Abstract
AIM
To demonstrate local dry vitrectomy combined with segmental scleral buckling and viscoelastic tamponade for the treatment of partial rhegmatogenous retinal detachment (RRD) with local vitreous traction in patients at high-risk for proliferative vitreoretinopathy (PVR).
METHODS
Eleven eyes of 11 patients were retrospectively studied, including 5 retinal dialysis and 6 retinal detachment (RD; 5 eyes with peripheral retinal hole and 1 eye with giant tear). All patients exhibited partial RD and local vitreous traction. Combined local dry vitrectomy without conventional infusion and segmental scleral buckling was performed. Viscoelastic fluid was injected into the vitreous cavity if needed. Demographic information, preoperative and post-operative complications, and outcomes were recorded.
RESULTS
The mean age of the patients at presentation was 26.55±13.52y. All 11 patients obtained retinal reattachment after a single surgical intervention. Postoperative visual acuities were improved or remained stable in all patients. None of them developed complications, except for temporary mildly increased intraocular pressure in 3 cases.
CONCLUSION
Combined local dry vitrectomy and segmental scleral buckling are effective for patients of RRD with local vitreous traction. The technique avoids many complications associated with regular surgery and was minimally invasive to both the external and internal eye.
Keywords: dry vitrectomy, retinal detachment, scleral buckling
INTRODUCTION
Primary rhegmatogenous retinal detachment (RRD) is an important condition encountered in retinal clinics. The annual RRD incidence has been reported to be 5.4-18.2 per 100 000 people with a peak incidence of 52.5 per 100 000 people of 55- to 59-year-old[1]–[4]. RRD can be surgically treated using scleral buckling, and/or pars plana vitrectomy (PPV)[5]–[9]. However, different types of retinal detachments (RDs) behave differently and may need special considerations in the selection of surgical procedures[10]. Proliferative vitreoretinopathy (PVR) causing membrane formation and traction occurs in 5%-10% of all RRD and is implicated in redetachment after surgery in 75% of cases[11]. In RRD patients without posterior vitreous detachment (PVD) at high risk for PVR with vitreous traction, performing segmental scleral buckling alone poses a significant surgical challenge because persistent vitreous traction may lead to failure of the surgery[12]. However, conventional vitrectomy has some potential complications, such as cataract formation, especially in young patients. Vitrectomy may also result in more diffuse vitreous-base disruption if the vitreous base is shaved over the peripheral retina and pars plana during aggressive vitreous removal[13]. Pneumatic retinopexy is a minimally invasive, non-incisional procedure for repairing RD, but successful retinal re-attachment will only be achieved when strict selection criteria are applied. It is primarily indicated for the repair of uncomplicated RDs without PVR[14].
The objective of this article is to introduce a modified technique that combines local dry vitrectomy (without regular infusion) and segmental scleral buckling, and to demonstrate the applicability of managing RRD in patients without PVD at high risks for PVR, especially in young patients.
SUBJECTS AND METHODS
Ethical Approval
This study was approved by the Ethics Committee of Xinhua Hospital Affiliated to Shanghai Jiao Tong University School of Medicine. Informed consent was obtained from all individual participants or his/her legal guardians if under 18y.
Subjects
The indications for this combined surgery were partial RRD with local vitreous traction around the retinal hole or tear with preoperative PVR B or C[15]. No one had PVD preoperatively. The following situations would be considered but not mandatory when making the decision, such as young age, macula-on status, and good preoperative visual acuity of the operated eye, since conventional vitrectomy may lead to more complications, such as cataract formation. All surgeries were performed by one surgeon (Zhao PQ). All patients underwent comprehensive ophthalmic examinations before surgical intervention including fundus photography, B-scan, slit-lamp examination, and indirect biomicroscopy. Medical history, best-corrected visual acuity (BCVA) and intraocular pressure (IOP) were also taken.
Surgical Technique
Making conjunctival incision for segmental scleral buckling according to the range and location of the retinal breaks
If the retinal hole was small, minimal in situ radial conjunctival incision (5 to 6 mm) was made[16]. If the retinal break or dialysis was extensive, the conjunctiva was dissected at the limbus. Transconjunctival traction sutures were placed under the rectus muscles.
