Abstract
This review describes both magnitude and patterns of major behavioral risk factors for NCDs. Positive changes in tobacco use were identified, though this is far to meet the established expectation. Harmful alcohol consumption was reported, especially for males. Only small proportion of the population consumed an adequate amount of fruits and vegetables daily. Average salt intake was approximately doubled, in comparison to WHO’s recommendations. Physical activity has shifted gradually negatively, but future trends are unpredictable. An organized surveillance system should be developed initially with adequate tools and public resources to maintain and ensure sustainability over time.
Keywords: lifestyle, non-communicable diseases, risk factor, Vietnam
Introduction
Non-communicable diseases (NCDs) have been identified as a major health issue in the 21st century and cause an estimated 71% of all global deaths in 2016 (World Health Organization, 2018c). The rising burden of NCDs has been referred to as the accumulation of behavioral risk factors which negatively impact an individuals’ life span (World Health Organization, 2005). The combination of four major NCD behavioral risk factors: tobacco use, harmful consumption of alcoholic beverages, insufficient physical activity, and unhealthy diet were found to contribute to over 40% of all cancers and 80% of cardiovascular diseases (World Health Organization, 2005). Approximately 78% of global NCDs-caused deaths were found to be associated with low and middle income countries (LMICs) (World Health Organization, 2018c). LMICs are burdened with 85% of the global premature adult deaths worldwide, in which adults from these countries are at a double risk of death from NCDs as compared to adults in high-income countries (World Health Organization, 2018c). Like other LMICs, Vietnam has suffered from the rising burden of NCDs in the last 20 years. Specifically, during the period of 1986–2015, hospital admissions of patients with NCDs and their mortality rate have risen from 39% to 65.6%, and 41.8% to 73.4%, respectively (Vietnam Ministry of Health, 2017). It was estimated in 2016 that nearly one—in—five (17.4%) Vietnamese aged from 30 to 70 years of age, will suffer a premature death due to one of four common NCDs (cardiovascular diseases, cancer, chronic respiratory diseases, and diabetes) (World Health Organization, 2018c). However, most NCD patients are unable to receive treatment at an early stage of illness due to a lack of health awareness, in addition to inadequate coverage of preventive services (Nguyen et al., 2012b; Son et al., 2012).
In the early 2000s, the Vietnamese government recognized the widespread impact of NCDs and its profound influence on human health and economic development. Therefore, two phases of the National Program on NCDs Prevention & Control were implemented in 2002–2010 and 2010–2015, yet this program the program achieved minuscule success. This was due to the fragmented implementation of the program, in addition to the lack of both inter-sectoral coordination and direction for NCD prevention in Vietnam (Vietnam Ministry of Health, 2015). Hence, an updated National Strategy on Prevention and Control of NCDs for the period of 2015–2025 was developed in 2014. This focused primarily on communication activities, screening, early detection, treatment management, network development, and capacity enhancement (Vietnam Ministry of Health, 2015; Vietnam Ministry of Health and Health Partnership Group, 2015). Vietnamese Ministry of Health has conducted large household surveys in Vietnam, such as Vietnam Living Standard Surveys (VLSS), Multiple Indicator Cluster Surveys (MICS), Demographic and Health Surveys (DHS) on a regular basis since the early 1990s, but these surveys provide limited data on NCDs burden and risk factors. In the last 20 years, several studies which assess NCDs and associated risk factors have been carried out in response to the rising burden of NCDs. These include the STEPwise Survey on NCD Risk factors (STEPS), Global Adult Tobacco Use Surveys (GATS), and Global Youth Tobacco Use Surveys (GYTS) in addition to other national studies on hypertension, diabetes, obesity, and cancer (Nguyen and Hoang, 2018; Vietnam Ministry of Health, 2015). However, these surveys were carried out separately from one another and employed inconsistent methodology for data collection and analysis. This in turn has led to difficulties in the validation and comparison of findings across a variety of surveys.
Presently, we identified a number of literature reviews describing NCDs risk factors in Vietnam until the early 2010s. However, with regard to the rapid change in NCDs burden and the political and social context, there is a need for an updated comprehensive review. This is necessary to frame the overall landscape of NCDs and related behavioral risk factors in Vietnam to further inform the design of future research agenda. In this paper, we describe the magnitude and trends in major behavioral risk factors for NCDs which include smoking, alcohol use, physical inactivity, and unhealthy diet over the past decades in Vietnam.
Methods
Design
This is a narrative scoping literature review.
Review approach
This scoping review was adopted in alignment with a narrative synthesis approach. The scoping review follows the proposed methodology based on the JBI Framework of Evidence Synthesis (Khalil et al., 2016) which seeks to identify all relevant documents within a studied topic. Based on the main purpose of this narrative synthesis to describe patterns of most common behavioral risk factors, we specified relevant inclusion and exclusion criteria as well as specific information to be extracted from the identified materials. As there are no guidelines for designing a narrative scoping review, the process of reviewing and reporting was done in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) framework (Tricco et al., 2018) and suggested guidelines on systematic scoping reviews by Peters and colleagues (Peters et al., 2015).
Data source and search strategies
Given that the overall goal of this scoping review is to describe and analyze the most common behaviors attributed to the NCD burden in Vietnam, four common risk factors were included in this study: tobacco use, harmful use of alcoholic beverages, physical inactivity, and unhealthy diet. All population-based studies which provide data on at least one of the four main NCD-related behavioral risk factors were gathered and reviewed for information extraction. The search was performed from December 2019 to February 2020. Peer-reviewed articles published in English language were searched through online databases including PubMed, EMBASE, and the Cochrane Database of Systematic Reviews. Peer-reviewed articles in Vietnamese language were retrieved from Hanoi Medical Library, Hanoi University of Public Health Library, and other Vietnamese online journals. A variety of grey literature sources were gathered from the online portals of Vietnamese governmental agencies, WHO, international organizations, and non-governmental organizations working in the field of NCDs. The reference lists of the included studies were also screened and reviewed for additional eligible studies. The search strategy was developed by using keywords with the following combinations: “Vietnam” OR “Viet Nam” AND “non communicable diseases” OR “chronic diseases” OR “cancer” OR “cardiovascular diseases” OR “hypertension” OR “diabetes” OR “overweight” OR “COPD” AND “risk factors” OR “tobacco” OR “alcohol” OR “physical activity” OR “physical inactivity” OR “diet” OR “salt intake” OR “fruit intake” OR “vegetable intake” in the title/ abstract/ keywords. There was no set limit or range in chronological time to search for published documents, this was necessary to accurately capture patterns of health behaviors over time.
Inclusion and exclusion criteria
Eligible publications for the inclusion of this scoping review are studies or reports which were conducted on the Vietnamese population without pre-existing health conditions (pregnant, hypertension, overweight, etc.). Surveys conducted specifically on minority populations or conducted outside of Vietnam were excluded. The included materials must report statistics on at least one of major behavioral risk factors that is relevant to this study (smoking, alcohol use, physical activity, diet-related risk factors) as original research or literature reviews. Studies that were included must also report data from a national or subnational representative sample of the entire Vietnamese population or its findings are representative for the specific demographic settings (rural/urban). Studies with a small sample size (preferably to be at least 1000) or study findings which could not be generalized to a larger scale of population, were excluded following the recommendation of Hoy et al. (2013) and Nethan et al (2017). Since there is a lack of population-based research on dietary behaviors among the Vietnamese population, this study focuses on salt intake and the consumption of fruits and vegetables. Excess intake of salt and low consumption of fruits and vegetables represents dietary related risk factors which follow the NCD Global Monitoring Framework adopted by the UN General Assembly in 2012 (UN General Assembly, 2012).
Data processing, extraction, and synthesis
All articles/reports that were identified with the previously mentioned search terms were initially screened by title and abstract. Relevant literature was then assessed by thoroughly reading the full text. All data which was extracted from eligible literature and when possible, was stratified by age, sex, and geographical setting. The extracted information includes the article title, author list, year of publication, year of data collection, study design, sampling method, sample size, definitions of measured risk factors, main findings, and so forth. Further analysis and data validation of the extracted data was done with the application of a data extraction spreadsheet. Relevant findings were presented and interpreted for the modeling of a general framework to describe behavioral risk factors which could influence NCD burden and prevention strategies in Vietnam for the forthcoming future.
