Abstract
Background
To track triage, routing, and treatment status regarding access to endovascular treatment (EVT) after acute ischemic stroke (AIS) at a national level.
Methods
From national stroke audit data, potential candidates for EVT arriving within 6 hours with National Institute of Health Stroke Scale score of ≥ 7 were identified. Acute care hospitals were classified as thrombectomy-capable hospitals (TCHs, ≥ 15 EVT cases/year) or primary stroke hospital (PSH, < 15 cases/year), and patients' initial routes and subsequent inter-hospital transfer were described. Impact of initial routing to TCHs vs. PSHs on EVT and clinical outcomes were analyzed using multilevel generalized mixed effect models.
Results
Out of 14,902 AIS patients, 2,180 (14.6%) were EVT candidates. Eighty-one percent of EVT candidates were transported by ambulance, but only one-third were taken initially to TCHs. Initial routing to TCHs was associated with greater chances of receiving EVT compared to initial routing to PSHs (33.3% vs 12.1%, P < 0.001; adjusted odds ratio [aOR], 2.21; 95% confidence interval [CI], 1.59–2.92) and favorable outcome (38.5% vs. 28.2%, P < 0.001; aOR, 1.52; 95% CI, 1.16–2.00). Inter-hospital transfers to TCHs occurred in 17.4% of those initially routed to a PSH and was associated with the greater chance of EVT compared to remaining at PSHs (34.8% vs. 7.5%, P < 0.001), but not with better outcomes.
Conclusion
Two-thirds of EVT candidates were initially routed to PSHs despite greater chance of receiving EVT and having favorable outcomes if routed to a TCH in Korea. Process improvement is needed to direct appropriate patients to TCHs.
Keywords: Stroke, Endovascular Treatment, Stroke Center, Organization, Transfer
Graphical Abstract
INTRODUCTION
Along with introducing recombinant tissue plasminogen activator (tPA) for acute ischemic stroke (AIS), it was a priority to triage patients to the nearest tPA-available hospital and shortening door-to-needle time.1 These tenets lead to recruit hospitals into regional stroke care networks to ensure rapid accessibility.2
However, as substantial benefits of endovascular treatment (EVT) have been demonstrated in pivotal trials,3,4 re-organization of regional stroke systems have occurred to allow for delivering both of IVT and EVT.5 Traditional routing of patients to the nearest acute stroke care hospital may not be the best strategy, unless the latter hospital has capacity to provide EVT. Moreover, a recent study from North America reported that inter-hospital transfers affected the treatment delay and decreasing the chance of favorable outcomes.6
In most of western countries, rates of EVT are rapidly increasing7,8 and health systems are evolving towards improving access to EVT at a small distractive regional level.9 However, at a national level, there is a lack of information on how EVT-eligible patients are triaged, routed and treated, and what is their outcome.
The aim of this study was, using national stroke audit data, to describe triage and channel routing of EVT-eligible AIS patients at a national level in Korea and to compare treatment status and clinical outcomes between patients initially routed to thrombectomy-capable hospitals (TCH) vs. those to primary stroke hospitals (PSHs).
METHODS
Study protocol, data source and ethics statement
This study used the Acute Stroke Quality Assessment Program (ASQAP) data to assess the quality of care in nationwide acute stroke hospitals by the Health Insurance Review and Assessment Service (HIRA) under Ministry of Health and Welfare, Korea.10,11 It collected pre-specified quality indicators of hospitalized stroke patients whose diagnostic disease codes at discharge are through I60–I64 of the International Classification of Diseases, Tenth Revision, and who are admitted within 7 days of symptom onset.12
For this study, we included patients with ischemic stroke (I63) in the 5th (from March to May, 2013) and 6th (from June to August, 2014) assessments and extracted their patient- and hospital-level information. Post-stroke mortality was confirmed by a linkage between the ASQAP database and the insurance database of the National Health Insurance Service, which is a compulsory government insurance service system subscribed to by all citizens.
Study subjects and data collection
For included subjects, EVT candidates were defined as follows: 1) aged 18 years or greater; 2) hospitalized within 6 hours of last known well time; and 3) having a baseline National Institute of Health Stroke Scale (NIHSS) score of 7 or higher.4,13 Of them, patient-level characteristics such as age, sex, use of ambulance, transfer information, time to arrival, baseline stroke severity as measured by NIHSS or the Glasgow Coma Scale (GCS), whether a patient received IVT and EVT, door-to-needle time for IVT, and hospital-level characteristics such as bed size, number of neurologists, and provision of stroke unit care were collected. A favorable outcome at discharge was defined as either modified Rankin Scale of ≤ 2 or Barthel Index of ≥ 95.14 Mortality was determined at 3 months and 1 year from onset of the index stroke.
Because there was no certified thrombectomy-capable stroke center in the study time (the Korean Stroke Society started the Primary Stroke Center Certification Program in 2018), acute care hospitals were classified using a modified criterion of the Joint Commission for thrombectomy capable stroke center.15 Hospitals were operationally dichotomized into TCHs and PSHs according to an annual EVT volume of 15 or more or less than 15, respectively. Hospitals that were excluded from the ASQAP due to a stroke volume of less than 10 cases per 3-month period were classified as PSH. Channel routes of EVT-screening candidates were schematized as follows: the initial routes were divided into initial routing to TCHs versus PSHs. In the next step, patients' routes were divided into secondary inter-hospital transfer and remaining at the hospital to which they were initially routed (Supplementary Fig. 1).