Local dry vitrectomy
Three-port (or 2-port) sclerotomies were made 3.5-4 mm from the limbus. Dry local vitrectomy without balanced salt solution (BSS) plus liquid infusion by 23-gauge vitreous cutter was performed to remove the vitreous traction and the margin was trimmed around the retinal break under a noncontact wide-angle viewing system, or under microscopy directly with scleral depression if the retinal tear was in the periphery, such as retinal dialysis. Viscoelastic fluid was injected into the vitreous cavity to maintain IOP if needed through one of the ports during the operation.
Scleral buckling
After cryopexy, the precise location of the retinal break was marked. One or two explants (silicone/silicone sponge) were placed according to the extent of the break to perform scleral buckling. The Tenon's capsule and the conjunctiva ere sutured.
RESULTS
Eleven eyes of eleven patients were included in this series: 5 retinal dialysis and 6 RDs (5 eyes with peripheral retinal hole and 1 eye with giant tear). All patients exhibited local dense vitreous traction and a high risk for PVR.
Eight of the patients were male and three were female. The mean±SD age at presentation was 26.55±13.52y (range 7-48y), including four teenagers. All patients exhibited partial RD. Eight patients were macula-on at the time of surgery, with visual acuity of 20/40 or better. Three patients were macula-off, with visual acuity of 20/1000, 20/300 and 20/200. The average follow-up duration was 17.36±11.40 mo (range 3-43mo).
All eleven patients obtained retinal attachment after a single surgical intervention. Postoperative visual acuities were improved in eight patients and remained stable in three patients including 20/20 in 5 eyes, and 20/25 in 2 eyes, which were preoperative macula-on cases. No patients developed intraoperative and postoperative complications, except temporary mildly increased IOP in the 1st to 2nd week postoperatively in 3 cases (Table 1, Figures 1–3).
Table 1. Clinical characteristic of RRD patients.
| Case | Age | Eye | Diagnosis | Preoperative BCVA | RD | Retinal break | Preoperative PVR | Vitreous traction | Macular status | History of ocular surgery | Postoperative BCVA | Postoperative complications | Postoperative retinal status | Follow-up (mo) |
| 1 | 7 | OD | RRD, PHPV | 20/25 | 9 o'clock | Retinal hole, temporal | CP | + | On | - | 20/20 | - | Attached | 43 |
| 2 | 17 | OS | RRD | 20/1000 | 4 to 7 o'clock | Dialysis of ora serrata, temporal inferior | B | + | Off | - | 20/300 | - | Attached | 31 |
| 3 | 13 | OD | RRD, HM | 20/25 | 5:30 to 8 o'clock | Dialysis of ora serrata, temporal inferior | B | + | On | Fellow eye vitrectomy+ silicone oil tamponade | 20/25 | Temporarily mild increased IOP | Attached | 23 |
| 4 | 45 | OD | RRD, HM | 20/30 | 11 to 1 o'clock | Retinal hole, superior | B | + | On | Failure of photocoagulation | 20/20 | Temporarily mild increased IOP | Attached | 18 |
| 5 | 38 | OS | RRD | 20/300 | 3 to 6 o'clock | Giant break, temporal inferior | B | + | Off | - | 20/200 | - | Attached | 17 |
| 6 | 25 | OD | RRD | 20/30 | 12 to 2 o'clock | Dialysis of ora serrata, superior | B | + | On | - | 20/25 | - | Attached | 15 |
| 7 | 12 | OD | RRD | 20/40 | 11 to 4 o'clock | Retinal hole, temporal | CP | + | On | Fellow eye vitrectomy+ silicone oil tamponade | 20/20 | - | Attached | 8 |
| 8 | 27 | OD | RRD | 20/20 | 4:30 to 9:30 o'clock | Dialysis of ora serrata, Temporal inferior | B | + | On | Fellow eye vitrectomy+silicone oil tamponade | 20/20 | - | Attached | 12 |
| 9 | 31 | OS | RRD | 20/200 | 3:30 to 8:30 o'clock | Dialysis of ora serrata, temporal inferior | CP | + | Off | Fellow eye scleral buckling | 20/60 | - | Attached | 11 |
| 10 | 29 | OS | RRD, FEVR | 20/40 | 4 to 8 o'clock | Retinal hole, temporal inferior | B | + | On | Fellow eye scleral buckling | 20/40 | Temporarily mild increased IOP | Attached | 10 |
| 11 | 48 | OS | RRD | 20/20 | 6:30 to 8:30 o'clock | Retinal hole, inferior | B | + | On | - | 20/20 | - | Attached | 3 |
BCVA: Best corrected visual acuity; RRD: Rhegmatogenous retinal detachment; PHPV: Persistent hyperplastic primary vitreous; HM: High myopia; IOP: Intraocular pressure; FEVR: Familial exudative vitreoretinopathy.
