Abstract
Background
Hypertension is a major health problem throughout the world which affects over one billion people due to severe complications and inadequate control. Even though lifestyle modification is one of the most effective ways to prevent and control hypertension, only little emphasis has been given for it compared with treating hypertension with medication. Therefore, the aim of this study was to assess adherence to lifestyle modifications and associated factors among hypertensive patients attending Dessie referral hospital.
Materials and Methods
Institutional-based cross-sectional study design was conducted among 301 hypertensive patients during May and June, 2020. The study participants were selected with a convenient sampling technique due to the COVID-19 pandemic. Data were collected using pre-tested and structured face to face interviewer-administered questionnaire and checked, cleaned and entered into Epi data version 4.4 and exported to SPSS version 25.0 software for analysis. The associations between independent variables and dependent variable were analyzed using binary logistic regression models.
Results
A total of 301 respondents participated in the study yielding a response of 100%. The overall adherence in this study was only 23.6%. Independent predictors of adherence to lifestyle modifications were divorced (AOR=0.35; 95% CI (0.13–0.94)) and widowed (AOR=0.27; 95% CI (0.10–0.75)), secondary school education (AOR=4.85; 95% CI (1.54–15.22)), no regular income (AOR=0.22; 95% CI (0.08–0.65)) or monthly income of ≥3000 ETB (AOR=5.58; 95% CI (2.46–12.66)), having co-morbidities (AOR=2.37; CI (1.23–4.57)), good knowledge about the disease (AOR=1.83; CI (0.92–3.65)) and good self-efficacy (AOR=3.64; CI (1.75–7.55)).
Conclusion and Recommendations
The overall adherence to recommended lifestyle modifications was very low. The independent predictors were marital status, educational level, monthly income, having co-morbidities, knowledge and self-efficacy. Therefore, multifaceted and collaborative implementation of strategies about lifestyle modifications for hypertension prevention and control are needed to address barriers at the patient, provider, system and community levels.
Keywords: hypertension, adherence, lifestyle modification, patient
Introduction
Hypertension or raised blood pressure is a leading risk for death and disability globally along with increasing co-morbidity.1 Around 1.39 billion of the world adult population lives with hypertension, of these 349 million are in high-income countries while 1.04 billion are in low- and middle-income countries.2 Even though it is a global public health issue, it disproportionately affects populations in low- and middle-income countries that account for nearly 80% of deaths where health systems are weak.3 In Ethiopia, the prevalence of hypertension is increasing over time with current prevalence 34.7%, of these 53.8% were male and 46.2% were female.4
Uncontrolled hypertension is a risk for the occurrence of cardiovascular diseases such as stroke, myocardial infarction, congestive heart failure as well as complications such as renal and eye diseases, stroke and chronic kidney disease.5 Complications of hypertension account for 9.4 million of the 17 million cardiovascular deaths worldwide every year. Furthermore hypertension is responsible for at least 45% of deaths due to heart disease and 51% of deaths due to stroke.3
Despite all its known adverse health consequences, high blood pressure is still poorly controlled globally due to low non-pharmacological interventions such as lifestyle modifications.5,6 Therefore health promotion should integrate the use of prescribed medications and lifestyle modifications, as they have been proven to prevent and control high blood pressure.6 Lifestyle modifications consist of five components: adoption of Dietary Approach to Stop Hypertension plans (DASH), low sodium diet, engage in physical activity, moderate alcohol consumption and cease smoking.7,8 Even though most people choose therapeutic drugs, the adherence to pharmacological and non-pharmacological treatment should be considered equally.7
To reduce morbidity and mortality various studies have been conducted in different parts of the world. Though, there was significant variation across countries, adherence to lifestyle modifications for hypertension is less than optimal in all countries. Adherence to self-care practice in Ethiopia is still poor at 23% but for antihypertensive medications adherence is at about 67%.8 Lifestyle- and diet-related factors are often modifiable, so their effects have specific importance in hypertension prevention and treatment. Lifestyle modification is particularly helpful in the large proportion of hypertensive patients who have additional risk factors for premature cardiovascular diseases, especially dyslipidemia and diabetes.9,10
Hypertension is affected by different factors. Among these adherence to lifestyle modification and to therapeutic drugs are the most important. Adherence to recommended lifestyle modification can be affected by demographic factors; patients’ level of monthly income, educational level, age, co-morbidity, knowledge about the disease, self-efficacy, social support, smoking, obesity, harmful use of alcohol and sedentary lifestyle, continuity of health education and counseling as well as motivation.5–8,11
To achieve lifestyle modification activities, it is likely that system changes are needed, such as the creation of multidisciplinary teams with expertise in counseling and the remuneration of time spent in lifestyle counseling. Promotion will need to include a component indicating that hypertension in itself is not a condition that hampers one’s lifestyle – on the contrary, if controlled, it will allow a normal lifestyle for a longer period of time. Generally primary care practitioners should recommend lifestyle modifications for all their pre-hypertensive and hypertensive patients.9,12
Hypertension is an important public health challenge in the developing and the developed world alike. It is not always taken seriously and is often poorly controlled mostly due to neglected causes resulting from unhealthy lifestyles. It is possible to prevent the development of hypertension and to lower blood pressure levels by simply adopting a healthy lifestyle. From the available literature search there is no study that showed lifestyle modifications adherence and associated factors in the study area despite its advantages. Therefore this study aimed to assess adherence to lifestyle modifications and associated factors among hypertensive patients attending chronic follow-up units of Dessie referral hospital.
