Abstract
Aim:
To document how changes in the hospital work environment and nurse staffing over time are associated with changes in missed nursing care.
Background:
Missed nursing care is considered an indicator of poorer care quality and has been associated with worse patient care experiences and health outcomes. Several systematic reviews of cross-sectional studies report that nurses in hospitals with supportive work environments and higher staffing miss less care. Causal evidence demonstrating these relationships is needed.
Methods:
This panel study utilized secondary data from 23,650 nurses surveyed in 2006 and 14,935 surveyed in 2016 in 458 hospitals from a four-state survey of random samples of licensed nurses.
Results:
Over the 10-year period, most hospitals exhibited improved work environments, better nurse staffing and more missed care. In hospitals with improved work environments or nurse staffing, the prevalence and frequency of missed care decreased significantly. The effect on missed care of changes in the work environment was greater than that of nurse staffing.
Conclusions:
Changes in the hospital work environment and staffing influence missed care.
Implications for Nursing Management:
Modifications in the work environment and staffing are strategies to mitigate care compromise. Nurse managers should investigate work settings in order to identify weaknesses.
Keywords: missed nursing care, nurse staffing, work environment
1 |. INTRODUCTION
Over the past decade, missed nursing care has been studied extensively as a reflection of nursing care quality. Five systematic reviews (Griffiths et al., 2018; Jones, Hamilton, & Murry, 2015; Kalisch & Xie, 2014; Papastavrou, Andreou, & Efstathiou, 2014; Recio-Saucedo et al., 2017; Zhao et al., 2019) have documented the predictors and consequences of missed nursing care. These reviews identify the common organisational determinants of missed care to be the work environment and staffing. Supportive work environments and adequate staffing are linked to less missed care. The evidence base has been limited to cross-sectional studies, from which causality cannot be inferred. Without causal associations between organisational change and missed care, hospital managers lack empirical evidence that such changes are warranted and productive. The following panel study presents an innovative longitudinal design that permits causal inference. This study evaluates how organisational change over a 10-year period yields changes in missed care. This evaluation substantially contributes to the existing literature by providing resounding evidence to persuade hospital administrators to intervene with the aim of improving quality.
2 |. BACKGROUND
Missed care is defined as any aspect of required patient care that is omitted or significantly delayed (Kalisch, Landstrom, & Hinshaw, 2009). Missed nursing care is conceptualized as a process measure that is directly related to patient outcomes and the quality of care (Kalisch, Tschannen, Lee, & Friese, 2011; VanFosson, Jones, & Yoder, 2016). Empirical attention to missed care has been growing over the past decade in part because of the lack of process measures and the implications for care quality.
Missed care is common, and the types of care that are missed are consistent across populations. Between 55 and 98% of nurse respondents report missing at least one required care activity during the time of assessment (Griffiths et al., 2018; Jones et al., 2015). Nurses most often miss care activities related to emotional and psychological needs, rather than physiological needs (Jones et al., 2015). This is reiterated by a nurse in B. J. Kalisch (2006)’s study: ‘We have to give them meds to keep them alive, we have to make sure they can breathe, and we have to keep the heart going. Things after that get missed’ (p. 307). Determinants of missed care include a lack of time, training, resources and staffing (Griffiths et al., 2018; Papastavrou et al., 2014). The consequences of missed care include decreased patient satisfaction, increased medication errors, urinary tract infections, patient falls, pressure ulcers, critical incidents, quality of care and patient readmissions (Recio-Saucedo et al., 2017).
Care processes such as missed care are central to Donabedian’s framework of quality assessment, which theorizes that quality outcomes are derived from structures and processes. In this study, we theorize that the organisational structures of nurse staffing and the hospital work environment influence missed nursing care. The nurse work environment is defined as the ‘organisational characteristics of a work setting that facilitate or constrain professional nursing practice’ (Lake, 2002). The organisational support for professional nursing practice includes modifiable traits such as supportive frontline managers, adequate resources, foundations for quality care, nurse participation in organisational decision-making and collaborative relationships with physicians (Aiken, Clarke, & Sloane, 2002; Lake, 2002). The nurse work environment explains a significant amount of variation in missed care (Ausserhofer et al., 2014).
Nurse staffing levels predict both the likelihood that a nurse misses care as well as the amount of care missed (Ausserhofer et al., 2014; Ball, Murrells, Rafferty, Morrow, & Griffiths, 2014; Cho, Kim, Yeon, You, & Lee, 2015; Kalisch et al., 2011). Missed care may be a key mechanism by which insufficient staffing influences care processes and subsequent patient outcomes (Needleman, 2016). Indeed, mediation analysis has shown that missed care explains the association between nurse staffing and patient care experience (Bruyneel et al., 2015) and mortality (Ball et al., 2018).
Huber, Sutcliffe, Miller, and Glick (1993) defined organisational change as ‘change that involves differences in how an organisation function, who its members and leaders are, what form it takes, and how it allocates resources.’ The organisational context of health care is constantly evolving, but the nature and extent of such changes are rarely documented. Longitudinal changes in organisational features such as the nurse work environment have been shown to influence the rate of nurse burnout, intention to leave one’s current position and job dissatisfaction (Kutney-Lee, Wu, Sloane, & Aiken, 2013). Similarly, longitudinal changes in nurse staffing have been shown to influence fall and pressure ulcer rates (He, Staggs, Bergquist-Beringer, & Dunton, 2016) as well as other outcomes (Shekelle, 2013). Missed care, however, has not been evaluated. Focusing on missed care in relation to organisational change is an important extension as improvements in the work environment are one potential strategy to reduce care omissions and improve patient outcomes (Brooks-Carthon, Lasater, Rearden, Holland, & Sloane, 2016). The missed care literature is lacking evidence providing a definitive connection between organisational change and missed nursing care. The purpose of this longitudinal study is to demonstrate how changes in nursing organisational factors, namely staffing and the work environment, influence the prevalence and frequency of missed nursing care.