Statistical analysis
Baseline characteristics of patients and hospitals were presented as frequency (%) and mean ± standard deviation or median with an interquartile range as appropriate. As stroke severity was reported as either NIHSS or GCS scores, the projected NIHSS score was substituted for the GCS score having closed probability for 3-month mortality (Supplementary Table 1).
Comparisons were made between initial routing to TCHs versus PSHs in terms of patient-level and hospital-level characteristics, implementation of recanalization therapy, and outcomes. The effect of initial routing to TCHs versus PSHs on EVT, functional outcomes at discharge, and mortality was evaluated using multilevel generalized mixed effect models with predetermined adjustments for age, sex and baseline NIHSS scores (fixed effects) and hospital (random effect). Since a substantial proportion of patients initially routed to a PSH had missingness on functional outcomes, the primary analysis was complete case analysis, and sensitivity analysis was performed to check the robustness of its results with imputation for missing cases. The imputation was performed by randomly imputing a favorable outcome to a missing case at the rate of y% and y + 10%, where y was the projected favorable outcome rate obtained from the complete case analysis.
Patients who were treated with EVT were compared separately regarding treatment metrics and outcomes according to channel routing to final treatment hospitals which was categorized as follows; 1) initially routed to a TCH (“mothership” model); 2) initially routed to a PSH and secondarily transferred to a TCH (“drip-and-ship” model); and 3) initially routed to a PSH and remaining there (“small-sized mothership” model).
TCHs and PSHs were compared in terms of the capacity of the facilities and monthly stroke patient volume. Finally, regional disparities were evaluated by 1) locating TCHs and PSHs on the national administrative district map and assessing the corresponding population density; and 2) analyzing the correlation of initial routing to TCH with EVT rates and 1-month mortality by regions. Statistical tests were two-tailed and the threshold for statistical significance was set at P < 0.05. All statistical analyses were performed using SAS Enterprise Guide 6.1 (SAS Institute Inc., Cary, NC, USA) and R software version 3.3.3 (R Foundation for Statistical Computing, Vienna, Austria).
Ethics statement
This study was exempt from the necessity for approval of the Institutional Review Board of Seoul National University Bundang Hospital due to anonymity of participants, its retrospective nature, and minimal risk to enrolled subjects (No. X-1704-393-906). According to the Act on the Protection of Personal Information and Maintenance by Public Institutions, the HIRA provided anonymized patient and hospital data using the web-based ASQAP data warehouse, and only pre-authorized researchers had access to data housed remotely on a separate server managed by the HIRA.
RESULTS
Over a total of 6 months, 14,902 patients with ischemic stroke were admitted. Among them, 2,180 (14.6%) visited to 201 acute care hospitals within 6 hours of onset with a baseline NIHSS score of ≥ 7 and analyzed as EVT candidates whose mean age was 72.9 years and the median NIHSS score was 14 (Table 1 and Supplementary Fig. 2).
Table 1. Baseline characteristics of thrombectomy-eligible patients and hospitals where they were treated.
| Variables | Patients with ischemic stroke (n = 14,902) | Thrombectomy-eligible patients (n = 2,180) | |
|---|---|---|---|
| Patient-level characteristics | |||
| Male | 8,585 (57.6) | 1,132 (51.9) | |
| Age, yr | 69.6 ± 12.6 | 72.9 ± 12.5 | |
| Ambulance use | 7,422 (49.8) | 1,770 (81.2) | |
| Onset-to-arrival time, min | 583.0 (161.0–1,535.0) | 109.0 (49.0–202.5) | |
| NIHSS scorea | 4 (2–8) | 14 (9–19) | |
| Hospital-level characteristics | |||
| No. of hospitals | 216 | 201 | |
| Bed size | 514.5 (355–797.8) | 515 (355–798) | |
| Availability of stroke unit care | 67 (31.0) | 67 (33.3) | |
| No. of neurologists | 2 (1–5) | 2 (1–5) | |
Values represent number of patients (%), mean ± standard deviation, or median (interquartile range).
NIHSS = National Institute of Health Stroke Scale.
aNIHSS score was merged values of NIHSS score and transformed NIHSS score from Glasgow Coma Scale score, and excluded the missing 110 (5.1%) thrombectomy-eligible patients and the overall 1,180 (7.9%) patients with ischemic stroke.