Methods and Materials
Study Design and Area
An institution-based cross-sectional study was carried out in Dessie referral hospital in the South Wollo Zone from May 10 to July 8, 2020. South Wollo Zone is one of the 11 zones found in Amhara regional state. Its major city administration is Dessie town located 401 km away from Addis Ababa, the capital city of Ethiopia and 480 km from Bahir Dar, the capital city of Amhara regional state. Dessie referral hospital is the only referral hospital in Wollo province, serving about 7 million people including the neighboring regions.
Populations
Source Population
All hypertensive patients who were on antihypertensive therapy and attending chronic follow-up units of Dessie referral hospital.
Study Population
All adult registered hypertensive patients who fulfilled the inclusion criteria and were available during the time of data collection were included in the study. Data collectors approached 301 adult registered hypertensive patients and no one refused to participate.
Eligibility Criteria
Inclusion Criteria: All hypertensive patients who were 18 years and older and on anti-hypertensive treatment for at least for 6 months before commencement of the study were included.
Exclusion Criteria: Hypertensive patients who were unable to communicate, were critically ill, had mental health issues or refused to participate at the time of data collection were excluded.
Sample Size Determination and Procedure
Sample Size Determination
Sample size was determined using a single population proportion formula by considering proportion of adherence to recommended lifestyle modifications 23%,7 95% CI and 5% of marginal error. Sample size was estimated using the following assumptions.
 |
n= 273
Where, n = minimum sample size Zα/2= Z value at (α = 0.05) = 1.96
d = Margin of error (0.05)
After adding non-response rate of 10% to increase power, total sample size was 273+28=301 participants.
Sampling Procedure
Patients who were found during the study period in the study area who fulfilled the inclusion criteria were included in the study exclusively for lifestyle modification adherence at Dessie referral hospital. The reason why we selected a convenient sampling technique was the occurrence of the COVID-19 pandemic that only allowed anti-hypertensive treatment appointments every 3 months rather than every month. This method meant that we could reach 301 hypertensive patients during the study period. Before starting data collection informed consent was obtained from each interviewee by assuring confidentiality and explaining the objective of the study.
Study Variables
Dependent variable: Adherence to recommended lifestyle modifications.
Independent variables: Socio-demographic factors (age, sex, marital status, religion, ethnicity, level of education), Personal factors (co-morbidities, knowledge about the disease, duration of hypertension, type and duration of anti-hypertensive medication intake), Behavioral factors (self-efficacy), Social factors (support from families and non-family members of the society).
Duke Social Support and Stress Scale with 12 items was used to assess support gained from family and non-family.13 Responses were coded as: “none” = 0, “some” = 1, “a lot” = 2, “yes” = 2, “no” = 0 and “there is no such person” = 0. Blank responses were considered as “0”.
A modified 10-item hypertension evaluation of lifestyle and management (HELM) scale was used as a tool to measure respondents’ knowledge.14 Responses were coded as right answer as “1” and wrong answer as “0”.
Self-efficacy was assessed by Chronic Disease Self-Efficacy Scale which contains 6 items with internal reliability of Cronbach’s Alpha value 0.879.15 Responses were coded as completely unconfident = 1, unconfident = 2, not sure = 3, confident = 4, and totally confident = 5.