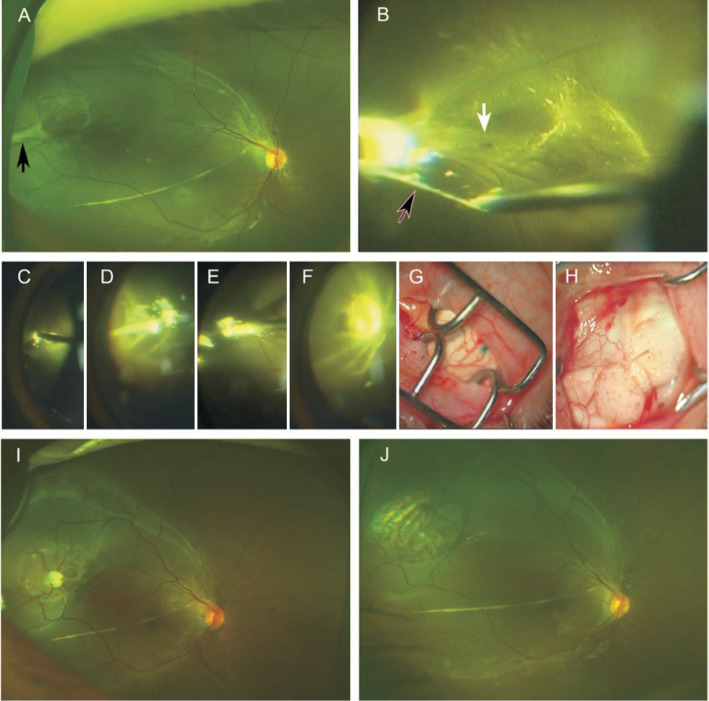
Figure 1. Case 1, a 7-year-old boy diagnosed as PHPV with temporal RD at the right eye.
A: Preoperative fundus photo. Black arrow shows the vitreous traction. B: Small retinal hole was found beneath the vitreous traction under the microscopy. C-H: Key steps of the surgical procedures; C: Coagulation of the vitreous traction; D: Cutting the vitreous traction; E: Trimming the traction by vitrectomy cutter; F: Cryocoagulation under microscopy; G, H: Minimal invasive conjunctival incision and silicone scleral buckle. I, J: Retinal reattachment with temporal ridge 2-day and 1-month after surgery, respectively.
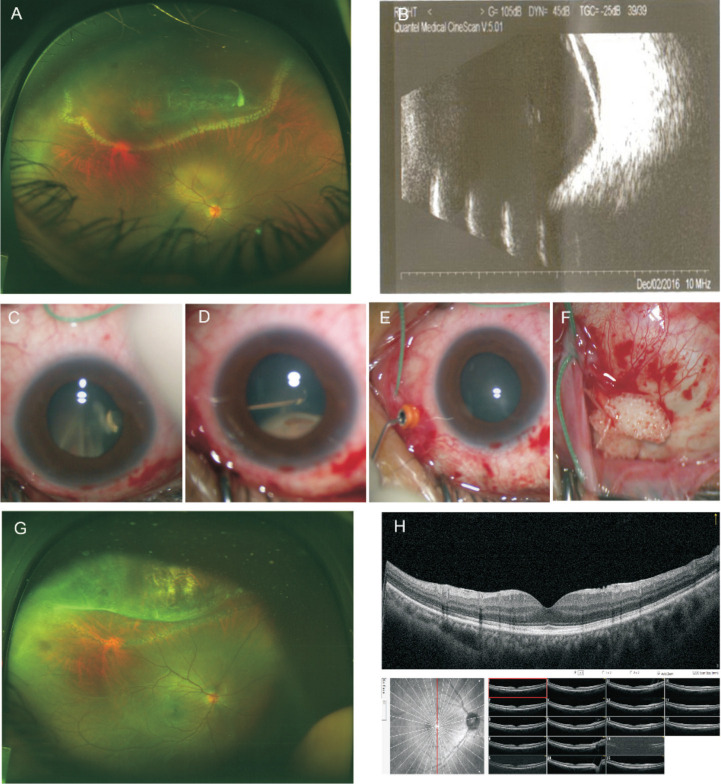
Figure 3. Case 4, a 45-year-old woman with superior RD at the right eye and high myopia of both eyes and had a history of retinal photocoagulation at the right eye.