Results
Search results
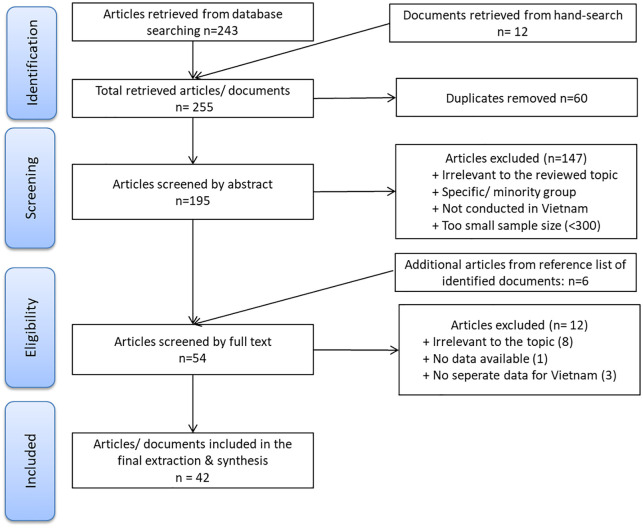
From the previously described search methodology, a total of 243 articles were procured from peer reviewed online databases (PubMed = 116; EMBASE = 118; Cochrane = 9). Additionally, we also identified 12 documents from the databases of World Health Organization (WHO), Vietnam Ministry of Health (MOH), National Institute of Nutrition (NIN) and General Statistics Office of Vietnam (GSO). Among the total retrieved articles of 255, 60 duplicate materials were identified and removed. After screening the abstracts of the identified literature, 48 articles or documents were found to have met the inclusion criteria; six additional articles were identified by reviewing the reference list of included documents. The full texts of 54 articles and documents were gathered and reviewed. In this final review, 12 articles were excluded for reasons such as: not providing data that was exclusive for Vietnam (three articles), irrelevant data sources for the reviewed topic (eight articles), and no data available (one article). A total of 42 articles and documents were included in the final synthesis and reported in this paper (See Figure 1).
Figure 1.
PRISMA flow chart of screening and reviewing process.
The majority of included studies reported data between the years 2001 to 2015. Four literature reviews were included, given their inclusion of explicit data prior to 2000 while the original reports or articles could not be acquired. Among the 42 included studies, 24 studies employed a national representative sampling frame and five used datasets from the Vietnam Health and Demographic Surveillance System (subnational sampling). Among the remaining studies, one article provided data with the community-based observational sample in Da Nang (sample size 1621), one article provided data from an urban setting in Ho Chi Minh City (HCM) (sample size 1488), and seven articles focused on lifestyle risk factors in adolescent populations.
The theme which emerged from the systematic review of research includes the major behavioral risk factors which contribute to NCDs, primarily these include tobacco-use, alcohol-use, physical activity, fruit and vegetable consumption, and salt intake. Tobacco usage was the most common risk factor reported, with results being reported in 22 studies, followed by physical activity (19 studies), alcohol use (17 studies), fruit and vegetable consumption (14 studies), and salt consumption (eight studies). In the presented review, substantive findings in each of these areas are summarized to characterize the patterns of these behavioral risk factors over time in Vietnam.
Tobacco use
As the leading cause of premature deaths in Vietnam, smoking behaviors have been studied in Vietnam since the early 1990s and is reported in 22 major studies. Among these, 11 studies have reported national representative results and four national surveys which include Vietnam Living Standards Survey (VLSS) 1992–93, 1997–98, Vietnam National Health Survey (VNHS) 2001–02, Vietnam National Surveys on NCD Risk Factors (STEPS) 2005, and Global Adults Tobacco Use (GATS) in both 2010 and 2015. The definition of smoking behavior was observed to be consistent across studies since 2005 with WHO’s definition in STEPS survey protocols (in which a current smoker is defined as individuals who used any type of tobacco products in the last 30 days). For data collected prior to 2005, the question “Do you currently smoke any tobacco products, such as cigarettes, cigars or pipes?” was mostly used to classify current smokers, former smokers, and those who never smoked.
In Vietnam, it has been observed that tobacco usage is the most common among men and tends to increase with age, especially from 25 years old and above (Hoy et al., 2013; Nguyen and Hoang, 2018; Nguyen et al., 2012b; Vietnam Ministry of Health, 2012; Vietnam Ministry of Health and Health Partnership Group, 2015; Vietnam Ministry of Health et al., 2010; Vietnam Ministry of Health et al., 2016). In 2015, it was estimated that the number of current smokers in Vietnam was 15.6 million or equal to 22.5% of the total population in that year (45.3% in men and 1.1% among women) (Vietnam Ministry of Health et al., 2016). Among current smokers, cigarettes were identified to be the most popular product for tobacco consumption and is used by approximately 80.6% of current smokers, though the use of electronic cigarettes has been observed to increase in recent years (Vietnam Ministry of Health et al., 2016). Noticeably, current smokers were found to additionally use traditional water pipes which accounted for approximately one third (29.3%) of the smoking population (Vietnam Ministry of Health et al., 2016) and ranks first among Asian countries (Jawad et al., 2018). It has been reported that a high proportion of both men and women report secondhand exposure to tobacco smoke at home and at work or public places (Minh An et al., 2013; Nguyen et al., 2013; Vietnam Ministry of Health and Health Partnership Group, 2015; Vietnam Ministry of Health et al., 2010; Vietnam Ministry of Health et al., 2016).
Tobacco use was extensively reported in men, conversely in women, and reflects a consistent pattern across both national and local surveys which use large sample cohorts (Cuong et al., 2007; Ly et al., 2013). The smoking prevalence in males has been shown to be in a downward trend for the last 40 years starting from 60.5% in 1992–1993 (General Statistics Office of Vietnam, 1998; Morrow and Barraclough, 2003), to 56.1% in 2001–2002 (Son et al., 2012; Vietnam Ministry of Health and Health Partnership Group, 2015), then 47.4% in 2010 (Vietnam Ministry of Health et al., 2010), and finally to 45.3% in 2015 (Vietnam Ministry of Health et al., 2016). Similarly, the smoking prevalence among women decreased throughout the years from 1.8% in 2001 (General Statistics Office of Vietnam, 2003; Morrow and Barraclough, 2003), to 1.4% in 2010 (Vietnam Ministry of Health et al., 2010), and finally to 1.1% in 2015 (Vietnam Ministry of Health et al., 2016). Throughout the time frame from 1992 to 2015, smoking prevalence for both sexes residing in rural areas was slightly higher than urban areas (Van Minh et al., 2017). Data on tobacco usage among adults in Vietnam from 1992 to 2015 is gathered in Table 1 using data from national surveys. It should be specifically noted that the sampling method employed in these surveys differs from the GATS protocol, in respect to the use of similar classifications and definitions.
Table 1.
Tobacco consumption among adults in Vietnam from 1992 to 2015.
| 1992–1993a | 1997–1998a | 2001b | 2005c,d | 2006a | 2010e | 2015e | |
|---|---|---|---|---|---|---|---|
| Smoking prevalence by sex | |||||||
| Male | 63.1% | 50.7% | 56.1% | 66.1%c | 49.2% | 47.4% | 45.3% |
| 58.8% (North) | |||||||
| 57.7% (HCM) | |||||||
| 67.8% (Mekong Delta) | |||||||
| Female | 4.7% | 3.5% | 1.8% | 1.7%c | 1.5% | 1.4% | 1.1% |
| 1.6% (North) | |||||||
| 1.6% (HCM) | |||||||
| 1.1% (Mekong Delta) | |||||||
| Smoking prevalence in urban areas | |||||||
| Male | 56.6 | 47.4 | 55.1 | N/A | 46.9 | 47.7 | 42.7 |
| Female | 2.7 | 1.9 | 1.4 | N/A | 1.2 | 1.0 | 0.7 |
| Smoking prevalence in rural areas | |||||||
| Male | 62.6 | 51.7 | 56.4 | N/A | 50.0 | 47.3 | 46.7 |
| Female | 4.6 | 3.6 | 2.0 | N/A | 1.6 | 1.7 | 1.3 |
| Daily consumption (number of cigarettes, among current smokers) | |||||||
| Male | 11.4 | 11.1 | N/A | N/A | N/A | 13.6 | 13.8 |
| Female | 9.9 | 9.5 | N/A | N/A | N/A | 10.9 | 10.5 |
Vietnam Living Standard Survey 1992/93; 1997/98; 2006: national household survey, 3-stage random stratified cluster sampling; aged 6 years and over. (General Statistics Office of Vietnam, 1993, 1998; Morrow and Barraclough, 2003).
Vietnam National Health Survey 2001: 3-stage cluster sampling; national household survey (General Statistics Office of Vietnam, 2003; Morrow and Barraclough, 2003; Nguyen et al., 2012b).
National Adult Overweight Survey 2005: 2-stage cluster sampling of adults aged 25–64 (Do et al., 2015; Hoang et al., 2007; Pham et al., 2009; Trinh et al., 2008, 2010; Van Minh et al., 2008).
Vietnam STEPS 2005 in 3 representative regions (North, South, Mekong Delta): multi-stage sampling with national representative sample of adults aged 25–64 (General Statistics Office of Vietnam, 2007).
Vietnam GATS 2010, 2015: national representative sampling aged 15+ (Vietnam Ministry of Health et al., 2010, 2016).
