Abstract
Background:
Racial-ethnic minority disparities in diagnosis of mental health problems and access to treatment are apparent across different behavioral conditions, particularly in the quality of treatment for depression. However, how much disparities differ across providers is not clear.
Method:
Bayesian mixed effects models estimated if disparities in patient adherence to antidepressant medication (n=331,776) or psychotherapy (n=275,095) were associated with specific providers. Models also tested if providers who performed better on average with non-Hispanic white patients had lower disparities, and if the percentage of racial-ethnic minority patients in a provider caseload was associated with disparities.
Results:
Disparities in both adherence to antidepressant medication and psychotherapy were associated with the provider. Performance with non-Hispanic white patients was negatively correlated with provider specific disparities in psychotherapy, but not in medication. The proportion of racial-ethnic minority patients in a provider’s caseload was associated with lower adherence for non-Hispanic white patients and the size of disparities.
Conclusion:
A racial-ethnic minority patient’s successful adherence to depression treatment was related to how their provider performed with non-Hispanic white patients, but there was also evidence of provider-specific disparities. Provider focused efforts to decrease disparities might focus on improving the general skill of providers who treat more racial-ethnic minority patients, as well as offering culturally based training to providers with notable disparities.
Keywords: Provider effects, racial-ethnic mental health disparities, cultural competence, treatment adherence, Bayesian multilevel modeling
INTRODUCTION
Racial-ethnic minority disparities are apparent across multiple diagnoses and treatments.1–5 In particular, racial-ethnic minority patients adhere to both psychotherapy and medication for depression less than non-Hispanic white patients.4 While inequalities could result from interactions with different levels of the health system,6 disparities that may result from providers have received substantial attention.5,7
Many initiatives for addressing disparities (see8) operate based on the belief that disparities are, in part, a provider specific problem.7,9–14 However, there is not yet clear evidence that disparities can be localized to specific providers. Determining if some providers do have larger disparities in their caseloads than others is an important step in understanding how levels of the health system impact racial-ethnic minority health, as well as developing targeted quality improvement efforts that will reduce disparities.
Provider Differences in the Quality of Mental Healthcare
Psychotherapy providers vary in their effectiveness,15,16 and initial evidence suggest that medication providers vary in their effectiveness when treating depression.17 There is initial evidence that racial disparities in mental health treatment quality and outcome can also be specific to providers.18–23 However, the research involves small samples in clinical trials or is restricted to college counseling centers. Furthermore, larger studies have not focused on specific diagnoses, and no research has examined if racial-ethnic disparities vary across providers in antidepressant treatment, which is the most common treatment for depression.4,24
Proportion of Racial-Ethnic Minorities in a Provider Caseload
If disparities partially depend on the provider, it is then important to test what factors explain these differences. A provider is situated in a milieu that serves patients with different demographic profiles. Providers who work with more racial-ethnic minority patients in their practice might be better with racial-ethnic minority patients than those who see few (e.g., they have more exposure to racial-ethnic minority patients). Alternatively, it is also possible that providers with a higher proportion of racial-ethnic minority in their caseload are different than providers who see few racial-ethnic minority patients.25,26 For instance, there are differences in qualifications, knowledge, and resource accessibility among providers treating a higher proportion of African-Americans versus providers with a higher proportion of white patients in primary care settings.25–27 However, no research has examined differences in provider performance that may be associated with having a higher proportion of racial-ethnic minority patients.
Current Study
The goal of this study is to examine whether mental health providers are a source of racial-ethnic disparities in an insurance-based health care system. We examined how much providers differ in the relative adherence of their non-Hispanic white and racial-ethnic minority patients to either antidepressant medication (ADM) or psychotherapy. We hypothesized that racial-ethnic minority differences in adherence rates would vary across providers, with some revealing substantial adherence disparities, while others would show minimal or no disparities (Hypothesis 1). Secondly, we examined if the proportion of racial-ethnic minority patients in a caseload is associated with the adherence disparity in a providers’ caseload. We hypothesized that providers with a lower proportion of racial-ethnic minority patients in their caseload would have better adherence rates, but higher disparities between racial groups (Hypothesis 2).
METHODS
Mental Health Research Network (MHRN).
Electronic medical record data were obtained from a subsample of records from the MHRN’s Virtual Data Warehouse (VDW)4,16,28 from health systems in Southern California and Washington and is subject to an ongoing approved IRB to the MHRN. The patient sample was limited to depression care episodes of patients 18 and older who had a new episode of psychotherapy (n=275,095) between January 1, 2010, and December 31, 2013, and/or a new antidepressant treatment (n=331,776) between January 1, 2009, and December 31, 2013. Data regarding how patients were assigned to providers was not available.
To ensure adequate representation of non-Hispanic white and racial-ethnic minority patients within caseloads we restricted the sample to providers who at least saw 10 patients, from whom at least 1 was self-identified as a racial-ethnic minority. The number of providers offering antidepressant treatment were 4,821 and 4,794 for psychotherapy. Antidepressant treatment was offered by nurse practitioners, physician assistants, physicians, and an “other” category; while psychotherapy was offered by nurse practitioners, physician assistants, physicians, psych associates, psychologists, social workers, and also an “other” category. The mean number of patient episodes within provider’s caseloads was 255.7 (SD = 312.3), ranging from 10 to 1,811.