Moderation of alcohol consumption was assessed by the 4-item Fast Alcohol Screening Test (FAST) questionnaire which is a short version of the Alcohol Use Disorders Identification Test (AUDIT)16 with internal consistency of Cronbach’s Alpha value 0.783 and scored “never” as 0, “less than monthly” = 1, “monthly” = 2, “weekly” = 3, and “daily or almost daily” = 4.
Operational Definitions
Adherence: the extent to which a persons’ behavior corresponds with recommendations from health-care providers.
Adherence to lifestyle modifications: respondents who were adherent to diet, exercise, smoking and alcohol consumption related recommendations.
DASH: a diet rich in fruits, vegetables; low sodium, reduced saturated and total fat.
Diet-related adherence: in this study, those respondents who reported that they usually or always consumed a diet rich in vegetables, grains and fruits; rarely or never consume salt; rarely or never consumed foods rich in spices and saturated fat were considered to be adherent.
Exercise-related adherence: respondents who reported that they exercise for >30 minutes per day, at least three times per week.
Smoking-related adherence: respondents who reported that they either never smoked or have stopped smoking.
Alcohol consumption related adherence: respondents who reported that they either never consumed alcohol or whose overall score on FAST is < 3 were taken as adherent to moderation of alcohol consumption.
Co-morbidities: respondents with one or more medical conditions in addition to hypertension.
Knowledge about hypertension: respondents with scores above the mean value on hypertension evaluation of lifestyle and management scale were taken as having good knowledge about hypertension.
Social support: the support gained from family and non-family members. In this study, respondents whose score was above the mean value on the Duke Social Support and Stress scale were taken as having social support.
Self-efficacy: is the belief in one’s capabilities to organize and execute the courses of action required to produce given attainment. In this study, respondents who scored above the mean value on the 6-item Chronic Disease Self-Efficacy Scale were considered as having good self-efficacy to cope with and manage their disease.
Data Collection Tools
Data were collected through a structured, validated and pretested face to face interviewer-administered questionnaire which was adapted from different reviewed literatures3,8,13–16 since there were no available standard questionnaires to assess total adherence to lifestyle modifications. Primarily the questions were prepared in English and translated to the local language (Amharic); the Amharic version was used for interview and then retranslated back to English to ensure its consistency by bilingual experts. The interview took on average a total of 20 minutes.
The questionnaire contained information on socio-demographic, personal, social support, knowledge and behavioral related variables and lifestyle modification related variables which can be expressed in terms of DASH and low sodium diet, regular exercise, moderation of alcohol consumption and cessation of smoking. Duke Social Support and Stress Scale with 12 items was used to assess support gained from family and non-family.13 A modified 10-item hypertension evaluation of lifestyle and management (HELM) scale was used as a tool to measure respondents’ knowledge.14 Self-efficacy was assessed by Chronic Disease Self-Efficacy Scale which contains 6 items with internal reliability of Cronbach’s alpha value 0.879.15 Moderation of alcohol consumption was assessed with the 4-item Fast alcohol screening test (FAST) which is a short version of Alcohol Use Disorders Identification Test (AUDIT) with internal consistency of Cronbach’s alpha value 0.783.16
Pre-test in 5% of the selected patients was done by the principal investigator in Boru hospital which was not included in the study, to assess the content, approach of the questionnaire and to correct unclear and vague issues on the questionnaires.
Data Collection Procedure
Two data collectors (BSc nurses) and one BSc nurse for supervision activities were recruited. The data collectors and supervisor had previous experience of data collection. They were given training for one day on the method of extracting the needed information, how to fill the information on a structured questionnaire and the ethical aspect in approaching the participants as well as the aim of the study and contents of the instruments. Therefore, the data collectors were familiar for each question. They were to approach the participants in a polite and respectful manner. The supervisor monitored the data collection process of the data collectors daily and if any problem happened she tried to solve it or contact the principal investigator by phone or in person.
Data Quality Control
To assure the data quality, the questionnaire was originally prepared in English then translated to Amharic, then back to English by bilingual experts to keep its consistency and the data were collected and supervised by trained nurses. Each questionnaire was pre-tested and checked for its completeness, followed by modification. The principal investigator and supervisor were making spot-checks of at least 5 questionnaires per day. Reviewing the completed questionnaire by the data collectors ensures completeness and consistency of the informations that were collected.
