The Spanish lockdown during the COVID-19 pandemic has been one of the strictest among European countries since neither short walks nor individual sports were allowed for 7 weeks. Because of such confinement, physical activity was disrupted and cancellation of medical consultations occurred in rheumatic patients. As a consequence, an exacerbation of rheumatic symptomatology may have occurred [1]. In the same way, social isolation could have affected behavior and mental health, especially in older patients.
The aim of this survey was to evaluate treatment adherence during the COVID-19 pandemic and the impact of strict confinement on behaviors, disease activity and emotional status in Spanish rheumatic patients.
An observational, cross-sectional, nationwide study was conducted through the use of an anonymous electronic survey using the SurveyMonkey® tool between 25 April and 5 May (5 weeks after lockdown restrictions). This survey was released via patient organizations and social media to rheumatic patients around the country. Some details of this survey have been published previously elsewhere [2].
Patients were asked about their level of physical activity at home, the current treatments prescribed by the participants’ rheumatologist and treatment adherence. The question “Do you consider that your level of pain due to the disease has worsened during the confinement?” was asked. Two similar questions were also formulated to assess the worsening of fatigue and stiffness. A composite variable defined as “worsening of disease activity” was calculated using worsening of pain and worsening of stiffness and worsening of fatigue. Finally, the emotional status was also evaluated.
A total of 644 patients completed the survey. In total, 79.7% of patients continued their treatment as they had been doing before confinement; however, 9.8% and 10.5% spaced and stopped their treatment, respectively, specially the biologic therapy (20.3%). Among patients who spaced or stopped their treatment, 63.5% did so because they were afraid to develop COVID-19, and 49.2% did it by themselves without consulting any physician.
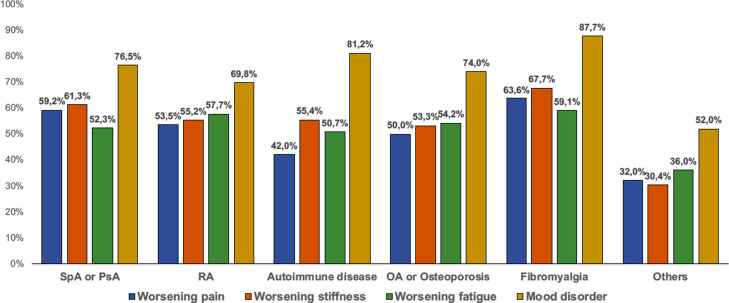
The prevalence of worsening of pain, stiffness, fatigue and mood disorder with regard to the diagnosis is represented in Fig. 1 . Overall, a worsening of disease activity was found in 37.4% patients, and the factors associated with this outcome after adjustment for treatment adherence are represented in Table 1 . The appearance of mood disorder during confinement was found in 75.7% patients. The multivariate analysis showed that, after adjustment for treatment adherence, factors independently associated with mood disorder (P < 0.05) were female sex (OR 2.48), Rheumatoid Arthritis (OR 0.54), other rheumatic diseases (OR 0.28) and worsening of disease activity (OR 2.95).
Fig. 1.
Worsening in symptoms during the confinement with regard to the diagnosis. OA: osteoarthritis; PsA: psoriatic arthritis; RA: rheumatoid arthritis; SpA: spondyloarthritis.
Table 1.
Factors associated with a worsening of disease activity (worsening of pain, stiffness and fatigue) during confinement.
