueda H, Ochi E. Supplementation of eicosapentaenoic acid-rich fish oil attenuates muscle stiffness after eccentric contractions of human elbow flexors. J Int Soc Sports Nutr. 2019;16:19. doi: 10.1186/s12970-019-0283-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Biazon TMPC, Ugrinowitsch C, Soligon SD, et al. The association between muscle deoxygenation and muscle hypertrophy to blood flow restricted training performed at high and low loads. Front Physiol. 2019 doi: 10.3389/fphys.2019.00446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cadore EL, González-Izal M, Grazioli R, et al. Effects of concentric and eccentric strength training on fatigue induced by concentric and eccentric exercises. Int J Sports Physiol Perform. 2019;14:91–98. doi: 10.1123/ijspp.2018-0254. [DOI] [PubMed] [Google Scholar]
- 45.Botton CE, Umpierre D, Rech A, et al. Effects of resistance training on neuromuscular parameters in elderly with type 2 diabetes mellitus: a randomized clinical trial. Exp Gerontol. 2018;113:141–149. doi: 10.1016/j.exger.2018.10.001. [DOI] [PubMed] [Google Scholar]
- 46.Fukumoto Y, Tateuchi H, Ikezoe T, et al. Effects of high-velocity resistance training on muscle function, muscle properties, and physical performance in individuals with hip osteoarthritis: a randomized controlled trial. Clin Rehabil. 2014;28:48–58. doi: 10.1177/0269215513492161. [DOI] [PubMed] [Google Scholar]
- 47.Fukumoto Y, Ikezoe T, Yamada Y, et al. Skeletal muscle quality assessed from echo intensity is associated with muscle strength of middle-aged and elderly persons. Eur J Appl Physiol. 2012;112:1519–1525. doi: 10.1007/s00421-011-2099-5. [DOI] [PubMed] [Google Scholar]
- 48.da Orssatto LBR, Detanico D, Kons RL, et al. Photobiomodulation therapy does not attenuate fatigue and muscle damage in judo athletes: a randomized, triple-blind, placebo-controlled trial. Front Physiol. 2019 doi: 10.3389/fphys.2019.00811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chen T, Chen H-L, Lin M-J, et al. Contralateral repeated bout effect of eccentric exercise of the elbow flexors. Med Sci Sports Exerc. 2016;48:2030–2039. doi: 10.1249/MSS.0000000000000991. [DOI] [PubMed] [Google Scholar]
- 50.Lau WY, Blazevich AJ, Newton MJ, et al. Reduced muscle lengthening during eccentric contractions as a mechanism underpinning the repeated-bout effect. Am J Physiol Regul Integr Comp Physiol. 2015;308:R879–R886. doi: 10.1152/ajpregu.00338.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Nosaka K, Newton M, Sacco P, et al. Partial protection against muscle damage by eccentric actions at short muscle lengths. Med Sci Sports Exerc. 2005;37:746–753. doi: 10.1249/01.MSS.0000162691.66162.00. [DOI] [PubMed] [Google Scholar]
- 52.Nosaka K, Sakamoto K. Effect of elbow joint angle on the magnitude of muscle damage to the elbow flexors. Med Sci Sports Exerc. 2001;33:22. doi: 10.1097/00005768-200101000-00005. [DOI] [PubMed] [Google Scholar]
- 53.Radaelli R, Bottaro M, Wagner DR, et al. Men and women experience similar muscle damage after traditional resistance training protocol. IES. 2014;22:47–54. doi: 10.3233/IES-130519. [DOI] [Google Scholar]
- 54.Pereira MC, Bottaro M, Brown LE, et al. Do compression sleeves worn during exercise affect muscle recovery? Isokinet Exerc Sci. 2014;22:265–271. doi: 10.3233/IES-140537. [DOI] [Google Scholar]