Channel routes of the EVT candidates
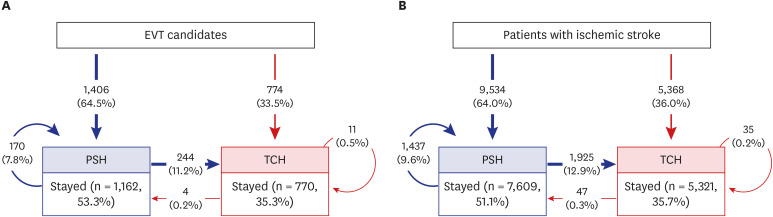
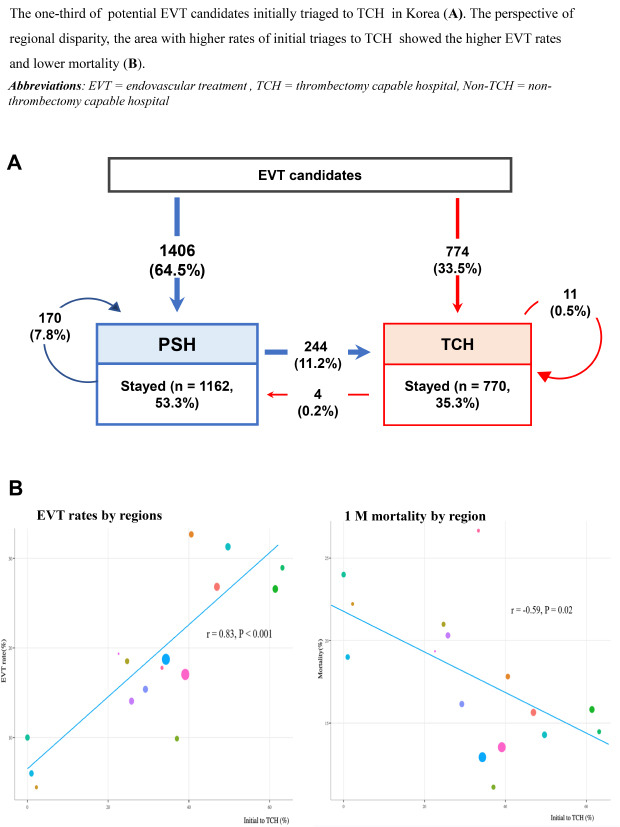
Initial routes were to TCHs for one-third of patients (n = 774) and to PSHs for the remaining two-thirds (n = 1,406). In the latter group (initial to PSHs), 244 (17.4%) were secondarily transferred to TCHs (Fig. 1A). Channel routing of the overall AIS population was similar trend to that of the EVT candidates (Fig. 1B).
Fig. 1. Nationwide channel routing of ischemic stroke patients. (A) Channel routing of nationwide ischemic stroke patients who were eligible for thrombectomy and (B) patients with ischemic stroke. According to the initial routes, patients were separated into patients initially routed to a TCH (red box) or a PSH (blue box). There were three outflow routes for the former; stayed-on, transferred to another TCH, or transferred to PSH (red). The outflow routes of patients initially routed to PSHs were: stayed-on, transferred to another PSH, or transferred to a TCH (blue). Values represent number of patients.
EVT = endovascular treatment, TCH = thrombectomy capable hospital, PSH = non-thrombectomy capable hospital.
Initial routing and its effects: TCH versus PSH
Patients initially routed to TCHs were more likely to be younger, higher use of ambulance, shorter arrival time interval, higher proportion of atrial fibrillation, and lower NIHSS scores compared to those initially routed to PSHs (Table 2). These differences were similarly observed in the whole AIS population (Supplementary Table 2).
Table 2. Comparisons between TCHs and PSHs.
| Variables | Patients initially routed to a TCH (n = 774) | Patients initially routing to a PSH (n = 1,406) | P value | |
|---|---|---|---|---|
| Patient-level characteristics | ||||
| Male | 401 (51.8) | 731 (52.0) | 0.930 | |
| Age, yr | 70.8 ± 12.6 | 74.0 ± 12.2 | < 0.001 | |
| Use of ambulance | 641 (82.8) | 1,129 (80.3) | 0.020 | |
| Onset-to-arrival time, min | 82.0 (42.0–179.0) | 124.0 (57.0–211.0) | < 0.001 | |
| Atrial fibrillation | 309 (44.9) | 373 (30.6) | < 0.001 | |
| Smoking | 155 (20.4) | 265 (20.7) | 0.320 | |
| NIHSS scores | 13 (9–17) | 14 (10–19)a | < 0.001 | |
| Recanalization therapy | ||||
| IVT | 515 (53.8) | 395 (35.5) | < 0.001 | |
| EVT | 319 (33.3) | 172 (12.2) | < 0.001 | |
| Outcomes | ||||
| Favorable outcome at dischargeb | 260 (38.5) | 257 (28.2) | < 0.001 | |
| 3-month mortality | 152 (19.6) | 325 (23.1) | 0.060 | |
| 1-year mortality | 227 (29.3) | 506 (36.0) | 0.002 | |
Values represent number of patients (%), mean ± standard deviation, or median (interquartile range).
P values were obtained with Pearson's χ2 test, t-tests, or Mann-Whitney U tests as appropriate.
TCH = thrombectomy capable hospital, PSH = non-thrombectomy capable hospital, IVT = intravenous thrombolysis, EVT = endovascular treatment.
aDenotes that estimations exclude the 110 missing patients; bIndicates the exclusion of the 99 cases for TCHs and the 495 cases for PSHs.