A result that should be highlighted is that tobacco use among adolescents was less likely to be reported, in comparison to adults in most studies during the early 2000s. Vietnam had first surveyed smoking behaviors among individuals aged 15–24 through National Survey Assessment of Vietnamese Youth (SAVY) in both 2003 and 2006 (Nguyen Thanh Liem et al., 2010). Additionally, there were three rounds of Global Youth Tobacco Use Surveys (GYTS) conducted in 2003, 2007, and 2014 which provided information on the overall pattern of smoking among youth under 15 years of age. In general, boys showed a higher smoking prevalence as compared to girls (Hanoi Medical University, 2013; Vietnam Ministry of Health, 2003, 2007; Vietnam Ministry of Health et al., 2014). The recent results from Vietnam Global School-based Student Health Survey 2013 found that 4.1% of students aged 13–17 smoked in the past 30 days (7.5% among boys and 1.2% among girls) (Hanoi Medical University, 2013). The number of adolescent smoking increased slightly from 3.7% (in 2003) (Vietnam Ministry of Health, 2003), to 3.8% (in 2007) (Vietnam Ministry of Health, 2007), and 4.0% (in 2014) (Vietnam Ministry of Health et al., 2014) throughout the three rounds of the Global Youth Tobacco Survey. Tobacco use among male adolescents was relatively low, this is in comparison to the next age group bracket, 15–24; these observations illustrate a significant transition in smoking behaviors, as individuals move from adolescence into young adulthood (Sirichotiratana et al., 2008; Vietnam Ministry of Health, 2003, 2007; Vietnam Ministry of Health et al., 2014, 2016). In 2003, the first round of SAVY (Nguyen Thanh Liem et al., 2010) provided illuminating evidence on the remarkable increase of smoking prevalence from 10% (ages 14–17) to 41% (ages 18–21) and up to 59% (ages 22–25). Similarly, the smoking prevalence of the youth population aged from 14–17, 18–21, 22–25 years old was 11%, 41%, and 47% respectively, in 2008 as observed in SAVY II (Nguyen Thanh Liem et al., 2010).
Alcohol consumption
The results from this review identified 17 materials which report on alcohol consumption in the Vietnamese population. Among identified documents, the results from four national surveys were reported within 10 different articles (Do et al., 2015; Hoy et al., 2013; Nguyen and Hoang, 2018; Trinh et al., 2008; Van Bui et al., 2016; Vietnam Ministry of Health, 2012, 2016; Vietnam Ministry of Health and Health Partnership Group, 2015; World Health Organization, 2014, 2018b) and four studies used regional sampling methods (Huu Bich et al., 2009; Ly et al., 2013; Pham et al., 2009; Trinh et al., 2010; Van Minh et al., 2008). Also, we found two studies with data describing youth alcohol use (aged 10–19, sample size = 1408) (Hanoi Medical University, 2013; Thoa et al., 2013). The analyzed documents have provided descriptive statistics on the percentage of current drinkers within the population, average amount of alcohol consumption, and a percentage which described the number of current drinkers engaged with hazardous or harmful binge drinking behaviors.
The average amount of alcohol consumption per capita demonstrates an increasing trend over time. The WHO’s 2014 Global Status Report on Alcohol has reported that the annual alcohol consumption in 2008–2010 (6.6 L per capita) was almost doubled, in comparison to the 2003–2005 figure (3.8 L per capita) (World Health Organization, 2014). Similarly, the 2018 Global Status Report on Alcohol estimated that the amount of pure alcohol consumption annually rose from 4.7 L in 2009–2011 to 8.3 L in 2015–2017, per capita (World Health Organization, 2018b). Generally, alcoholic beverages were more likely to be consumed by men than women through all surveyed periods (2009–2011: 8.2 L vs 1.3 L, respectively; 2015–2017: 14.5 L vs 2.5 L, respectively) (Vietnam Ministry of Health and Health Partnership Group, 2015; World Health Organization, 2018b). The percentage of current drinkers was found to be extraordinarily high among males (about 70%–80% from 2005–2015), in regard to the limited time period of the definition (“Did you drink at least once in the last 30 days/ 6 months/ 12 months?”) (Do et al., 2015; Pham et al., 2009; Van Bui et al., 2016; Vietnam Ministry of Health, 2012, 2016). Thoa et al. (2013) also found that the rate of adolescents who consumed alcohol among the ages 10–19 was approximately 16.5% (32.0% among boys and 10.6% among girls).
For current drinkers, the typical indicator for assessing the risk of alcohol use can be determined from the number of standard drinks consumed in any drinking occasion. In many countries, including Vietnam, one standard drink was defined as equivalent to 10 g of pure alcohol as followed by the WHO’s recommendation, but a wide variation of this definition was reported from eight grams (UK) to 20 g (Japan, Austria) (Kalinowski and Humphreys, 2016). The WHO has recommended that the hazardous level of drinking alcohol is if the average consumption reaches 4.0–5.9 standard drinks per occasion for males (2.0–3.9 drinks for women); the harmful level for the average consumption of alcoholic beverages is ⩾6 standard drinks per occasion (⩾4 drinks for women) (Vietnam Ministry of Health, 2012, 2016). Overall in Vietnam, the mean number of standard drinks consumed in any occasion was found to be 5.2 drinks (5.5 drinks among men and 2.7 drinks among women) (Vietnam Ministry of Health, 2016) following the most recent survey from 2015. From 2010 to 2015, the percentage of current drinkers who drank at hazardous or harmful levels was observed to have declined among men. There were about 16.2% of the male population drinks alcohol at hazardous levels in 2010, this proportion decreased to 5.9% in 2015 (Vietnam Ministry of Health, 2012, 2016). Likewise, the proportion of harmful use of alcohol (heavy episodic drinkers) among men reduced from 11% in 2010 to 5.9% in 2015 (Vietnam Ministry of Health, 2012, 2016). While the percentage of male drinkers who consume alcohol at both hazardous and harmful levels decreased over time, the proportion of heavy episodic drinkers among females was shown to have doubled from 2010 (0.9%) (Vietnam Ministry of Health, 2012) to 2015 (2.1%) (Vietnam Ministry of Health, 2012).
Excessive alcohol consumption is noted to be one of the most common and deadly patterns of alcohol consumption (Esser et al., 2014; Sacks et al., 2015; Stahre et al., 2014). This was reported in seven studies which were included in this scoping review as binge drinking or at-risk drinking reported among current drinkers. However, the definition of excessive drinking varies largely between studies (See Table 2 for detailed information). Findings from STEPS 2010 uses the cut-off point at ⩾5 drinks per drinking occasion (⩾4 for women); additionally, this study shows that one fourth of current male drinkers have reported binge drinking, while binge drinking only occurs in less than 1% of female drinkers (Vietnam Ministry of Health, 2012). A survey on diabetes and its risk factors from 2008 to 2009 in two Northern provinces of Vietnam uses the cut-off point of ⩾3 drinks per occasion (2 for women) and reports 24.1% men and 1.1% women have at-risk drinking behaviors (Nguyen et al., 2012a).
Table 2.
Alcohol consumption among adults in Vietnam.
| Indicator | Time | Both sexes | Male | Female | Definition | Sources |
|---|---|---|---|---|---|---|
| % of Current drinkers | 2005 | N/A | 40.2% | 3.5% | In last 6 months | National Adult Overweight Survey 2005 (Do et al., 2015) |
| 2010 | 37.0% | 69.6% | 5.6% | In last 30 days | STEPS 2010 (Vietnam Ministry of Health, 2012) | |
| 2015 | 43.8% | 77.3% | 11.1% | In last 30 days | STEP 2015 (Vietnam Ministry of Health, 2012) | |
| 2005 | N/A | 80.9% | 9.3% | In last 12 months | STEPS 2005 (Mekong Delta) (Pham et al., 2009) | |
| 2010 | 47.4% | 84.3% | 11.8% | In last 12 months | STEPS 2010 (Vietnam Ministry of Health, 2012) | |
| 2015 | 42.6% | 79.2% | 11.1% | In last 12 months | STEPS 2015 (Van Bui et al., 2016; Vietnam Ministry of Health, 2016) | |
| Amount of alcohol consumed (liters) | 2002 | 6.8 | N/A | N/A | Amount of pure alcohol consumed per month (liter) *12 months | VLSS 2001/02 (General Statistics Office of Vietnam, 2003) |
| 2003–2005 | 3.8 | N/A | N/A | Amount of pure alcohol consumed in 1 year (liter) (adjusted for tourist consumption) | Global report on alcohol and health 2014 (Vietnam Ministry of Health and Health Partnership Group, 2015; World Health Organization, 2014) | |
| 2009–2011 | 4.7 | 8.2 | 1.3 | Amount of pure alcohol consumed in 1 year (liter) (adjusted for tourist consumption) | Global report on alcohol and health 2018 (World Health Organization, 2018b) | |
| 2015–2017 | 8.3 | 14.5 | 2.5 | Amount of pure alcohol consumed in 1 year (liter) (adjusted for tourist consumption) | Global report on alcohol and health 2018 (World Health Organization, 2018b) | |
| % Drinkers with intermediate (hazardous) level of drink | 2010 | 8.8% | 16.2% | 2.4% | 4–5.9 drinks/ occasion (2–3.9 for women) | STEPS 2010 (Van Bui et al., 2016; Vietnam Ministry of Health, 2012) |
| 2015 | 5.3% | 5.9% | 1.3% | 4–5.9 drinks/ occasion (2–3.9 for women) | STEPS 2015 (Vietnam Ministry of Health, 2016) | |
| % Drinkers with high-end/ Harmful level of drink | 2010 | 11.0% | 22.8% | 0.9% | ⩾6 drinks/ occasion (⩾4 for women) | STEPS 2010 (Van Bui et al., 2016; Vietnam Ministry of Health, 2016) |
| 2015 | 5.5% | 5.9% | 2.1% | ⩾6 drinks/ (⩾4 for women) | STEPS 2015 (Vietnam Ministry of Health, 2016) | |
| Excessive drink (binge drink/ at-risk drink) | 2005 | N/A | 38.6% | 0.4% | ⩾5 drinks in any drinking day, both sexes | STEPS 2005 (Mekong Delta) (Pham et al., 2009) |
| 2005 | N/A | 31.0% | 0.4% | ⩾5 drinks in any drinking day; (⩾4 for women) - Filabavi, rural | STEPS 2005 (North Vietnam) (Hoy et al., 2013; Huu Bich et al., 2009) | |
| 2005 | N/A | 17.0% | 0.3% | >5 drinks in any drinking day; (⩾4 for women) - Chililab, rural | STEPS 2005 (North Vietnam) (Hoy et al., 2013; Huu Bich et al., 2009) | |
| 2005 | 32.1% | 60.9% | 5.0% | ⩾3 drinks/ occasion (⩾2 for women) | STEPS 2005 (North Vietnam) (Van Minh et al., 2008) | |
| 2009 | N/A | 24.1% | 1.1% | ⩾3 drinks/ occasion (⩾2 for women) | National survey on diabetes & risk factors 2008–09 (Nguyen et al., 2012a) | |
| 2010 | 12.7% | 25.1% | 0.6% | ⩾5 drinks/ occasion (⩾4 for women) | STEPS 2010 (Van Bui et al., 2016; Vietnam Ministry of Health, 2012) |
One standard drink defined as one unit of alcoholic beverage equivalent to 10 g of pure alcohol.
