Abstract
India enforced stringent lockdown measures on March 24, 2020 to mitigate the spread of the Severe Acute Respiratory Syndrome Coronovirus-2 (SARS-CoV-2). Here, we examined the impact of lockdown on the air quality index (AQI) [including ambient particulate matter (PM10 and PM2.5), nitrogen dioxide (NO2), sulfur dioxide (SO2), carbon monoxide (CO), ozone (O3), and ammonia (NH3)] and tropospheric NO2 and O3 densities through Sentinel-5 satellite data approximately 1 d post-lockdown and one month pre-lockdown and post-lockdown. Our findings revealed a marked reduction in the ambient AQI (estimated mean reduction of 17.75% and 20.70%, respectively), tropospheric NO2 density, and land surface temperature (LST) during post-lockdown compared with the pre-lockdown period or corresponding months in 2019, except for a few sites with substantial coal mining and active power plants. We observed a modest increase in the O3 density post-lockdown, thereby indicating improved tropospheric air quality. As a favorable outcome of the COVID-19 lockdown, road accident-related mortalities declined by 72-folds. Cities with poor air quality correlate with higher COVID-19 cases and deaths (r = 0.504 and r = 0.590 for NO2; r = 0.744 and r = 0.435 for AQI). Conversely, low mortality was reported in cities with better air quality. These results show a correlation between the COVID-19 vulnerable regions and AQI hotspots, thereby suggesting that air pollution may exacerbate clinical manifestations of the disease. However, a prolonged lockdown may nullify the beneficial environmental outcomes by adversely affecting socioeconomic and health aspects.
Keywords: COVID-19, Ground AQI, Tropospheric pollutants, Pandemic lockdown, India
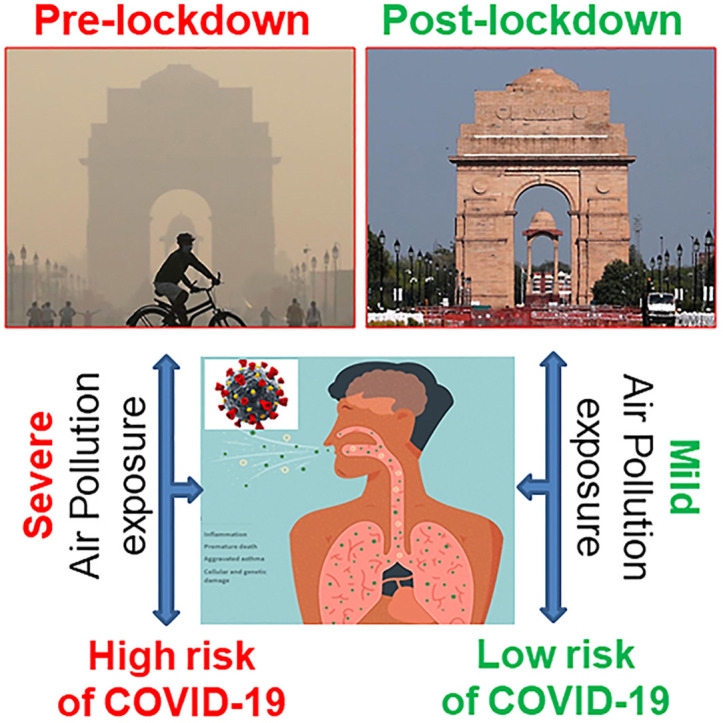
Graphical abstract
1. Introduction
The year 2020 commenced with the incidence of a highly contagious SARS-CoV-2 that rapidly spread worldwide and declared a pandemic by the World Health Organization (WHO) (Huang et al., 2020; Cucinatta and Venelli, 2020). The first cases of pneumonia-associated with coronavirus (COVID-19) were reported at the end of 2019 in Wuhan, China (Huang et al., 2020), and became a worldwide public health concern (Chen et al., 2020a; Gilbert et al., 2020). In India, the first case of SARS-CoV-2 was reported in Kerala State in January 2020 (Gautam and Hens, 2020). India is a densely populated country, and owing to the fear of spreading SARS-CoV-2 infection, a nationwide lockdown was imposed on March 24, 2020 for three weeks up to April 14, and was later extended until the end of June.
As a beneficial impact of the COVID-19 lockdown, pollution levels have been significantly reduced in different nations worldwide, such as major cities in China, the United States (US), Italy, and Brazil (Dutheil et al., 2020; Zangari et al., 2020; Xiang et al., 2020; Conticini et al., 2020; Krecl et al., 2020). A report published by the Centre for Research on Energy and Clean Air also highlighted that the decline in power generation from coal and lower oil consumption in Europe are responsible for an average reduction of 40% and 10% in nitrogen dioxide (NO2) and particulate matter (PM) pollution, respectively. They estimated approximately 11000 avoided deaths from air pollution (AP) during COVID-19 lockdown (Myllyvirta and Thieriot, 2020). A recent study showed a reduction in the tropospheric NO2 across India using Sentinel-5P satellite images, and noted a decline in NO2 emissions of approximately 40%–50% in the cities of Mumbai and Delhi (Shehzad et al., 2020). However, a systematic and comprehensive analysis of the COVID-19 lockdown on AP in India and its impact on mortality has not been conducted.