Measures
Race/ethnicity.
Self-reported race/ethnicity was obtained from the VDW. Members were asked to complete a self-report form that included separate questions for race/ethnicity. The recoding of race/ethnicity followed national recommendations for mutually exclusive race categories.29 Our final analyses used a binary race/ethnicity variable which was coded as Racial-Ethnic Minority (52.8%) and non-Hispanic white (47.1%). We used this binary variable because our prior work with MHRN data showed lower adherence rates among all racial-ethnic minority groups when compared to non-Hispanic white patients.4
Early Antidepressant (ADM) Adherence.
We defined early adherence to ADM as any antidepressant refill of at least 90 days supply within 180 days of a first prescription fill. We identified medical records and insurance claims with filled antidepressant prescriptions following the index date visit. Eligible antidepressant medication treatment included all drugs approved by the US Food and Drug Administration for treatment of major depression, excluding trazodone (often prescribed for insomnia). This definition of adherence is consistent with prior work and the Healthcare Effectiveness Data and Information Set (HEDIS) benchmarks.30–32
Early Psychotherapy Adherence.
We defined adherence as attending at least 1 psychotherapy visit within 90 days after the diagnostic interview date (see16). We defined an episode of psychotherapy with the Current Procedural Terminology Codes (diagnostic interview and assessment, individual psychotherapy, insight-oriented, etc.). We excluded codes that captured visits of less than 30 minutes or that were designated for medication management only.
Co-variates.
To control for differences in case-mix across providers, we used measures of a patient’s (1) prior mental health visits, (2) prior prescription for antidepressant medication in the last 5 years prior to the new episode date, and (3) neighborhood income. We used census data to measure the patient’s neighborhood income. We defined lower income as having a neighborhood median income lower than $40,000.
Statistical Analyses
We used Bayesian logistic mixed effects models to estimate provider specific disparities in adherence.33 Each model included racial-ethnic minority identification, neighborhood income, grand-mean centered prior mental health visits, and prior antidepressant prescription as fixed effects. Random effects were at the provider-level and included a random intercept and a random slope for racial-ethnic minority status. The random slope for racial-ethnic minority status estimates a provider-specific difference in adherence of racial-ethnic minority patients and non-Hispanic white patients. Negative value provider-specific differences indicate that racial-ethnic minority patients of a specific provider had a lower probability of adhering to treatment than non-Hispanic white patients. The variance component of the random slope provided the test of our main hypothesis - how much disparities in adherence between racial-ethnic minority and non-Hispanic white patients varied across providers. Model 1 included a correlation between the random effect for the intercept and the random slope of the racial-ethnic status effect, which tested if a provider’s adherence rate with their non-Hispanic white patients was related to the disparities – i.e., the difference between racial-ethnic minority and non-Hispanic white patients in their caseload.
Model 2 is identical to Model 1, but also examined if the proportion of racial-ethnic minority patients in providers’ caseload was associated with patient adherence above and beyond the individual patient’s own racial/ethnic background. Said another way, Model 2 examined whether the proportion of minority patients in a provider’s caseload was associated with patients’ adherence. Model 2 also included an interaction between the proportion of racial-ethnic minority patients within a provider caseload and patient racial-ethnic minority status. This interaction tested whether the racial-ethnic diversity of a providers’ caseload moderated the size of the difference in adherence between non-Hispanic white and racial-ethnic minority patients in a caseload.
Weakly-informative prior distributions included: (a) a normal distribution with a mean of 0 and standard deviation of 2 for fixed effects, (b) a half-cauchy with a location of 0 and scale of 1 for the standard deviation of the random effects, and (c) LKJ-prior with a shape parameter of 2 for the correlation between random effects.33,34
RESULTS
The primary test of whether provider was associated with adherence disparities was the standard deviation for the random slope for patient’s race/ethnic status. As predicted, the difference in adherence between non-Hispanic white and racial-ethnic minority patients varied across providers, s1j=0.21, CI=0.18 to 0.24 in psychotherapy and s1j =0.1, CI=0.03 to 0.16 in ADM. That is, some providers’ racial-ethnic minority and non-Hispanic white patients’ had more similar rates of adherence, whereas others demonstrated higher within-caseload disparities.
Figure 1 illustrates the extent of differences in disparities across providers in psychotherapy and ADM derived from the model. In psychotherapy, there were some providers whose racial-ethnic minority patients and non-Hispanic white patients had an equal probability of adhering (in some instances racial-ethnic minority patients had a higher probability of return), but there were also providers whose racial-ethnic minority patients were 10% less likely to return than their non-Hispanic white patients. In ADM, on the left side of the figure, providers’ racial-ethnic minority patients had a 9% lower probability of refilling as compared to non-Hispanic white patients, but on the far right, providers’ racial-ethnic minority patients had a 19% lower probability of filling their prescription. There were no providers where racial-ethnic minority patients had a higher rate of medication adherence than non-Hispanic white patients.