Physical Inactivity
Since 2005, physical activity was included in most national surveys of NCDs and its associated risk factors, such as the National Adult Overweight Survey 2005, National survey on Diabetes and its risk factors 2008–2009, and Vietnam STEPS 2005, 2010, and 2015. The Global Physical Activity Questionnaire (GPAQ) developed by WHO is the most common tool for physical activity surveillance. The total time spent and the intensity of physical activity during a typical week were used as metrics to calculate the total number of MET-minutes per week, in which one MET is defined as 1 kcal/kg/hour and equivalent to the level of energy spent during sitting quietly (Vietnam Ministry of Health, 2016). The cut-off points for the determination of physical activity have been established at <600 MET-min/week (low), 600–2999 MET-min/week (moderate), and ⩾ 3000 MET-min/week (high); this can then be applied to classify the percent of a population that does not meet the WHO recommendations for physical activity (Vietnam Ministry of Health, 2012, 2016).
About one third of the Vietnamese population is physically inactive. The total time that one spent for physical activities was found to be higher in rural areas (Bui et al., 2015; Thu Hien et al., 2013; Vietnam Ministry of Health, 2012, 2016) and largely came from work-related activities (Bui et al., 2015; Vietnam Ministry of Health, 2012, 2016). Hien and colleagues reported that approximately 31.5% of the urban population has a high level of physical activity in comparison to 40.8% of population in rural areas (Thu Hien et al., 2013). Table 3 illustrates the level of physical activity among the adult population by sex. The most recent data from 2015 shows that about 30.4% of Vietnamese population does not meet the WHO recommendations (defined as less than 150 minutes of moderate to intense physical activity per week or equivalent <600 MET-min/week) (25.6% among men; 38.6% among women) (Vietnam Ministry of Health, 2016). The results were consistent with previous national studies (Ahmed et al., 2009; Do et al., 2015; Hoy et al., 2013; Ng et al., 2009; Nguyen et al., 2012a; Pham et al., 2009; Van Bui et al., 2016; Vietnam Ministry of Health, 2012) as well as other local studies (Hoy et al., 2013; Nguyen et al., 2012a; Thu Hien et al., 2013). The average time spent on physical activity per day tends to be higher among men (221.0 MET-min/day), in comparison to women (162.9 MET-min/day) in 2015 (Vietnam Ministry of Health, 2016). The unweighted data from STEPS 2010 showed a similar pattern of physical activity by sex with the median time of physical activity among men at 171.4 MET-min/day, in comparison to 115.7 MET-min/day among women (Vietnam Ministry of Health, 2012).
Table 3.
Level of physical activity by sex in Vietnam from 2005 to 2015.
| Year | Age range | Men | Women | Sources | ||||
|---|---|---|---|---|---|---|---|---|
| Low | Moderate | High | Low | Moderate | High | |||
| 2005 | 25–64 | 10.9% | 9.5% | 79.6% | 7.9% | 8.8% | 83.3% | National Adult Overweight Survey 2005 (Do et al., 2015) |
| 2005 | 25–64 | 32.7% | 16.7% | 50.6% | 40.4% | 24.2% | 35.4% | STEPS2005 – Mekong Delta region* (Pham et al., 2009) |
| 2005 | 25–64 | 46.5% | 17.9% | 35.6% | 41.2% | 28.5% | 30.3% | STEPS2005 - Ho Chi Minh City (Trinh et al., 2008) |
| 2005 | 25–64 | 10.9% | 9.5% | 79.6% | 7.9% | 8.8% | 83.3% | STEPS2005 – North Vietnam (Filabavi & Chililab) (Ahmed et al., 2009; Ng et al., 2009) |
| 2009 | ⩾25 | N/A | N/A | 13.7% | N/A | N/A | 11.5% | Survey on diabetes and its risk factors from 2008 to 2009* (Nguyen et al., 2012a) |
| 2010 | 25–64 | 26.4% | 20.8% | 52.0% | 31.1% | 27.8% | 41.1% | Vietnam STEPS 2010 (Nguyen and Hoang, 2018; Van Bui et al., 2016; Vietnam Ministry of Health, 2012; Vietnam Ministry of Health and Health Partnership Group, 2015) |
| 2015 | 18–69 | 25.6% | 15.8% | 58.6% | 38.6% | 23.6% | 37.9% | Vietnam STEPS 2015 (Nguyen and Hoang, 2018; Vietnam Ministry of Health, 2016) |
All results were calculated by using Global Physical Activity Questionnaire, except for the STEPS survey 2005 in Mekong Delta region and the National Survey on Diabetes and its risk factors 2008–2009 using self-reported data.
Among the population under 18 years old, physical activity was found to have a similar pattern by sex and tends to decrease with adolescence (Trang et al., 2009, 2012a, 2012b). A 5-year longitudinal cohort in Ho Chi Minh City (Trang et al., 2009, 2012a, 2012b), which employed both an accelerometer and the Adolescent Physical Activity Recall Questionnaire, found that that total time spent on physical activity decreased significantly in a 5-year period from 87 to 50 minutes per day (Trang et al., 2012a). In general, it was observed that boys tend to be more physically active than girls, in which approximately 16.7% of boys were shown to be physically inactive in comparison to 31.8% of girls (Trang et al., 2012b).
Unhealthy diet
In Vietnam, nutritional status and national strategy programs in 1996–2000 focused on the mitigation of malnutrition, micronutrient deficiency, poverty, and hunger. Hence, assessing healthy dietary behaviors in relation to NCDs was not discussed by Vietnamese regulatory bodies until 2002, with the development of the first National Strategy on NCD Prevention and Control. According to the NCD Global Monitoring Framework, there are at least three dietary risk behaviors which should be evaluated and managed at a population level for WHO Member States including: (1) fruit and vegetable consumption, (2) salt or sodium consumption, and (3) fat intake (especially saturated fat) (UN General Assembly, 2012). In regards to the lack of documented information on fat intake (only one available study (National Institute of Nutrition, 2012), our review summarizes findings on both fruit and vegetable consumption, and salt intake, while other dietary risk factors can be found in the discussion section below.
Low fruit and vegetable consumption
Data on fruit and vegetable consumption was first reported in the National Nutrition Survey in 1985 and later in the National Survey for NCDs, such as cardiovascular diseases or diabetes. In the National Nutrition Surveys, the consumption of fruit and vegetables was previously reported as the daily amount of fruit and vegetables consumed in kilogram or in percentage of total daily calories (Khue, 2015; National Institute of Nutrition, 2010; Vietnam Ministry of Health and Health Partnership Group, 2015). From 1985 to 2000, the consumption of fruits and vegetables did not change much in terms of proportion (fluctuating at about 5% of total daily energy intake) (Khue, 2015; Vietnam Ministry of Health and Health Partnership Group, 2015). From 2005, with the promotion of NCD burden and the variety of dietary risk factors associated with it, a significant shift in dietary habits have been recorded (Khue, 2015; Nguyen and Hoang, 2018). The percentage of the population reporting a low daily consumption of fruits and vegetables (less than 5 servings of fruits and vegetables per day), decreased in both males and females over time (See detailed information in Table 4). Low consumption of both fruits and vegetables was reported in approximately 87.0% of the male population in 2005 (Ahmed et al., 2009; Hoy et al., 2013; Kanungsukkasem et al., 2009), dropped to 80.2% in 2010 (Bui et al., 2016; Van Bui et al., 2016; Vietnam Ministry of Health, 2012), and was observed to be 63.1% in 2015 (Nguyen et al., 2020; Vietnam Ministry of Health, 2016). Otherwise, among women, the low consumption of fruit and vegetables was found to be 87.5%, 80.6% and 51.4% in 2005, 2010, and 2015, respectively (Bui et al., 2016; Hoy et al., 2013; Kanungsukkasem et al., 2009; Nguyen et al., 2020; Van Bui et al., 2016; Vietnam Ministry of Health, 2012, 2016). Overall, there is a rising trend in average quantity of fruits and vegetables consumed daily overtime in both sexes. In 2005, the Health and Demographic Surveillance System (HDSS) in Vietnam estimated that the number of fruits and vegetable servings per day ranged from 2.3 to 2.7 servings per day in the suburban areas of North Vietnam (Ahmed et al., 2009; Hoy et al., 2013; Kanungsukkasem et al., 2009). These figures rose to 3.2 servings per day for both sexes in 2010 (Vietnam Ministry of Health, 2012) and reached 5.1 servings per day in 2015 (4.7 in men and 5.5 in women) (Vietnam Ministry of Health, 2012).
