Abstract
A 19‐year‐old female affected by dentinogenesis imperfecta type II (DI‐II), a genetic disease that affects the structural integrity of the dentin, presented with a chief complaint of discolored teeth. For this patient, digital techniques, including digital smile design (DSD), the ARCUSdigma axiograph and computer‐aided design/computer‐aided manufacturing (CAD/CAM), were extensively used in all phases of the rehabilitation process. Compared to traditional analog methods, these digital techniques could reduce the constant confirmation of occlusion, promote communication between clinicians and dental technicians, achieve accurate occlusion with relatively high efficiency, and improve the efficacy of esthetic rehabilitation in the treatment of this patient with DI‐II.
Keywords: Dentinogenesis imperfecta, digital techniques, ARCUSdigma axiograph, CAD/CAM, esthetic rehabilitation
Dentinogenesis imperfecta (DI) is a gene‐related defect that results in irregular dentin structure. Clinically, teeth affected by DI appear gray‐blue and opalescent. The enamel is easily worn and broken, exposing the affected dentin that wears rapidly. Radiographically, teeth present with bulbous crowns and marked cervical constriction. In the initial stages of DI, pulp chambers of the teeth appear abnormally wide, resembling shell teeth, but they undergo progressive obliteration. 1
DI can be broadly classified into 3 types2: type I is a defect accompanied by osteogenesis imperfecta (OI); type II, known as classical hereditary opalescent dentin, is an autosomal dominant genetic disease; and type III is the Brandywine isolate type, which is very rare and found mostly in the United States. 2 , 3 DI‐II has similar clinical and radiographical characteristics to DI‐I but without OI. As the most common subtype with an approximate incidence of 1:8000, 4 DI‐II severely impacts the affected teeth.
In the treatment of DI‐II teeth, routine restorative techniques, including composite restorations and veneers, may be used for patients who do not exhibit enamel fracture or extensive wear. 5 In more severe cases in which patients exhibit extensive wear, full‐coverage crowns are the treatment of choice. For elderly patients or those with extremely worn dentitions, overdentures retained and supported by abutment teeth or dental implants are another restorative option. 6 In general, eliminating pain and restoring esthetics and functions are the goals of treatment. 7 Most of these patients require full‐mouth rehabilitation, which requires precise control of the occlusion at both the provisional and definitive phases. However, it may be difficult to achieve precise occlusion with conventional restorative approaches that are usually time‐consuming and uncomfortable to patients. 8 , 9
Compared to conventional analog methods, dental restoration through a digitalized process is a promising technology. The benefits of digital workflows include improved time efficiency, greater predictability of treatment, a minimally invasive operation with improved functional and esthetic outcomes, and simplified technical production. 10 , 11 The advent of the digital industry has led to a change in the way that dental prostheses are planned, created, and delivered. 12 Smile esthetics are related to the shape, texture, color, and gingival contour of teeth, as well as their relationship with the face. 13 Thus, digital smile design (DSD) is useful for developing an ideal treatment plan that could provide patients with a smile that meets their esthetic requirements. 14 The ARCUSdigma axiograph is a noninvasive diagnostic tool that can measure and record mandibular movement. 15 This device can export and store hinges, condylar paths, kinematic axis locations, and Bennett angles in numerical and graphical formats. 16 CAD/CAM systems are designed to allow the restoration of one or more teeth in the same quadrant at the same time with a precise result. Additionally, digital chairside systems allow clinicians to achieve predictable and repeatable results from anatomical‐functional aspects. 17
Recently, the authors published a clinical report using a multidisciplinary approach integrating orthodontics, periodontics and prosthodontics in the treatment of a patient with DI‐II. 18 However, a rehabilitation method using multiple digital techniques in the workflow, including DSD, the ARCUSdigma axiograph and CAD/CAM, is presented in this new clinical report and has not been reported previously in the treatment of DI‐II patients. The present clinical report aims to demonstrate how to achieve optimal esthetic and functional outcomes using a full digital workflow.
