Key Points
Question
What is the within-couple concordance of cardiovascular (CV) risk factors and behaviors?
Findings
In this cross-sectional study of 5364 couples consisting of employees and spouses (or domestic partners) undergoing an annual employer-sponsored health assessment, 79% of the couples were in the nonideal category of a CV health score. This within-couple concordance of nonideal CV health scores was associated mostly with unhealthy diet and inadequate physical activity.
Meaning
The high concordance of nonideal CV risk factors and behaviors within couples suggests that behavioral modification programs may benefit both the targeted and the nontargeted member of the couple.
Abstract
Importance
Married couples and domestic partners have been reported to share similar environmental exposures, adopt similar behavior patterns, and have similar transferable characteristics. However, the degree to which couples share similar levels of cardiovascular risk factors and behaviors is uncertain.
Objective
To assess within-couple concordance of the American Heart Association–defined Life’s Simple 7 (LS7).
Design, Setting, and Participants
Cross-sectional study with a longitudinal substudy of employees and spouses (or domestic partners) who participated in an employer-sponsored health assessment program throughout the United States between October 2014 and December 2018. Data were analyzed from November 1, 2019, to August 4, 2020.
Exposures
Having a spouse or domestic partner.
Main Outcomes and Measures
The LS7 risk factors and behaviors (smoking status, body mass index, exercise, diet, total cholesterol, blood pressure, and fasting glucose) were assessed by questionnaires, examinations, and laboratory tests. LS7 categories were scored as 2 for ideal, 1 for intermediate, or 0 for poor and summed to generate a CV health score.
Results
The study included 10 728 participants (5364 couples): 7% were African American, 11% Hispanic, 21% Asian, and 54% White (median [interquartile range] age, 50 [41-57] years for men and 47 [39-55] for women). For most couples, both members were in the ideal category or both were in a nonideal category. Concordance ranged from 53% (95% CI, 52%-54%) for cholesterol to 95% (95% CI, 94%-95%) for diet. For the CV health score, in 79% (95% CI, 78%-80%) of couples both members were in a nonideal category, which was associated mainly with unhealthy diet (94% [95% CI, 93%-94%] of couples) and inadequate exercise (53% [95% CI, 52%-55%] of couples). However, in most couples, both members were in the ideal category for smoking status (60% [95% CI, 59%-61%] of couples) and glucose (56% [95% CI, 55%-58%]). Except for total cholesterol, when 1 member of a couple was in the ideal category, the other member was likely also to be in the ideal category: the adjusted odds ratios for also being in the ideal category ranged from 1.3 (95% CI, 1.1-1.5; P ≤ .001) for blood pressure to 10.6 (95% CI, 7.4-15.3; P ≤ .001) for diet. Concordance differed by ethnicity, socioeconomic status, and geographic location. A 5-year longitudinal analysis of 2186 couples found modest changes in concordance of blood pressure (from 55% [95% CI, 53%-57%] to 59% [95% CI, 57%-61%]; P < .001 for trend) and fasting glucose (from 64% [95% CI, 62%-66%] to 59% [95% CI, 57%-61%]; P < .001 for trend) with no change in other factors.
Conclusions and Relevance
In this study, high concordance of nonideal behaviors was found within couples; behavioral modification programs may benefit both the targeted and the nontargeted member of a couple.
This cross-sectional study assesses the within-couple concordance of cardiovascular risk factors and behaviors within couples who participated in a nationwide US employer-sponsored health assessment program.
Introduction
Risk factors for cardiovascular (CV) disease include environmental exposures,1,2 behaviors such as minimal physical activity, smoking status, and unhealthy dietary choices,1 and genetic factors.3,4 Couples, both married couples and domestic partners, are likely to share similar environmental exposures, adopt similar behavior patterns, and have similar transferable characteristics due to assortative mating (nonrandom partner selection based on similarity of observable characteristics).5 However, the degree to which couples share similar levels of these CV risk factors and behaviors is uncertain.
Assessing the concordance of CV risk factors and behaviors within couples may help inform public health policy decisions about the potential effectiveness of programs that target couples. If high levels of poor CV risk factor measures and behaviors are common in both members of a couple, programs that target improvement of these risk factors and behaviors may benefit CV health in both members of the couple. Prior studies of the concordance of CV and diabetes risk factors and behaviors within couples and in large social networks were limited to 1 or 2 factors, or were small local studies that may not be representative of the US geographic distribution, ethnic makeup, or socioeconomic distribution.6,7,8,9,10,11,12,13,14,15,16
Therefore, for a large cohort of 10 728 employees and their spouses or domestic partners (5364 couples) who participated in a nationwide US employer-sponsored health assessment program, we determined whether characteristics of each individual were categorizable into an ideal, intermediate, or poor category for each of the American Heart Association (AHA)-defined Life’s Simple 7 (LS7) risk factors and behaviors.17 We also investigated the concordance within couples in a nested longitudinal study of 2186 couples who participated in the 5 consecutive annual health risk assessment examinations from 2014 to 2018. In addition, we assessed whether the concordance differed by ethnicity, socioeconomic status, or geographic location.