A: Preoperative fundus photo showed RD with retinal holes and vitreous traction. Laser spot was seen around the posterior margin of the RD area. B: B-scans of the right eye preoperatively. C-F: The key steps of the surgical procedures. C, D: Trimming the vitreous traction around the retinal holes by vitrectomy cutter; E: Injecting the viscoelastic solution into the vitreous cavity to maintain the ocular pressure; F: Minimal invasive conjunctival incision and silicone scleral buckle. G: Postoperative fundus photo showed retinal reattachment. H: Postoperative OCT showed normal macula.
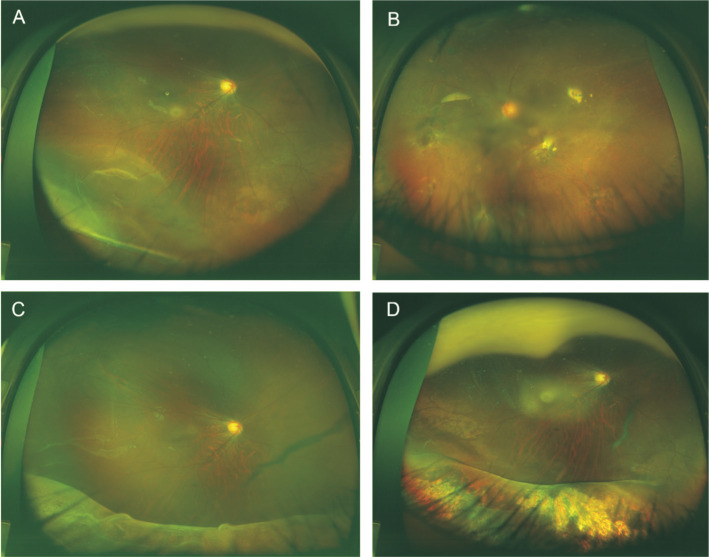
Figure 2. Case 3, a 13-year-old boy diagnosed as retinal dialysis at the right eye and had a history of vitrectomy at his left eye due to RD.
A: Retinal dialysis of right eye with vitreous traction around the dialysis of ora serrata; B: Fundus of left eye with silicone oil tamponade; C, D: Retinal reattachment of the right eye with inferior ridge 3-weeks and 3-months after combined local dry vitrectomy and minimal scleral buckling.
DISCUSSION
Surgical approaches for low-to-moderate complexity RDs have been well studied[12]–[13],[17]. The most common cause for surgical failure in RRD is PVR. However, less is known about surgical outcomes in patients at high risk for PVR. This study presented a new technique involving combined local dry vitrectomy and segmental scleral buckling in RRD patients without PVD at high risks for PVR.
Scleral buckling has been successfully used to repair RRDs for over 60y. Scleral buckling has an important role in the repair of certain categories of RRDs. These include detachments in young phakic patients, detachments associated with dialysis, and also in conjunction with vitrectomy in patients who sustain trauma or have developed PVR[18]. However, in patients of RRD with vitreous traction, who are also at high risk for PVR, performing segmental scleral buckling alone poses a significant surgical challenge because persistent vitreous traction may lead to failure of the surgery. For patients at high risk for PVR, PPV-scleral buckling has been associated with significantly higher anatomical success rate compared with PPV alone[12].