Initial routing significantly affected the implementation of recanalization therapy. EVT rates were 33.3% in patients initially routed to TCH and 12.2% in those to PSH, with IVT rates of 53.8% and 35.5%, respectively (P < 0.001). The increased odds of receiving EVT from initial routing to TCH was independent of age, sex, baseline NIHSS score and hospital (adjusted odds ratio [OR], 2.21; 95% confidence interval [CI], 1.59–2.92).
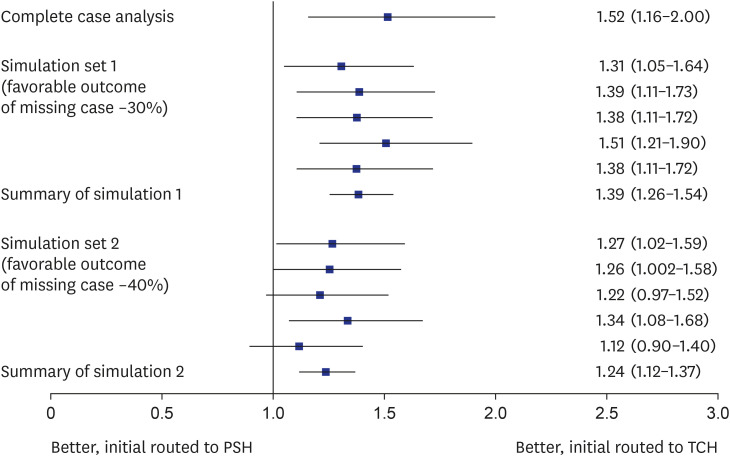
In the crude analysis, initial routing appeared to affect clinical outcomes. There was a significant difference in favorable outcome at discharge (38.5% vs. 28.2%; P < 0.001) and 1-year mortality (29.3% vs. 36.0%, P = 0.002) but not in 3-month mortality (19.6% vs. 23.1%, P = 0.06) between initial routing to TCHs vs. PSHs, respectively. The multivariable models showed the independent positive effect of initial routing to a TCH on favorable outcome at discharge (OR, 1.52; 95% CI, 1.16–2.00) but did not support the preventive effect of initial routing to a TCH on post-stroke mortality (3-month mortality: 1.09; 0.85–1.39; 1-year mortality: 0.98; 0.79–1.23; Supplementary Table 3). The sensitivity analysis with the imputation of favorable outcome rates of missing cases (n = 594, 27.2%) being projected as 30% and 40% showed the similar findings (Fig. 2).
Fig. 2. Effects of initial routing to TCHs on favorable outcome. Adjusted OR (95% CI) of initial routing to a TCH for favorable outcome with two level adjustments for hospital-level and patient-level covariates (age, sex, and baseline National Institute of Health Stroke Scale score). Robust multivariable analyses were tested by complete cases plus simulation set 1 and simulation set 2 (projected favorable outcome rate of missing cases was around 30% and around 40%, respectively). Each simulation set was transformed into 5 random sample sets for missing cases, and results were depicted with the summary value. Squares represent the OR and lines represent the 95% CI.
OR = odds ratio, CI = confidence interval, TCH = thrombectomy capable hospital, PSH = non-thrombectomy capable hospital.
PSH: secondary inter-hospital transfer versus remaining at initial hospital
Out of the 1,406 patients initially routed to PSHs, secondary inter-hospital transfer to TCHs occurred in 17.4% and was significantly associated with higher EVT rates (34.8% in patients with inter-hospital transfer versus 7.5% in those remaining at PSHs, P < 0.001). But, there was no difference in IVT rates or 3-month and 1-year mortality (Supplementary Table 4).
Comparisons of patients receiving EVT according to channel routing
In total, 423 EVTs were performed; 59.3% by initial routing to a TCH (mothership), 20.1% by secondary inter-hospital transfer to a TCH (drip-and-ship), 20.6% remaining at a PSH (small sized mothership) (Table 3). Between these groups, onset-to-arrival time at the final treatment hospital was significantly different (P < 0.001). Those receiving EVT at the initial routing to a TCH had more favorable outcomes at discharge compared to those receiving EVT after inter-hospital transfer (drip and ship) and those remaining at a PSH and receiving EVT (37.5%, 21.2% and 21.8%, respectively; P = 0.003).
Table 3. Comparisons of patients treated by EVT in terms of treatment metrics and outcomes according to channel routes to the final treatment hospitals.
| Variables | Initially routing to TCH (n = 251) | Transferred to TCH (n = 85) | Staying at PSH (n = 87) | P value |
|---|---|---|---|---|
| Onset-to-arrival time at final treating hospitals, mina | 61.5 (39.0–138.0) | 152.0 (109.0–227.0) | 63.0 (31.0–129.0) | < 0.001 |
| Combined IVT | 163 (64.9) | 42 (49.4) | 52 (59.8) | 0.040 |
| Door-to-needle time, min | 40.0 (30.0–50.0) | 30.5 (22.0–40.0) | 50.0 (36.0–58.0) | < 0.001 |
| Favorable functional outcomeb | 94 (37.5) | 18 (21.2) | 19 (21.8) | 0.007 |
| Three-month mortality | 42 (16.7) | 19 (22.4) | 22 (25.3) | 0.170 |
| One-year mortality | 58 (23.1) | 28 (32.9) | 30 (34.5) | 0.050 |
Values are presented as median (interquartile range) or number (%).