Methods
The study population was drawn from 32 388 employees and spouses or domestic partners who participated in a voluntary health assessment program at baseline (October 2014 to August 2015) at Quest Diagnostics (eFigure 1 in the Supplement). We excluded those without a participating spouse (n = 20 448) and couples with missing data for either member of a couple (606 couples; 1212 individuals). The remaining 5364 couples (10 728 individuals) were included in the study. A retrospectively identified longitudinal substudy included 2186 couples who participated in the same health assessment program for 5 consecutive years (October 2014 to December 2018). This report follows the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline for cross-sectional studies.18 The Western Institutional Review Board determined that this research was conducted according to the HIPAA Privacy Rule (Title 45 Code of Federal Regulations, Section 164.514e) which governs research conducted by Covered Healthcare Entities and allows retrospective analysis using a limited data set without requiring an Institutional Review Board approval.
Description of the health assessment program (which included self-assessment questionnaires, examinations, and laboratory tests) is included in eMethods in the Supplement. Metabolic syndrome was defined using criteria reported in the 2018 AHA/ACC guideline on the management of blood cholesterol.19 Ethnicity was assessed from participant response to a multiple choice questionnaire (eMethods in the Supplement). Geographic regions (Northeast, South, Midwest, or West) were defined according to the US Census Bureau definition.20 Socioeconomic status was determined according to the participant’s zip code. The median income of each zip code (as a percent of the state median income) was categorized into 4 groups according to predefined US government definitions of low-income areas.21
LS7 risk factors and behaviors included smoking status, body mass index (BMI), physical activity, healthy diet score, total cholesterol, blood pressure, fasting glucose were assessed by questionnaires, examinations, and laboratory tests. The LS7 categories (poor, intermediate, and ideal) were defined according to the AHA definitions.17 The diet and exercise questions were similar but not identical to the score definitions of LS7. We defined a modified diet score based on self-reported daily servings of fruits and vegetables, high-fiber foods, and high-fat foods. The physical activity score was based on self-reported minutes per week of aerobic exercise and strength training (eMethods in the Supplement). The LS7 categories were scored as 2 for ideal, 1 for intermediate, 0 for poor. A CV health score was defined as the sum of scores for each of the LS7 risk factors and behaviors. Couples were considered in concordance of an ideal category when both were in the ideal category, in concordance of a nonideal category when both were in nonideal categories, and in discordance otherwise.
Statistical Analysis
Continuous variables were summarized as median and interquartile range (IQR). Categorical variables were summarized as count and percent. Comparison between groups for continuous variables was assessed by Wilcoxon rank sum tests. Comparison between groups for categorical variables was assessed by the χ2 tests. To assess the association between 1 member of a couple (member 1) being in the ideal category of CV risk factor or behavior and the other member (member 2) also being in the ideal category (vs nonideal) a member 1 label was randomly assigned to 1 member of a couple. The association was assessed in logistic regression models that adjusted for the age and sex of member 2 as well as the status (ideal, intermediate, or poor) of the remaining 6 risk factors and behaviors of member 2. The model takes the following form (in which LS1 is the factor of interest and LS2-LS7 are the other 6 factors): [member2_LS1status] ~ [member1_LS1status] + [member2_age] + [member2_sex] +[member2_LS2status] + [member2_LS3status]+…. Within-couple correlation was assessed by Spearman correlation coefficient. Concordance of LS7 risk factors and behaviors within couples was assessed by square-weighted κ coefficients.22 The variation in the percent of couples in concordance of nonideal categories according to ethnicity, socioeconomic status, and geographic location was assessed by χ2 test. The variations of within-couple concordance over time and in the percent of participants in ideal LS7 and CV health categories over time were assessed by generalized estimating equations with an exchangeable correlation structure between LS7 risk factors and behaviors as well as CV health score to account for within-couple variation in couples or in individuals. The estimates of the percent of participants in ideal categories of LS7 risk factors and behaviors as well as CV health score over time were adjusted for age and sex. Additional generalized estimating equations models were used to model the incidence of newly attained ideal status of a risk factor among 1 member of a couple (member 2) who had nonideal risk factor status in the prior year. Attaining ideal status of the risk factor for member 2 in year t was modeled as a function of the risk factor status of member 1 in the prior year (t-1) and adjusted for year as well as the sex and prior year age of member 2. Robust standard errors in generalized estimating equations were used to estimate P values. Significance level was set as 2-sided P < .005 to account for multiple testing. All analyses were performed in R software, version 3.5.1 (R Project for Statistical Computing).
Results
We evaluated 10 728 working-age individuals, consisting of 5364 married couples or domestic partners, with median age for men 50 (IQR, 41 to 57) years, and for women 47 (IQR, 39 to 55) years. The study population was diverse geographically (from all 50 US states), ethnically (7% African American, 11% Hispanic, 21% Asian, 54% white), and socioeconomically (Table 1). More than 50% of the individual participants were in the ideal category of 3 LS7 risk factors and behaviors: smoking status (never smoked), total cholesterol (<200 mg/dL [to convert to millimoles per liter, multiply by 0.0259]), and fasting glucose (<100 mg/dL [to convert to millimoles per liter, multiply by 0.0555]) (Table 2). In contrast, more than one-quarter of the individuals were in the poor categories for BMI, physical activity, and CV health score with no more than one-third of the individuals reaching the ideal categories—only 12% were in the ideal category for the CV health score.