Figure 1. Distribution of the Difference in the Probability of non-Hispanic White and racial-ethnic minority Return Rates.
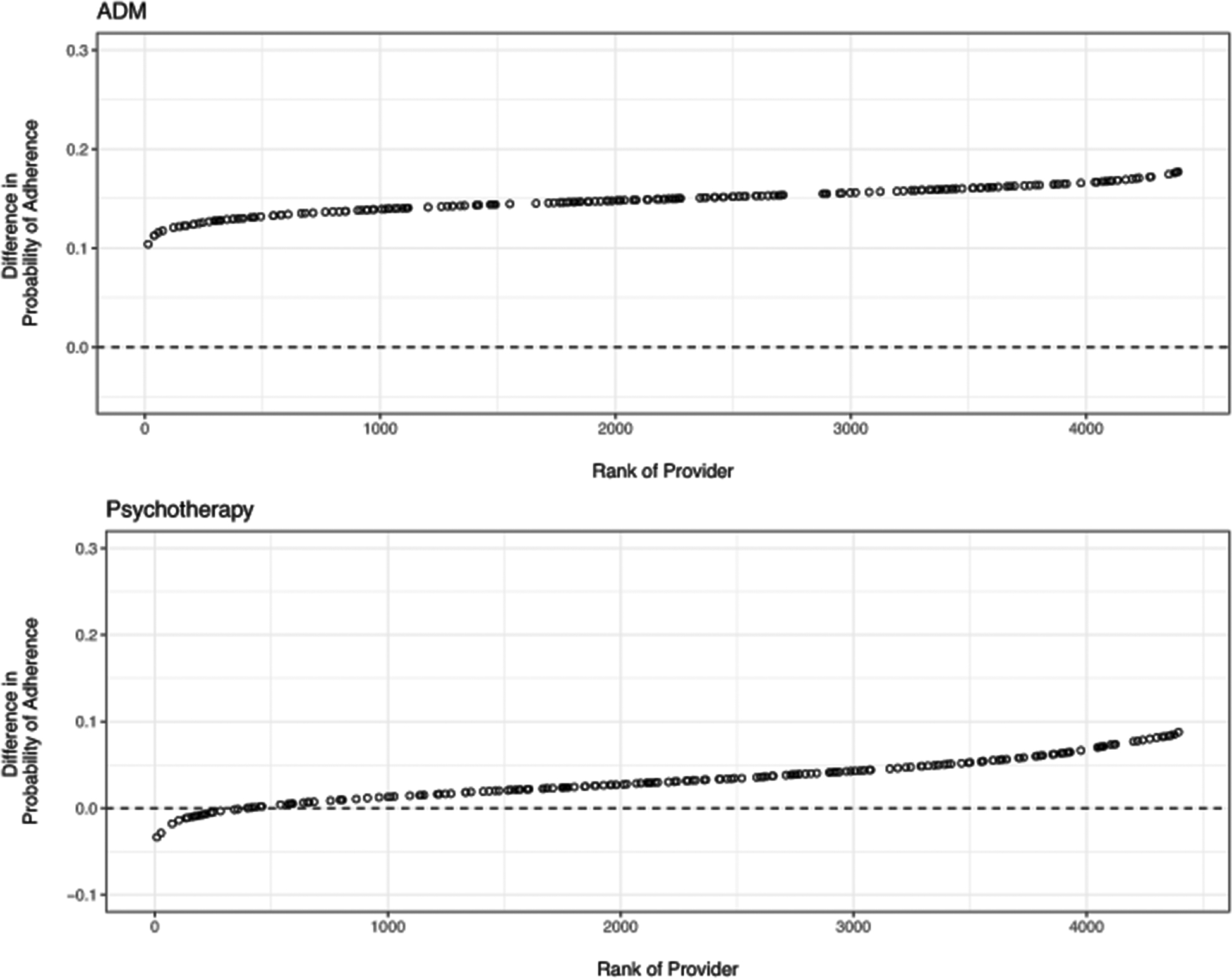
This figure illustrates the model derived provider-specific disparities (e.g., random effects) in psychotherapy and medication (based on randomly selected 5% of the provider sample to increase readability of plot). Each circle is a provider. Circles above zero indicate non-Hispanic white patients had a greater probability of adhering to the treatment. Differences between plot and model results in the narrative are due to using a subsample of the providers in the plot.
The correlation between the adherence rate of a provider’s non-Hispanic white patients and the disparity in adherence between their racial-ethnic minority and non-Hispanic white patients was large and negative, r=−0.80,CI=−0.87 to −0.72 in psychotherapy and very small, r =0.05,CI=−0.20 to 0.51 in ADM. The correlation for ADM suggests no relationship between providers’ outcomes with non-Hispanic white patients and the difference between racial-ethnic minority patients and non-Hispanic white patients. In contrast, the correlation for psychotherapy indicates when a provider’s non-Hispanic white patients had higher rates of adherence, the difference between racial-ethnic minority patients and non-Hispanic white patients were more negative (i.e., disparities were larger). Both correlations should be interpreted with caution, given the relatively small range of within-provider difference between racial-ethnic minority patients and non-Hispanic white patients.