Table 4.
Fruit and vegetable consumption in Vietnam from 2005 to 2010.
| Time | Low consumption of fruit/vegetables (<5 servings/day) | Number of fruit/vegetables servings/day | Sources | ||
|---|---|---|---|---|---|
| Men | Women | Men | Women | ||
| 2005 | 87.0% | 87.5% | 2.6 | 2.7 | STEPS2005 (Filabavi) (Ahmed et al., 2009; Hoy et al., 2013; Kanungsukkasem et al., 2009) |
| 2005 | 63.5% | 57.5% | 2.3 | 2.4 | STEPS2005 (Chililab) (Ahmed et al., 2009; Hoy et al., 2013; Kanungsukkasem et al., 2009) |
| 2005 | 30.2% | 26.5% | N/A | N/A | STEPS2005 (Mekong Delta region) (Hoy et al., 2013; Pham et al., 2009) |
| 2009 | 44.3% | 38.1% | N/A | N/A | National survey on diabetes and its risk factors 2008–09 (Hoy et al., 2013; Nguyen et al., 2012a) |
| 2010 | 80.2% | 80.6% | 3.2 | 3.2 | STEPS 2010 (Bui et al., 2016; Hoy et al., 2013; Van Bui et al., 2016) |
| 2015 | 63.1% | 51.4% | 4.7 | 5.5 | STEPS 2015 (Nguyen et al., 2020; Vietnam Ministry of Health, 2016) |
Salt consumption
Only eight studies included in this scoping review mentioned salt intake for the Vietnamese population among the 42 identified documents. Since the measurement of salt intake requires urine samples, only two studies had empirical data enabling the calculation of salt consumption from a 24-hour urinary sodium excretion (Jensen et al., 2018; Vietnam Ministry of Health, 2016). The method for this technique is described elsewhere (Jensen et al., 2018). Findings from a dataset acquired from STEPS 2010 exhibited that the average consumption of salt within the Vietnamese population was approximately 9.9 g of salt per person per day (10.2 g in men and 9.5 g in women) (Jensen et al., 2018). In 2015, the average salt consumption was 9.4g per person per day (10.5 g in men and 8.3 g in women) which was not significantly different than the 2010 figure (Vietnam Ministry of Health, 2016; World Health Organization, 2018c). Prior to 2010, the amount of salt intake was much higher and found to be approximately 18–22 g per person per day as reported by National Institute of Nutrition in 2007 (Nguyen and Hoang, 2018; Vietnam Ministry of Health and Health Partnership Group, 2015; Vietnam National Institute of Nutrition, 2007). Other studies reported the at-risk salt consumption by asking the question: “always/ often/ preferred daily food containing more salts” (Nguyen and Hoang, 2018; Nguyen et al., 2012a, 2020; Vietnam Ministry of Health, 2012, 2016). About one-third of the population reported to have included salt additives as part of their dietary habits in 2009 (men 32.2%, 27.1% women) (Nguyen et al., 2012a), while the figure in 2015 was about 22.2% overall (men 22.3%, women 22.2%) (Nguyen et al., 2020; Vietnam Ministry of Health, 2016).
Discussion
Tobacco use
Our scoping review identified that the pattern of tobacco usage in Vietnam has been well documented by numerous studies throughout the last few decades. In 2015, Vietnam was noted to be one of the top 25 countries in the world with highest smoking prevalence worldwide with a disproportionate pattern of tobacco consumption by sex, skewed on males (World Health Organization, 2015). The high-profile of smoking in the Vietnamese male population (nearly 50%) is understandable, given that smoking remains socially acceptable for men in Vietnamese culture. In contrast, tobacco usage among women is approximately 2% over the reviewed time frame and is expected to remain stable at this level in the future. This pattern was similar to other neighboring countries such as Thailand (Ministry of Health of Thailand, 2012) or Malaysia (Ministry of Health of Malaysia, 2012), but the smoking prevalence remains lower than the reported data from both China (Ministry of Health of China, 2011) and Indonesia (Ministry of Health of Indonesia, 2012). On the other hand, there has been an observed significant increase in tobacco use from adolescents under 15 years of age into young adulthood aged 15–24 years old (12.6% overall, 24.3% in boys); generally the smoking initiation age of Vietnamese begins at around 18–19 years of age (Vietnam Ministry of Health et al., 2016). Hence, this fact implies a priority toward young populations on the national tobacco control plan in Vietnam.
Several studies have also suggested that special attention should be paid to higher figures of tobacco use which is reported among disadvantaged Vietnamese groups, such as individuals living in a rural area, having a low level of education, or having lower quantile of income (Morrow and Barraclough, 2003; Nguyen et al., 2012b; Van Minh et al., 2017). Data reflect two crucial pieces of information: the first being that social and demographic factors play key roles in smoking prevalence and the second, that the lack of interventions which target these groups or prior interventions may need to be tailor-made to fit such groups. Another worthy point in the pattern of tobacco use, is the common use of traditional water-pipes for smoking tobacco (“thuốc lào”) in rural areas and the rising number of smokers who use electronic cigarettes, especially among younger individuals. A common usage of such traditional water-pipes in rural Vietnam is likely due to misperception of low risks of health problems. Therefore, this ought to be one area for designing prevention plans for people in a rural setting. Unfortunately, such patterns are not frequently mentioned or detailed among reviewed materials, but previous studies have noted that there is a necessity to appropriately monitor and evaluate the harmful effects of thuốc lào on smoking populations (Korfei, 2018; Saleheen et al.).
Observations in several studies have noted that the pattern of tobacco use in Vietnam and its transition, this has been greatly modified by social norms and the changing awareness of Vietnamese people (Jawad et al., 2018; Minh An et al., 2013; Morrow and Barraclough, 2003). Undoubtedly, tobacco control in Vietnam has made certain achievements which are highly recognized by international agencies. Synchronous efforts of putting tobacco use into the national policy agenda for over 20 years and the implementation of MPOWER package could have explained this change. Over the last 20 years, the consumption of tobacco has shown a downward trend, but the reduction of its use has not yet been met as expected, especially in rural areas. This fact should be important information to decision-makers with consideration to the nature of tobacco use in many countries (Giovino, 2002; Institute of Medicine, 2007). An analysis of smoking indicators from the WHO Comprehensive Information Systems for Tobacco Control estimated that the age–standardized prevalence of current smoking among males in the Western Pacific region would decrease by merely 1% by 2025 (Bilano et al., 2015). As a result, more adequate action plans on tobacco control should be developed and implemented to increase compliance of the MPOWER package to maintain both the current achievement on changing awareness and behavior of community toward tobacco use.
Alcohol consumption
Vietnam was not identified as one of the world’s top countries with a high consumption of alcohol; however, the increasing tendency presented in Table 2 has illustrated the opposite tendency in comparison with the situation of alcohol consumption in European countries. The rising tendency of alcohol consumption in Vietnam is in line with the increase of per capita alcohol consumption by 34% in Southeast Asian region between 2010 and 2017 (Manthey et al., 2019). In contrast, European countries which once had the world’s heaviest alcohol consumption has shown a significant decrease in harmful alcohol use due to the effective implementation of long-period alcohol policies (Manthey et al., 2019). The most recent data on alcohol consumption in Vietnam was reported to be 8.3 L per person per year (World Health Organization, 2018b), is higher than the figure in the Western Pacific region at 7.3 L, and the global average consumption at 6.4 L per person per year (World Health Organization, 2018b). This figure was higher for the actual consumption of current drinkers in Vietnam (22.8 L overall; 29.1 L in males and 10.4 L in females) (World Health Organization, 2018b). These findings are equivalent to the daily consumption of 63.8 g of pure alcohol among male drinkers and 22.8 g of pure alcohol in female drinkers. Another issue of alcohol consumption in Vietnam’s context is the use of unrecorded or home-made alcoholic beverages, which seemed to be increasing in quantity and difficult to measure (Lachenmeier et al., 2009).