Although dialysis theoretically has a lower rate of PVR compared with RD in general and success rates of surgery for retinal dialysis were high, patients with PVR had very poor surgical outcome. In Qiang Kwong et al's study[19], the presence of PVR in retinal dialysis was a significant factor in cases of failed retinal reattachment (P<0.001). The strategies to deal with PVR in these patients need to be developed. There are three cases of retinal dialysis with PVR B in our case series. We performed combined local dry vitrectomy and segmental scleral buckling. All the patients obtained retinal re-attachment with good visual results.
All cases in the present study were partial RD, including five macula-on cases. The patients were young, and four were younger than 18 years old. Two teenage patients' fellow eye had poor visual acuity [counting fingers (FC)/40 cm (case 3) and FC/10 cm (case 7)] with a history of RD. We did not perform conventional vitrectomy because the minimal interference of the vitreous cavity may lead to better prognosis, especially in young patients with less cataract formation.
Lens opacification is a common complication following vitrectomy. Nuclear sclerotic cataract (NSC) is the most common type of cataract seen after vitrectomy. It is the most common cause of the post-operative decrease in visual acuity after successful treatment of the disease and may further requires surgical correction. In Shu et al's multicenter study[20], the incidences of cataract development within 1y after PPV was 6.5% versus 1.0% in the scleral buckle (SB) group. In Feng and Adelman's study[21], patients developed posterior subcapsular and NSC almost within 24mo after the surgery. The percentages of eyes with mild lens change were 96% after 20-gauge PPV, 72% after small gauge (23- and 25-gauge) PPV, 38% after SB, 38% after pneumatic retinopexy, and 91% after PPV plus SB. There was a statistically significant difference between PPV and non-PPV. There are several mechanisms which may contribute to the development of post-vitrectomy NSC. The main cause is probably oxidative stress. In a normal eye, the vitreous served as a barrier to the diffusion of oxygen from the retina into the vitreous gel. If vitreous gel liquefies with age or is removed by vitrectomy surgery, vitreous fluid can circulate delivering more oxygen to the lens[22]. After vitrectomy, such barrier was disrupted and the lens was exposed to higher concentration of oxygen than normal. Infusion fluids used during vitrectomy may also contribute to post-vitrectomy NSC[23]–[25]. The temporary increase of oxygen brought in by infusion fluid during the surgery may also expose lens to high oxygen challenge. Local dry vitrectomy only removes the vitreous limited to the vitreous traction around retinal hole, tear or retinal dialysis without fluid infusion, which limited the lens exposure to excessive oxidative stress both during the operation and post-operatively and may lead to less post-operative cataract formation.
Our case series suggests that this technique could be effective for partial RRD with local vitreous traction around the retinal hole or tear with preoperative PVR B or C. The following situations further favored the application of this technique: young age, macula-on status and good preoperative visual acuity. One case in our series was diagnosis as persistent hyperplastic primary vitreous (PHPV), so the results might not be generalizable to all RD.
The technique appeared to be safe. None of the cases experienced significant surgical complications intraoperatively or postoperatively. The entire procedure involves minimal surgical injury. The benefits of minimally invasive scleral buckling were well addressed in our previously published study[16]. Local limited dry vitrectomy can relieve vitreous traction with minimal disturbance of the vitreous cavity, avoid the potential negative effect of intraocular infusion solutions on the retina and carries less risk for PVR and cataract formation[26].
We observed minimal complications in 2 patients, who experienced mildly increased IOP 1 to 2wk postoperatively (cases 3 and 4). The IOP returned to normal 2 to 3wk after the operation. This was likely caused by the diffusion of the viscoelastic solution from the vitreous cavity into the anterior chamber via the fragile zonule. The IOP returned to normal after the absorbance of viscoelastic solution.
Limitations of this study also include a relatively small sample size and its retrospective design. Moreover, this was only a single surgeon's experience. A larger prospective cohort study involving multiple surgeons with longer follow-up time would be needed to assess the exact success and complication rates of this technique.
In summary, combined local dry vitrectomy and segmental scleral buckling was a highly successful method of managing RRD with local vitreous traction in patients at high risk for PVR, especially in young patients. Careful preoperative and intraoperative planning should be undertaken to achieve minimal invasiveness and the best postoperative visual results.