Table 1. Baseline Characteristics of Individual Participantsa.
| Characteristic | No. (%) | |
|---|---|---|
| Men (n = 5353)b | Women (n = 5375)b | |
| Age, median (IQR), y | 50 (41-57) | 47 (39-55) |
| Race/ethnicity | ||
| African American | 410 (7.7) | 365 (6.8) |
| Hispanic | 581 (10.9) | 608 (11.3) |
| Asian | 1088 (20.3) | 1202 (22.4) |
| White | 2936 (54.8) | 2858 (53.2) |
| Otherc | 338 (6.3) | 342 (6.4) |
| Geographic region | ||
| Northeast | 1374 (25.7) | 1377 (25.6) |
| Midwest | 982 (18.3) | 993 (18.5) |
| South | 1704 (31.8) | 1714 (31.9) |
| West | 1293 (24.2) | 1291 (24.0) |
| Socioeconomic statusd | ||
| <60% | 105 (2.0) | 107 (2.0) |
| 60%-100% | 1418 (26.5) | 1428 (26.6) |
| >100%-140% | 1940 (36.2) | 1941 (36.1) |
| >140% | 1856 (34.7) | 1869 (34.8) |
| Othere | 34 (0.6) | 30 (0.6) |
| BMI, median (IQR) | 27.6 (25.0-31.0) | 26.0 (22.8-30.6) |
| Waist circumference, median (IQR), cm | 94.0 (86.4-101.6) | 83.8 (76.2-94.0) |
| Smoking status | ||
| Current | 674 (12.6) | 348 (6.5) |
| Former | 1082 (20.2) | 745 (13.9) |
| Never | 3597 (67.2) | 4282 (79.7) |
| Cholesterol, median (IQR), mg/dL | ||
| HDL | 47 (40-56) | 60 (50-72) |
| LDL | 111 (89-132) | 106 (87-127) |
| Total | 186 (162-211) | 189 (167-214) |
| Triglycerides, median (IQR), mg/dL | 116 (83-165) | 93 (67-132) |
| Fasting glucose, median (IQR), mg/dL | 95 (88-103) | 89 (83-96) |
| Hypertensionf | 1995 (37.3) | 1339 (24.9) |
| Diabetesg | 701 (13.1) | 384 (7.1) |
| Physical activity, median (IQR), min/wk | 75 (0-188) | 60 (0-158) |
| Healthy diet score, median (IQR)h | 3 (2-4) | 4 (3-4) |
| CV Health score, median (IQR)i | 8 (7-10) | 10 (8-11) |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); CV, cardiovascular; HDL, high-density lipoprotein; IQR, interquartile range; LDL, low-density lipoprotein.
SI conversion factors: To convert HDL, LDL, and total cholesterol to millimoles per liter, multiply by 0.0258; triglycerides to millimoles per liter, multiply by 0.0113; and glucose to millimoles per liter, multiply by 0.0555.
All values were different between men and women (P < .001), except for ethnicity, geographic region, and socioeconomic status.
Including 25 same-sex male couples and 36 same-sex female couples.
Native American individuals (25 men and 14 women) and missing data.
Median income of zip code as percent of state median income.
Zip codes without corresponding census-defined median income were excluded.
Systolic blood pressure ≥140 mm Hg, diastolic blood pressure ≥90 mm Hg, or a self-reported physician diagnosis of hypertension.
Fasting glucose >125 mg/dL, hemoglobin A1c >6.4, %, or self-reported physician diagnosis of diabetes.
Healthy diet score ranged from 0 to 6.
CV Health score ranged from 1 to 14.
Table 2. Cardiovascular Risk Factors and Behaviors of 10 728 Individual Participants at Baseline.
| Factor | CV risk factors and behaviors categories | ||||||
|---|---|---|---|---|---|---|---|
| Poor | Intermediate | Ideal | |||||
| Criteria | % | Criteria | % | Criteria | % | ||
| Smoking status | Current | 9.5 | Former | 17.0 | Never | 73.4 | |
| BMI | ≥30 | 29.5 | 25-29.9 | 37.1 | <25 | 33.4 | |
| Physical activity, min/wk | 0 | 26.1 | 1-149 | 42.6 | ≥150 | 31.3 | |
| Healthy diet scorea | ≤2 | 21.3 | 3-5 | 75.0 | ≥6 | 3.7 | |
| Total cholesterol, mg/dL | ≥240 | 9.1 | 200-239 | 36.8 | <200b | 54.2 | |
| Blood pressure, mm Hg | SBP ≥140 or DBP ≥90 | 16.3 | SBP 120-139 or DBP 80-89 | 47.1 | SBP <120 and DBP <80b | 36.6 | |
| Fasting glucose, mg/dL | ≥126 | 5.9 | 100-125 | 20.2 | <100b | 74.0 | |
| CV health scorec | ≤7 | 26.7 | 8-11 | 61.3 | >11 | 12.1 | |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); CV, cardiovascular; DBP, diastolic blood pressure; SBP, systolic blood pressure.
SI conversion factors: To convert total cholesterol to millimoles per liter, multiply by 0.0259; glucose to millimoles per liter, multiply by 0.0555.