3 |. METHODS
3.1 |. Design and data
This was a two-period panel study of a cohort of hospitals in four large US states in which nurses were surveyed ten years apart. All measures were aggregated to the hospital level to evaluate change as the samples of nurses in the two years were not necessarily identical. The data were derived from two large-scale surveys on nursing care and patient safety of nurses in California, Florida, New Jersey and Pennsylvania during 2006 and 2016. We refer to the years 2006 and 2016; however, states were surveyed sequentially across the period 2005–2008 (Aiken et al., 2011) and similarly in 2016 (Lasater et al., 2019). The surveys were conducted by mailing questionnaires, return envelopes and reminder postcards to the homes of randomly sampled nurses from the four-state licensure lists. Questionnaires were mailed to 273,000 nurses in 2006 and to 231,000 nurses in 2016. The surveys yielded response rates of 39% and 26%, respectively. The questionnaire requested that nurses who are currently working at a hospital indicate the hospital from a list of all the hospitals in their state. This allowed for the linkage of survey respondents to specific hospitals from the American Hospital Association (AHA) Annual Survey data. This linkage enabled the creation of a cross-year observation for each hospital. Information was obtained from a common set of 737 hospitals in both survey years. For the current study, hospitals with at least 10 respondents in both years were included to achieve stable hospital-level measures (McHugh & Stimpfel, 2012).
3.2 |. Measures
These analyses focus on longitudinal associations of two nursing organisational features with two missed care variables. The two nurse organisational features are the work environment and staffing. These nursing features have been used as independent variables in previous studies and reflect core nursing organisational factors (Aiken et al., 2011, 2002, 2014; Aiken, Clarke, Sloane, Lake, & Cheney, 2008; Sloane, Smith, McHugh, & Aiken, 2018). All variables were measured at the hospital level.
3.2.1 |. Nurse work environment
The nurse work environment was measured at the hospital level using a composite measure of the 31-item Practice Environment Scale of the Nurse Work Index (PES-NWI) (Lake, 2002), a National Quality Forum-endorsed nursing performance measure (National Quality Forum, 2017). Nurses indicated the extent to which they agree that each of the following features is present in their primary job. The four response categories were strongly disagree (1), somewhat disagree (2), somewhat agree (3) and strongly agree (4). There are 31 items in five subscales.
3.2.2 |. Nurse staffing
Nurse staffing was measured by asking each nurse, ‘How many patients were assigned to you on your last shift?’ An average was computed across all nurses in each hospital.
3.2.3 |. Missed care
Missed care was measured using the survey question ‘On the most recent shift/day you worked, which of the following activities were necessary but left undone because of time constraints?’ This question was developed in order to capture the fourteen essential nursing care activities. This missed care question has been used in five international samples (Aiken et al., 2012; Al-Kandari & Thomas, 2009; Ausserhofer et al., 2014; Ball et al., 2014; Zhu et al., 2012).
The first missed care variable ‘any missed care’ represents the proportion of nurses who missed at least one care activity. The second missed care variable, ‘Total missed care activities,’ is the summed average of missed care activities for each nurse. Hospital-level change variables for missed care, the work environment and staffing were created by subtracting the value 2016 from the value in 2006. The changes for the key variables were divided into terciles representing the top, middle and bottom categories to classify hospitals into greater and lesser degrees of change based on the sample change distribution.
3.2.4 |. Hospital characteristics
Hospital characteristics were derived from the 2015 AHA Annual Survey data. These characteristics were used to describe the sample and as control variables. Bed size was classified into three categories: small, medium and large. Teaching status was based on the medical resident-to-bed ratio and categorized into major, minor and none. High-technology status was classified by the hospital’s capacity for open-heart surgery or major organ transplants. Hospital ownership was categorized as public, for-profit and not-for-profit.
3.3 |. Analysis
Descriptive statistics were used to describe the hospitals, nursing organisational features and missed care. Linear regression models were used to estimate the changes in the two missed care variables. The independent variables, work environment and staffing, were specified as dummy variables for the top and middle terciles (reference category was the bottom tercile). The regression coefficients indicate the change in the dependent variable given a hospital is in the top (or middle) versus the bottom tercile. Adjusted models included hospital characteristics (bed size, ownership, teaching status, nurse unit composition and technology capability), as they may impact changes in these key variables. Statistical significance was set at p < .05 for a two-tailed test. Analyses were conducted using STATA version 15.1.
4 |. RESULTS
The nurse respondent inclusion criteria yielded a sample of 23,650 nurses in 2006 and 14,935 in 2016 in a total of 458 hospitals (Table 1). The typical hospital was a not-for-profit hospital with a bed size of greater than 300 beds. The fractions of hospitals with teaching commitment and meeting high-technology criteria increased from about half in 2006 to 59% in 2016.
TABLE 1.