Clinical report
A 19‐year‐old female presented to the Department of Prosthodontics Clinic, Affiliated Stomatology Hospital of Wenzhou Medical University, China. Discolored and unsightly anterior teeth were her chief complaints. A panoramic radiograph (Fig 1) showed narrow, short and bulbous crowns, constricted cementoenamel junctions, obliteration of the pulp chambers and root canals, and roots that were thinner and shorter than those found on normal teeth. She presented with a history of similar tooth discoloration in her cousin who had previously received treatment in our hospital. There was no history of unusual bone brittleness in her family or any other systemic diseases or drug usage in the past. A family history of the previous four generations (Fig 2) also supported a preliminary diagnosis of DI‐II.
Figure 1.

Panoramic radiograph.
Figure 2.
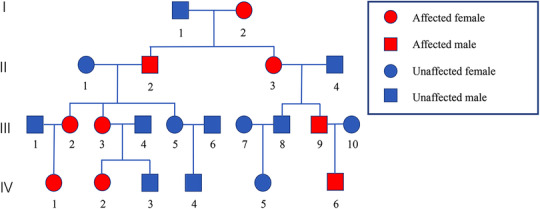
Family pedigree chart. Each branch of the family was recorded separately. The patient was IV‐2.
Preoperative photographs (Fig 3) showed low attachment of the maxillary labial frenum and anterior teeth with morphological defects. The teeth exhibited amber coloration with an opalescent and translucent shine. Some teeth showed wear on the incisal edges and cracks into the dentinal layers. The clinical crowns of the maxillary anterior teeth were shorter than normal. A family medical history covering four generations, in association with the clinical and radiographic manifestations, and a lack of systemic bone disease supported the diagnosis of DI‐II in this patient.
Figure 3.

Preoperative photographs.
The aim of treatment was to use a digital approach to achieve esthetic and functional outcomes of the anterior teeth using full‐coverage crowns. Since the molars only exhibited minimal attrition, they were left untouched during the treatment. Dietary advice and oral hygiene instructions were given to the patient before the treatment, and after the completion of restorative procedures, follow‐up visits were expected twice per year.
The use of a digital software program (Smile Linker; Hengdasheng, Shenzhen, China) provided excellent communication with the patient, and the patient was able to view the designed smile esthetic results before starting treatment (Fig 4). Photographs were taken and uploaded to the software, and rectangles with ovate outlines and suitable length/width ratios were set on the maxillary anterior teeth. The position of the incisal edge followed the smile line of the lower lip, and the color of the teeth was chosen according to the patient's desire. 19 The designed shape and ideal length/width proportion of the teeth as well as the gingival contour were transferred to the dental casts and used to make the diagnostic wax‐up (Fig 5).
Figure 4.
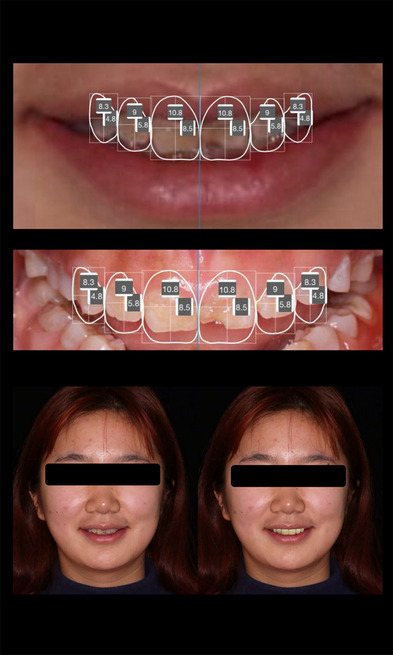
Process of digital smile design.
Figure 5.

Waxed diagnostic casts.