Acknowledgments
The manuscript was presented at the 120th Annual Meeting of the Korean Ophthalmological Society Organizing Committee (Seoul, Korea, Nov. 2, 2018).
Foundations: Supported by the National Natural Science Foundation of China (No.81770963; No.81500725; No.81770964); Shanghai Shen Kang Hospital Development Center Program (No.16CR4017A).
Conflicts of Interest: Fei P, None; Jin HY, None; Zhang Q, None; Peng J, None; Li JK, None; Lyu J, None; Tian T, None; Lu ZP, None; Li J, None; Zhao PQ, None.
REFERENCES
- 1.Park SJ, Choi NK, Park KH, Woo SJ. Five year nationwide incidence of rhegmatogenous retinal detachment requiring surgery in Korea. PLoS One. 2013;8(11):e80174. doi: 10.1371/journal.pone.0080174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li JQ, Welchowski T, Schmid M, Holz FG, Finger RP. Incidence of rhegmatogenous retinal detachment in Europe-a systematic review and Meta-analysis. Ophthalmologica. 2019;242(2):81–86. doi: 10.1159/000499489. [DOI] [PubMed] [Google Scholar]
- 3.van de Put MAJ, Hooymans JMM, Los LI. The incidence of rhegmatogenous retinal detachment in the Netherlands. Ophthalmology. 2013;120(3):616–622. doi: 10.1016/j.ophtha.2012.09.001. [DOI] [PubMed] [Google Scholar]
- 4.Bechrakis NE, Dimmer A. Rhegmatogenous retinal detachment: epidemiology and risk factors. Der Ophthalmol. 2018;115(2):163–178. doi: 10.1007/s00347-017-0647-z. [DOI] [PubMed] [Google Scholar]
- 5.Rijal RK, Byanju R, Pandey A, Mourya D. Anatomical and visual outcome of rhegmatogenous retinal detachment managed with scleral buckling at a tertiary eye centre in Nepal. Nep J Oph. 2018;10(2):151–155. doi: 10.3126/nepjoph.v10i2.18832. [DOI] [PubMed] [Google Scholar]
- 6.Eibenberger K, Georgopoulos M, Rezar-Dreindl S, Schmidt-Erfurth U, Sacu S. Development of surgical management in primary rhegmatogenous retinal detachment treatment from 2009 to 2015. Curr Eye Res. 2018;43(4):517–525. doi: 10.1080/02713683.2018.1428996. [DOI] [PubMed] [Google Scholar]
- 7.Nagpal M, Chaudhary P, Wachasundar S, Eltayib A, Raihan A. Management of recurrent rhegmatogenous retinal detachment. Indian J Ophthalmol. 2018;66(12):1763–1771. doi: 10.4103/ijo.IJO_1212_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Haugstad M, Moosmayer S, Bragadόttir R. Primary rhegmatogenous retinal detachment - surgical methods and anatomical outcome. Acta Ophthalmol. 2017;95(3):247–251. doi: 10.1111/aos.13295. [DOI] [PubMed] [Google Scholar]
- 9.Haritoglou C, Wolf A. Surgical managment of retinal detachment. Klinische Monatsblatter Fur Augenheilkunde. 2015;232(5):669–675. doi: 10.1055/s-0034-1383068. [DOI] [PubMed] [Google Scholar]
- 10.Ho CL, Chen KJ, See LC. Selection of scleral buckling for primary retinal detachment. Ophthalmologica. 2002;216(1):33–39. doi: 10.1159/000048294. [DOI] [PubMed] [Google Scholar]
- 11.Sadaka A, Giuliari GP. Proliferative vitreoretinopathy: current and emerging treatments. Clin Ophthalmol Auckl N Z. 2012;6:1325–1333. doi: 10.2147/OPTH.S27896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alexander P, Ang A, Poulson A, Snead MP. Scleral buckling combined with vitrectomy for the management of rhegmatogenous retinal detachment associated with inferior retinal breaks. Eye (Lond) 2008;22(2):200. doi: 10.1038/sj.eye.6702555. [DOI] [PubMed] [Google Scholar]