Characteristics of the hospital samples in 2006–2016
| Variable | Percent (n = 458) in 2006 | Percent (n = 458) in 2016 |
|---|---|---|
| Hospital state | ||
| California | 40 (181) | 40 (181) |
| Florida | 27 (125) | 27 (125) |
| New Jersey | 11 (51) | 11 (51) |
| Pennsylvania | 22 (101) | 22 (101) |
| Technology status | ||
| Low | 49 (225) | 41 (190) |
| High | 51 (233) | 59 (268) |
| Teaching status | ||
| None | 50 (228) | 41 (189) |
| Minor | 41 (189) | 48 (218) |
| Major | 9 (41) | 11 (51) |
| Bed size | ||
| 0–199 | 32 (146) | 27 (125) |
| 200–299 | 29 (133) | 28 (126) |
| 300+ | 39 (179) | 45 (207) |
| Ownership | ||
| Not-for-profit | 74 (337) | 70 (322) |
| For-profit | 16 (75) | 20 (90) |
| Public | 10 (46) | 10 (46) |
Table 2 displays descriptive characteristics on missed care, the work environment and staffing in 2006 and 2016. Overall, missed care increased over the period. The percent of nurses missing one or more activities increased from 67% to 75%. In 2006 SD units, this was equivalent to a 0.8 SD increase. The 2006 SD is used as a measure of change across the two time points. The total missed nursing care activities increased from 2.38 to 2.56, a 0.28 SD increase. Additionally, there was an increase in the nurse-reported work environment composite score, from 2.70 to 2.77, a 0.32 SD change. Lastly, the number of patients assigned per nurse decreased from 4.89 to 4.74, a 0.16 SD change. Figures 1 and 2 are histograms depicting the numbers of hospitals that had certain increases and decreases in the key variables from 2006 to 2016. Here, the modal change in the work environment was a 0.10 increase in the PES-NWI composite, evident for 82 hospitals (18% of the sample). The modal change for nurse staffing was a decrease of between 0.10 and 0.20 patients per nurse, evident for 50 hospitals (11% of the hospitals). As per Figure 2, the modal change in missed care prevalence was a 10% increase, evident for 135 hospitals (30%). Similarly, the modal change in total missed care activities was 0.20 increase, noted in 33 hospitals (7%).
TABLE 2.
Descriptive statistics on missed care, the work environment and staffing, 2006–2016
| Variable | Survey question | Variable measurement | Mean (SD) in 2006 | Mean (SD) in 2016 |
|---|---|---|---|---|
| Any missed nursing care | On the most recent shift/day you worked, which of the following activities were necessary but left undone because of time constraints? (Mark all that apply) | Percent of nurses who reported missing one or more activities | 0.67 (0.10) | 0.75 (0.12) |
| Total missed nursing care activities | Adequate patient surveillance | Sum of activities missed | 2.38 (0.64) | 2.56 (0.70) |
| Oral hygiene/mouth care | ||||
| Comfort/talk with patients | ||||
| Adequately document nursing care | ||||
| Administer medications on time | ||||
| Treatments and procedures | ||||
| Prepare patients and families for discharge | ||||
| Develop or update patient plan of care | ||||
| Skincare | ||||
| Pain management | ||||
| Teach/counsel patients and family | ||||
| Coordinate patient care | ||||
| Nurse work environment | Please indicate the extent to which you agree that each of the following features is present in your primary job. The four response categories were strongly disagree (1), somewhat disagree (2), somewhat agree (3) and strongly agree (4). There are 31 items in five subscales | Composite score of the Practice Environment Scale of the Nursing Work Index (PES-NWI) calculated as the mean of the five subscale scores | 2.70 (0.22) | 2.77 (0.25) |
| Nurse staffing | How many patients were assigned to you on your last shift? | Number of patients | 4.89 (0.96) | 4.74 (0.87) |
Note: All measures are at the hospital level (n = 458 hospitals).
Abbreviation: SD, standard deviation.
FIGURE 1.