The most dominant risk behavior of alcohol consumption was reported to be binge drinking, especially among young people (Archie et al.; Hermens et al.; US Department of Health and Human Services, 2009). In Vietnam, from 2005 to 2015, the prevalence of binge drinking was reported to be approximately one-fourth of the male population and less than 1% among females. Though the National Institute on Alcohol Abuse and Alcoholism recommended measuring alcohol consumption from 2004 (National Institute of Alcohol Abuse and Alcoholism, 2004), binge drinking was not reported in many studies. The exception is the STEPS surveys which suggested the inclusion of this indicator for future research in regards to NCDs. Prior to 2020, Vietnam had already imposed a number of policies for controlling the harmful use of alcohol (excise tax, drinking, and driving enforcement, mandatory business license to sell alcohol, and regulations on both advertising and sales in specific locations) but the implementation and the compliance to such regulations were determined to be poor (Giang et al., 2013). This may reflect not only a lack of stronger and strictly imposed control policies, but also that the monitoring of these policies is not well implemented. The enactment of Law on Prevention and Control of Harmful effects of Alcoholic beverages in 2020 is therefore expected to bring substantial changes in the drinking behavior of the entire Vietnamese population.
Physical activity
The Vietnamese adult population is slightly more physically active than the world population for both sexes. The percent of insufficient physical activities for the national population is at 19.9% among males and 30.6% among females; in comparison with worldwide statistics physical activity is approximately 23.4% in males and 31.7% in females (World Health Organization, 2018a). However, the physical activity in Vietnam’s population is low as compared to the average level of the Western Pacific region in which 18.8% males and 18.5% females were reported to have a low level of physical activity (World Health Organization, 2018a), but reported to be similar with other developing countries in Asia and Africa (Bui et al., 2015). This difference was assumed to be caused by the diversity of cultures, religions, and patterns of agricultural activities between countries (Bui et al., 2015). We identified a pattern of physical activity among adolescents in which Vietnamese youth between 11 and 17 years of age had a low level of physical activity (86.4%), which was higher than both the global prevalence (81.1%) and Western Pacific Region’s figure (85.8%). It was highlighted that the prevalence of insufficient physical activity was approximately three to four times higher among adolescents than in the adult population. Previous studies have explained that this pattern may be due to the change of adolescent social roles (moving out of family, school/work environment, etc.) and the establishment of good lifestyle behaviors in adolescence and youth adulthood (Bell and Lee, 2005; Corder et al., 2019; Nelson et al., 2008). Given the overall understanding of physical activity in community, more considerations should be taken into account for adolescent groups when developing a control policy for the mitigation of NCDs. Currently, questionnaires are the most widely used tool to monitor physical activity levels in community-based studies. However, given the numerous approaches in physical activity measurement, a better understanding of the existing standardized measurements is necessary. This is needed to ensure not only the validity of a survey, but also to both discuss and share results with involved researchers and decision makers to apply novel approaches to future research.
Unhealthy diets
Although the traditional diet in Vietnam and other Western countries has been known for a high proportion of plant-based foods, the average consumption of fruits and vegetables during 1987 until 2010 in Vietnam (175–251 g) was lower than the recorded consumption of half of European countries (Nguyen and Hoang, 2018; Nguyen et al., 2020; Vietnam Ministry of Health, 2012). Yet, the findings from STEP 2015 illustrated that Vietnam’s figure had increased to become higher than most of European countries; this was done in pace with the rising awareness of eating more fruits and vegetables for a healthy lifestyle (Nguyen et al., 2020; Vietnam Ministry of Health, 2016). Salt consumption among Vietnamese population was assessed to be at 9.9 g/day (2010) and 9.4 gram/day (2015) respectively, almost double of the WHO recommendations, but similar to other countries around the world (Vietnam Ministry of Health, 2016; World Health Organization, 2012). These figures reflect the concerted efforts of WHO on salt intake reduction. Therefore, there is a need for coordinated actions by regional agencies to provide recommendations to boost Vietnam’s national salt reduction strategies.
Additionally, this review has identified data on dietary indicators which likely affect the burden of developing a NCD over time. The National Nutrition Survey in 1985, 2000, and 2010 demonstrated that there is no virtual change in total energy intake in the Vietnamese adult population since 1985 (1925 kcal in 1985 and 1925.4 kcal in 2010). However, consumption of lipids in proportion to total energy intake increased remarkably from only 6.2% in 1985 to 17.6% (±8.7%) in 2010 (National Institute of Nutrition, 2012). The pattern of fat intake among Vietnamese population was assessed to be lower than the WHO recommendation of less than 30% of total energy intake (World Health Organization, 2003), appropriate monitoring and surveillance of this factor should be taken into account for future studies.
From our review, we identified that dietary evidence in Vietnam can be considered as poor-quality in relation to other NCD risk factors which have led to the lack of representative data for decision making. Given its critical role in the manifestation of NCDs, the measurement of dietary risk factors should be included in future studies to enrich the evidence pool for a Vietnamese specific diet. Furthermore, government actions are needed to promote a healthier lifestyle that is accustomed to Vietnamese culture, with the application of both worldwide recommendations and lessons.
Broad context and further steps
From a scattered picture with limited data which was available from 2000 up to 15 years later, the mapping of major behavior risk factors at the national level has been created leading to the increased use of empirical data for addressing the burden of NCDs in Vietnam. Lessons learned from other developed countries in the world illustrate that when a population begins to age, NCD burden surges rapidly and severely with the accumulation of lifestyle risk factors. Similar issues that are presented by NCDs would challenge Vietnam due to the unavoidable aging population trend and the rapid economic growth. However, there is a possibility that Vietnam could keep pace with the growing burden of NCDs by controlling and directing change by modifying NCD risk factors.
To redirect limited resources for health policies and programs in NCDs, monitoring and surveillance of NCDs in a timely fashion is a necessary step to approach this problem. However, with exception of However, with the exception of the STEPS surveys which were conducted every 5 years since 2005 (smoking behavior has been separated into the GATS survey since 2010), there is a lack of an established and organized surveillance system in Vietnam to monitor and evaluate NCDs risk factors regularly. At present, monitoring and evaluating NCD modifiable risk factors is still not a major priority in Vietnamese policymaking. This has made the integration of NCD risk-factor surveillance into national health information systems fall short when attempting to translate the disease patterns in real-time and for future applications. On the other hand, our review has identified multiple surveys that have been conducted at the subnational or regional scale which overlap with the content of STEPS surveys, thereby wasting resources. Therefore, in a low-resource setting, a possible approach is to encourage the collection of NCD-related information on a regular basis, even at a small-scale. Through this, information about the patterns of NCDs and NCDs-related health behaviors would be surveyed and later incorporate into large datasets. Most importantly, the use of nine voluntary targets for NCDs and the Global Monitoring Framework for NCDs indicators should be better informed in NCD-related research to ensure the consistency of data quality for decision making. Additionally, the consistency in health behaviors surveillance which use a set of nine voluntary targets for NCDs and the Global Monitoring Framework for NCDs indicators, would be better informed in using this service to strengthen the database for decision-making. This way not only saves resources and time, but enables Vietnam to monitor progress across the entire country and allow comparison with neighboring countries. In the long run, the establishment and maintenance of such program would require both adequate tools and public resources to ensure sustainability over time. Given its fundamental role and the long-term utilization of health data for policy evaluation, the development of such database is highly recommended.
Limitations
A few limitations should be noted in this review. First, numerous documents published in the Vietnamese language before 2000 were not available as an electronic version at the time of review, resulting in the limited access and assessment of their validity. Secondly the definitions and the methods for calculation were not fully described in some retrieved published articles. This may hinder or mislead the explanation and comparison of findings across all included materials. As a result, the findings of this review could be limited to generalizations both actual and local studies, rather than in a wider context.
Conclusion
Our review illustrates current patterns of behavioral risk factors for non-communicable diseases in Vietnam. First, tobacco use across a vast number of long-term daily smokers still remains a significant challenge that requires novel initiatives to expand the current impact to a higher degree. Second, as the use of alcoholic beverages is a long-standing cultural tradition, Vietnam has just been confronted with the enactment of Law on Prevention and Control of Alcohol-related harms in 2020 as the first country-level action. Third, diet and physical activity have shifted gradually but are unpredictable under the influence of rapid economic growth. The lack of information and supporting environment for the regular practices surrounding a healthy lifestyle have been recognized as the front-line barrier in Vietnam and many other developing countries (Bui et al., 2015; Heath et al., 2012). It should be noted that the application of current data is not fully met, based on the demand of program and policy planning. This is due to the fact that findings tend to be fragmented and are not regularly updated, in addition to the lack of a total representation for all disadvantaged groups. Thus, the major issues in present are both the lack of an organized surveillance system and the heavy reliance on international funds, which have hindered the implementation of effectively tailored interventions at the national level.
As a result, surveillance and monitoring of behavioral risk factors should be at the forefront and primary step at present to control NCDs. A standardized surveillance framework system should first be initially developed, allocated with adequate public budget and tools for the regular monitoring of the current situation and to assess upcoming trends. Depending on the priority, the surveillance system should target diverse socioeconomic groups and evaluate both the policy implementation and impact. Following the population-based data, a major benefit can be received not only in terms of NCD prevention and control, but also the health sector and other central agencies who can make use of the detailed and up-to-date analytics provided by selecting health priorities through the allocation of available resources. This manuscript will hopefully serve as a reference for health authorities, health activists, and researchers in Vietnam in developing long term initiatives for NCD prevention and control.