AP contributes to elevated morbidity and mortality rates globally (Sanyal et al., 2018; Wong et al., 2010), with 12.4 million deaths reported in 2016 (Balakrishnan et al., 2018). A study conducted by Forouzanfar et al. (2015) also highlighted AP as a causative factor that damages body systems and organs, particularly the respiratory and cardiovascular systems, which is ultimately responsible for 4.2 million deaths (7.6% of the total global deaths). The significant ancillary roles of AP have been observed in 16% of lung cancer deaths, 25% of chronic obstructive pulmonary disease deaths, 17% of heart ailments, and 26% of respiratory infection deaths. Suspended particulate matter (SPM) constitutes a major fraction of the AP and classified as PM10 (diameter ≤10 μm) or PM2.5 (diameter ≤2.5 μm) based on the aerodynamic diameter. The association between high concentrations of PM and adverse health outcomes is known (WHO, 2016; Cohen et al., 2017). India is the third-most polluted country in the world, with 1.24 million deaths related to AP in 2017, which amounted to 12.5% of the total deaths recorded in that year (https://ourworldindata.org/country/india). Over the past three decades, the Indian government has adopted numerous policies to curtail AP with limited success (WHO, 2018).
Qin et al. (2020) examined a correlation between high mortality and atmospheric pollution and they showed that communities living in polluted areas are more susceptible to COVID-19 due to inhalation of toxic pollutants for a prolonged time. Another study found that long-term exposure to poor air quality increases vulnerability to the incidence of more severe outcomes from COVID-19 (Wu et al., 2020). Poor air quality generally suppresses the immune system, which may exacerbate virus replication and diminish virus clearance by the host (Viehmann et al., 2015; Schraufnagel et al., 2019). AP can aggravate symptoms in individuals with respiratory infections, which can lead to the risk of hospitalization and death (Urrutia-Pereira et al., 2020). The present research demonstrated the post-lockdown improvement in air quality, associated mortalities through spatial mapping, and the relationship between AP and COVID-19 cases and mortalities in India.
2. Materials and methods
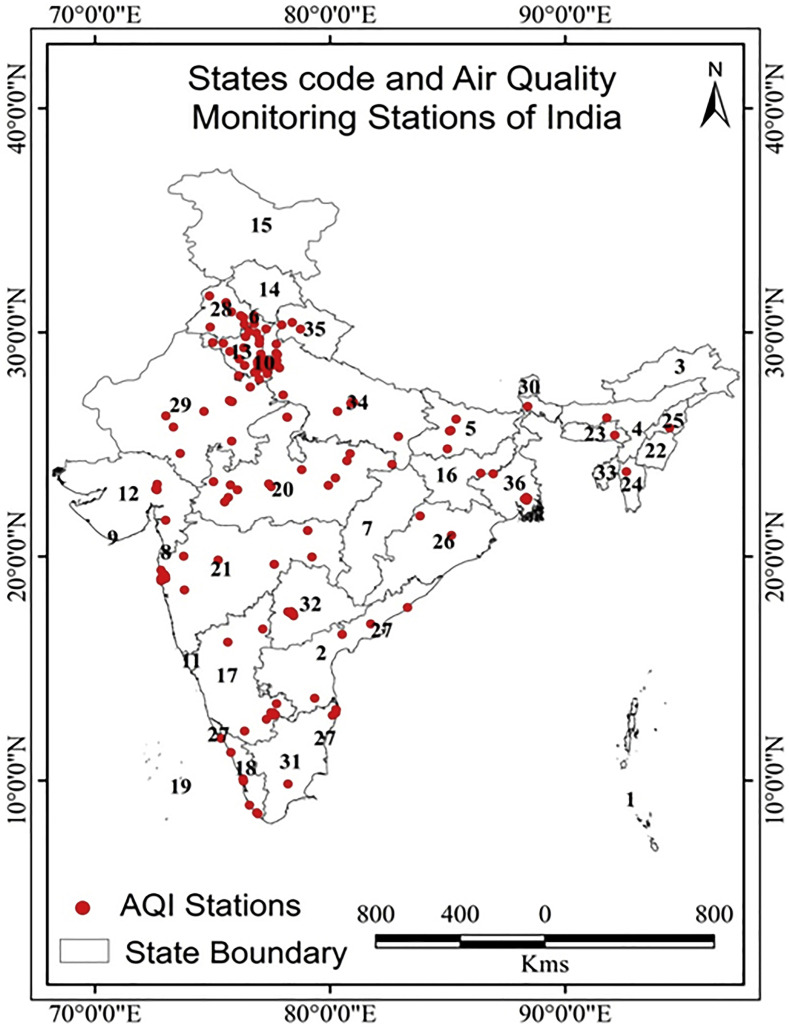
We employed various datasets to examine the immediate environmental impact of the COVID-19 lockdown and associated mortalities in India. Air quality index (AQI) data from 194 ground-monitoring stations (Fig. 1 ) and satellite data for tropospheric pollutants were used to assess the spatiotemporal variation in India.
Fig. 1.
Study area. Spatial locations of Air Quality Index (AQI) ground monitoring stations in the different states of India.