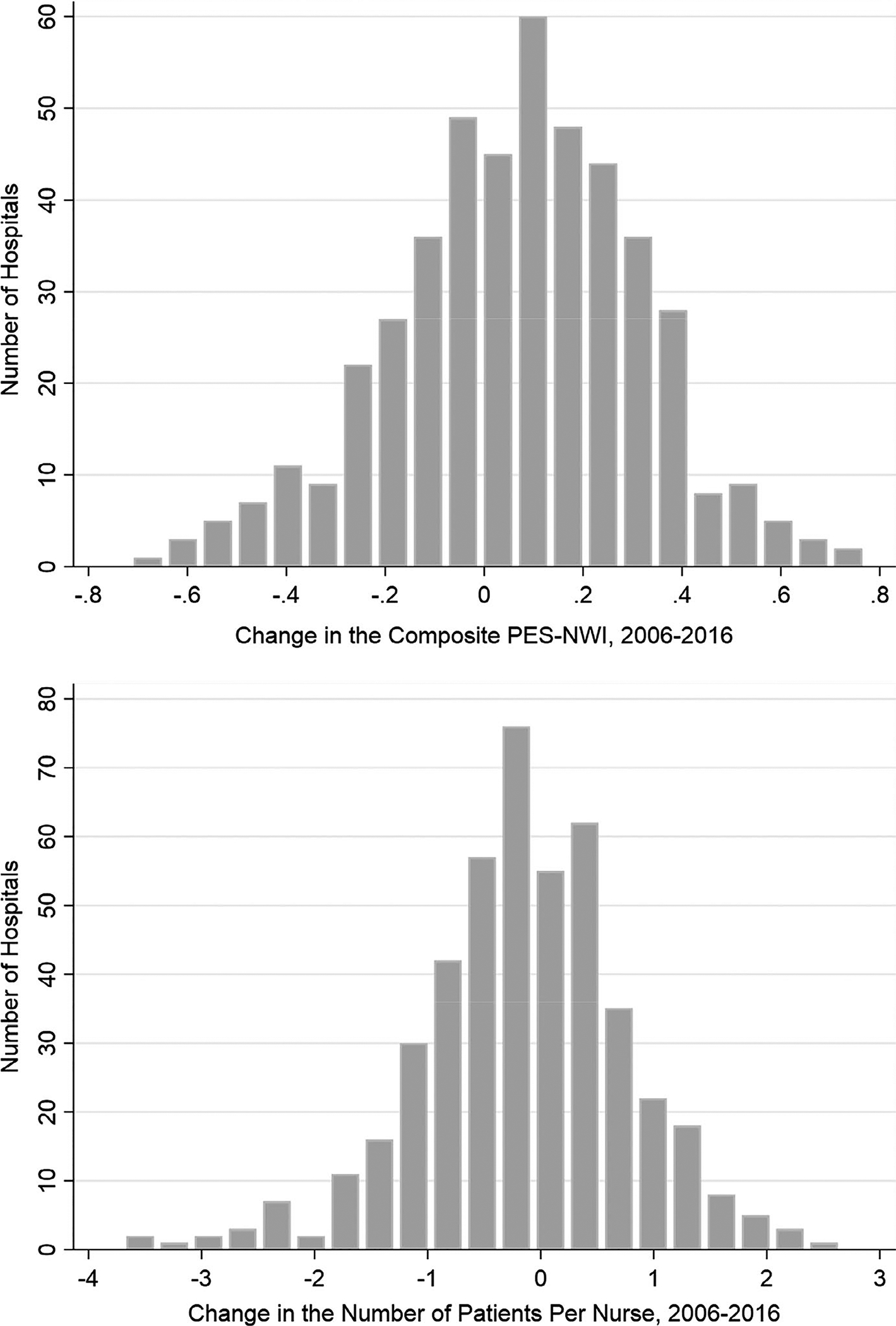
Change in nurse work environment and staffing, 2006–2016
FIGURE 2.
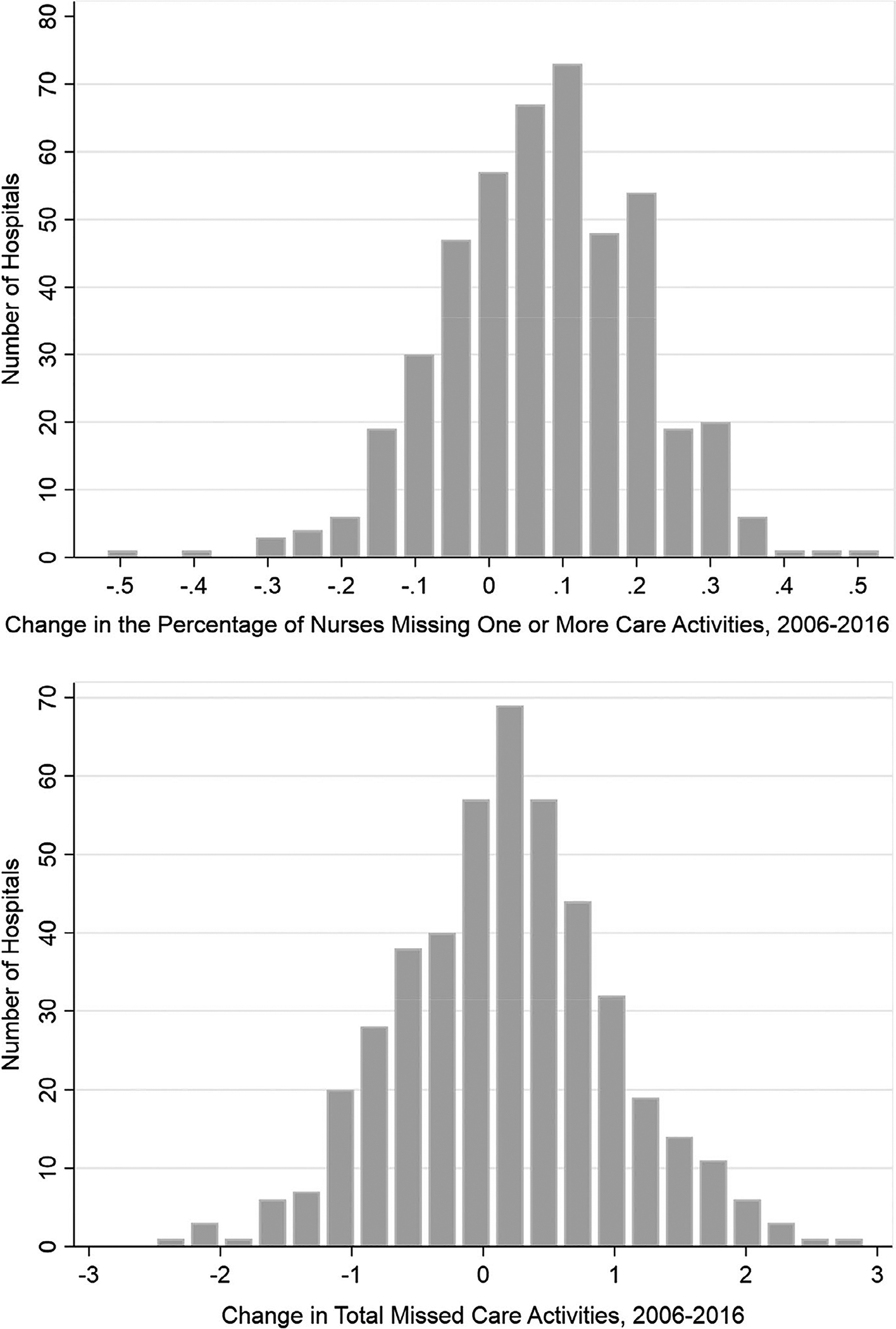
Change in missed care, 2006–2016
Results of the unadjusted and adjusted models regressing missed care on the two nursing organisational features are shown in Table 3. The unadjusted and adjusted model results were quite similar; only the latter are described in text. As compared to hospitals with worsened work environments in 2016, in hospitals with improved (or stable) work environments, 11% (or 6%) fewer nurses missed care in 2016 (p < .001). Similarly, in hospitals with poorer staffing in 2016, 5% fewer nurses missed care in 2016 (p < .01). For total missed care activities, in hospitals with improved (or stable) work environments, 0.86 (or 0.55) fewer care activities were missed in 2016 (p < .001). Similarly, in hospitals with poorer staffing in 2016, 0.32 more care activities were missed in 2016 (p < .001). An improved work environment reduced missed care prevalence by one SD, relative to the 2006 SD, and reduced total missed care by 1.3 SDs. For comparison, improved nurse staffing yielded relatively smaller effects; that is, it reduced missed care prevalence by 0.5 SD and total missed care activities by 0.5 SDs.
TABLE 3.
Linear regression results
| Unadjusted Model 1: difference in missed any nursing care (n = 458 hospitals) | Adjusted Model 1: difference in missed any nursing care (n = 458 hospitals) | Unadjusted Model 2: difference in total missed care activities (n = 458 hospitals) | Adjusted Model 2: difference in total missed care activities (n = 458 hospitals) | |
|---|---|---|---|---|
| Nursing resource | Coefficient (SE) | Coefficient (SE) | ||
| Nurse work environment | ||||
| Stable | −0.06 (0.01)*** | −0.06 (0.01)*** | −0.57 (0.08)*** | −0.55 (0.08)*** |
| Improved | −0.11 (0.01)*** | −0.11 (0.02)*** | −0.88 (0.08)*** | −0.86 (0.09)*** |
| Nurse staffing | ||||
| Stable | −0.02 (0.01) | −0.02 (0.02) | −0.16 (0.08) | −0.17 (0.09) |
| Improved | −0.04 (0.01)** | −0.05 (0.02)** | 0.28 (0.08)** | −0.32 (0.09)*** |