Sum of scores for servings per day of the following: fruits and vegetables (score of 0 for 0-1 servings, 1 for 2-3, 2 for ≥4), high-fiber foods (score of 0 for 0-1 servings, 1 for 2-4, 2 for ≥5), and high-fat foods (score of 0 for ≥4 servings, 1 for 2-3, 2 for 0-1).
Without medications. Those with medications were considered intermediate.
Global cardiovascular health score ranged from 1 to 14.
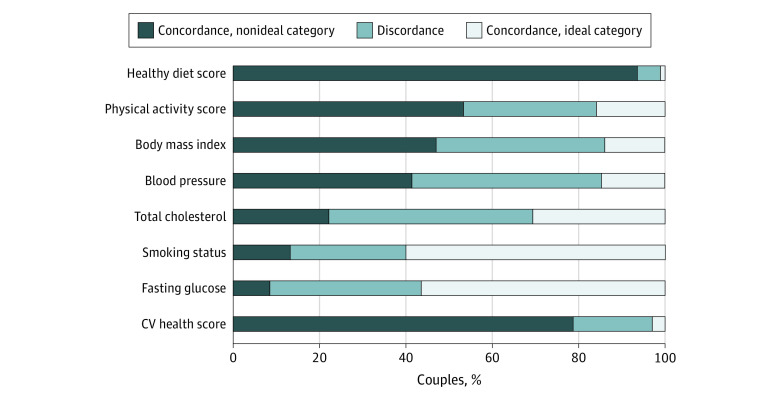
For all LS7 risk factors and behaviors, as well as for CV health score, the overall within-couple concordance was greater than 50%, ranging from a low of 53% (95% CI, 52%-54%) for total cholesterol to a high of 95% (95% CI, 94%-95%) for healthy diet score. For most couples, both member were in the ideal category for smoking (60%; 95% CI, 59%-61%; never smoked) and fasting glucose (56%; 95% CI, 55%-58%; had fasting glucose <100 mg/dL) (Figure 1). Conversely, both members of most couples were in the nonideal categories of healthy diet score (94%; 95% CI, 93%-94%), physical activity score (53%; 95% CI, 52%-55%), and CV health score (79%; 95% CI, 78%-80%). We also investigated the within-couples concordance of metabolic syndrome (a measure of metabolic risk factor clustering) and found that 73% (95% CI, 72%-74%) were concordant: either both had metabolic syndrome (6%; 95% CI, 5%-6%), or both did not have metabolic syndrome (67%; 95% CI, 66%-69%). The concordance of CV health score and LS7 factors and behaviors within couples was assessed by the κ coefficient which accounts for concordance due to chance. We found that all κ coefficients were greater than expected by chance (for example, observed concordance for smoking status was 85.5% vs expected concordance of 78.5%; κ = 0.33; P ≤ .001) (eTable 1 in the Supplement).
Figure 1. Percentage of Couples in Concordance Categories of CV Risk Factors and Behaviors.
Percentage of couples in concordance categories of each CV risk factor and behavior is indicated. Couples were considered in concordance of a nonideal category when both were in nonideal categories (dark blue), in concordance of an ideal category when both were in the ideal category (light gray), and in discordance otherwise (gray).
When 1 member of a couple was in the ideal category, the second member was more likely to be in the ideal category for all factors except for total cholesterol (Table 3) after adjusting for age, sex and the status of the remaining risk factors and behavior of the second member. These associations had a moderate effect size for blood pressure (adjusted odds ratio [aOR], 1.3; 95% CI, 1.1-1.5; P ≤ .001) and fasting glucose (aOR, 1.4; 95% CI, 1.2-1.7; P < .001); had a larger effect size for BMI (aOR, 2.0; 95% CI, 1.7-2.3; P < .001), physical activity (aOR, 3.3; 95% CI, 2.9-3.8; P < .001), and CV Health score (aOR, 3.6; 95% CI, 2.9-4.6; P < .001); and a substantial effect size for smoking status (aOR, 5.4; 95% CI, 4.7-6.3; P < .001) and healthy diet score (aOR, 10.6; 95% CI, 7.4-15.3; P < .001).
Table 3. Association Between CV Risk Categories in 1 Member With the Status of the Other Member of a Couple.
| Category | Unadjusted model | Adjusted modela | ||
|---|---|---|---|---|
| OR (95% CI) | P value | OR (95% CI) | P value | |
| Smoking status | 4.5 (3.9-5.1) | <.001 | 5.4 (4.7-6.3) | <.001 |
| BMI | 1.7 (1.5-1.9) | <.001 | 2.0 (1.7-2.3) | <.001 |
| Physical activity score | 3.6 (3.1-4) | <.001 | 3.3 (2.9-3.8) | <.001 |
| Healthy diet score | 13.3 (9.3-18.8) | <.001 | 10.6 (7.4-15.3) | <.001 |
| Total cholesterol | 1.2 (1.1-1.4) | <.001 | 1.1 (0.9-1.2) | .32 |
| Blood pressure | 1.3 (1.1-1.4) | <.001 | 1.3 (1.1-1.5) | <.001 |
| Fasting glucose | 1.6 (1.4-1.8) | <.001 | 1.4 (1.2-1.7) | <.001 |
| CV Health scoreb | 2.8 (2.2-3.4) | <.001 | 3.6 (2.9-4.6) | <.001 |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); CV, cardiovascular.