- 55.Chen H-L, Nosaka K, Chen TC. Muscle damage protection by low-intensity eccentric contractions remains for 2 weeks but not 3 weeks. Eur J Appl Physiol. 2012;112:555–565. doi: 10.1007/s00421-011-1999-8. [DOI] [PubMed] [Google Scholar]
- 56.Hill EC, Housh TJ, Keller JL, et al. Early phase adaptations in muscle strength and hypertrophy as a result of low-intensity blood flow restriction resistance training. Eur J Appl Physiol. 2018;118:1831–1843. doi: 10.1007/s00421-018-3918-8. [DOI] [PubMed] [Google Scholar]
- 57.Rowe GS, Blazevich AJ, Haff GG. pQCT- and ultrasound-based muscle and fat estimate errors after resistance exercise. Med Sci Sports Exerc. 2019;51:1022–1031. doi: 10.1249/MSS.0000000000001873. [DOI] [PubMed] [Google Scholar]
- 58.Jenkins NDM, Miramonti AA, Hill EC, et al. Greater neural adaptations following high- vs. low-load resistance training. Front Physiol. 2017 doi: 10.3389/fphys.2017.00331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lynch NA, Metter EJ, Lindle RS, et al. Muscle quality. I. Age-associated differences between arm and leg muscle groups. J Appl Physiol. 1999;86:188–194. doi: 10.1152/jappl.1999.86.1.188. [DOI] [PubMed] [Google Scholar]
- 60.McGregor RA, Cameron-Smith D, Poppitt SD. It is not just muscle mass: a review of muscle quality, composition and metabolism during ageing as determinants of muscle function and mobility in later life. Longev Healthspan. 2014 doi: 10.1186/2046-2395-3-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Goodpaster BH, Carlson CL, Visser M, et al. Attenuation of skeletal muscle and strength in the elderly: the Health ABC Study. J Appl Physiol. 2001;90:2157–2165. doi: 10.1152/jappl.2001.90.6.2157. [DOI] [PubMed] [Google Scholar]
- 62.Heckmatt JZ, Leeman S, Dubowitz V. Ultrasound imaging in the diagnosis of muscle disease. J Pediatr. 1982;101:656–660. doi: 10.1016/S0022-3476(82)80286-2. [DOI] [PubMed] [Google Scholar]
- 63.Overend TJ, Cunningham DA, Paterson DH, Lefcoe MS. Thigh composition in young and elderly men determined by computed tomography. Clin Physiol. 1992;12:629–640. doi: 10.1111/j.1475-097X.1992.tb00366.x. [DOI] [PubMed] [Google Scholar]
- 64.Scanlon TC, Fragala MS, Stout JR, et al. Muscle architecture and strength: adaptations to short-term resistance training in older adults: muscle adaptations. Muscle Nerve. 2014;49:584–592. doi: 10.1002/mus.23969. [DOI] [PubMed] [Google Scholar]
- 65.Reimers K, Reimers CD, Wagner S, et al. Skeletal muscle sonography: a correlative study of echogenicity and morphology. J Ultrasound Med. 1993;12:73–77. doi: 10.7863/jum.1993.12.2.73. [DOI] [PubMed] [Google Scholar]
- 66.Spiegler AWJ, Schindler S, Herrmann FH. Becker muscular dystrophy: carrier detection by real-time ultrasound. J Neurol. 1985;232:307–309. doi: 10.1007/BF00313871. [DOI] [PubMed] [Google Scholar]
- 67.Pillen S, Tak RO, Zwarts MJ, et al. Skeletal muscle ultrasound: correlation between fibrous tissue and echo intensity. Ultrasound Med Biol. 2009;35:443–446. doi: 10.1016/j.ultrasmedbio.2008.09.016. [DOI] [PubMed] [Google Scholar]
- 68.Chen TC, Chen H-L, Lin M-J, et al. Effect of two maximal isometric contractions on eccentric exercise-induced muscle damage of the elbow flexors. Eur J Appl Physiol. 2013;113:1545–1554. doi: 10.1007/s00421-012-2581-8. [DOI] [PubMed] [Google Scholar]