Note: For the two variables ‘Missing Any Nursing Care’ and ‘Total Missed Care Activities,’ the reference group is the ‘Worsened’ subgroup of hospitals. Models controlled for hospital characteristics (bed size, technology status, teaching status, ownership and medical–surgical and intensive care unit nurse composition). The independent variables, nurse work environment and nurse staffing are hospital level. The dependent variables for missed nursing care are at the hospital level. Pseudo-R2 for adjusted model 1 = 0.1372 and adjusted model 2 = 0.2366. Results were considered statistically significant at p < .05 for a two-tailed test.
Abbreviations: CI, confidence interval; OR, odds ratio.
p < .05;
p < .01;
p < .001.
5 |. DISCUSSION
This study was motivated by the absence of empirical evidence demonstrating whether changes in nursing organisational factors influence care processes. Research on nursing organisational factors and their association with quality and safety of care and health outcomes now spans three decades, yet only a handful of studies have utilized a longitudinal approach. This weakness in the field limits the impact of the results. The current study demonstrates clearly that organisational improvements in nursing result in less nursing care compromises. Plentiful evidence linking missed nursing care to poor patient health and nurse job outcomes invites solutions to reduce missed care. Herein, we show that both the prevalence of nurses who miss care and the frequency of care missed lowered in hospitals that improved their work environments and staffing over the period 2006–2016. Hospitals in the four states represented in the sample account for one-fifth of annual hospitalizations nationally. This paper offers modifiable features of the organisation as candidates for managerial and executive attention.
Over the 10-year period studied, changes in the key variables exhibited notable trends. Both work environment and staffing improved in most hospitals, as shown in the figures. The extent of change was sizable: most (i.e. the modal value) hospitals changed (i.e. improved) the equivalent of one SD over the decade in their PES-NWI composite score (in 2006 SD), and one-third of an SD reduction in patients per nurse. Surprisingly, the trend towards improving work environments and staffing was accompanied by an increase in the frequency of missed care in most hospitals. The modal change in missed care reflected a one SD (in 2006 metric) increase in prevalence as well as a one-third SD increase in total missed care activities.