The association between 1 member of the couple (member 1) being in the ideal category, and the other member (member 2) also being in the ideal category (vs nonideal). The associations were adjusted for member 2 age, sex, and the status (ideal, intermediate, poor) of the remaining 6 risk factors and behaviors of member 2.
Adjusted model for age and sex only.
We investigated the concordance of LS7 factors and CV health score over time by analyzing 2186 couples who participated in 5 consecutive annual health risk assessment examinations from 2014 to 2018 in a nested longitudinal analysis. The 2186 couples had a slightly better CV risk factor profile than couples who did not participate in the health assessment program in each of the 5 consecutive years (for example, median [IQR] BMI for those who completed was 26.6 [23.6-30.4] vs 27.2 [24.0-31.1] for those who did not) (eTable 2 in the Supplement). Over this 5-year period, the percent of couples in concordance for blood pressure (both members of a couple were in a nonideal category or in an ideal category) modestly increased (55% [95% CI, 53%-57%] to 59% [95% CI, 57%-61%]; P < .001 for trend), whereas the percent of couples in concordance for fasting glucose modestly decreased (from 64% [95% CI, 62%-66%] to 59% [95% CI, 57%-61%]; P < .001 for trend) (Figure 2). There was no significant change in other LS7 factors or in the CV health score over time. The percent of individual participants in the ideal category (vs nonideal) was also mostly unchanged (eFigure 2 in the Supplement). However, we found that attaining ideal status by 1 member of a couple was associated with the ideal status of the other member in the prior year for smoking status (aOR, 2.3; 95% CI, 1.6-3.2; P < .001), BMI (aOR, 1.6; 95% CI,1.2-2.0; P < .001), physical activity score (aOR, 2.0; 9% CI, 1.7-2.4; P < .001), and healthy diet score (aOR, 6.4; 95% CI, 4.2-9.6; P < .001) (eTable 3 in the Supplement).
Figure 2. Percent of Couples in Concordance Categories of CV Risk Factors and Behaviors During 5 Years.
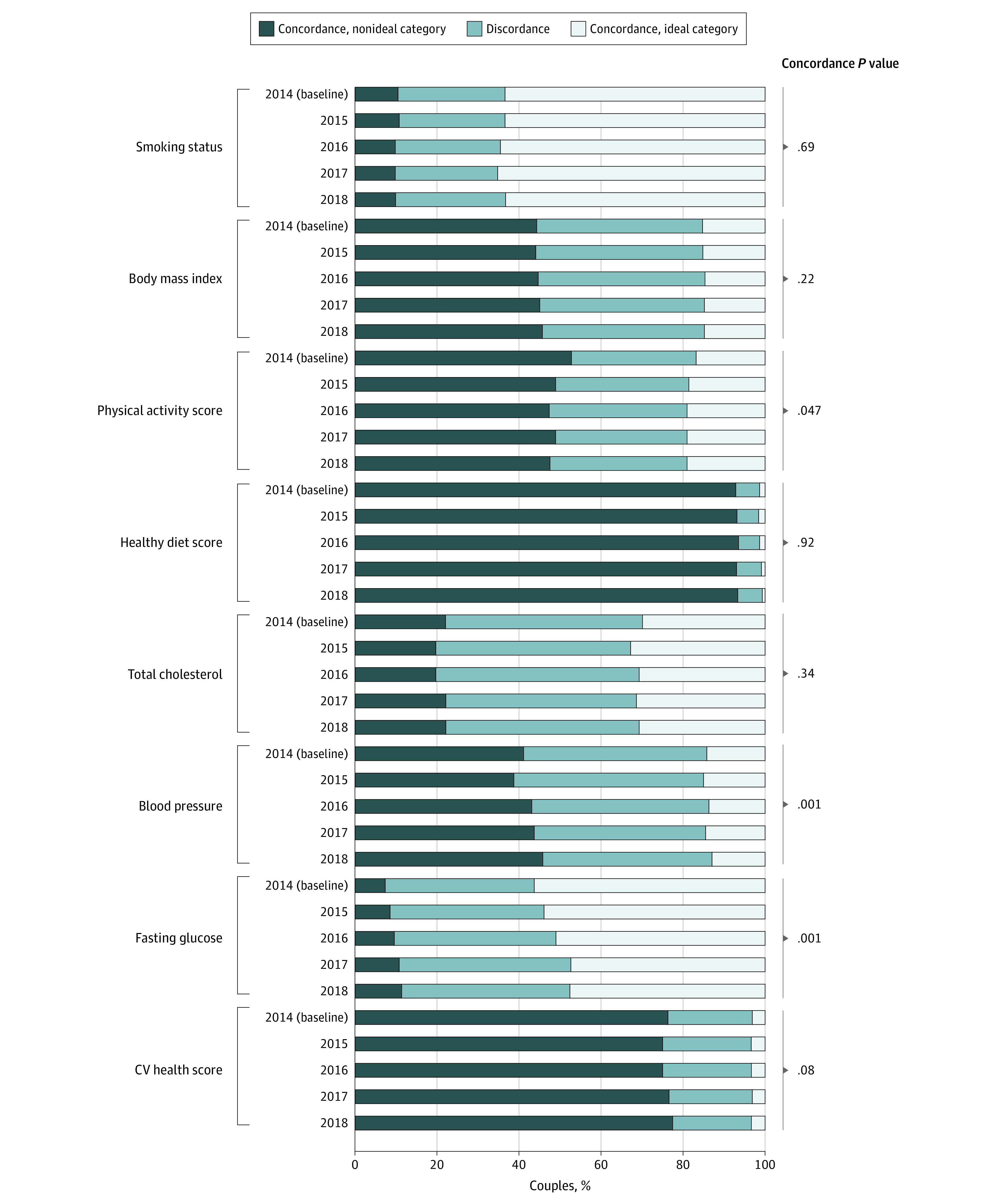
Percent of couples in concordance of each CV risk factor or behavior is indicated for baseline year (2014) and each follow-up year. Couples were considered in concordance of a nonideal category when both were in nonideal categories (dark blue), in concordance of an ideal category when both were in the ideal category (light gray), and in discordance otherwise (gray). P values assess the change in percent of concordant couples (combined ideal and nonideal) over time.