TCH = thrombectomy capable hospital, PSH = non-thrombectomy capable hospital, EVT = endovascular treatment, IVT = intravenous thrombolysis.
aIndicates that the time delay to the final treatment hospital was estimated after excluding the missing cases of initial routing to a TCH (n = 1), secondary inter-hospital transfer to a TCH (n = 1) and stay at a PSH (n = 0); bIndicates that the percentages are estimated after exclusion of the missing 37 (14.7%) cases for initial routing to a TCH, 11 (12.9%) for inter-hospital transfer to a TCH and 28 (32.2%) for remaining at a PSH. P values were obtained by Kruskal-Wallis test or Pearson's χ2 test as appropriate.
Treatment capacity of acute care hospitals: TCHs versus PSHs
TCHs accounted for 20.4% of acute stroke care hospitals. In terms of facility capacity, TCHs had more hospital beds and neurologists and higher availability of stroke unit care compared to PSHs (Supplementary Table 5). With respect to monthly treatment volume, TCHs treated more EVT candidates, and had more EVT and IVT cases. The median case volume per month in TCHs versus PSHs was 2.0 versus 0.2 for IVT and 2.0 versus 0.0 for EVT, respectively.
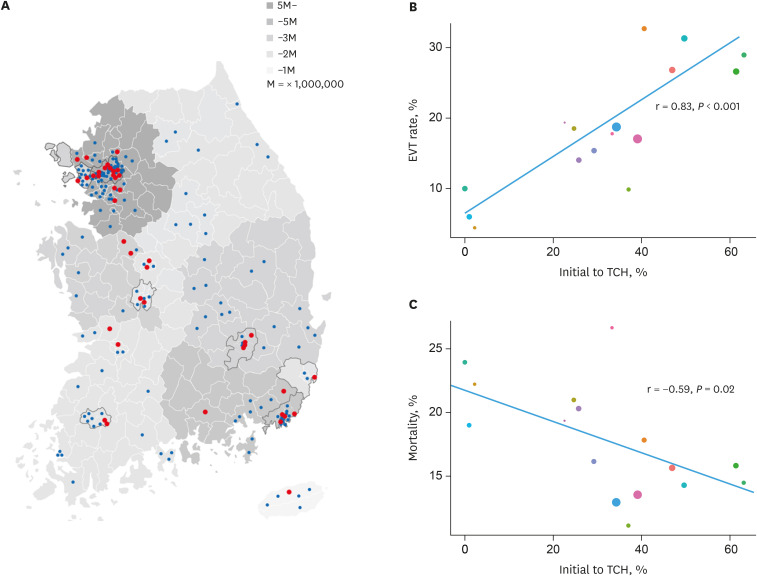
Regional disparities: TCHs versus PSHs
TCHs were mostly located in regions with high population densities, while PSHs were more evenly distributed throughout the nation (Fig. 3A). The regional rates of initial routing to a TCH among the EVT-potential candidates ranged from 0 to 63.2% (P < 0.001) (Supplementary Table 6). The regional EVT rates varied from 9.9% to 32.7%. In these regional comparisons, initial routing to a TCH positively correlated with EVT (r = 0.68, P = 0.01), while negatively with 1-month mortality (r = −0.57, P = 0.03) (Fig. 3B and C).
Fig. 3. Acute stroke care hospitals in Korea. Distribution of TCHs and PSHs (A) and correlations between routing to a TCH and treatment (B) and mortality (C). Distribution of TCHs and PSHs on a map of the population density of the Republic of Korea (A). Plots depicting the correlation between the proportion of those initially routed to a TCH and EVT rates (B) and those initially routed to a TCH and 1-month mortality (C) based on region. Red circles represent TCHs and blue circles represent PSHs. Population density is reflected by the intensity of grey (A). Circles denote individual regions whereby the color represents different area and size depending on the number of thrombectomy-screening candidates (B). Correlations were estimated with Pearson's correlation test.
EVT = endovascular treatment, TCH = thrombectomy capable hospital, PSH = non-thrombectomy capable hospital.
DISCUSSION
This study assessed the accessibility for EVT in patients potentially eligible for EVT at a national level, and ascertained the effects of channel routing on EVT rates and clinical outcomes in real-world practice. Although more than 80% of patients arrived at the emergency room via ambulance, only one-third were brought to TCHs and two-thirds to PSHs at the initial routing. About 17% of those with initial routing to PSHs were secondarily transferred to TCHs for further treatment.
Compared to initial routing to a PSH and inter-hospital transfer to a TCH, initial routing to a TCH has been repeatedly reported to lead to faster treatment and a greater chance of good outcome.16,17,18 However, previous studies registered patients who received EVT in the comprehensive stroke center, and could not investigate the impact of initial routing to a TCH compared to a PSH with regard to the accessibility to EVT in the whole EVT-eligible population. Furthermore, they were conducted by most of voluntarily participated large centers, they may not be representative of whole real-world practice. Our results from the entire EVT-eligible population in Korea would have merits to figure out the EVT triage system, in summary, an EVT rate of 22.5% across the whole EVT potential candidates, and 33.3% and 12.2% among those with or without initial routing to a TCH, respectively. Initial routing to a TCH compared a PSH increased the odds of receiving EVT by more than 2-fold and of having favorable outcome at discharge by around 50% independent of age, sex and stroke severity. Such results have not been previously reported at a national level.