Our results demonstrated that among hospitals with notable improvements over a decade in their work environments or staffing levels, missed care prevalence and frequency reduced significantly. We defined notable improvement as the top tercile of the change distribution for our independent variables. A typical change in the improved tercile for work environment, a 0.33 increase in the composite score, resulted in an 11% reduction in missed care prevalence and a 0.86 reduction in missed care frequency. These reductions are sizable, equivalent to a one SD change in prevalence and a 1.3 SD change in frequency (based on the 2006 SD value). A typical change in the improved tercile of the change distribution for staffing, a reduction of 1.14 patients per nurse, resulted in a 5% reduction in missed care prevalence and a 0.32 reduction in missed care frequency. These reductions are equivalent to one-half SD reduction in missed care prevalence and frequency. Thus, notable improvement in the work environment yielded larger reductions in missed care than did notable improvement in staffing.
Similar effects of nursing system changes on nurse and patient outcomes have been observed in the few studies with a longitudinal design. Kutney-Lee et al. (2013) observed in a sample of 137 Pennsylvania hospitals over a 7-year period from 1999 to 2006 that in improved work environments, fewer nurses reported negative job outcomes such as burnout, intention to leave and job dissatisfaction. In that same sample, achieving Magnet recognition, a designation for excellence in nursing standards, was accompanied by improvement in the work environment. In hospitals that achieved Magnet status, patient outcomes were improved, including lower rates of surgical mortality and failure to rescue compared to non-Magnets (Kutney-Lee et al., 2015).
Regarding nurse staffing, studies of outcomes in hospitals exhibited comparable effects to this study. In 283 California general acute care hospitals from 1996 to 2001, changes in nurse staffing were associated with reductions in mortality and failure to rescue (Harless & Mark, 2010). This same relationship was observed in 39 Michigan hospitals from 2003 to 2006. An increased level of nurse staffing was associated with a decrease in the absolute risk of mortality by 0.25 percentage points for each additional full-time equivalent nurse per patient-day (Schilling, Campbell, Englesbe, & Davis, 2010). Finally, the results from our longitudinal study of how changes in the work environment and nurse staffing influence missed care corroborate results from numerous cross-sectional studies (Griffiths et al., 2018; Jones et al., 2015; Lake, Staiger, Edwards, Smith, & Rogowski, 2018; Papastavrou et al., 2014; Zhao et al., 2019).
Several limitations to this study need to be acknowledged. The change was measured at two time points separated by ten years. The pace of change within a decade, including potential improvement and worsening for key variables, was not available in these data. Classifying change as improvement or worsening could be done a variety of ways. We chose terciles for ease of interpretation. Further research studies are needed to better understand how to clarify organisational change at the hospital level.
6 |. CONCLUSION
Motivated by a long-standing limitation in the field of nursing system research, this study utilized a longitudinal design to study how changes in core organisational dimensions of hospital nursing yield theorized changes in nursing care processes. Nursing processes were operationalized as missed nursing care. Consistent with the cross-sectional literature, changes in these modifiable dimensions, that is nurse staffing and a supportive work environment, were associated with anticipated changes in the prevalence and frequency of missed care in a large, geographically diverse panel of hospitals. Modifications in staffing and the work environment are potential strategies to remedy care compromise.
7 |. IMPLICATIONS FOR NURSING MANAGEMENT
Nurse managers are in an ideal position to offer solutions to reduce missed care. This study provides the nurse manager with actionable solutions to mitigate missed care. Nurse managers can survey their staff to identify problematic domains in their work environment. Two systematic reviews (Swiger et al., 2017; Warshawsky & Havens, 2010) report values for the PES-NWI subscales and composite from multiple studies. Hospital administrators may consider voluntary participation in the National Database of Nursing Quality Indicators, which provides peer benchmark values on the PES-NWI measures through a nurse survey for all participating nursing units. Some hospitals have utilized nurse survey results on the Nurse Manager subscale to identify high-performing managers who can share best practices throughout the institution (Anderson, Manno, O’Connor, & Gallagher, 2010).
Managers can assess their staffing adequacy through several approaches. One source is the PES-NWI subscale, Staffing and Resource Adequacy. Values below 2.5 on this or any subscale indicate an inadequately resourced setting (Lake, 2002). Alternatively, NDNQI provides peer benchmarks at the unit level for comparison (Montalvo, 2007). Several states have mandated public reporting of unit-level staffing to provide transparency regarding available nursing resources (de Cordova, Rogowski, Riman, & McHugh, 2019). The results of this study can be employed to develop targeted interventions aimed at reduced missing care in the hospital setting.
ACKNOWLEDGEMENTS
Research for this article was conducted at the Center for Health and Policy Research, University of Pennsylvania School of Nursing, Philadelphia, PA. The authors are thankful to Dr. Douglas Sloane for his advice on methodology.
Funding information
This study was supported by grants from the National Institute of Nursing Research (T32-NR-007104 and R01-NR-014855, to L.H. Aiken, principal investigator). Equipment is not applicable to this project.
Footnotes
ETHICAL APPROVAL
Institutional Review Board approval was obtained from the principal investigator’s institution.