Proportion of Minority Racial-Ethnic Minority Patients in Caseload
In Model 2, we examined the relationship of the proportion of racial-ethnic minority patients in provider caseloads with adherence. The interaction between patients’ racial-ethnic minority status and the proportion of racial-ethnic minority patients in a providers’ caseload tested whether disparities in adherence were moderated by the proportion of minority patients in the providers caseload. The interactions were b60=0.29, CI=0.18 to 0.39 for psychotherapy and b60=−0.39, CI=−0.48 to −0.30 for ADM.
Figure 2 assists with the interpretation of the interaction by illustrating how disparities are affected by the proportion of racial-ethnic minority patients for ADM and psychotherapy within a caseload. For both treatments, disparities changed when the percentage of racial-ethnic minority patients was larger. Specifically, Figure 2 shows that for medication, disparities were highest when the proportion of racial-ethnic minority patients in a provider’s caseload was highest. In contrast, for psychotherapy, disparities were the smallest when the proportion of racial-ethnic minority patients in a provider’s caseload was highest (though disparities were never large in psychotherapy compared to those in ADM).
Figure 2. Effect of the Proportion of racial-ethnic minority Patients in Provider Caseload Adherence Rates.
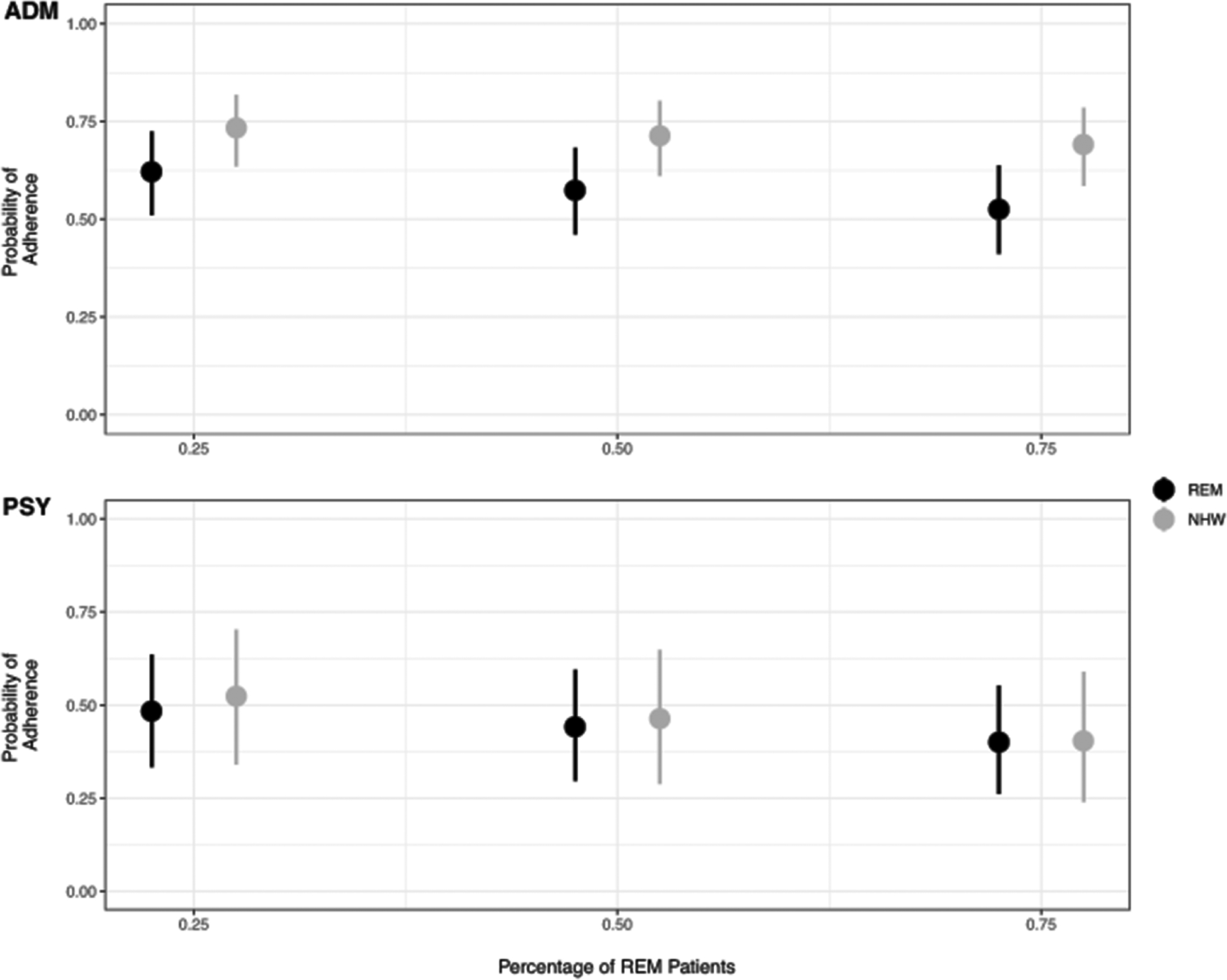
The effects of the proportion for ADM and psychotherapy. For ADM, adherence among non-Hispanic white and racial-ethnic minority patients diverged when the percentage of racial-ethnic minority patients was larger. For psychotherapy it was the opposite, adherence rates converged when the percentage of racial-ethnic minority patients was larger.