Secondary inter-hospital transfer to a TCH appeared to increase the accessibility to EVT more than 4-fold (34.8% vs. 7.5%) but did not improve clinical outcomes in those receiving EVT (Table 3) or in EVT candidates (Supplementary Table 4) compared to those remaining at a PSH. No benefits were identified for inter-hospital transfer over remaining at a PSH despite there being no differences in baseline NIHSS and higher EVT rates upon transfer. This finding requires validation. One possible explanation is that there was a difference of 90.5 minutes in onset-to-arrival at final treatment hospitals in those receiving EVT between the mothership and drip-and-ship models (Table 3), which is close in time to the 84 minutes of time gap for onset-to-puncture time identified between two channel routes in a recent large prospective EVT registry-based study.6
In a registry-based study from France,19 56% of the EVT-eligible patients were transferred from other hospitals to a comprehensive stroke center (compared to 17% in this study), and 25% of those transferred were treated with EVT (compared to 35% in this study). The proportion of those with favorable outcomes was not significantly altered by inter-hospital transfer, which is consistent with the findings of our study. These findings supported that initial transportation of patients eligible for EVT to a TCH, or centralization may be an optimizing strategy.20
Previously, stroke triage streamlined stroke patient delivery to the nearest IVT-enable emergency departments.21 Our study showed that channel routing in the Korean stroke delivery system configured to provide appropriate accessibility to IVT and apparently operated well at a national level. However, the high rate of national channel routing of two-thirds of AIS patients to PSHs suggests reconfiguring its process of acute stroke patient delivery in the era of EVT. Along with the paradigm shift to EVT, stroke systems of care have been moving towards screening patients to select those who are expected to benefit from EVT at prehospital stage, and timely transport of the patient to the proper facility.22
In regard to how to improve the low rate of initial routing to a TCH, the prehospital triage system is key.23 In our study, about 80% of potential thrombectomy candidates used the EMS ambulance. Given the large number of patients remaining at PSHs in our study (82.6% of those initially routed to PSHs), an increase of initial routing to TCHs by about 10% would raise the absolute number of EVT cases by about 5.6%. Of course, this requires reform of the prehospital triage with a more EMS-personnel friendly triage protocol or active mobile stroke unit, a preferential directing system, more organized regional stroke systems, and a direct communication tool between EMS and stroke centers.24
The low rate of inter-hospital transfer to TCHs among those initially routed to PSHs and eligible for EVT (17.4%) merits further discussion. Even though an effective inter-hospital network may be challenging to establish,25 treatment rates and clinical outcomes at a regional level could be improved by increasing the absolute number of inter-hospital transfers and reducing the transfer time. Common imaging protocols with an efficient imaging transmission, and health information sharing systems between network hospitals would facilitate inter-hospital transfer. The streamlined hub-and-spoke workflow of fast and high-priority referral systems by EMS or equivalent agencies would enable more efficient transfers.26
Regional rates of initial routing to TCHs correlated with regional EVT rates and 1-month mortality (Fig. 3). These findings, along with the paucity of TCHs in areas with a low population density support the view that initial routing to a TCH would be a preferential model in these areas, even a little more time delays of bypassing the closest hospital.6,26 In most of urban area, effective secondary inter-hospital transfer may be more practical in this case, however, our data does not support this is a good option, especially in the EVT-eligible population.
Limitations of this study should be noted. First, this study used national stroke audit data in 2013 and 2014, when EVT had just begun to be applied to AIS patients in clinical practice. Although the number of EVT cases was not low in this study, 2013 and 2014 could be considered as the dawn of the EVT era. Second, the ASQAP aimed to assess the quality of general stroke care in acute care hospitals, and therefore did not collect information that determined exact EVT-eligibility criteria. Rather than the existence of large vessel occlusion, the NIHSS score and onset-to-arrival time were used to determine eligibility for EVT, which could be more practical metrics for real-world prehospital triage.26 Third, information on functional outcomes at discharge was missing in 35% of AIS patients treated at PSHs, though we tried to compensate for this through sensitivity analysis with imputation.
In conclusion, the initial routing of stroke patients affected the chance of receiving EVT in Korea. Process improvement is needed to direct potentially eligible patients to TCHs with consideration of regional situations.
Footnotes
Funding: This study was performed by the Joint Project on Quality Assessment Research of the Health Insurance Review and Assessment Service, Republic of Korea, and supported by a fund (2017ER620101#) by Research of Korea Centers for Disease Control and Prevention.
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Kang J, Kim SE, Kim JY, Lee KB, Lee JS, Lee J, Bae HJ.
- Data curation: Yang KH, Choi AR, Kang MY.
- Formal analysis: Kim SE, Lee JS, Lee J.
- Investigation: Kang J, Park HK, Cho YJ, Park JM, Lee SJ, Kim JY, Park KY, Gorelick PB.