2.1. Data assimilation for the assessment of air pollution parameters
Remote sensing data were analyzed on Google Earth Engine, which allows geospatial analysis (Gorelick et al., 2017). NO2 and O3 data were collected from the Copernicus Sentinel-5 Precursor Tropospheric Monitoring Instrument, which is widely used for air quality-based applications (Veefkind et al., 2012) to monitor the daily changes in tropospheric NO2 column number density (Tobias et al., 2020). The in situ sensor used for the overall AQI data (including ambient PM10, PM2.5, NO2, SO2, CO, O3, and NH3) was procured for pre-lockdown (February 25, 2020 and March 20, 2020) and post-lockdown (March 25, 2020 and April 25, 2020) from the Central Pollution Control Board (CPCB) website (Air Pollution Monitoring Data of India. Central Pollution Control Board) under the Ministry of Environment, Forests and Climate Change. To ascertain that the changes in air quality in 2020 were related to the COVID-19 lockdown, we compared different parameters for the corresponding period in 2019. We chose to perform a single year comparison based on the previously published literature, where only 2019 was used as a control period (Singh et al., 2020; Mesas-Carrascosa et al., 2020). The spatial distribution and variation in AQI data were interpolated using the inverse distance weighted (IDW) method. The IDW estimate is equal to the spatial mean of all sampled points and is one of the most widely used interpolation methods for generating real-time AQI spatial predictions (Eberly et al., 2004). To examine the impact of the COVID-19 lockdown on tropospheric air quality, we procured 5 d mean data of tropospheric NO2 and O3 column number densities (mol/m2) before the lockdown (February 25–29, 2020), immediately after the lockdown (March 25–30, 2020), and almost one month after the lockdown (April 20–25, 2020) for India. For land surface temperature (LST) analysis and spatial variation, MOD11A1.006 Terra Land Surface Temperature and Emissivity Daily Global 1 km data products (Wan et al., 2015) were procured for March 25–30 and April 25–30 of 2019 and 2020 (during lockdown).
2.2. Air pollution and COVID-19-associated mortalities and correlation analysis
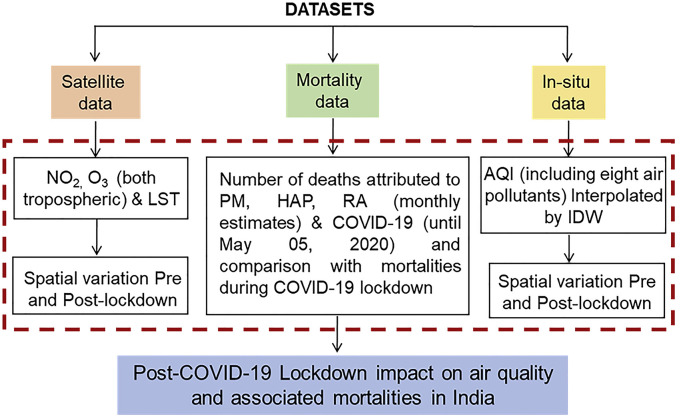
Statewide data for PM-related and household air pollution (HAP)-related deaths were procured from Balakrishnan et al. (2018), with yearly rates converted to monthly estimates. Monthly road accident (RA) deaths for each state were estimated using data from the Ministry of Road Transport & Highway Transport Research Wing (MoRTHTRW, 2019) and projected on a map. All the estimated datasets for PM, HAP, and RA were obtained for one month to include the COVID-19 lockdown period (March 25 to April 25, 2020) to estimate the monthly mortalities, and were represented using the graduated color map method using ArcMap software (version 10.3). For the same period, COVID-19 cases and deaths were obtained from different portals handled by the Ministry of Health & Family Welfare (COVID-19 Data of India. Ministry of Health & Family Welfare; COVID-19 Data of India). Regression and correlation analyses (Pearson correlation) were performed for a few sampled metropolitan cities (based on data availability up to May 5, 2020) with high and low air quality concentrations using ambient NO2 (μg/m3) and AQI (mainly dominated by SPM) pollution data. A schematic of the data collection sources and methodology adopted for the study is shown in Fig. 2 .
Fig. 2.
Datasets and methodology used for the study. Schematic depicting detailed data assimilation for ambient and tropospheric pollutants, PM-, HAP- and RA-attributed mortalities, and COVID-19 infections/mortalities.
3. Results and discussion
3.1. Significant improvement in air quality by the COVID-19 lockdown in India
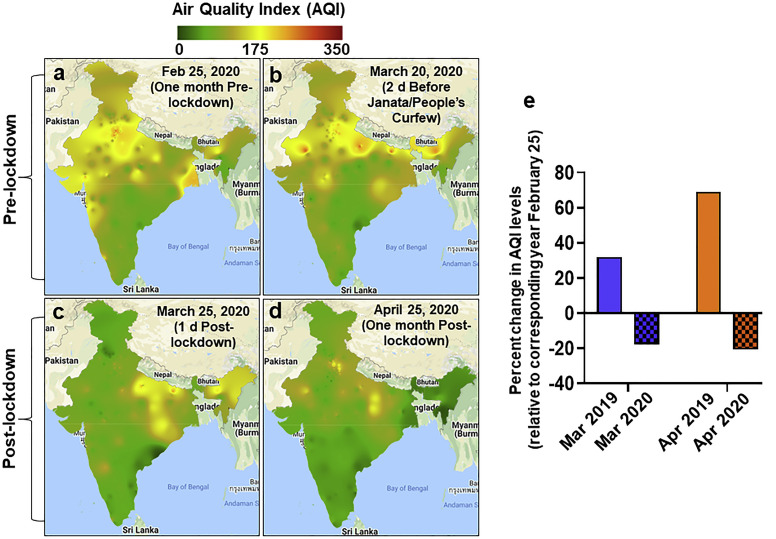
With the first sign that there might be a mass transmission of COVID-19 in the subcontinent, India imposed a strict lockdown starting on March 25, 2020 as a precautionary measure to curb the spread of the pandemic. Our results showed that the AQI across India remained similar one month pre-lockdown and 2 d before the Janata/People’s Curfew (Fig. 3 a and b; Table S1). A marked reduction in AQI was observed 1 d post-lockdown for most of the stations (Fig. 3c). The air quality improved one month post-lockdown with further reduction nationally (Fig. 3d). The direct and immediate impact of the lockdown was reflected by an estimated mean reduction of 17.75% and 20.70% in the AQI for 1 d and one month post-lockdown, respectively, compared to one month pre-lockdown (Fig. 3e). A similar analysis for 2019 showed a significant increase in AQI pollutant concentrations from February 25, 2019 to March 25, 2019 (32.00%) or April 25, 2019 (69.15%) (Fig. 3e). However, coal mining and steel producing states, including Chhattisgarh, Odisha, Bihar, and Jharkhand, continued to show poor air quality that could be attributed to uninterrupted industrial activity. These regions naturally generate NO2 from the coal mine belt; therefore, no changes were observed before or after the lockdown. In most of the Indian cities/regions, traffic emissions predominantly contributed to NO2 concentrations and showed a marked reduction following the COVID-19 lockdown. These observations suggest that AP could be improved in a short time period and highlight the predominant role of anthropological factors in augmenting AP in India. Our findings strongly suggest that the COVID-19 lockdown effectively reduced the overall AP throughout India.