We investigated the association of ethnicity, socioeconomic status, and geographic location with the percent of couples in concordance. Results differed by ethnicity for the percent in concordance of nonideal category for smoking status, BMI, physical activity score, total cholesterol, blood pressure, and CV health score (eFigure 3 in the Supplement), and were similar for diet and fasting glucose. For example, the percent of couple who were both in the nonideal category of BMI varied from a low of 26% in Asian individuals to a high of 68% in African American individuals (P < .001). For total cholesterol, the percent of couples who were both in the nonideal category varied from a low of 13% in African American individuals to a high of 27% among White participants (P < .001). The percent of couples who were both in the nonideal category decreased with higher socioeconomic status (eFigure 4 in the Supplement) for all risk factors and behaviors (P = .002 for glucose, all other P < .001) except for total cholesterol and blood pressure. For example, 68% (95% CI, 59%-77%) of the couples in the lowest socioeconomic status were in the nonideal category of BMI but only 40% (95% CI, 38%-42%) of the couples in the highest socioeconomic status were in the nonideal category. Results by geographic location also varied, with significant differences noted for the percent of couples who were both in the nonideal category of smoking status and BMI. Couples in the Midwest had the highest percent of couples who were both in the nonideal category for smoking (19%; 95% CI, 16%-21%) and BMI (51%; 95% CI, 48%-54%), and couples in the West had the lowest percent of couples who were both in the nonideal category for smoking (10%; 95% CI, 9%-12%) and BMI (42%; 95% CI, 39%-45%) (eFigure 5 in the Supplement).
Discussion
We investigated the concordance of the AHA-defined LS7 risk factors and behaviors within couples among 5364 married or domestic partners in a US nationwide employee health assessment program that was ethnically, socioeconomically, and geographically diverse. We found that within-couple concordance (ie, the percent of couples who were both in an ideal category or both in a nonideal category) was common (>50%) for all LS7 factors as well as the CV health score. Behaviors that affect risk (smoking status, diet, and physical activity) had particularly high concordance (>69%), consistent with a previous study that investigated within-couple concordance of these behaviors.23 A total of 79% of the couples were in the nonideal category for the CV health score, a result associated with lifestyle behaviors. These couples remained in the nonideal category over a 5-year longitudinal analysis.
We were particularly interested in investigating the concordance of nonideal categories (in which both members of the couple were in a nonideal category) because this information could inform public health programs that target couples. High concordance of nonideal categories was observed for BMI (47%), as well as behavioral factors associated with BMI: diet (94%) and physical activity (53%). The high concordance of nonideal diet is consistent with the low fraction of individuals with ideal diet in the study population (3.4%). A 2016 critical review reported that only 4 of 14 studies reported a prevalence greater than 10% and that the remaining studies mostly reported ideal diet in the low single digit percent.24 This high concordance of nonideal categories for factors that are amenable to behavioral interventions suggests that, when possible, interventions targeting these behaviors should be designed to influence both members of the couple. It has also been shown that programs aimed at couples can be more effective in improving risk factors of the targeted individual compared with programs that target only the individual,25,26 perhaps because couple interventions benefit from the inherent social support provided to and by each member of the couple. Thus, since well-designed public health programs intended to promote healthy lifestyles could promote public health by improving CV risk factors and behaviors of both members of a couple as well as dependents in the same household, a potential effect that should be considered when evaluating the cost-effectiveness of public health programs.
A previous study has suggested that 1 member of a couple improving their health-related behavior (eg, starting to exercise) over time is associated with a similar change in the other member of the couple.27 This pattern of correlated behavior change has also been reported to extend to other members an individual’s social network.8,11,12 Therefore, the within-couple concordance of behaviors could be expected to increase over time because couples would have longer opportunity to adopt similar lifestyle. We have found an association between a newly attained ideal status by 1 spouse and the status of the other spouse in the prior year for smoking status, BMI, physical activity, and diet score. However, during the 5 annual examination of this study, a substantial decrease in within-couple discordance was not found. The small (though statistically significant) change found for blood pressure (a modest decrease in discordance) and fasting glucose (a modest increase) does not support the expectation of decreased discordance over time. This lack of decreased discordance might be explained by the relatively short observation time of this study or by the inability to consider the duration of the marriage or domestic partnership at baseline. For example, for many couples, most of the expected couple-driven increase in concordance may have already occurred before the baseline of this study. Alternatively, concordance might be mainly associated with assortative mating, in which case there would be no expectation for an increase in concordance over time.