DISCUSSION
Consistent with prior work,18, 20–23 the extent of disparities partially depended on the provider. In psychotherapy, some providers overcame adherence disparities entirely - their non-Hispanic white and racial-ethnic minority patients adhered to treatment at equal rates. For some medication providers, the disparity was half of the overall main effect. Psychotherapy providers (but not medication providers) whose non-Hispanic white patients adhere more had relatively larger disparities among patients in their caseload. This psychotherapy finding points to the possible distinction between a provider’s ability to encourage patients from majority groups to adhere to treatment, and his/her specific ability to work with racial-ethnic minority patients in psychotherapy.35
One important caveat is that providers (of both medication and psychotherapy) who achieve high adherence rates with non-Hispanic white patients also had racial-ethnic minority patients with higher on average adherence rates. That is, even though they had higher disparities, providers who had the highest adherence rates with white patients obtained better return rates with racial-ethnic minority patients. This pattern of findings suggests that both racial-ethnic minority and non-Hispanic white patients are more likely to adhere with some providers, but minority patients don’t match the gains that non-Hispanic white patients experience. A mirror of this experience might be found in how some racial-ethnic minority individuals experience other social domains (e.g., restaurants, education systems).36–41 Racial-ethnic minority individuals might have specific negative experiences in these settings that are unique to their group membership (e.g., low expectations, not feeling welcomed, microaggressions, etc.).
The source of provider specific disparities cannot be determined from this data. It is possible that patients experience biased messages from their providers,42 or have other negative experiences during their visit associated with the provider (e.g., check-in staff). Disparities might result from processes beyond the control of the health system (i.e., discriminatory experiences during transit in a predominantly white area). Indeed, as no ADM providers had racial-ethnic minority patients with higher adherence rates, provider variability seems constrained by factors that are not unique to specific providers. The behavioral process of attending psychotherapy sessions is more complex than medication (i.e., travel to multiple offices visits) and could be subject to a number of additional factors - flexibility in work schedule, child-care, that are beyond a providers control. Alternatively, it is possible that disparities are smaller for providers with patients who generally adhered at lower rates than others because of a floor effect such that some providers simply provide poor care indiscriminately. Racial-ethnic disparities may still be among these providers but might be masked by more general problems with engaging patients. Future research should target providers and settings with overall good performance, but where disparities remain.
We also found that patients with a provider who treated a higher proportion of racial-ethnic minority patients had lower adherence regardless of the patient’s own racial-ethnic minority identity. Providers and patients in practices with more racial-ethnic minority patients may face different challenges than providers delivering care in majority non-Hispanic white practices.
Accordingly, the proportion of racial-ethnic minority patients in provider caseload may be a proxy for other clinic or neighborhood characteristics affecting adherence.25,43–45 Caseloads that have more minority patients could be a marker for practicing in a more segregated and/or disadvantaged area – which might affect white patients in the same panel or area. It is possible that these provider-specific disparities are also interacting with patient and clinical factors, as racial-ethnic minority patients who visit providers located in majority non-Hispanic white practices may engage with medical care based on other individual factors (e.g., increased English fluency, SES, generational status).
The proportion of racial-ethnic minority patients had opposite effects on disparities for psychotherapy and ADM. For psychotherapy, disparity decreased as the proportion of racial-ethnic minority patients increased. Alternatively, for ADM, the disparity was larger for providers with caseloads that were more diverse. The difference in the proportion effect between treatment modalities could be associated with increased use of different therapeutic skills when delivering psychotherapy as opposed to medication management, or a general difference in multicultural perspectives during academic training between providers delivering psychotherapy and medication.
Limitations
A primary limitation of this study is that patients were not randomly assigned to providers, thus it is possible that some differences between providers are the result of differences in patients rather than providers. Indeed, we raised this possibility above when noting that the non-Hispanic white patients seen by providers with more racial-ethnic minority patients may be different than white patients seen by providers who saw mostly white patients. The findings in the current study are consistent with those from smaller samples in clinical trials where bias in assignment is likely to be even smaller.18 Second, we were not able to model site or clinic location along with provider. Thus, it is possible that some of the provider differences in this study are actually due to the clinics in which those providers practice.