REFERENCES
- Aiken LH, Cimiotti JP, Sloane DM, Smith HL, Flynn L, & Neff DF (2011). Effects of nurse staffing and nurse education on patient deaths in hospitals with different nurse work environments. Medical Care, 49(12), 1047–1053. 10.1097/MLR.0b013e3182330b6e [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken LH, Clarke SP, & Sloane D (2002). Hospital staffing, organization, and quality of care: Cross-national findings. International Journal for Quality in Health Care, 14(1), 5–13. 10.1093/intqhc/14.1.5 [DOI] [PubMed] [Google Scholar]
- Aiken LH, Clarke SP, Sloane DM, Lake ET, & Cheney T (2008). Effects of hospital care environment on patient mortality and nurse outcomes. Journal of Nursing Administration, 38(5), 223–229. 10.1097/01.NNA.0000312773.42352.d7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken LH, Sermeus W, Van den Heede K, Sloane DM, Busse R, McKee M, … Kutney-Lee A (2012). Patient safety, satisfaction, and quality of hospital care: Cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. British Medical Journal, 344, e1717 10.1136/bmj.e1717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken LH, Sloane DM, Bruyneel L, Van den Heede K, Griffiths P, Busse R, … Sermeus W (2014). Nurse staffing and education and hospital mortality in nine European countries: A retrospective observational study. Lancet, 383(9931), 1824–1830. 10.1016/S0140-6736(13)62631-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Kandari F, & Thomas D (2009). Factors contributing to nursing task incompletion as perceived by nurses working in Kuwait general hospitals. Journal of Clinical Nursing, 18(24), 3430–3440. 10.1111/j.1365-2702.2009.02795.x [DOI] [PubMed] [Google Scholar]
- Anderson BJ, Manno M, O’Connor P, & Gallagher E (2010). Listening to nursing leaders: Using national database of nursing quality indicators data to study excellence in nursing leadership. Journal of Nursing Administration, 40(4), 182–187. 10.1097/NNA.0b013e3181d40f65 [DOI] [PubMed] [Google Scholar]
- Ausserhofer D, Zander B, Busse R, Schubert M, De Geest S, Rafferty AM, … Schwendimann R (2014). Prevalence, patterns and predictors of nursing care left undone in European hospitals: Results from the multicountry cross-sectional RN4CAST study. BMJ Quality & Safety, 23(2), 126–135. 10.1136/bmjqs-2013-002318 [DOI] [PubMed] [Google Scholar]
- Ball JE, Bruyneel L, Aiken LH, Sermeus W, Sloane DM, Rafferty AM, … Griffiths P (2018). Post-operative mortality, missed care and nurse staffing in nine countries: A cross-sectional study. International Journal of Nursing Studies, 78, 10–15. 10.1016/j.ijnurstu.2017.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ball JE, Murrells T, Rafferty AM, Morrow E, & Griffiths P (2014). ‘Care left undone’ during nursing shifts: Associations with workload and perceived quality of care. BMJ Quality & Safety, 23(2), 116–125. 10.1136/bmjqs-2012-001767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks-Carthon JM, Lasater KB, Rearden J, Holland S, & Sloane DM (2016). Unmet nursing care linked to rehospitalizations among older Black AMI patients: A cross-sectional study of US hospitals. Medical Care, 54(5), 457–465. 10.1097/Mlr.0000000000000519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruyneel L, Li B, Ausserhofer D, Lesaffre E, Dumitrescu I, Smith HL, … Sermeus W (2015). Organization of hospital nursing, provision of nursing care, and patient experiences with care in Europe. Medical Care Research and Review, 72(6), 643–664. 10.1177/1077558715589188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho SH, Kim YS, Yeon KN, You SJ, & Lee ID (2015). Effects of increasing nurse staffing on missed nursing care. International Nursing Review, 62(2), 267–274. 10.1111/inr.12173 [DOI] [PubMed] [Google Scholar]
- de Cordova PB, Rogowski J, Riman KA, & McHugh MD (2019). Effects of public reporting legislation of nurse staffing: A trend analysis. Policy, Politics, & Nursing Practice, 20(2), 92–104. 10.1177/1527154419832112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths P, Recio-Saucedo A, Dall’Ora C, Briggs J, Maruotti A, Meredith P, … Missed Care Study Group (2018). The association between nurse staffing and omissions in nursing care: A systematic review. Journal of Advanced Nursing, 74(7), 1474–1487. 10.1111/jan.13564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harless DW, & Mark BA (2010). Nurse staffing and quality of care with direct measurement of inpatient staffing. Medical Care, 48(7), 659–663. 10.1097/MLR.0b013e3181dbe200 [DOI] [PubMed] [Google Scholar]
- He J, Staggs VS, Bergquist-Beringer S, & Dunton N (2016). Nurse staffing and patient outcomes: A longitudinal study on trend and seasonality. BMC Nursing, 15(1), 60 10.1186/s12912-016-0181-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huber GP, Sutcliffe KM, Miller CC, & Glick WH (1993). Understanding and predicting organizational change In Huber GP, & Glick WH (Eds.), Organizational change and redesign: Ideas and insights for improving performance (pp. 215–265). New York, NY: Oxford University Press. [Google Scholar]
- Jones TL, Hamilton P, & Murry N (2015). Unfinished nursing care, missed care, and implicitly rationed care: State of the science review. International Journal of Nursing Studies, 52(6), 1121–1137. 10.1016/j.ijnurstu.2015.02.012 [DOI] [PubMed] [Google Scholar]