- Methodology: Kang J, Lee J, Kim SE, Bae HJ, Lee KJ.
- Writing - original draft: Kang J, Kim SE.
- Writing - review & editing: Kang J, Kim JY, Lee KB, Gorelick PB, Choi NC, Bae HJ.
SUPPLEMENTARY MATERIALS
Summarized scores between NIHSS and GCS scores
Comparisons of patient-level characteristics by initial routing hospital of patients with ischemic stroke
Results of multilevel generalized mixed effect models of initial routing to TCH versus PSH
Comparisons of baseline characteristics, recanalization therapy and outcomes by secondary interhospital transfer to TCH versus staying at PSH among patients with initial routing to PSH
Comparisons of hospital-level characteristics and monthly treatment volume between TCH and PSH
Regional disparities in channel routing, EVT rates and 1-month mortality of the thrombectomy-eligible patients
Schematic flow of nationwide channel routing system. At patients' level, initial direct routing was divided into TCH and PSH. When patients initially visited to PSH, their secondary paths were schematized as stayed on PSH, transfer to another PSH and transfer to TCH (blue lines). In case of initial visit to TCH, they were as stayed on TCH, transfer to another TCH and transfer to PSH (red lines).
The flow chart of enrollment. Data was from ASQAP by the Health Insurance Review and Assessment Service, Republic of Korea.
References
- 1.Alberts MJ, Latchaw RE, Jagoda A, Wechsler LR, Crocco T, George MG, et al. Revised and updated recommendations for the establishment of primary stroke centers: a summary statement from the brain attack coalition. Stroke. 2011;42(9):2651–2665. doi: 10.1161/STROKEAHA.111.615336. [DOI] [PubMed] [Google Scholar]
- 2.Abilleira S, Dávalos A, Chamorro A, Alvarez-Sabín J, Ribera A, Gallofré M, et al. Outcomes of intravenous thrombolysis after dissemination of the stroke code and designation of new referral hospitals in Catalonia: the Catalan Stroke Code and Thrombolysis (Cat-SCT) monitored study. Stroke. 2011;42(7):2001–2006. doi: 10.1161/STROKEAHA.110.605030. [DOI] [PubMed] [Google Scholar]
- 3.Saver JL, Goyal M, van der Lugt A, Menon BK, Majoie CBLM, Dippel DW, et al. Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: a meta-analysis. JAMA. 2016;316(12):1279–1288. doi: 10.1001/jama.2016.13647. [DOI] [PubMed] [Google Scholar]
- 4.Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019;50(12):e344–418. doi: 10.1161/STR.0000000000000211. [DOI] [PubMed] [Google Scholar]
- 5.Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. 2018 Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018;49(3):e46–110. doi: 10.1161/STR.0000000000000158. [DOI] [PubMed] [Google Scholar]
- 6.Froehler MT, Saver JL, Zaidat OO, Jahan R, Aziz-Sultan MA, Klucznik RP, et al. Interhospital transfer before thrombectomy is associated with delayed treatment and worse outcome in the STRATIS registry (systematic evaluation of patients treated with neurothrombectomy devices for acute ischemic stroke) Circulation. 2017;136(24):2311–2321. doi: 10.1161/CIRCULATIONAHA.117.028920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fang MC, Cutler DM, Rosen AB. Trends in thrombolytic use for ischemic stroke in the United States. J Hosp Med. 2010;5(7):406–409. doi: 10.1002/jhm.689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Scherf S, Limburg M, Wimmers R, Middelkoop I, Lingsma H. Increase in national intravenous thrombolysis rates for ischaemic stroke between 2005 and 2012: is bigger better? BMC Neurol. 2016;16(1):53. doi: 10.1186/s12883-016-0574-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Raychev RI, Stradling D, Patel N, Gee JR, Lombardi DA, Moon JL, et al. Evolution of a US county system for acute comprehensive stroke care. Stroke. 2018;49(5):1217–1222. doi: 10.1161/STROKEAHA.118.020620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang JH, Kim SM, Han SJ, Knaak M, Yang GH, Lee KD, et al. The impact of Value Incentive Program (VIP) on the quality of hospital care for acute stroke in Korea. Int J Qual Health Care. 2016;28(5):580–585. doi: 10.1093/intqhc/mzw081. [DOI] [PubMed] [Google Scholar]
- 11.Kim JY, Lee KJ, Kang J, Kim BJ, Kim SE, Oh H, et al. Acute stroke care in Korea in 2013–2014: national averages and disparities. J Korean Med Sci. 2020;35(20):e167. doi: 10.3346/jkms.2020.35.e167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Park HK, Kim SE, Cho YJ, Kim JY, Oh H, Kim BJ, et al. Quality of acute stroke care in Korea (2008–2014): retrospective analysis of the nationwide and nonselective data for quality of acute stroke care. Eur Stroke J. 2019;4(4):337–346. doi: 10.1177/2396987319849983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Heldner MR, Hsieh K, Broeg-Morvay A, Mordasini P, Bühlmann M, Jung S, et al. Clinical prediction of large vessel occlusion in anterior circulation stroke: mission impossible? J Neurol. 2016;263(8):1633–1640. doi: 10.1007/s00415-016-8180-6. [DOI] [PubMed] [Google Scholar]
- 14.Lai SM, Duncan PW. Stroke recovery profile and the Modified Rankin assessment. Neuroepidemiology. 2001;20(1):26–30. doi: 10.1159/000054754. [DOI] [PubMed] [Google Scholar]
- 15.The Joint Commission. Certification for thrombectomy-capable stroke centers. [Updated 2020]. [Accessed September 7, 2019]. https://www.jointcommission.org/certification/certification_for_thrombectomycapable_stroke_centers.aspx.