Third, it is possible that provider variability in the systems we studied is relatively minimized compared to other systems due to the implementation of best practice guidelines.46 One of the guidelines to maximize medication adherence involved an automated refill ordering process via online patient portals or a telephone system. To that end, it is possible that we might observe greater provider variability in medication in less structured settings. Fourth, it is possible that severity, and income adjustments did not fully account for differences in patient case-mix across providers.
Conclusions
Depending on the provider, the expected disparity in adherence to depression treatment between non-Hispanic white and minority patients can vary substantially. Disparities in the quality of depression treatment are not monolithic across the health system. Reducing differences between providers both in terms of practice patterns, patient demographics, and clinical milieus is likely to be an important component of efforts to address disparities in mental health. There is initial evidence that focusing in particular on providers who see the most racial-minority patients will be important - as their patients tend to adhere less regardless of their racial-ethnic identity. Future research might focus on evaluating the clinical interactions of providers who have racial-ethnic minority patients that adhere at similar rates to non-Hispanic white patients. Evaluating what these providers do and say to their patients could provide important insights into health disparities. Healthcare facilities could develop specific skills training programs targeting lower performing providers and providers with notable disparities between groups of patients and track whether these efforts have a measurable impact on disparities.
Supplementary Material
Table 1.
Bayesian Multilevel Models of Adherence to Medication and Psychotherapy
| Model 1 | Model 2 | |||
|---|---|---|---|---|
| Estimate | 95% Cl | Estimate | 95% Cl | |
| Antidepressant | ||||
| Fixed Effects | ||||
| Intercept (b00) | 1.08 | [1.06, 1.10] | 1.26 | [1.23, 1.30] |
| Racial-Ethnic status (b10) | −0.67 | [−0.69, −0.66] | −0.44 | [−0.48, −0.39] |
| Prior Mental Health (b20) | 0.17 | [0.16, 0.19] | 0.18 | [0.16, 0.20] |
| Prior Medication treatment(b30) | 0.24 | [0.22, 0.26] | 0.24 | [0.22, 0.26] |
| Neighborhood Income (b40) | −0.13 | [−0.15, −0.12] | −0.12 | [−0.13, −0.10] |
| Proportion Minority Patients (b50) | - | - | −0.42 | [−0.50, −0.34] |
| Prop Minority X Racial-Ethnic Status (b60) | - | - | −0.39 | [−0.48, −0.30] |
| Provider-Level Random Effects | ||||
| Intercept (S0j) | 0.36 | [0.34, 0.38] | 0.35 | [0.33, 0.37] |
| R-E status (S1j) | 0.10 | [0.03, 0.16] | 0.07 | [0.00, 0.13] |
| Correlation (rj) | 0.05 | [−0.20, 0.51] | −0.25 | [−0.69, 0.26] |
| Psychotherapy | ||||
| Fixed Effects | ||||
| Intercept (b00) | −0.04 | [−0.07, 0.01] | 0.42 | [0.36, 0.48] |
| Racial-Ethnic status (b10) | −0.14 | [−0.16, −0.11] | −0.26 | [−0.31, −0.20] |
| Prior Mental Health (b20) | 0.08 | [0.06, 0.09] | 0.08 | [0.06, 0.09] |
| Prior Medication treatment (b30) | −0.14 | [−0.16, −0.12] | −0.14 | [−0.16, −0.12] |
| Neighborhood Income (b40) | −0.06 | [−.0.07, −0.04] | −0.05 | [−0.06, −0.03] |
| Proportion Minority Patients (b50) | - | - | −1.06 | [−1.18, −0.94] |
| Prop Minority X Racial-Ethnic Status (b60) | - | - | 0.29 | [0.18, 0.39] |
| Provider-Level Random Effects | ||||
| Intercept (S0j) | 0.72 | [0.69, 0.75] | 0.68 | [0.66, 0.71] |
| Racial-ethnic status (S1j) | 0.21 | [0.18, 0.24] | 0.20 | [0.17, 0.23] |
| Correlation (rj) | −0.80 | [−0.87, −0.72] | −0.78 | [−0.86, −0.70] |
95% CI 95% credible interval. Model 1 is a Bayesian mixed effects model that estimates if the effect of racial-ethnic minority status on adherence varied across providers. Model 2 is identical except that effect for the proportion of racial-ethnic minority patients in a providers caseload are added as co-variates.
Highlights (Key Points).
Limited research is available exploring the interaction of patient race-ethnicity with provider performance.
Racial-ethnic disparities in adherence to antidepressant medication and psychotherapy partially depended on the patient provider.
A larger percentage of racial-ethnic minority patients in a providers caseload was associated with lower adherence for non Hispanic-white patients.