To explore other factors that might be relevant in the design of public health programs that target couples who are in concordance of nonideal categories, we investigated differences by ethnicity, geographic location, and socioeconomic status. The variation according to ethnicity that we observed in the percent of couples concordant for nonideal categories largely reflected known ethnic variation in CV risk factors and behaviors. For example, lower BMI in Asian individuals compared with White individuals may be associated with the lower percent of those in concordance of nonideal BMI in Asian individuals.28 Similarly, geographic location was associated with concordance of smoking and BMI; this variability was consistent with known geographic variability of obesity and smoking in the US.29,30 As socioeconomic status decreased, a larger percent of the couples was found to be in concordance of nonideal categories for all but 2 of the CV risk factors and behaviors, providing a perspective on the established association between low socioeconomic status and poor CV health.31
Limitations
This study has several limitations. First, the analysis was performed on employees and spouses (or domestic partners) of a single employer. Although the population was ethnically, socioeconomically, and geographically diverse, results may not be generalizable to other populations. Second, we did not have information about the duration of the couple status at baseline and the study was limited to 5 annual health risk assessments. Therefore, drawing firm conclusions about the potential increase in couple similarity over longer duration may not be possible. Moreover, we did not have information about the coresidency status of couples, and thus were unable to analyze the association of coresidency with concordance. Third, diet and exercise data were drawn from questionnaires, which could overestimate desirable diet and exercise patterns because individuals are known to be overoptimistic in self-reporting such traits. Thus, the number of couples who are both in nonideal categories could be even higher than our analysis suggests.
Conclusions
Results of this study suggest the abundance of couples who are both in a nonideal category of CV risk factors and behaviors that are amenable to lifestyle interventions. The variation of within-couple concordance according to ethnicity, geography, and socioeconomic status warrants further investigation, but may have utility in tailoring behavioral intervention programs to reduce CV health disparities. Overall, these observations may help inform public health initiatives that focus on couples-targeted lifestyle modification and may help improve the probability of successful implementation of programs that would benefit both members of a couple.
eMethods.
eTable 1. Correlation and Concordance of Cardiovascular Health Metrics
eTable 2. Baseline Characteristics for Those With vs Without Follow-up
eTable 3. Association of Newly Attained Ideal Status With Other Member Prior Year Ideal Status
eFigure 1. Participant Flow Diagram
eFigure 2. CV Health Metrics Categories in Individual Participants During Follow-up
eFigure 3. CV Health Metrics Concordance by Ethnicity
eFigure 4. CV Health Metrics Concordance by Socioeconomic Status
eFigure 5. CV Health Metrics Concordance by Geographic Location
References
- 1.Chow CK, Lock K, Teo K, Subramanian SV, McKee M, Yusuf S. Environmental and societal influences acting on cardiovascular risk factors and disease at a population level: a review. Int J Epidemiol. 2009;38(6):1580-1594. doi: 10.1093/ije/dyn258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Malambo P, Kengne AP, De Villiers A, Lambert EV, Puoane T. Built environment, selected risk factors and major cardiovascular disease outcomes: a systematic review. PLoS One. 2016;11(11):e0166846. doi: 10.1371/journal.pone.0166846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tada H, Melander O, Louie JZ, et al. Risk prediction by genetic risk scores for coronary heart disease is independent of self-reported family history. Eur Heart J. 2016;37(6):561-567. doi: 10.1093/eurheartj/ehv462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Khera AV, Chaffin M, Aragam KG, et al. Genome-wide polygenic scores for common diseases identify individuals with risk equivalent to monogenic mutations. Nat Genet. 2018;50(9):1219-1224. doi: 10.1038/s41588-018-0183-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ruby JG, Wright KM, Rand KA, et al. Estimates of the heritability of human longevity are substantially inflated due to assortative mating. Genetics. 2018;210(3):1109-1124. doi: 10.1534/genetics.118.301613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cunningham SA, Adams SR, Schmittdiel JA, Ali MK. Incidence of diabetes after a partner’s diagnosis. Prev Med. 2017;105:52-57. doi: 10.1016/j.ypmed.2017.08.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schmittdiel JA, Cunningham SA, Adams SR, Nielsen J, Ali MK. Influence of a new diabetes diagnosis on the health behaviors of the patient’s partner. Ann Fam Med. 2018;16(4):290-295. doi: 10.1370/afm.2259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Christakis NA, Fowler JH. The collective dynamics of smoking in a large social network. N Engl J Med. 2008;358(21):2249-2258. doi: 10.1056/NEJMsa0706154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007;357(4):370-379. doi: 10.1056/NEJMsa066082 [DOI] [PubMed] [Google Scholar]