Acknowledgments
The authors would like to thank Jonathan Josephs-Spaulding for his editorial support which greatly improves the manuscript.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Nguyen Thuy Duyen  https://orcid.org/0000-0002-1522-3181
https://orcid.org/0000-0002-1522-3181
Kim Bao Giang  https://orcid.org/0000-0003-2290-0205
https://orcid.org/0000-0003-2290-0205
Vu Thu Trang  https://orcid.org/0000-0002-6790-6857
https://orcid.org/0000-0002-6790-6857
References
- Ahmed SM, Hadi A, Razzaque A, et al. (2009) Clustering of chronic non-communicable disease risk factors among selected Asian populations: Levels and determinants. Global Health Action 2: 68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Archie S, Zangeneh Kazemi A, Akhtar-Danesh N. Concurrent binge drinking and depression among Canadian youth: Prevalence, patterns, and suicidality. [DOI] [PubMed] [Google Scholar]
- Bell S, Lee C. (2005) Emerging adulthood and patterns of physical activity among young Australian women. International Journal of Behavioral Medicine 12: 227–235. [DOI] [PubMed] [Google Scholar]
- Bilano V, Gilmour S, Moffiet T, et al. (2015) Global trends and projections for tobacco use, 1990-2025: An analysis of smoking indicators from the WHO comprehensive information systems for tobacco control. The Lancet 385: 966–976. [DOI] [PubMed] [Google Scholar]
- Bui TV, Blizzard CL, Luong KN, et al. (2015) Physical activity in Vietnam: Estimates and measurement issues. PloS One 10: e0140941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bui TV, Blizzard CL, Luong KN, et al. (2016) Fruit and vegetable consumption in Vietnam, and the use of a ‘standard serving’ size to measure intake. British Journal of Nutrition 116: 149–157. [DOI] [PubMed] [Google Scholar]
- Corder K, Winpenny E, Love R, et al. (2019) Change in physical activity from adolescence to early adulthood: A systematic review and meta-analysis of longitudinal cohort studies. British Journal of Sports Medicine 53: 496–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuong TQ, Dibley MJ, Bowe S, et al. (2007) Obesity in adults: An emerging problem in urban areas of Ho Chi Minh City, Vietnam. European Journal of Clinical Nutrition 61: 673–681. [DOI] [PubMed] [Google Scholar]
- Do HTP, Geleijnse JM, Le MB, et al. (2015) National prevalence and associated risk factors of hypertension and prehypertension among Vietnamese adults. American Journal of Hypertension 28: 89–97. [DOI] [PubMed] [Google Scholar]
- Esser MB, Hedden SL, Kanny D, et al. (2014) Prevalence of alcohol dependence among US adult drinkers, 2009-2011. Preventing Chronic Disease 11: E206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- General Statistics Office of Vietnam (1993) Vietnam Living Standards Survey 1992-1993. Hanoi: Statistical Publishing House. [Google Scholar]
- General Statistics Office of Vietnam (1998) Vietnam Living Standards Survey 1997-1998. Hanoi: Statistical Publishing House. [Google Scholar]
- General Statistics Office of Vietnam (2003) Vietnam Living Standards Survey 2001-2002. Hanoi: Statistical Publishing House. [Google Scholar]
- General Statistics Office of Vietnam (2007) Vietnam Living Standards Survey (VLSS) 2006. Hanoi: Statistical Publishing House. [Google Scholar]
- Giang KB, Van Minh H, Allebeck P. (2013) Alcohol consumption and household expenditure on alcohol in a rural district in Vietnam. Global Health Action 6: 18937–18937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giovino GA. (2002) Epidemiology of tobacco use in the United States. Oncogene 21: 7326–7340. [DOI] [PubMed] [Google Scholar]
- Hanoi Medical University (2013) Vietnam Global School-Based Student Health Survey 2013 WHO - NCD Microdata Repository Hanoi: WHO. US Center for Disease Control and Prevention. [Google Scholar]
- Heath GW, Parra DC, Sarmiento OL, et al. (2012) Evidence-based intervention in physical activity: Lessons from around the world. Lancet 380: 272–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hermens DF, Lagopoulos J, Tobias-Webb J, et al. Pathways to alcohol-induced brain impairment in young people: A review. Cortex 49(1): 3. [DOI] [PubMed] [Google Scholar]
- Hoang VM, Byass P, Dao LH, et al. (2007) Risk factors for chronic disease among rural Vietnamese adults and the association of these factors with sociodemographic variables: Findings from the WHO STEPS survey in rural Vietnam, 2005. Preventing Chronic Disease 4: A22. [PMC free article] [PubMed] [Google Scholar]
- Hoy D, Rao C, Nhung NT, et al. (2013) Risk factors for chronic disease in Vietnam: A review of the literature. Preventing Chronic Disease 10: 120067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huu Bich T, Thi Quynh Nga P, Ngoc Quang L, et al. (2009) Patterns of alcohol consumption in diverse rural populations in the Asian region. Global Health Action 2: 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine (2007) Ending the Tobacco Problem: A Blueprint for the Nation. Washington, DC: The National Academies Press. [Google Scholar]
- Jawad M, Charide R, Waziry R, et al. (2018) The prevalence and trends of waterpipe tobacco smoking: A systematic review. PloS One 13: e0192191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen PN, Bao TQ, Huong TTT, et al. (2018) The association of estimated salt intake with blood pressure in a Viet Nam national survey. PloS One 13: e0191437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalinowski A, Humphreys K. (2016) Governmental standard drink definitions and low-risk alcohol consumption guidelines in 37 countries. Addiction (Abingdon, England) 111: 1293−1298. [DOI] [PubMed] [Google Scholar]
- Kanungsukkasem U, Ng N, Van Minh H, et al. (2009) Fruit and vegetable consumption in rural adults population in INDEPTH HDSS sites in Asia. Global Health Action 2: 35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khalil H, Peters M, Godfrey CM, et al. (2016) An evidence-based approach to scoping reviews. Worldviews on Evidence-Based Nursing 13: 118–123. [DOI] [PubMed] [Google Scholar]
- Khue NT. (2015) Diabetes in Vietnam. Annals of Global Health 81: 870–873. [DOI] [PubMed] [Google Scholar]
- Korfei M. (2018) The underestimated danger of E-cigarettes - also in the absence of nicotine. Respiratory Research 19: 159–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lachenmeier DW, Anh PTH, Popova S, et al. (2009) The quality of alcohol products in Vietnam and its implications for public health. International Journal of Environmental Research and Public Health 6: 2090−2101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ly KA, Ton TG, Ngo QV, et al. (2013) Double burden: A cross-sectional survey assessing factors associated with underweight and overweight status in Danang, Vietnam. BMC Public Health 13: 35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manthey J, Shield KD, Rylett M, et al. (2019) Global alcohol exposure between 1990 and 2017 and forecasts until 2030: A modelling study. The Lancet 393: 2493–2502. [DOI] [PubMed] [Google Scholar]
- Ministry of Health of China (2011) Global Adult Tobacco Survey (GATS) in China 2010. China: World Health Organization. [Google Scholar]
- Ministry of Health of Indonesia (2012) Global Adult Tobacco Survey (GATS) in Indonesia 2011. New Delhi: World Health Organization Regional Office in South-East Asia. [Google Scholar]
- Ministry of Health of Malaysia (2012) Global Adult Tobacco Survey (GATS) in Malaysia 2011. Malaysia: Institute for Public Health, National Institute of Health (Ministry of Health). [Google Scholar]
- Ministry of Health of Thailand (2012) Global Adult Tobacco Survey (GATS): Comparison Factsheet 2009−2011. Thailand: World Health Organization, Regional Office for South-East Asia. [Google Scholar]
- Minh An DT, Van Minh H, Huong T, et al. (2013) Knowledge of the health consequences of tobacco smoking: A cross-sectional survey of Vietnamese adults. Global Health Action 6: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrow M, Barraclough S. (2003) Tobacco control and gender in South-East Asia. Part II: Singapore and Vietnam. Health Promotion International 18: 373–380. [DOI] [PubMed] [Google Scholar]
- National Institute of Alcohol Abuse and Alcoholism (2004) NIAAA Council Approves Definition of Binge Drinking. USA: National Institutes of Health. [Google Scholar]
- National Institute of Nutrition (2010) A Review of the Nutrition Situation in Vietnam 2009-2010. Hanoi: Medical Publishing House. [Google Scholar]
- National Institute of Nutrition (2012) Summary of Main Findings of General Nutrition Survey 2009-2010. Hanoi: Medical Publishing House. [Google Scholar]
- Nelson MC, Story M, Larson NI, et al. (2008) Emerging adulthood and college-aged youth: An overlooked age for weight-related behavior change. Obesity (Silver Spring) 16: 2205–2211. [DOI] [PubMed] [Google Scholar]