References
- 1.Alegria M, Chatterji M, Wells K, et al. Disparity in depression treatment among racial and ethnic minority populations in the United States. Psychiatric Serv. 2008;59(11): 1264–1272. doi: 10.1176/appi.ps.59.11.1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. CDC health disparities and inequalities report-United States, 2013. Foreword. MMWR supplements. https://www.cdc.gov/mmwr/pdf/other/su6203.pdf. Published November 2013. Accessed March 2017. [PubMed]
- 3.US Department of Health and Human Services. Disparities in healthcare quality among racial and ethnic minority groups. 2011. Washington, DC: Department of Health and Human Services. [Google Scholar]
- 4.Coleman K, Stewart C, Waitzfelder B et al. Racial-ethnic differences in psychiatric diagnoses and treatment across 11 health care systems in the Mental Health Research Network. Psychiatric Serv. 2016; 67(7): 749–57. doi: 10.1176/appi.ps.201500217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Institute of Medicine. Unequal treatment: Confronting racial and ethnic disparities in health care (full printed version). 2002. Washington, DC: National Academies Press. [PubMed] [Google Scholar]
- 6.World Health Organization. A conceptual framework for action on the social determinants of health, social determinants of health discussion paper 2 (Policy and Practice). 2010. Geneva: Switzerland. [Google Scholar]
- 7.US Department of Health and Human Services, Office of the Secretary, Office of the Assistant Secretary for Planning and Evaluation and Office of Minority Health. HHS action plan to reduce racial and ethnic health disparities implementation progress report. 2015. Washington, DC: Office of the Assistant Secretary for Planning and Evaluation. [Google Scholar]
- 8.Office of Disease Prevention and Health Promotion. Healthy People 2020. https://www.healthypeople.gov/2020/topics-objectives. Accessed March 20, 2018.
- 9.Betancourt JR, Green AR, Carrillo JE, & Ananeh-Firempong O. Defining cultural competence: a practical framework for addressing racial/ethnic disparities in health and health care. Public Health Rep. 2003;118(4): 293–302. doi: 10.1377/hlthaff.24.2.499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cross TL, Bazron BJ, Dennis KW, Isaacs MR. Towards a Culturally Competent System of Care: A Monograph on Effective Services for Minority Children Who Are Severely Emotionally Disturbed. Washington, DC: Georgetown University Child Development Center; 1989. [Google Scholar]
- 11.United States Department of Health and Human Services, Office of Minority Health (2013). What is cultural competency? https://www.cdc.gov/nchhstp/socialdeterminants/docs/what_is_cultural_competency.pdf. Accessed May 20, 2018.
- 12.Roberts RN, Barclay-McLaughlin G, Cleveland J, et al. Developing culturally competent programs for families of children with special needs (2nd ed.). Washington, DC: Georgetown University, Child Development Center; 1990 [Google Scholar]
- 13.Sue DW, Arredondo P, McDavis RJ. Multicultural counseling competencies and standards: A call to the profession. J Couns Dev. 1992; 70(4): 477–486. doi: 10.1002/j.1556-6676.1992.tb01642.x [DOI] [Google Scholar]
- 14.Whaley AL, Davis KE. Cultural competence and evidence-based practice in mental health services: A complementary perspective. Am Psychol. 2007; 62(6), 563. [DOI] [PubMed] [Google Scholar]
- 15.Baldwin SA, Imel ZE. Therapist effects: Findings and methods Bergin and Garfield’s Handbook of Psychotherapy and Behavior Change, 6th ed. Hoboken, NJ: John Wiley & Sons;2013: 258–297. [Google Scholar]
- 16.Zeber JE, Coleman KJ, Fischer H. The impact of race and ethnicity on rates of return to psychotherapy for depression. Depress Anxiety. 2017;34(12):1157–1163. 10.1002/da.22696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McKay KM, Imel ZE, Wampold BE. Psychiatrist effects in the psychopharmacological treatment of depression. J Affect Disord. 2006;92(2):287–290. doi: 10.1016/j.jad.2006.01.020 [DOI] [PubMed] [Google Scholar]
- 18.Imel ZE, Baldwin S, Atkins DC, Owen J, Baardseth T, Wampold BE. Racial/ethnic disparities in therapist effectiveness: A conceptualization and initial study of cultural competence. J Couns Psychol. 2011;58:290–298. doi: 10.1037/a002328. [DOI] [PubMed] [Google Scholar]
- 19.Larrison CR, Schoppelrey SL. Therapist effects on disparities experienced by minorities receiving services for mental illness. Res Soc Work Pract. 2011;21:727–736. doi: 10.1177/1049731511410989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Drinane JM, Owen J, Kopta S. Racial/ethnic disparities in psychotherapy: does the outcome matter?. TPM Test Psychom Methodol Appl Psychol. 2016; 23(4):531–544. doi: 10.4473/TPM23. [DOI] [Google Scholar]
- 21.Hayes JA, McAleavey AA, Castonguay LG, Locke BD. Psychotherapists’ outcomes with Non-Hispanic White and racial/ethnic minority patients: First, the good news. J Couns Psychol. 2016;63(3):261–268. doi: 10.1037/cou0000098. [DOI] [PubMed] [Google Scholar]
- 22.Hayes JA, Owen J, Bieschke KJ. Therapist differences in symptom change with racial/ethnic minority patients. Psychotherapy. 2015;52(3):308–314. doi: 10.1037/a0037957. [DOI] [PubMed] [Google Scholar]
- 23.Owen J, Imel ZE, Adelson J, Rodolfa E. ‘No-show’: Therapist racial/ethnic disparities in client unilateral termination. J Couns Psychol. 2012;59(2):314. doi: 10.1037/a0027091 [DOI] [PubMed] [Google Scholar]
- 24.Olfson M, Marcus SC. National patterns in antidepressant medication treatment. Arch Gen Psychiatry. 2009;66(8):848–856. doi: 10.1001/archgenpsychiatry.2009.81. [DOI] [PubMed] [Google Scholar]
- 25.Bach PB, Pham HH, Schrag D, Tate RC, Hargraves JL. Primary care physicians who treat blacks and whites. N Engl J Med. 2004;351(6):575–584. [DOI] [PubMed] [Google Scholar]
- 26.Gemson DH, Elinson J, Messeri P. Differences in physician prevention practice patterns for white and minority patients. J Commun Health. 1998;13(1):53–64. [DOI] [PubMed] [Google Scholar]
- 27.Ashford A, Gemson D, Gorin SNS, et al. Cancer screening and prevention practices of inner-city physicians. Am J Prev Med. 2000;19(1):59–62. 10.1016/S0749-3797(00)00152-5 [DOI] [PubMed] [Google Scholar]
- 28.Mental Health Research Network, MHRN-Central. http://hcsrn.org/mhrn/en/. Accessed June 1, 2018.