Data Processing and Analysis
The collected data were checked visually for its completeness, and the responses were coded and entered into the computer using the Epi data version 4.4 statistical package and 10% of the responses were randomly selected and checked for the consistency of data entry. Then data were exported toStatistical Package for Social Science (SPSS) version 25.0 for data analysis. During the process of analysis, descriptive statistics was used to provide an overall and coherent presentation and description of the data. Binary logistic regression was done to evaluate the crude significant relation of each independent variable with dependent variable. Variables with a 95% CI and P-value ≤ 0.2 during the bivariable analysis were entered to multivariable logistic regression analysis to see the relative effect of confounding variables and interaction of variables. A P-value ≤ 0.05 was taken as a cut-off value for significance. The results were displayed by using tables and charts.
Results
Socio-Demographic Characteristics
A total of 301 eligible hypertensive patients who were attending chronic follow-up units of Dessie referral hospital were interviewed during the study period giving a response rate of 100%. The study included 154 (51.2%) males. The mean age of the respondents was 51 ± 17.16 years while 38.9% were more than 55 years old. The majority of the respondents (170; 56.5%) were Muslim by religion and 173 (57.5%) were married. About 268 (89.0%) of the respondents were Amhara by ethnicity. Out of the respondents 88 (29.2%) had attended college or university and 60 (19.9%) of respondents were governmental employees. One hundred and one (33.6%) respondents have an income of 1000–1999 Ethiopian Birr and 59 (19.6%) did not have a regular income and lived with support from others (Table 1).
Table 1.
Socio-Demographic Characteristics of Participating Respondents in Dessie Referral Hospital, North East Ethiopia, 2020 (n=301)
| Variables | Category | Frequency (n=301) | Percentage (100%) |
|---|---|---|---|
| Age | 18–35 | 67 | 22.3 |
| 36–45 | 69 | 22.9 | |
| 46–55 | 48 | 15.9 | |
| >55 | 117 | 38.9 | |
| Sex | Male | 154 | 51.2 |
| Female | 147 | 48.8 | |
| Religion | Orthodox | 84 | 27.9 |
| Muslim | 170 | 56.5 | |
| Protestant | 28 | 9.3 | |
| Catholic | 19 | 6.3 | |
| Ethnicity | Amhara | 268 | 89 |
| Oromo | 9 | 3 | |
| Tigre | 24 | 8 | |
| Marital status | Married | 173 | 57.5 |
| Not married | 28 | 9.3 | |
| Divorced | 45 | 15 | |
| Widowed | 55 | 18.3 | |
| Educational status | Cannot read and write | 67 | 22.3 |
| Read and write only | 43 | 14.3 | |
| Primary | 68 | 22.6 | |
| Secondary | 35 | 11.6 | |
| College/University | 88 | 29.2 | |
| Occupational status | Farmer | 38 | 12.6 |
| Governmental employee | 60 | 19.9 | |
| Private employee | 40 | 13.3 | |
| Private business | 51 | 16.9 | |
| Non-employed | 50 | 16.6 | |
| Laborer | 14 | 4.8 | |
| Retired | 48 | 15.9 | |
| Monthly income | No regular income | 59 | 19.6 |
| <1000 ETB | 33 | 11 | |
| 1000–1999 ETB | 101 | 33.6 | |
| 2000–2999 ETB | 61 | 20.3 | |
| ≥ 3000 ETB | 47 | 15.5 |
Personal Characteristics of Participants
Of the respondents 37 (12.3%) had blood pressure ≥160/100 mmHg and 139 (46.2%) participants had a normal BMI of between 18.5–24.9 kg/m2. One hundred and fifty-nine (52.8%) were hypertensive for four or more years and 130 (43.2%) were on hypertensive treatment for the same period. Most of the respondents (154; 51.2%) were on ≤ 2 antihypertensive medications. Most respondents (183; 60.8%) had co-morbidity, most commonly DM and renal disorder (85; 46.4%).