Fig. 3.
Improvement in air quality index (AQI) concentrations following the COVID-19 lockdown in India. Spatial variations in AQI a. one month pre-lockdown, b. 2 d before the Janata/People’s Curfew, c. 1 d post-lockdown, and d. one month post-lockdown. e. Histogram showing the percent change in mean AQI concentrations for March (1 d post-lockdown) and April (one month post-lockdown) relative to those in February (one month pre-lockdown). A similar analysis for the corresponding period in 2019 was also performed to compare the direct impact of the lockdown on air quality.
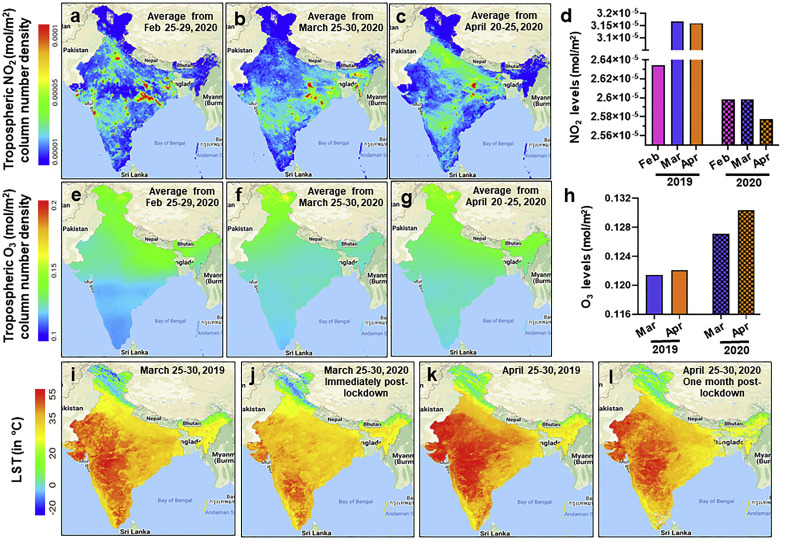
Next, we examined the tropospheric NO2 and O3 (mol/m2) densities, which indicate air quality. Compared to the pre-lockdown, national NO2 concentrations were reduced (Fig. 4 a–c), while the O3 density concurrently increased post-lockdown (Fig. 4e–g). The mean NO2 values gradually decreased from pre-lockdown (2.591E-05 mol/m2) to one month post-lockdown (2.577E-05 mol/m2), but no difference was observed for 1 d post-lockdown (2.591E-05 mol/m2) (Fig. 4d). On the contrary, the NO2 density (mol/m2) increased in March and April 2019 compared with that in February 2019 (Figs. S1a–c). The O3 (mol/m2) density improved one month post-lockdown (0.130 mol/m2) compared with the pre-lockdown level (0.128 mol/m2), while the 1 d post-lockdown value did not fluctuate (0.127 mol/m2) (Fig. 4h). However, no substantial difference in O3 density was observed in March and April of the previous year (2019) (Figs. S1d–f). Unlike the AQI parameters which are suspended air pollutants, NO2 and O3 (mol/m2) are tropospheric air quality indicators that may not change significantly in a short period; however, we noticed encouraging improvements in these indexes. In addition, compared with that in the same period in 2019, the LST analysis showed an encouraging reduction (approximately 2.5 °C) post-lockdown across the subcontinent (Fig. 4i–l). In 2019, the tropospheric densities of NO2 and O3 (mol/m2) did not improve in the hotspot regions throughout the month (Fig. S1). These observations suggest that the decrease in LST could be related to a concurrent modest reduction in ambient air quality (including PM), the tropospheric density of NO2, and improved O3 concentrations post-lockdown. AP can decrease the amount of sunlight that reaches the Earth because particles scatter and absorb solar radiation. Our findings of the correlation between LST and AP corroborate those of previous studies (Song et al., 2018; Feizizadeh and Blaschke, 2013). For instance, Song et al. (2018) analyzed the global LST from 2001 to 2016 and demonstrated an increase in LST with a modest increase in PM2.5 concentrations. However, a reduction in LST was observed with a marked increase in PM2.5. This surface temperature rise is at least partially caused by an increase in atmospheric greenhouse gases that can trap emitted energy. The relationship between LST and AP was assessed in Tabriz, Iran, and a strong correlation between highly polluted areas and LST was identified (Feizizadeh and Blaschke, 2013). Overall, our results clearly show that major air quality indicators improved gradually but considerably over one month post-COVID-19 lockdown and indirectly reduced the LST.