According to the DSD results and the diagnostic wax‐up, crown‐lengthening surgery and maxillary labial frenuloplasty were required on the maxillary anterior sextant due to short clinical crowns and low attachment of the maxillary labial frenum. Apically repositioned flap surgery in association with osseous resection was performed on the maxillary anterior teeth to ensure attachment of the junctional epithelium and connective tissue. After crown‐lengthening surgery, the maxillary anterior sextant was more esthetic with reduced exposure of gingival tissues when smiling. Maxillary labial frenuloplasty was performed due to the low attachment of the maxillary labial frenum, which impacted the esthetics of the maxillary anterior sextant (Fig 6).
Figure 6.

Crown‐lengthening surgery and maxillary labial frenuloplasty.
Three months after periodontal treatment, the ARCUSdigma axiograph (KaVo Dental, Biberach, Germany) was used to obtain personalized mandibular movement, and a KaVo PROTAR articulator report was transferred to the KaVo PROTAR articulator. Based on the exact condylar guidance inclinations and incisal guide angles from the report, new diagnostic wax‐up and transparent laminated film guides were made (Fig 7). Provisional restorations were made with bis‐acrylic resin (3M ESPE Protemp II; 3M ESPE, St. Paul, MN) and the fabricated transparent laminated film guides. Diamond rotary instruments were used to prepare predetermined depths based on the requirements for ceramic crowns. After tooth preparation, the upper and lower casts made by conventional impression techniques were scanned using a laboratory scanner (3Shape D2000; 3Shape, Copenhagen, Denmark). The provisional restorations were then designed using a software program (3Shape Dental System 2019; 3Shape, Copenhagen, Denmark). Subsequently, the designed provisional restorations were produced by a CAD/CAM system (CORiTEC 350i; imes‐icore, Fulda, Germany) and cemented with luting cement (HY‐Bond Glasionomer CX; SHOFU, Kyoto, Japan) (Fig 8).
Figure 7.
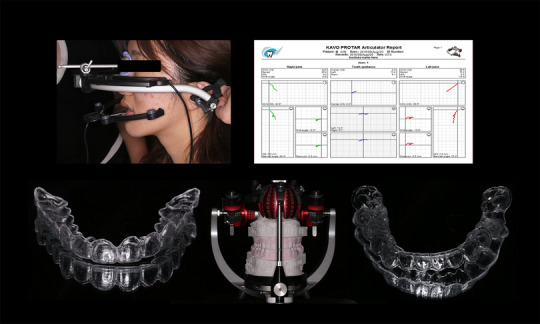
The use of the ARCUSdigma axiograph and the fabricated diagnostic wax‐up with transparent laminated film guides.
Figure 8.
Precise provisional restorations produced by the CORiTEC 350i CAD/CAM system.
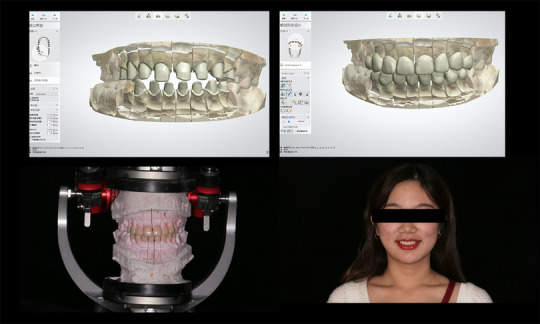
After 5 months using provisional restorations, the occlusion was stable, and the esthetics were approved by the patient. After removing the provisional restorations and cleaning the abutment teeth, chair‐side scanning (CEREC Omnicam; Dentsply Sirona, York, PA) was performed to obtain digital impressions, and technicians designed the definitive restorations (Fig 9A). Subsequently, zirconia ceramic crowns were fabricated by the CORiTEC 350i CAD/CAM system, and veneering porcelain was added for a more natural appearance. 20 The crowns were luted individually following the sequence from mesial to distal using a dual curing resin luting agent (RelyX Unicem; 3M ESPE, St. Paul, MN). Each crown was carefully positioned and light‐cured, and then excess cement was removed. After definitive restorations were delivered, intraoral and facial photographs were taken to document a satisfactory result with dental and gingival morphology as well as canine‐guided occlusion (Fig 9B).
Figure 9.