| Worsening of disease activity n = 237 |
No worsening of disease activity n = 396 |
Multivariate analysis OR (95% CI) |
|
|---|---|---|---|
| Sex (female) | 177/235 (75.3%) | 291/395 (73.7%) | |
| Age, mean (SD) | 48.4 (11.1) | 48.1 (13.3) | |
| SpA or psoriatic arthritis | 119/237 (50.2%) | 185/396 (50.2%) | |
| Rheumatoid arthritis | 46/237 (19.4%) | 78/396 (19.7%) | |
| Systemic autoimmune diseases | 20/237 (8.4%) | 48/396 (12.1%) | 0.56 (0.31–0.99)* |
| Fibromyalgia | 32/237 (13.5%) | 32/396 (8.1%)* | |
| Osteoarthritis or osteoporosis | 17/237 (7.2%) | 32/396 (8.1%) | |
| Other rheumatic diseases | 3/237 (1.3%) | 21/396 (5.3%)* | 0.28 (0.08–0.99)* |
| NSAIDs use | 162/237 (68.4%) | 234/396 (59.1%)* | |
| Corticosteroids use | 54/237 (22.8%) | 88/396 (22.2%) | |
| csDMARDs use | 77/237 (32.5%) | 144/396 (36.4%) | |
| bDMARDs use | 85/237 (35.9%) | 152/396 (38.4%) | |
| Degree of confinement I never leave home I only go out to make basic purchases I continue working thus I go out every day |
89/237 (37.6%) 124/237 (52.3%) 24/237 (10.1%) |
158/393 (40.2%) 181/393 (46.1%) 54/393 (13.7%) |
|
| Physical activity at home None Occasionally Regularly |
82/237 (34.6%) 90/237 (38.0%) 65/237 (27.4%) |
105/393 (26.7%)* 138/393 (35.1%) 150/393 (38.2%) |
Reference 0.78 (0.51–1.19) 0.61 (0.40–0.95)* |
| Feel anxious | 190/236 (80.5%) | 231/393 (58.8%)§ | 1.98 (1.25–3.14)† |
| Feel sad | 188/235 (80.0%) | 223/392 (56.9%)§ | 2.02 (1.28–3.20)† |
| Treatment adherence I continue my treatment as I have been doing I have spaced my treatment I have stopped my treatment |
182/235 (77.4%) 28/235 (11.9%) 25/235 (10.6%) |
311/385 (80.8%) 34/385 (8.8%) 40/385 (10.4%) |
Reference 1.36 (0.77–2.39) 0.86 (0.49–1.52) |
bDMARDs: biological disease-modifying antirheumatic drugs; csDMARDs: conventional synthetic disease-modifying antirheumatic drugs; NSAIDs: non-steroidal anti-inflammatory drugs; OR: odds ratio; PsA: psoriatic arthritis; SD: standard deviation; SpA: spondyloarthritis;*: P < 0.05; †: P < 0.010; §: P < 0.001.
These results suggest that a considerable proportion of rheumatic patients have suffered a worsening of their symptomatology as well as emotional and mood disturbances during the COVID-19 lockdown. A total of 20.3% spaced and stopped their rheumatic treatment, despite many of these drugs were frequently used to treat the COVID-19 disease [3], [4]. Overall, 37.4% of patients felt a worsening of disease activity during confinement. This may be explained, on one hand, by the disruption of daily physical activity, which in normal circumstances has an important beneficial effect on pain, stiffness and wellbeing [5], and on the other hand, by the non-adherence to treatment in some patients. The worsening of symptomatology during confinement may also have had an impact on mood status since worsening of disease activity was independently associated with anxiety and sadness.
Authorship criteria
CLM conceived and designed the study, analyzed the data, drafted the letter and approved the final version of the document. LLP, IGG, MAPL, JMSS, PAO, ROC, JLGC and AEC interpreted the data, revised critically the letter and approved the final version. EC-E designed the study, revised critically the letter and approved the final version.
Funding
No specific funding was received from any bodies in the public, commercial or not-for-profit sectors to carry out the work described in this article.
Disclosure of interest
The authors declare that they have no competing interest.
Acknowledgements
We would like to thank all patients and patients’ organizations, specially CEADE (Spanish Federation of Spondyloarthritis Associations), who participated in this study.
References
- 1.Richez C., Lazaro E., Lemoine M., et al. Implications of COVID-19 for the management of patients with inflammatory rheumatic diseases. Joint Bone Spine. 2020;87:187–189. doi: 10.1016/j.jbspin.2020.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.López-Medina C., Escudero A., Collantes-Estévez E. COVID-19 pandemic: an opportunity to assess the utility of telemedicine in patients with rheumatic diseases. Ann Rheum Dis. 2020 doi: 10.1136/annrheumdis-2020-218008. [DOI] [PubMed] [Google Scholar]
- 3.Felten R., Chatelus E., Arnaud L. How and why are rheumatologists relevant to COVID-19? Joint Bone Spine. 2020;87:279–280. doi: 10.1016/j.jbspin.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Quartuccio L., Valent F., Pasut E., et al. Prevalence of COVID-19 among patients with chronic inflammatory rheumatic diseases treated with biologic agents or small molecules: a population-based study in the first two months of COVID-19 outbreak in Italy. Joint Bone Spine. 2020;87:439–443. doi: 10.1016/j.jbspin.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sveaas S.H., Smedslund G., Hagen K.B., et al. Effect of cardiorespiratory and strength exercises on disease activity in patients with inflammatory rheumatic diseases: a systematic review and meta-analysis. Br J Sports Med. 2017;51:1065–1072. doi: 10.1136/bjsports-2016-097149. [DOI] [PubMed] [Google Scholar]