Fig. 4.
Restoration of NO2, O3, and land surface temperature (LST) post-COVID-19 lockdown. Spatial distribution and deviations in tropospheric a–c. NO2 and e–g. O3 concentrations over India derived from Sentinel-5 satellite data for the indicated period. Histograms showing improvement in tropospheric d. NO2 density and h. O3 density (5 d mean) one month post-lockdown compared with one month pre-lockdown or immediately post-lockdown. For comparison, the tropospheric densities of NO2 and O3 are included for the same period in 2019. i–l. Spatial distribution of LST (°C) immediately after lockdown and one month post-lockdown compared with that in the corresponding period in 2019.
3.2. Beneficial outcomes of the COVID-19 lockdown on air pollution-attributed monthly mortalities
Having established an association between the COVID-19 lockdown and superior air quality, we next examined its beneficial impact on mortality. The number of deaths attributed to COVID-19 (COVID-19 Data of India. Ministry of Health & Family Welfare), PM, HAP from Balakrishnan et al. (2018), and RA records (MoRTHTRW, 2019) were procured. The number of reported COVID-19 deaths (until May 5, 2020) was 1152, which was considerably lower compared with PM-, HAP-, or RA-related mortalities (Fig. 5 a; Table S2). The mean monthly PM, HAP, and RA concentrations accounted for 56094, 40144, and 12610 deaths, respectively. The spatial distribution of the estimated monthly PM, HAP, and RA mortalities is shown in Fig. 5b–d. Overall, Uttar Pradesh, Maharashtra, Haryana, and Rajasthan were the leading states among all the aforementioned mortality categories. In the case of RAs, Uttar Pradesh, Maharashtra, Tamil Nadu, and Rajasthan led the mortality charts. The monthly incident rate (per 100,000) of RAs during the lockdown was 0.04, compared with 2.90 for 2018, which amounted to a reduction of approximately 72-folds.
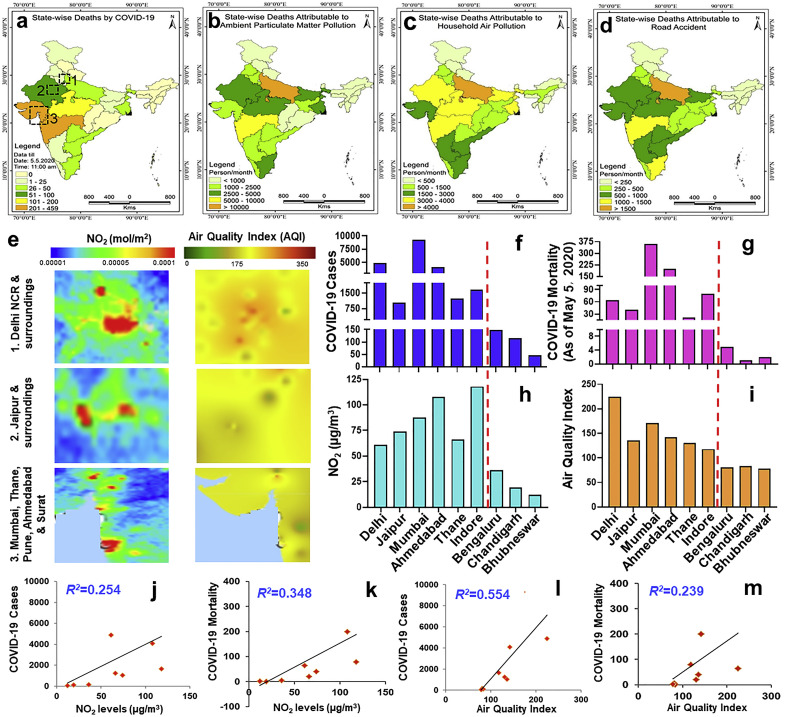
Fig. 5.