- Nethan S, Sinha D, Mehrotra R. (2017) Non communicable disease risk factors and their trends in India. Asian Pacific Journal of Cancer Prevention 18: 2005–2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng N, Hakimi M, Van Minh H, et al. (2009) Prevalence of physical inactivity in nine rural INDEPTH health and demographic surveillance systems in five Asian countries. Global Health Action 2: 44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen HN, Fujiyoshi A, Abbott RD, et al. (2013) Epidemiology of cardiovascular risk factors in Asian countries. Circulation Journal 77: 2851–2859. [DOI] [PubMed] [Google Scholar]
- Nguyen TT, Hoang MV. (2018) Non-communicable diseases, food and nutrition in Vietnam from 1975 to 2015: The burden and national response. Asia Pacific Journal of Clinical Nutrition 27: 19–28. [DOI] [PubMed] [Google Scholar]
- Nguyen QN, Pham ST, Do LD, et al. (2012. a) Cardiovascular disease risk factor patterns and their implications for intervention strategies in vietnam. International Journal of Hypertension 2012: 560397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen QN, Pham ST, Nguyen VL, et al. (2012. b) Time trends in blood pressure, body mass index and smoking in the Vietnamese population: A meta-analysis from multiple cross-sectional surveys. PloS One 7: e42825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen SM, Tran HTT, Tran BQ, et al. (2020) Compliance to dietary guidelines on fruit and vegetable intake and prevalence of hypertension among Vietnamese adults, 2015. European Journal of Preventive Cardiology 27: 39–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen Thanh Liem. (2010) Using Alcohol, Beer and Cigarette Among Vietnamese Youth - The Analysis Result of Survey Assessment of Vietnamese Youth 2003 and 2009 (SAVY). Hanoi: Asian Development Bank. [Google Scholar]
- Peters MD, Godfrey CM, Khalil H, et al. (2015) Guidance for conducting systematic scoping reviews. International Journal of Evidence-Based Healthcare 13: 141–146. [DOI] [PubMed] [Google Scholar]
- Pham LH, Au TB, Blizzard L, et al. (2009) Prevalence of risk factors for non-communicable diseases in the Mekong Delta, Vietnam: Results from a steps survey. BMC Public Health 9: 291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sacks JJ, Gonzales KR, Bouchery EE, et al. (2015) 2010 National and state costs of excessive alcohol consumption. American Journal of Preventive Medicine 49: e73–e79. [DOI] [PubMed] [Google Scholar]
- Saleheen D, Zhao W, Rasheed A. Epidemiology and public health policy of tobacco use and cardiovascular disorders in low- and middle-income countries. Arteriosclerosis, Thrombosis, and Vascular Biology 34(9): 10. [DOI] [PubMed] [Google Scholar]
- Sirichotiratana N, Sovann S, Aditama TY, et al. (2008) Linking data to tobacco control program action among students aged 13-15 in Association of Southeast Asian Nations (ASEAN) member states, 2000-2006. Tobacco Control 17: 372–378. [DOI] [PubMed] [Google Scholar]
- Son PT, Quang NN, Viet NL, et al. (2012) Prevalence, awareness, treatment and control of hypertension in Vietnam-results from a national survey. Journal of Human Hypertension 26: 268–280. [DOI] [PubMed] [Google Scholar]
- Stahre M, Roeber J, Kanny D, et al. (2014) Contribution of excessive alcohol consumption to deaths and years of potential life lost in the United States. Preventing Chronic Disease 11: E109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thoa LTK, Hoang DH, Vung ND, et al. (2013) Alcohol use, risk taking, leisure activities and health care use among young people in Northern Vietnam. Central Asian Journal of Global Health 2: 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thu Hien VT, Thi Lam N, Cong Khan N, et al. (2013) Monosodium glutamate is not associated with overweight in Vietnamese adults. Public Health Nutrition 16: 922–927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trang NHHD, Hong TK, Dibley MJ. (2012. a) Cohort profile: Ho Chi Minh City Youth cohort-changes in diet, physical activity, sedentary behaviour and relationship with overweight/obesity in adolescents. BMJ Open 2: e000362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trang NHHD, Hong TK, Dibley MJ, et al. (2009) Factors associated with physical inactivity in adolescents in ho chi minh city, vietnam. Medicine and Science in Sports and Exercise 41: 1374–1383. [DOI] [PubMed] [Google Scholar]
- Trang NHHD, Hong TK, Van Der Ploeg HP, et al. (2012. b) Longitudinal physical activity changes in adolescents: Ho Chi Minh City Youth cohort. Medicine and Science in Sports and Exercise 44: 1481–1489. [DOI] [PubMed] [Google Scholar]
- Tricco AC, Lillie E, Zarin W, et al. (2018) PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Annals of Internal Medicine 169: 467–473. [DOI] [PubMed] [Google Scholar]
- Trinh OTH, Nguyen ND, Dibley MJ, et al. (2008) The prevalence and correlates of physical inactivity among adults in Ho Chi Minh City. BMC Public Health 8: 204–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trinh OT, Nguyen ND, Phongsavon P, et al. (2010) Metabolic risk profiles and associated risk factors among Vietnamese adults in Ho Chi Minh City. Metabolic Syndrome and Related Disorders 8: 69–78. [DOI] [PubMed] [Google Scholar]
- UN General Assembly (2012) NCD Global Monitoring Framework. [Google Scholar]
- US Department of Health and Human Services (2009) Results from the 2008 National Survey on Drug Use and Health: Summary of National Findings. [Google Scholar]
- Van Bui T, Blizzard CL, Luong KN, et al. (2016) Alcohol consumption in Vietnam, and the use of ‘standard drinks’ to measure alcohol intake. Alcohol Alcohol 51: 186–195. [DOI] [PubMed] [Google Scholar]
- Van Minh H, Giang KB, Ngoc NB, et al. (2017) Prevalence of tobacco smoking in Vietnam: Findings from the global adult tobacco survey 2015. International Journal of Public Health 62: 121–129. [DOI] [PubMed] [Google Scholar]
- Van Minh H, Huong DL, Giang KB. (2008) Self-reported chronic diseases and associated sociodemographic status and lifestyle risk factors among rural Vietnamese adults. Scandinavian Journal of Public Health 36: 629–634. [DOI] [PubMed] [Google Scholar]
- Vietnam Ministry of Health (2003) Vietnam Global Youth Tobacco Survey (GYTS) 2003 in 5 cities (Fact Sheet). Hanoi: Vietnam Ministry of Health. [Google Scholar]
- Vietnam Ministry of Health (2007) Vietnam Global Youth Tobacco Survey (GYTS) 2007 (Fact Sheet). Hanoi: Vietnam Ministry of Health. [Google Scholar]
- Vietnam Ministry of Health (2012) National Survey on the Risk Factors of Non-Communicable Diseases (STEPS) Vietnam, 2010. Hanoi: Vietnam Ministry of Health. [Google Scholar]
- Vietnam Ministry of Health (2015) In: Health M (ed.) National Strategy for the Prevention and Control of Noncommunicable Disease Period 2015-2025. Hanoi: Vietnam Ministry of Health. [Google Scholar]
- Vietnam Ministry of Health (2016) National Survey on the Risk Factors of Non-Communicable Diseases (STEPS) Vietnam, 2015. Hanoi: Vietnam Ministry of Health. [Google Scholar]
- Vietnam Ministry of Health (2017) Health Statistics Yearbook 2015. Hanoi: Medical Publishing House. [Google Scholar]
- Vietnam Ministry of Health, Hanoi Medical University, General Statistics Office, et al. (2010) Global Adult Tobacco Survey (GATS) Vietnam 2010. Hanoi: Vietnam Ministry of Health. [Google Scholar]
- Vietnam Ministry of Health, Hanoi Medical University, General Statistics Office, et al. (2016) Global Adult Tobacco Survey (GATS) Vietnam 2015. Hanoi: Vietnam Ministry of Health. [Google Scholar]
- Vietnam Ministry of Health and Health Partnership Group (2015) Joint Annual Health Review: Strengthening Prevention and Control of Non-communicable Disease. Hanoi: Medical Publishing House. [Google Scholar]
- Vietnam Ministry of Health, Vietnam Standing Committe on Smoking and Health, Hanoi Medical University, et al. (2014) Vietnam Global Youth Tobacco Survey (GYTS) 2014. Hanoi: Medical Publishing House. [Google Scholar]
- Vietnam National Institute of Nutrition (2007) Overweight - Obesity and Related Factors in Vietnamese Adults Aged 25-64 Years Old. Hanoi: Medical Publishing House. [Google Scholar]
- World Health Organization (2003) Diet, nutrition and the prevention of chronic diseases. WHO technical report series. [PubMed] [Google Scholar]
- World Health Organization (2005) Preventing Chronic Disease: A Vital Investment. Geneva: World Health Organization. [Google Scholar]
- World Health Organization (2012) Sodium Intake for Adults and Children Guideline WHO 2012. Geneva: World Health Organization. [Google Scholar]
- World Health Organization (2014) Global Status Report on Alcohol and Health 2014 - Country Profile (Vietnam). Geneva: World Health Organization. [Google Scholar]
- World Health Organization (2015) Global Health Observatory Data: Prevalence of Tobacco Smoking (Aged 15 Years and Older, 2015, Male). Geneva: World Health Organization. [Google Scholar]
- World Health Organization (2018. a) Global Health Observatory Data: Prevalence of Insufficient Physical Activity (Adult Aged 18+ Years). Geneva: World Health Organization. [Google Scholar]
- World Health Organization (2018. b) Global Status Report on Alcohol and Health 2018 - Country Profile (Vietnam). Geneva: World Health Organization. [Google Scholar]
- World Health Organization (2018. c) Noncommunicable Diseases (NCD) Country Profile 2018. Geneva: World Health Organization. [Google Scholar]