- 29.Institute of Medicine. Ethnicity and language data: Standarization for health care quality improvement. Washington, DC: National Academies Press; 2009. [PubMed] [Google Scholar]
- 30.National Committee for Quality Assurance. The State of Health Care Quality 2017. Washington, DC: National Committee for Quality Assurance; 2017. [Google Scholar]
- 31.Rossom RC, Shortreed S, Coleman KJ, et al. Antidepressant adherence across diverse populations and healthcare settings. Depress Anxiety. 2016;33(8):765–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Simon GE, Stewart C, Beck A, et al. National prevalence of receipt of antidepressant prescriptions by persons without a psychiatric diagnosis. Psychiatric Serv. 201;65(7):944–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gelman A. Prior distributions for variance parameters in hierarchical models. Bayesian Analysis. 2006;1(3), 515–533. [Google Scholar]
- 34.Lewandowski D, Kurowicka D, Joe H. Generating random correlation matrices based on vines and extended onion method. Journal of Multivariate Analysis. 2009; 100(9), 1989–2001. 10.1016/j.jmva.2009.04.008 [DOI] [Google Scholar]
- 35.Coleman HL. General and multicultural counseling competency: Apples and oranges?. Journal of Multicultural Counseling and Development. 1998; 26(3), 147–156. [Google Scholar]
- 36.Upp Foundation. On course for success? Student retention at university. London, UK: Social Markey Foundation;2017. [Google Scholar]
- 37.Brewster ZW, Rusche SN. Quantitative evidence of the continuing significance of race: Tableside racism in full-service restaurants. Journal of Black Studies. 2012;43(4), 359–384. [DOI] [PubMed] [Google Scholar]
- 38.Shapiro D, Dundar A, Huie F, et al. A National View of Student Attainment Rates by Race and Ethnicity – Fall 2010 Cohort (Signature Report No. 12b). Herndon, VA: National Student Clearinghouse Research Center, 2017. [Google Scholar]
- 39.New Partnership to Support Mental Health of College Students of Color. JED Foundation; https://www.jedfoundation.org/Steve-Fund-JED-Announcement/. Accessed September 1, 2019. [Google Scholar]
- 40.Speaking Our Truths: A Senior Independent Research Project by Tailour Garbutt. Dartmouth College; https://journeys.dartmouth.edu/speakingourtruths/. Accessed Sept 1, 2019. [Google Scholar]
- 41.For Students of Color, Ivy League Schools Have a Long Way to Go. The Nation; https://www.thenation.com/article/for-students-of-color-ivy-league-schools-have-a-long-way-to-go/. Accessed Sep 1, 2019. [Google Scholar]
- 42.Snowden LR. Bias in mental health assessment and intervention: Theory and evidence. American Journal of Public Health. 2003;93(2), 239–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Diez-Roux A, Mair C. Neighborhoods and health. Ann N Y Acad Sci. 2010;1186(1):125–145. doi: 10.1111/j.1749-6632.2009.05333.x [DOI] [PubMed] [Google Scholar]
- 44.White K, Borrell LN. Racial/ethnic residential segregation: framing the context of health risk and health disparities. Health Place. 2011;17(2):438–448. 10.1016/j.healthplace.2010.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.White K, Haas JS, Williams DR. Elucidating the role of place in health care disparities: the example of racial/ethnic residential segregation. Health Serv. Res 2012;47(3):1278–1299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Imel ZE, Hubbard RA, Rutter CM, Simon G. Patient-rated alliance as a measure of therapist performance in two clinical settings. J Consult Clin Psychol. 2013;81(1):154–165. doi: 10.1037/a0030903 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