Decline in AP-attributed mortalities during COVID-19 lockdown and correlation of AP with COVID-19 cases/mortalities. Statewide estimation of monthly mortalities attributed to a. COVID-19, b. particulate matter, c. household air pollution, and d. road accidents. Regions (labelled 1, 2, and 3) with the highest COVID-19 mortalities (as of May 5, 2020) are highlighted in panel a. e. Spatial distribution of NO2 (tropospheric) and AQI in the COVID-19 vulnerable regions (highlighted in panel a). Histograms showing a comparison of f. COVID-19 cases, g. COVID-19 mortalities, h. ambient NO2, and i. AQI in metropolitan cities with severe or low air quality (separated by a dotted red line). Regression analysis of COVID-19 cases and mortalities with j. and k. NO2 (μg/m3) and l. and m. AQI, respectively. (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
3.3. Correlation between COVID-19 mortalities and air pollution
Our data showed that Maharashtra, Gujarat, Rajasthan, Madhya Pradesh, and Delhi contributed to approximately 70% of the COVID-19 afflictions. Some of the leading cities projecting the highest COVID-19 mortality in these states were Mumbai, Thane, Pune (Maharashtra), Ahmedabad, Surat (Gujarat), Indore (Madhya Pradesh), Jaipur (Rajasthan), and Delhi (COVID-19 Data of India. Ministry of Health & Family Welfare COVID-19 Data of India). The COVID-19 vulnerable regions were correlated with AQI hotspots, thereby suggesting that AP may exacerbate the clinical manifestations of the disease (Fig. 5e). The AQI is mainly dominated by the sub-index of SPM, and its strong relationships with infectious diseases and virus spread have been highlighted previously (Sedlmaier et al., 2009; Zhao et al., 2019). To verify this correlation, we further compared the AQI concentration and COVID-19 (both cases and mortalities) in nine metropolitan cities (six with high and three with low–moderate AP) across India. Cities with poor air quality were correlated with higher COVID-19 cases and deaths; conversely, low mortality was reported in cities with better air quality (Fig. 5f–i). Pearson correlation analysis showed a satisfactory association between the ambient NO2 (μg/m3) concentration and COVID-19 cases (r = 0.504; R 2 = 0.254; p = 0.045) and deaths (r = 0.59; R 2 = 0.348; p = 0.62) (Fig. 5j and k). Compared with that of NO2 (μg/m3), a strong correlation was observed between the AQI and COVID-19 cases (r = 0.744; R 2 = 0.554; p = 0.050) and deaths (r = 0.435; R 2 = 0.239; p = 0.33) (Fig. 5l, m). Our findings corroborate previous studies showing that long-term exposure to PM exacerbates the severity of the COVID-19 infection symptoms and high mortality rates (Wu et al., 2020; Setti et al., 2020). Analysis of exposure to AP and COVID-19 mortality in the US showed that an increase in PM2.5 by 1 g/m3 is associated with an approximately 15% rise in the COVID-19 death rate (Wu et al., 2020). Setti et al. (2020) demonstrated that a higher PM10 value could be a significant predictor of COVID-19 infection. They showed that northern Italian provinces with high PM10 had a median of 0.26 cases per 1000 residents, while southern provinces with low PM10 had a median of 0.03 infection cases per1000 residents. In addition to that with COVID-19, a correlation between air pollutants and the infection rate of other viruses, including respiratory syncytial virus (RSV) and measles, has been previously reported (Ye et al., 2016; Cheng et al., 2017). An association analysis between the RSV infection rate and PM2.5 (r = 0.446; p < 0.001) and PM10 (r = 0.397; p < 0.001) identified a positive correlation (Ye et al., 2016). Our data also showed a similar correlation between the AQI (which includes PM fractions) and COVID-19 cases (r = 0.744; p = 0.050) and mortality (r = 0.435; p = 0.33). Another study conducted by Chen et al. (2017) showed that an increase in PM2.5 equal to 10 μg/m3 is associated with a higher incidence of measles. Strategies aimed at mitigating AQI pollutants can slow the infection diffusion rate and contain the virus spread. These results show that PM and other pollutants can predict the spread and severity of virus-related pandemics in the future.
We acknowledge the limitations of this study, including the short study period, low cases of infection and mortality, and spatial uncertainty of IDW predictions. The objective of this study was to examine the immediate early impact of the COVID-19 lockdown on AP in the Indian subcontinent. These observations provide scientific evidence of the rapid environmental impact of the national pandemic response. In India, COVID-19 spread slowly until May 5, 2020 and began to exponentially increase after May 2020. Low cases of COVID-19 infection and mortality reported during the study period could also skew the correlation analysis. However, we specifically selected metropolitan cities with ≥1000 cases. We focused on the early spread in metropolitan cities with severe and low–moderate AP. Another limitation is the sparse spatial locations of the monitoring stations. This is primarily attributed to the limited number of air quality monitoring stations provided by the CPCB. In addition, some of the stations lacked complete AQI datasets; therefore, they were not included.
4. Conclusion
Our results showed that the COVID-19 lockdown was highly beneficial in reducing AP in India, one of the most polluted nations, in a relatively short period. The AQI was markedly improved post-lockdown compared with that pre-lockdown or in the corresponding month in 2019. In addition to ambient air quality, positive outcomes in the tropospheric NO2, O3, and LST values were observed. Our results provide strong evidence for a correlation between the COVID-19 lockdown and improvement in AQI parameters in India, except for the coal mining regions. This heterogeneity could be attributed to the incessant natural production of NO2 (and other greenhouse gases) from the coal mines; these areas showed no improvement post-lockdown, while anthropogenic-induced emissions in other regions showed a marked reduction following the COVID-19 lockdown. The COVID-19 lockdown reduced the mortalities associated with environmental pollutants and may additionally have a beneficial impact by curtailing RAs and numerous life-threatening chronic diseases attributed to these air pollutants. In addition to statistical correlation, our tropospheric NO2 and AQI spatial distribution also support a strong relationship between air pollutant concentration and COVID-19 cases/mortality. Our findings corroborate a recent study showing a possible correlation between AP (especially NO2) and COVID-19 mortality (Wu et al., 2020; Chen et al., 2020). We acknowledge that this analysis requires further investigation owing to the lack of data availability for all metropolitan cities in India. If this lockdown continues for a longer period, the beneficial impact in India maybe overshadowed by other emerging factors such as household pollution, increasing incidences of domestic violence, suicides, mental health concerns in adults and children, and rising food insecurity among the unemployed.