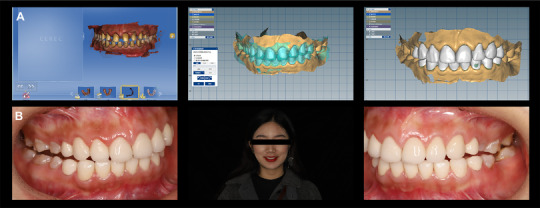
(A) Chair‐side scanning and digital design; (B) intraoral and facial views after definitive restorations were delivered.
At the 6‐month follow‐up visit (Fig 10A), all restorations remained intact. The patient's functional and esthetic outcomes had been achieved, including harmonious dental gingival morphology and stable occlusion. The patient was esthetically pleased and completely satisfied with the results. The clinical follow‐up after 1 year (Fig 10B) revealed good marginal contour, with the exception of a small defect on the edge of the maxillary right lateral incisor, no obvious abnormalities were found on the restorations.
Figure 10.
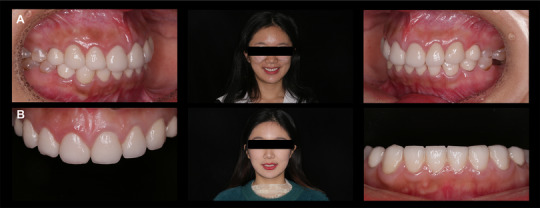
(A) Follow‐up after 6 months; (B) follow‐up after 1 year.
Discussion
Compromised tooth shape and color from DI may have a deleterious impact on a patient's self‐esteem, further affecting their interpersonal relationships and quality of life. 21 In treating DI patients, early identification and diagnosis of the disease are important in order to receive specialty treatment. In this clinical report, the patient was diagnosed with DI‐II rather than DI‐I, which is associated with OI. DI‐II can be specifically diagnosed by its inherited nature, the radiographic and clinical manifestations, and patient history.
Digital design software is an essential tool that has been widely used in the dental rehabilitation of esthetically discerning patients. 22 In this clinical report, Smile Linker, a precise and convenient DSD software used on an iPad, offered a final dental profile showing the relationship between the preoperative situation and the ideal outcomes. Moreover, it also served as a useful guide to fabricate the diagnostic wax‐up and the trial restorations. 23
The ARCUSdigma axiograph, as a computerized axiograph based on the analysis and imaging of the hinge axis and its movement, has been confirmed to have equivalent accuracy to conventional analog devices that have already been accepted by the scientific community. 16 For this patient, with the help of the ARCUSdigma axiograph, precise provisional restorations were fabricated based on the values of the condylar inclinations and the incisal guide angles, which had a significant role in protecting the periodontal tissue, preventing the movement of adjacent teeth, and maintaining esthetics and functions. 24 Additionally, precise vertical and horizontal occlusal dimensions and individual mandibular movements were transferred to the final prostheses.
The advantages of using CAD/CAM technology over conventional methods include speed, an enhanced overall experience for the patient, and the quality of the restorations. 12 , 25 In fabricating crowns, several studies have found that digital and conventional impression techniques have similar marginal fit. 26 , 27 However, as a more time‐efficient technique, digital impressions are more comfortable than conventional methods since the involved techniques are faster and do not provoke nausea. 9 Apart from this, in this clinical report, the provisional and definitive restorations produced by the CAD/CAM systems were precise. No interproximal adjustments were required, and only minor occlusal adjustments were performed.
A combination of periodontal and prosthodontic treatment was also essential to achieve a favorable outcome for this patient. Due to the short clinical crowns, disharmony of the gingival margins, and low attachment of the maxillary labial frenum, crown‐lengthening procedures and maxillary labial frenuloplasty were performed as an adjunct to prosthetic therapy. As the most common surgical procedure in periodontal practice, crown‐lengthening surgery is critical to achieve an esthetic outcome and allows sufficient tooth ferrules for adequate crown retention. 28 Limited by the attached gingiva, gingivectomy to lengthen the clinical crowns was not feasible, so apically repositioned flap surgery and osteotomy were performed. 29
The follow‐up of patients with DI‐II is of considerable importance. In this clinical report, at the 1‐year follow‐up visit, a small defect was found on the edge of the maxillary right lateral incisor. This may have been caused by eating habits according to the patient's description. Therefore, diet control and oral hygiene instructions were emphasized for the patient. The patient is currently under our maintenance care, and long‐term results will be reported in the future.