- 69.Tseng K-W, Tseng W-C, Lin M-J, et al. Protective effect by maximal isometric contractions against maximal eccentric exercise-induced muscle damage of the knee extensors. Res Sports Med. 2016;24:228–241. doi: 10.1080/15438627.2016.1202826. [DOI] [PubMed] [Google Scholar]
- 70.Fujikake T, Hart R, Nosaka K. Changes in B-mode ultrasound echo intensity following injection of bupivacaine hydrochloride to rat hind limb muscles in relation to histologic changes. Ultrasound Med Biol. 2009;35:687–696. doi: 10.1016/j.ultrasmedbio.2008.10.008. [DOI] [PubMed] [Google Scholar]
- 71.Chen L, Nelson DR, Zhao Y, et al. Relationship between muscle mass and muscle strength, and the impact of comorbidities: a population-based, cross-sectional study of older adults in the United States. BMC Geriatr. 2013;13:74. doi: 10.1186/1471-2318-13-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Loenneke JP, Thiebaud RS, Abe T. Does blood flow restriction result in skeletal muscle damage? A critical review of available evidence. Scand J Med Sci Sports. 2014;24:e415–e422. doi: 10.1111/sms.12210. [DOI] [PubMed] [Google Scholar]
- 73.Loenneke JP, Fahs CA, Rossow LM, et al. The anabolic benefits of venous blood flow restriction training may be induced by muscle cell swelling. Med Hypotheses. 2012;78:151–154. doi: 10.1016/j.mehy.2011.10.014. [DOI] [PubMed] [Google Scholar]
- 74.Loenneke JP, Fahs CA, Thiebaud RS, et al. The acute muscle swelling effects of blood flow restriction. Acta Physiol Hung. 2012;99:400–410. doi: 10.1556/APhysiol.99.2012.4.4. [DOI] [PubMed] [Google Scholar]
- 75.Kim D, Loenneke JP, Ye X, et al. Low-load resistance training with low relative pressure produces muscular changes similar to high-load resistance training. Muscle Nerve. 2017;56:E126–E133. doi: 10.1002/mus.25626. [DOI] [PubMed] [Google Scholar]
- 76.Cumming KT, Paulsen G, Wernbom M, et al. Acute response and subcellular movement of HSP27, αB-crystallin and HSP70 in human skeletal muscle after blood-flow-restricted low-load resistance exercise. Acta Physiol. 2014;211:634–646. doi: 10.1111/apha.12305. [DOI] [PubMed] [Google Scholar]
- 77.Dankel SJ, Abe T, Spitz RW, et al. Impact of acute fluid retention on ultrasound echo intensity. J Clin Densitom. 2019 doi: 10.1016/j.jocd.2019.02.008. [DOI] [PubMed] [Google Scholar]
- 78.Dankel SJ, Abe T, Bell ZW, et al. The impact of ultrasound probe tilt on muscle thickness and echo-intensity: a cross-sectional study. J Clin Densitom. 2018 doi: 10.1016/j.jocd.2018.10.003. [DOI] [PubMed] [Google Scholar]
- 79.Rabello R, Fröhlich M, Bueno AF, et al. Echo intensity reliability between two rectus femoris probe sites. Ultrasound. 2019 doi: 10.1177/1742271X19853859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Martín-Hernández J, Marín P, Menéndez H, et al. Changes in muscle architecture induced by low load blood flow restricted training. Acta Physiol Hung. 2013 doi: 10.1556/APhysiol.100.2013.011. [DOI] [PubMed] [Google Scholar]
- 81.Kenny GP, Reardon FD, Zaleski W, et al. Muscle temperature transients before, during, and after exercise measured using an intramuscular multisensor probe. J Appl Physiol. 2003;94:2350–2357. doi: 10.1152/japplphysiol.01107.2002. [DOI] [PubMed] [Google Scholar]