Credit author statement
Hasan Raja Naqvi: Conceptualization, Methodology, Validation, Formal analysis, Investigation, Resources, Writing - original draft, Reviewing and Editing. Manali Dutta: Conceptualization, Investigation, Resources, Writing - original draft. Guneet Mutreja: Methodology, Validation, Formal analysis, Resources. Masood Ahsan Siddiqui: Resources, Writing- Reviewing and Editing. Daraksha Fatima Naqvi: Validation, Formal analysis, Resources. Afsar Naqvi: Conceptualization, Investigation, Resources, Writing - original draft, Reviewing and Editing.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We thanks the editor and the anonymous reviewers for their useful suggestions. We also thank Nuzhat Arzoo for her help with graphical abstract.
Footnotes
This paper has been recommended for acceptance by Admir C. Targino.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.envpol.2020.115691.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Balakrishnan K. The impact of air pollution on deaths, disease burden, and life expectancy across the states of India: the Global Burden of Disease Study 2017. Lancet Planet. Health. 2018;5196(18) doi: 10.1016/S2542-5196(18)30261-4. 30261-30244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen G., Zhang W., Li S., Williams G., Liu C., Morgan G.G., Jaakkola J.J.K., Guo Y. Is short-term exposure to ambient fine particles associated with measles incidence in China? A multi-city study. Environ. Res. 2017;156:306–311. doi: 10.1016/j.envres.2017.03.046. [DOI] [PubMed] [Google Scholar]
- Chen H., Guo J., Wang C. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020;395:809–815. doi: 10.1016/S0140-6736(20)30360-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen K. Air pollution reduction and mortality benefit during the COVID-19 outbreak in China. Lancet Planet Health. 2020 doi: 10.1016/S2542-5196(20)30107-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen A.J. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015. Lancet. 2017;389:1907–1918. doi: 10.1016/S0140-6736(17)30505-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conticini E., Frediani B., Caro D. Can atmospheric pollution be considered a co-factor in extremely high level of SARS-CoV-2 lethality in Northern Italy?∗. Environ. Pollut. 2020;261:114465. doi: 10.1016/j.envpol.2020.114465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cucinotta D., Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020;91:157-160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- COVID-19 Data of India. Ministry of Health & Family Welfare, Government of India. (https://www.mohfw.gov.in/) Accessed on 5 May 2020.
- Dutheil F. COVID-19 as a factor influencing air pollution? Environ. Pollut. 2020 doi: 10.1016/j.envpol.2020.114466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eberly S. 2004. Developing Spatially Interpolated Surfaces and Estimating Uncertainty. Publication No. EPA-454/R-04-004, 159p. [Google Scholar]
- Feizizadeh B., Blaschke T. Examining urban heat island relations to land use and air pollution: multiple endmember spectral mixture analysis for thermal remote sensing. IEEE J. Sel. Top. Appl. Earth Observ. Rem. Sens. 2013;6(3):1749–1756. doi: 10.1109/jstars.2013.2263425. [DOI] [Google Scholar]
- Forouzanfar M.H., Afshin A., Alexander L.T., Anderson H.B., Brutta Z.A., Birykov S. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2015: a systematic analysis for the global burden of disease study. Lancet. 2015;388(10053):1659–1724. doi: 10.1016/S0140-6736(16)31679-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gautam S., Hens L. SARS-CoV-2 pandemic in India: what might we expect? Environ. Dev. Sustain. 2020;22:3867–3869. doi: 10.1007/s10668-020-00739-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert M., Pullano G., Pinotti F. Preparedness and vulnerability of African countries against importations of COVID-19: a modelling study. Lancet. 2020;395:871–877. doi: 10.1016/S0140-6736(20)30411-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorelick N. Google Earth engine: planetary-scale geospatial analysis for everyone. Remote Sens. Environ. 2017;202(2017):18–27. [Google Scholar]
- Huang C., Wang Y., Li X., Ren L. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20). [DOI] [PMC free article] [PubMed] [Google Scholar]
- COVID-19 Data of India. Government of India 2020. https://www.mygov.in/covid-19 Accessed on 5 May 2020.
- Krecl P., Targino A.C., Oukawa G.Y., Cassino Junior R.P. Drop in urban air pollution from COVID-19 pandemic: policy implications for the megacity of São Paulo. Environ. Pollut. 2020;265:114883. doi: 10.1016/j.envpol.2020.114883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mesas-Carrascosa F.J., Pérez Porras F., Triviño-Tarradas P., García-Ferrer A., Meroño-Larriva J.E. Effect of lockdown measures on atmospheric nitrogen dioxide during SARS-CoV-2 in Spain. Rem. Sens. 2020;12(14):210. doi: 10.3390/rs12142210. [DOI] [Google Scholar]
- Air Pollution Monitoring Data of India. Central Pollution Control Board. Ministry of Environment, Forest and Climate Change, Government of India. (https://cpcb.nic.in/) Accessed on 5 May 2020.