Summary
This clinical report demonstrates the successful rehabilitation of a DI‐II patient using a series of digital techniques, including DSD, the ARCUSdigma axiograph and CAD/CAM. A prosthodontic/periodontic interdisciplinary approach was also a crucial element in the successful treatment of this patient with DI‐II.
Acknowledgments
The authors thank Dr. Fei Zhu for performing the periodontal treatment, the technicians Zhigang Wang and Yuli Zhu for making the provisional and definitive restorations, and Dr. Xiaoyu Sun for English language editing.
Authors Shi Shi and Ning Li contributed equally to this article.
Supported by the National Natural Science Foundation of China (grants: 81870813); Zhejiang Provincial Science and Technology Project for Public Welfare (grants: 2017C33081); Wenzhou Municipal Science and Technology Project for Public Welfare (grants: Y20170026); Opening Project of State Key Laboratory of Oral Diseases (grants: SKLOD2019OF09)
The authors deny any conflicts of interest in regards to the study.
References
- 1. Andersson K, Malmgren B, Åström E, et al: Dentinogenesis imperfecta type II in Swedish children and adolescents. Orphanet J Rare Dis 2018;13:145‐151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Shields ED, Bixler D, El‐Kafrawy AM: A proposed classification for heritable human dentine defects with a description of a new entity. Arch Oral Biol 1973;18:543‐553 [DOI] [PubMed] [Google Scholar]
- 3. MacDougall M, Dong J, Acevedo AC: Molecular basis of human dentin diseases. Am J Med Genet A 2006;140:2536‐2546 [DOI] [PubMed] [Google Scholar]
- 4. Kim JW, Simmer JP: Hereditary dentin defects. J Dent Res 2007;86:392‐399 [DOI] [PubMed] [Google Scholar]
- 5. Bencharit S, Border MB, Mack CR, et al: Full‐mouth rehabilitation for a patient with dentinogenesis imperfecta: a clinical report. J Oral Implantol 2014;40:593‐600 [DOI] [PubMed] [Google Scholar]
- 6. Binger T, Rucker M, Spitzer WJ: Dentofacial rehabilitation by osteodistraction, augmentation and implantation despite osteogenesis imperfecta. Int J Oral Maxillofac Surg 2006;35:559‐562 [DOI] [PubMed] [Google Scholar]
- 7. Barron MJ, McDonnell ST, Mackie I, et al: Hereditary dentine disorders: dentinogenesis imperfecta and dentine dysplasia. Orphanet J Rare Dis 2008;3:31‐40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Berrendero S, Salido MP, Ferreiroa A, et al: Comparative study of all‐ceramic crowns obtained from conventional and digital impressions: clinical findings. Clin Oral Investig 2019;23:1745‐1751 [DOI] [PubMed] [Google Scholar]
- 9. Yuzbasioglu E, Kurt H, Turunc R, et al: Comparison of digital and conventional impression techniques: evaluation of patients' perception, treatment comfort, effectiveness and clinical outcomes. BMC Oral Health 2014;14:10‐16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. van Noort Richard: The future of dental devices is digital. Dent Mater 2012;28:3‐12 [DOI] [PubMed] [Google Scholar]
- 11. Joda T Brägger U: Time‐efficiency analysis comparing digital and conventional workflows for implant crowns: a prospective clinical crossover trial. Int J Oral Maxillofac Implants 2015;30:1047‐1053 [DOI] [PubMed] [Google Scholar]
- 12. Guichet DL: Digital workflows in the management of the esthetically discriminating patient. Dent Clin North Am 2019;63:331‐344 [DOI] [PubMed] [Google Scholar]