- 13.Fenberg MJ, Hainsworth KJ, Rd RF, Hainsworth DP. Vitrectomy as a risk factor for complicated cataract surgery. Mo Med. 2016;113(1):44–47. [PMC free article] [PubMed] [Google Scholar]
- 14.Stewart S, Chan W. Pneumatic retinopexy: patient selection and specific factors. Clin Ophthalmol Auckl N Z. 2018;12:493–502. doi: 10.2147/OPTH.S137607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Böni C, Thorne JE, Spaide RF, Ostheimer TA, Sarraf D, Levinson RD, Goldstein DA, Rifkin LM, Vitale AT, Jaffe GJ, Holland GN. Fundus autofluorescence findings in eyes with birdshot chorioretinitis. Invest Ophthalmol Vis Sci. 2017;58(10):4015. doi: 10.1167/iovs.17-21897. [DOI] [PubMed] [Google Scholar]
- 16.Jin HY, Zhang Q, Zhao PQ. Minimal in situ conjunctival incision for segmental scleral buckling surgery. Ophthalmic Surg Lasers Imaging Retina. 2014;45(6):574–576. doi: 10.3928/23258160-20141118-14. [DOI] [PubMed] [Google Scholar]
- 17.Bonnet M. The development of severe proliferative vitreoretinopathy after retinal detachment surgery. Grade B: a determining risk factor. Graefes Arch Clin Exp Ophthalmol. 1988;226(3):201–205. doi: 10.1007/BF02181181. [DOI] [PubMed] [Google Scholar]
- 18.Papakostas TD, Vavvas D. Postoperative complications of scleral buckling. Semin Ophthalmol. 2018;33(1):70–74. doi: 10.1080/08820538.2017.1353816. [DOI] [PubMed] [Google Scholar]
- 19.Qiang Kwong T, Shunmugam M, Williamson TH. Characteristics of rhegmatogenous retinal detachments secondary to retinal dialyses. Can J Ophthalmol. 2014;49(2):196–199. doi: 10.1016/j.jcjo.2013.12.013. [DOI] [PubMed] [Google Scholar]
- 20.Shu I, Ishikawa H, Nishikawa H, et al. Scleral buckling versus vitrectomy for young Japanese patients with rhegmatogenous retinal detachment in the era of microincision surgery: real-world evidence from a multicentre study in Japan. Acta Ophthalmol. 2019;97(5):e736–e741. doi: 10.1111/aos.14050. [DOI] [PubMed] [Google Scholar]
- 21.Feng H, Adelman RA. Cataract formation following vitreoretinal procedures. Clin Ophthalmol Auckl N Z. 2014;8:1957–1965. doi: 10.2147/OPTH.S68661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Harocopos GJ, Shui YB, McKinnon M, Holekamp NM, Gordon MO, Beebe DC. Importance of vitreous liquefaction in age-related cataract. Investig Ophthalmol Vis Sci. 2004;45(1):77–85. doi: 10.1167/iovs.03-0820. [DOI] [PubMed] [Google Scholar]
- 23.Holekamp NM, Shui YB, Beebe DC. Vitrectomy surgery increases oxygen exposure to the lens: a possible mechanism for nuclear cataract formation. Am J Ophthalmol. 2005;139(2):302–310. doi: 10.1016/j.ajo.2004.09.046. [DOI] [PubMed] [Google Scholar]
- 24.Petermeier K, Szurman P, Bartz-Schmidt U, Gekeler F. Pathopysiology of cataract formation after vitrectomy. Klin Monbl Augenheilkd. 2010;227(3):175–180. doi: 10.1055/s-0029-1245271. [DOI] [PubMed] [Google Scholar]
- 25.Sawa M, Saito Y, Hayashi A, Kusaka S, Ohji M, Tano Y. Assessment of nuclear sclerosis after nonvitrectomizing vitreous surgery. Am J Ophthalmol. 2001;132(3):356–362. doi: 10.1016/s0002-9394(01)01025-x. [DOI] [PubMed] [Google Scholar]
- 26.AbdEl Dayem H, Hartzer M, Williams G, Ferrone P. The effect of vitrectomy infusion solutions on postoperative electroretinography and retina histology. BMJ Open Ophthalmol. 2017;1(1):e000004. doi: 10.1136/bmjophth-2016-000004. [DOI] [PMC free article] [PubMed] [Google Scholar]