- Ministry of Road Transport & Highway Transport Research Wing (MoRTHTRW) 2019. Road Accidents in India 2018. Report on. [Google Scholar]
- Myllyvirta L., Thieriot H. 11.000 air pollution-related deaths avoided in Europe as coal, oil consumption plummet. 2020. https://energyandcleanair.org/wp/wp-content/uploads/2020/04/CREA-Europe-COVID-impacts.pdf Available in:
- Our world in data https://ourworldindata.org/country/india Available at:
- Qin C., Zhou L., Hu Z., Zhang S., Yang S., Tao Y., Xie C., Ma K., Shang K., Wang W., Tian S.D. Dysregulation of immune response in patients with COVID-19 in Wuhan, China. Clin. Infect. Dis. 2020 doi: 10.1093/cid/ciaa248. Accepted (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanyal S. Long-term effect of outdoor air pollution on mortality and morbidity: a 12-year follow-up study for metropolitan France. Int. J. Environ. Res. Publ. Health. 2018;15(11):2487. doi: 10.3390/ijerph15112487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schraufnagel D.E. Air pollution and non-communicable diseases: a review by the forum of international respiratory societies’ environmental committee, Part 2: air pollution and organ systems. Chest. 2019;155:417-426. doi: 10.1016/j.chest.2018.10.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sedlmaier N., Hoppenheidt K., Krist H., Lehmann S., Lang H., Buttner M. Generation of avian influenza virus (AIV) contaminated fecal fine particulate matter (PM2.5): genome and infectivity detection and calculation of immission. Vet. Microbiol. 2009;139:156–164. doi: 10.1016/j.vetmic.2009.05.005. [DOI] [PubMed] [Google Scholar]
- Setti L., Passarini F., De Gennaro G., Barbieri P., Perrone M.G., Borelli M. Airborne transmission route of COVID-19: why 2 meters/6 feet of inter-personal distance could not Be enough. Int. J. Environ. Res. Publ. Health. 2020;17(8):2932. doi: 10.3390/ijerph17082932.e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shehzad K., Sarfraz M., Meran Shah S.G. The impact of COVID-19 as a necessary evil on air pollution in India during the lockdown. Environ. Pollut. 2020;115080 doi: 10.1016/j.envpol.2020.115080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh R.P., Chauhan A. Impact of lockdown on air quality in India during COVID-19 pandemic. Air Qual Atmos Health. 2020;13:921–928. doi: 10.1007/s11869-020-00863-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song Z. Global land surface temperature influenced by vegetation cover and PM2.5 from 2001 to 2016. Rem. Sens. 2018;10:2034. doi: 10.3390/rs10122034. [DOI] [Google Scholar]
- Tobías A. Changes in air quality during the lockdown in Barcelona (Spain) one month into the SARS-CoV-2 epidemic. Sci. Total Environ. 2020;726:1–4. doi: 10.1016/j.scitotenv.2020.138540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urrutia-Pereira M., Mello-da-Silva C.A., Solé D. COVID-19 and air pollution: a dangerous association? Allergol. Immunopathol. 2020 doi: 10.1016/j.aller.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veefkind J.P. TROPOMI on the ESA Sentinel-5 Precursor: a GMES mission for global observations of the atmospheric composition for climate, air quality and ozone layer applications. Remote Sens. Environ. 2012;120:70–83. [Google Scholar]
- Viehmann A. Long-term residential exposure to urban air pollution, and repeated measures of systemic blood markers of inflammation and coagulation. Occup. Environ. Med. 2015;72:656-663. doi: 10.1136/oemed-2014-102800. [DOI] [PubMed] [Google Scholar]
- Wan Z., Hook S., Hulley G. NASA EOSDIS Land Processes DAAC; 2015. MOD11A1 MODIS/Terra Land Surface Temperature/Emissivity Daily L3 Global 1km SIN Grid V006 [Data Set] Accessed on 2020-05-19. [DOI] [Google Scholar]
- Wong C.M. vol. 154. Health Effects Institute; 2010. pp. 377–418. (Public Health and Air Pollution in Asia (PAPA): a Combined Analysis of Four Studies of Air Pollution and Mortality). Research Report. [PubMed] [Google Scholar]
- World Health Organization (WHO) 2016. Mortality and Burden of Disease from Ambient Air Pollution, Situation and Trends.https://www.who.int/gho/phe/outdoor_air_pollution/burden_text/en/ [Google Scholar]
- World Health Organization (WHO) India takes steps to curb air pollution. Bull. World Health Organ. 2018;94:487–488. doi: 10.2471/BLT.16.020716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu X. 2020. Exposure to Air Pollution and COVID-19 Mortality in the United States: A Nationwide Cross-Sectional Study.https://www.medrxiv.org/content/10.1101/2020.04.05.20054502v2 Preprint at. [Google Scholar]
- Xiang J., Austin E., Gould T. Science of the Total Environment; 2020. Impacts of the COVID-19 Responses on Traffic-Related Air Pollution in a Northwestern US City. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye Q., Fu J.F., Mao J.H., Shang S.Q. Haze is a risk factor contributing to the rapid spread of respiratory syncytial virus in children. Environ. Sci. Pollut. Res. 2016;23 doi: 10.1007/s11356-016-7228-6. 20178–20185. [DOI] [PubMed] [Google Scholar]
- Zangari S., Hill D.T., Charette A.T., Mirowsky J.E. Air quality changes in New York City during the COVID-19 pandemic. Sci. Total Environ. 2020;742:140496. doi: 10.1016/j.scitotenv.2020.140496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Y., Richardson B., Takle E., Chai L., Schmitt D., Win H. Airborne transmission may have played a role in the spread of 2015 highly pathogenic avian influenza outbreaks in the United States. Sci. Rep. 2019;9:11755. doi: 10.1038/s41598-019-47788-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.