- 10.Pachucki MC, Lovenheim MF, Harding M. Within-family obesity associations: evaluation of parent, child, and sibling relationships. Am J Prev Med. 2014;47(4):382-391. doi: 10.1016/j.amepre.2014.05.018 [DOI] [PubMed] [Google Scholar]
- 11.Pachucki MA, Jacques PF, Christakis NA. Social network concordance in food choice among spouses, friends, and siblings. Am J Public Health. 2011;101(11):2170-2177. doi: 10.2105/AJPH.2011.300282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Raghavan S, Pachucki MC, Chang Y, et al. Incident type 2 diabetes risk is influenced by obesity and diabetes in social contacts: a social network analysis. J Gen Intern Med. 2016;31(10):1127-1133. doi: 10.1007/s11606-016-3723-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Del Brutto OH, Mera RM. Stroke risk factors in couples. A population-based study in community-dwelling adults living in a remote rural setting (the Atahualpa Project). J Neurol Sci. 2019;398:98-100. doi: 10.1016/j.jns.2019.01.037 [DOI] [PubMed] [Google Scholar]
- 14.Cobb LK, McAdams-DeMarco MA, Gudzune KA, et al. Changes in body mass index and obesity risk in married couples over 25 years: The ARIC Cohort Study. Am J Epidemiol. 2016;183(5):435-443. doi: 10.1093/aje/kwv112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Macken LC, Yates B, Blancher S. Concordance of risk factors in female spouses of male patients with coronary heart disease. J Cardiopulm Rehabil. 2000;20(6):361-368. doi: 10.1097/00008483-200011000-00005 [DOI] [PubMed] [Google Scholar]
- 16.Erqou S, Ajala O, Bambs CE, et al. Ideal cardiovascular health metrics in couples: a community-based study. J Am Heart Assoc. 2018;7(10):e008768. Published online May 4, 2018. doi: 10.1161/JAHA.118.008768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lloyd-Jones DM, Hong Y, Labarthe D, et al. ; American Heart Association Strategic Planning Task Force and Statistics Committee . Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation. 2010;121(4):586-613. doi: 10.1161/CIRCULATIONAHA.109.192703 [DOI] [PubMed] [Google Scholar]
- 18.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative . Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335(7624):806-808. doi: 10.1136/bmj.39335.541782.AD [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139(25):e1082-e1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.US Census Bureau . Census regions and divisions of the United States. Accessed September 30, 2020. https://www2.census.gov/geo/pdfs/maps-data/maps/reference/us_regdiv.pdf
- 21.Berkowitz SA, Traore CY, Singer DE, Atlas SJ. Evaluating area-based socioeconomic status indicators for monitoring disparities within health care systems: results from a primary care network. Health Serv Res. 2015;50(2):398-417. doi: 10.1111/1475-6773.12229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cohen J. Weighted kappa: nominal scale agreement with provision for scaled disagreement or partial credit. Psychol Bull. 1968;70(4):213-220. doi: 10.1037/h0026256 [DOI] [PubMed] [Google Scholar]
- 23.Meyler D, Stimpson JP, Peek MK. Health concordance within couples: a systematic review. Soc Sci Med. 2007;64(11):2297-2310. doi: 10.1016/j.socscimed.2007.02.007 [DOI] [PubMed] [Google Scholar]
- 24.Younus A, Aneni EC, Spatz ES, et al. A systematic review of the prevalence and outcomes of ideal cardiovascular health in US and non-US populations. Mayo Clin Proc. 2016;91(5):649-670. doi: 10.1016/j.mayocp.2016.01.019 [DOI] [PubMed] [Google Scholar]
- 25.Arden-Close E, McGrath N. Health behaviour change interventions for couples: A systematic review. Br J Health Psychol. 2017;22(2):215-237. doi: 10.1111/bjhp.12227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Richards EA, Franks MM, McDonough MH, Porter K. ‘Let’s move:’ a systematic review of spouse-involved interventions to promote physical activity. Int J Health Promot Educ. 2018;56(1):51-67. doi: 10.1080/14635240.2017.1415160 [DOI] [Google Scholar]
- 27.Falba TA, Sindelar JL. Spousal concordance in health behavior change. Health Serv Res. 2008;43(1 Pt 1):96-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fryar CD, Kruszon-Moran D, Gu Q, Ogden CL. Mean body weight, height, waist circumference, and body mass index among adults: United States, 1999-2000 through 2015-2016. Natl Health Stat Report. 2018;(122):1-16. [PubMed] [Google Scholar]
- 29.Centers for Disease Control and Prevention . Current cigarette smoking among adults in the United States. Accessed February 11, 2020. https://www.cdc.gov/tobacco/data_statistics/fact_sheets/adult_data/cig_smoking/index.htm
- 30.Centers for Disease Control and Prevention . Adult obesity prevalence maps. Accessed February 11, 2020. https://www.cdc.gov/obesity/data/prevalence-maps.html
- 31.Clark AM, DesMeules M, Luo W, Duncan AS, Wielgosz A. Socioeconomic status and cardiovascular disease: risks and implications for care. Nat Rev Cardiol. 2009;6(11):712-722. doi: 10.1038/nrcardio.2009.163 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods.
eTable 1. Correlation and Concordance of Cardiovascular Health Metrics
eTable 2. Baseline Characteristics for Those With vs Without Follow-up
eTable 3. Association of Newly Attained Ideal Status With Other Member Prior Year Ideal Status
eFigure 1. Participant Flow Diagram
eFigure 2. CV Health Metrics Categories in Individual Participants During Follow-up
eFigure 3. CV Health Metrics Concordance by Ethnicity
eFigure 4. CV Health Metrics Concordance by Socioeconomic Status
eFigure 5. CV Health Metrics Concordance by Geographic Location