- 13. Cervino G, Fiorillo L, Arzukanyan AV, et al: Dental restorative digital workflow: digital smile design from aesthetic to function. Dent J (Basel) 2019;7:30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Coachman C, Paravina RD: Digitally enhanced esthetic dentistry‐from treatment planning to quality control. J Esthet Restor Dent 2016;28:3‐4 [DOI] [PubMed] [Google Scholar]
- 15. Kobs G, Didziulyte A, Kirlys R, et al: Reliability of ARCUSdigma (KaVo) in diagnosing temporomandibular joint pathology. Stomatologija 2007;9:47‐55 [PubMed] [Google Scholar]
- 16. Wieckiewicz M, Zietek M, Nowakowska D, et al: Comparison of selected kinematic facebows applied to mandibular tracing. Biomed Res Int 2014;2014:818694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Saratti CM, Del Curto F, Rocca GT, et al: Vertical dimension augmentation with a full digital approach: a multiple chairside sessions case report. Int J Comput Dent 2017;20:423‐438 [PubMed] [Google Scholar]
- 18. Fan F, Li N, Huang S, et al: A multidisciplinary approach to the functional and esthetic rehabilitation of dentinogenesis imperfecta type II: a clinical report. J Prosthet Dent 2019;122:95‐103 [DOI] [PubMed] [Google Scholar]
- 19. Meereis CT, de Souza GB, Albino LG, et al: Digital smile design for computer‐assisted esthetic rehabilitation: two‐year follow‐up. Oper Dent 2016;41:13‐22 [DOI] [PubMed] [Google Scholar]
- 20. Tabatabaian F: Color in zirconia‐based restorations and related factors: a literature review. J Prosthodont 2018;27:201‐211 [DOI] [PubMed] [Google Scholar]
- 21. Beltrame AP, Rosa MM, Noschang RA, et al: Early rehabilitation of incisors with dentinogenesis imperfecta type II: a case report. J Clin Pediatr Dent 2017;41:112‐115 [DOI] [PubMed] [Google Scholar]
- 22. Silva BP, Mahn E, Stanley K, et al: The facial flow concept: An organic orofacial analysis‐the vertical component. J Prosthet Dent 2019;121:189‐194 [DOI] [PubMed] [Google Scholar]
- 23. Trushkowsky R, Arias DM, David S: Digital smile design concept delineates the final potential result of crown lengthening and porcelain veneers to correct a gummy smile. Int J Esthet Dent 2016;11:338‐354 [PubMed] [Google Scholar]
- 24. Alt V, Hannig M, Wostmann B, et al: Fracture strength of temporary fixed partial dentures: CAD/CAM versus directly fabricated restorations. Dent Mater 2011;27:339‐347 [DOI] [PubMed] [Google Scholar]
- 25. Beuer F, Schweiger J, Edelhoff D: Digital dentistry: an overview of recent developments for CAD/CAM generated restorations. Br Dent J 2008;204:505‐511 [DOI] [PubMed] [Google Scholar]
- 26. Abdel‐Azim T, Rogers K, Elathamna E, et al: Comparison of the marginal fit of lithium disilicate crowns fabricated with CAD/CAM technology by using conventional impressions and two intraoral digital scanners. J Prosthet Dent 2015;114:554‐559 [DOI] [PubMed] [Google Scholar]
- 27. Nagarkar SR, Perdigão J, Seong W‐J, et al: Digital versus conventional impressions for full‐coverage restorations. A systematic review and meta‐analysis. J Amer Dent Assoc 2018;149:139‐147 [DOI] [PubMed] [Google Scholar]
- 28. Kalsi HJ, Bomfim DI, Hussain Z, et al: Crown lengthening surgery: an overview. Prim Dent J 2020;8:48‐53 [DOI] [PubMed] [Google Scholar]
- 29. Marzadori M, Stefanini M, Sangiorgi M, et al: Crown lengthening and restorative procedures in the esthetic zone. Periodontol 2000 2018;77:84‐92 [DOI] [PubMed] [Google Scholar]