- Kalisch BJ (2006). Missed nursing care: A qualitative study. Journal of Nursing Care Quality, 21(4), 306–313; quiz 314–305. 10.1097/00001786-200610000-00006 [DOI] [PubMed] [Google Scholar]
- Kalisch BJ, Landstrom GL, & Hinshaw AS (2009). Missed nursing care: A concept analysis. Journal of Advanced Nursing, 65(7), 1509–1517. 10.1111/j.1365-2648.2009.05027.x [DOI] [PubMed] [Google Scholar]
- Kalisch BJ, Tschannen D, Lee H, & Friese CR (2011). Hospital variation in missed nursing care. American Journal of Medical Quality, 26(4), 291–299. 10.1177/1062860610395929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalisch BJ, & Xie B (2014). Errors of omission: Missed nursing care. Western Journal of Nursing Research, 36(7), 875–890. 10.1177/0193945914531859 [DOI] [PubMed] [Google Scholar]
- Kutney-Lee A, Stimpfel AW, Sloane DM, Cimiotti JP, Quinn LW, & Aiken LH (2015). Changes in patient and nurse outcomes associated with magnet hospital recognition. Medical Care, 53(6), 550–557. 10.1097/MLR.0000000000000355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kutney-Lee A, Wu ES, Sloane DM, & Aiken LH (2013). Changes in hospital nurse work environments and nurse job outcomes: An analysis of panel data. International Journal of Nursing Studies, 50(2), 195–201. 10.1016/j.ijnurstu.2012.07.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lake ET (2002). Development of the practice environment scale of the Nursing Work Index. Research in Nursing & Health, 25(3), 176–188. 10.1002/nur.10032 [DOI] [PubMed] [Google Scholar]
- Lake ET, Staiger D, Edwards EM, Smith JG, & Rogowski JA (2018). Nursing care disparities in neonatal intensive care units. Health Services Research, 53(Suppl 1), 3007–3026. 10.1111/1475-6773.12762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lasater KB, Jarrin OF, Aiken LH, McHugh MD, Sloane DM, & Smith HL (2019). A methodology for studying organizational performance: A multistate survey of front-line providers. Medical Care, 57(9), 742–749. 10.1097/MLR.0000000000001167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh MD, & Stimpfel AW (2012). Nurse reported quality of care: A measure of hospital quality. Research in Nursing & Health, 35(6), 566–575. 10.1002/nur.21503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montalvo I (2007). The national database of nursing quality indicators® (NDNQI®). The Online Journal of Issues in Nursing, 12(3), 112–214. 10.3912/ojin.vol12no03man02 [DOI] [Google Scholar]
- National Quality Forum (2017). Practice Environment Scale - Nursing Work Index (PES-NWI) (composite and five subscales). Retrieved from http://www.qualityforum.org/QPS/0206
- Needleman J (2016). The economic case for fundamental nursing care. Canadian Journal of Nursing Leadership, 29(1), 26–36. 10.12927/cjnl.2016.24643 [DOI] [PubMed] [Google Scholar]
- Papastavrou E, Andreou P, & Efstathiou G (2014). Rationing of nursing care and nurse–patient outcomes: A systematic review of quantitative studies. The International Journal of Health Planning and Management, 29(1), 3–25. 10.1002/hpm.2160 [DOI] [PubMed] [Google Scholar]
- Recio-Saucedo A, Dall’Ora C, Maruotti A, Ball J, Briggs J, Meredith P, … Smith GB (2017). What impact does nursing care left undone have on patient outcomes? Review of the literature. Journal of Clinical Nursing. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schilling PL, Campbell DA Jr, Englesbe MJ, & Davis MM (2010). A comparison of in-hospital mortality risk conferred by high hospital occupancy, differences in nurse staffing levels, weekend admission, and seasonal influenza. Medical Care, 48(3), 224–232. 10.1097/MLR.0b013e3181c162c0 [DOI] [PubMed] [Google Scholar]
- Shekelle PG (2013). Nurse – Patient ratios as a patient safety practice. Annals of Internal Medicine, 158, 404–409. [DOI] [PubMed] [Google Scholar]
- Sloane DM, Smith HL, McHugh MD, & Aiken LH (2018). Effect of changes in hospital nursing resources on improvements in patient safety and quality of care: A panel study. Medical Care, 56(12), 1001–1008. 10.1097/MLR.0000000000001002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swiger PA, Patrician PA, Miltner RSS, Raju D, Breckenridge-Sproat S, & Loan LA (2017). The practice environment scale of the nursing work index: An updated review and recommendations for use. International Journal of Nursing Studies, 74, 76–84. 10.1016/j.ijnurstu.2017.06.003 [DOI] [PubMed] [Google Scholar]
- VanFosson CA, Jones TL, & Yoder LH (2016). Unfinished nursing care: An important performance measure for nursing care systems. Nursing Outlook, 64(2), 124–136. 10.1016/j.outlook.2015.12.010 [DOI] [PubMed] [Google Scholar]
- Warshawsky NE, & Havens DS (2010). Global use of the practice environment scale of the nursing work index. Nursing Research, 60(1), 17–31. 10.1097/NNR.0b013e3181ffa79c [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Y, Ma D, Wan Z, Sun D, Li H, & Jiao S (2019). Association between work environment and implicit rationing of nursing care: An integrative literature review. Journal of Nursing Management. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- Zhu X-W, You L-M, Zheng J, Liu KE, Fang J-B, Hou SX, … Zhang L-F (2012). Nurse staffing levels make a difference on patient outcomes: A multisite study in Chinese hospitals. Journal of Nursing Scholarship, 44(3), 266–273. 10.1111/j.1547-5069.2012.01454.x [DOI] [PubMed] [Google Scholar]