- 16.Kodankandath TV, Wright P, Power PM, Geronimo MD, Libman RB, Kwiatkowski T, et al. Improving transfer times for acute ischemic stroke patients to a comprehensive stroke center. J Stroke Cerebrovasc Dis. 2017;26(1):192–195. doi: 10.1016/j.jstrokecerebrovasdis.2016.09.008. [DOI] [PubMed] [Google Scholar]
- 17.Venema E, Groot AE, Lingsma HF, Hinsenveld W, Treurniet KM, Chalos V, et al. Effect of interhospital transfer on endovascular treatment for acute ischemic stroke. Stroke. 2019;50(4):923–930. doi: 10.1161/STROKEAHA.118.024091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gerschenfeld G, Muresan IP, Blanc R, Obadia M, Abrivard M, Piotin M, et al. Two paradigms for endovascular thrombectomy after intravenous thrombolysis for acute ischemic stroke. JAMA Neurol. 2017;74(5):549–556. doi: 10.1001/jamaneurol.2016.5823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sablot D, Gaillard N, Smadja P, Bonnec JM, Bonafe A. Thrombectomy accessibility after transfer from a primary stroke center: analysis of a three-year prospective registry. Int J Stroke. 2017;12(5):519–523. doi: 10.1177/1747493017701151. [DOI] [PubMed] [Google Scholar]
- 20.Mohamad NF, Hastrup S, Rasmussen M, Andersen MS, Johnsen SP, Andersen G, et al. Bypassing primary stroke centre reduces delay and improves outcomes for patients with large vessel occlusion. Eur Stroke J. 2016;1(2):85–92. doi: 10.1177/2396987316647857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Higashida R, Alberts MJ, Alexander DN, Crocco TJ, Demaerschalk BM, Derdeyn CP, et al. Interactions within stroke systems of care: a policy statement from the American Heart Association/American Stroke Association. Stroke. 2013;44(10):2961–2984. doi: 10.1161/STR.0b013e3182a6d2b2. [DOI] [PubMed] [Google Scholar]
- 22.Détraz L, Ernst M, Bourcier R. Stroke transfer and its organizational paradigm: review of organizational paradigms and the impact on outcome. Clin Neuroradiol. 2018;28(4):473–480. doi: 10.1007/s00062-018-0715-z. [DOI] [PubMed] [Google Scholar]
- 23.Schlemm E, Ebinger M, Nolte CH, Endres M, Schlemm L. Optimal transport destination for ischemic stroke patients with unknown vessel status: use of prehospital triage scores. Stroke. 2017;48(8):2184–2191. doi: 10.1161/STROKEAHA.117.017281. [DOI] [PubMed] [Google Scholar]
- 24.Saposnik G, Baibergenova A, O'Donnell M, Hill MD, Kapral MK, Hachinski V, et al. Hospital volume and stroke outcome: does it matter? Neurology. 2007;69(11):1142–1151. doi: 10.1212/01.wnl.0000268485.93349.58. [DOI] [PubMed] [Google Scholar]
- 25.Song S, Saver J. Growth of regional acute stroke systems of care in the United States in the first decade of the 21st century. Stroke. 2012;43(7):1975–1978. doi: 10.1161/STROKEAHA.112.657809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Meretoja A, Roine RO, Kaste M, Linna M, Roine S, Juntunen M, et al. Effectiveness of primary and comprehensive stroke centers: PERFECT stroke: a nationwide observational study from Finland. Stroke. 2010;41(6):1102–1107. doi: 10.1161/STROKEAHA.109.577718. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Summarized scores between NIHSS and GCS scores
Comparisons of patient-level characteristics by initial routing hospital of patients with ischemic stroke
Results of multilevel generalized mixed effect models of initial routing to TCH versus PSH
Comparisons of baseline characteristics, recanalization therapy and outcomes by secondary interhospital transfer to TCH versus staying at PSH among patients with initial routing to PSH
Comparisons of hospital-level characteristics and monthly treatment volume between TCH and PSH
Regional disparities in channel routing, EVT rates and 1-month mortality of the thrombectomy-eligible patients
Schematic flow of nationwide channel routing system. At patients' level, initial direct routing was divided into TCH and PSH. When patients initially visited to PSH, their secondary paths were schematized as stayed on PSH, transfer to another PSH and transfer to TCH (blue lines). In case of initial visit to TCH, they were as stayed on TCH, transfer to another TCH and transfer to PSH (red lines).
The flow chart of enrollment. Data was from ASQAP by the Health Insurance Review and Assessment Service, Republic of Korea.