Knowledge About Hypertension
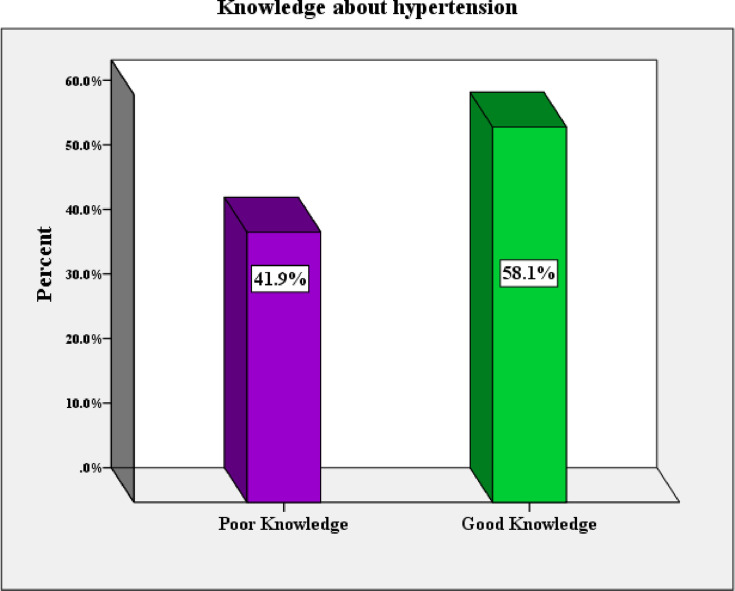
In order to determine level of respondents’ knowledge regarding hypertension, 10 modified questions from the 14-item hypertension evaluation of lifestyle and management (HELM) scale were used. We used the mean score (5.77+1.155) as the cut-off point (Figure 1).
Figure 1.
Knowledge about hypertension among respondents attending chronic follow-up units of Dessie referral hospital, North East Ethiopia, 2020.
Behavioral Characteristics of Participants
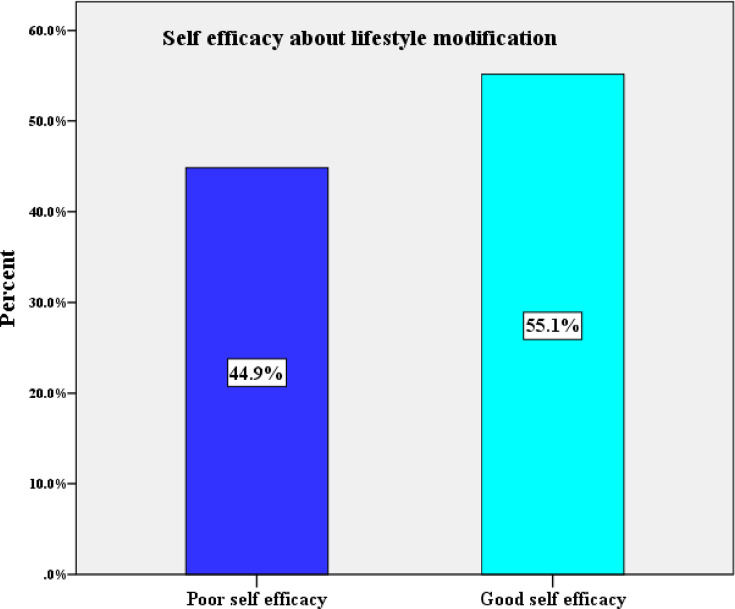
The 6-item Chronic Disease Self-Efficacy Scale was used to measure self-efficacy with 5 modified alternatives. The minimum and maximum score were 11 and 25 out of 30 respectively with a mean score of 19.85 and the standard deviation 3.51. Based on this mean value, 166 (55.1%) of study participants had good self efficacy (Figure 2).
Figure 2.
Self-efficacy of respondents attending chronic follow-up units of Dessie referral hospital, North East Ethiopia, 2020.
Social Characteristics of Participants
The Duke Social Support and Stress Scale which contains 12 items was used to assess support gained from family, friends or significant others. The total mean score of respondents’ social support on this scale was 48.38±16.75. By using this mean score as a cut-off point 148 (51%) of respondents benefited from social support from family, friends or significant others while 142 (49%) did not. From 148 respondents 143 (96.62%) got social support from their family whereas 5 (3.38%) respondents got non-family support.
Adherence to Diet
A majority (188; 62.5%) of the respondents included fruits, vegetables, grains and beans in their diet since their hypertension diagnosis. Almost 58%, 81.5% and 75.4% of total participants rarely or never consumed foods that contain high saturated fat, spicy foods and salt in their food since being diagnosed respectively.
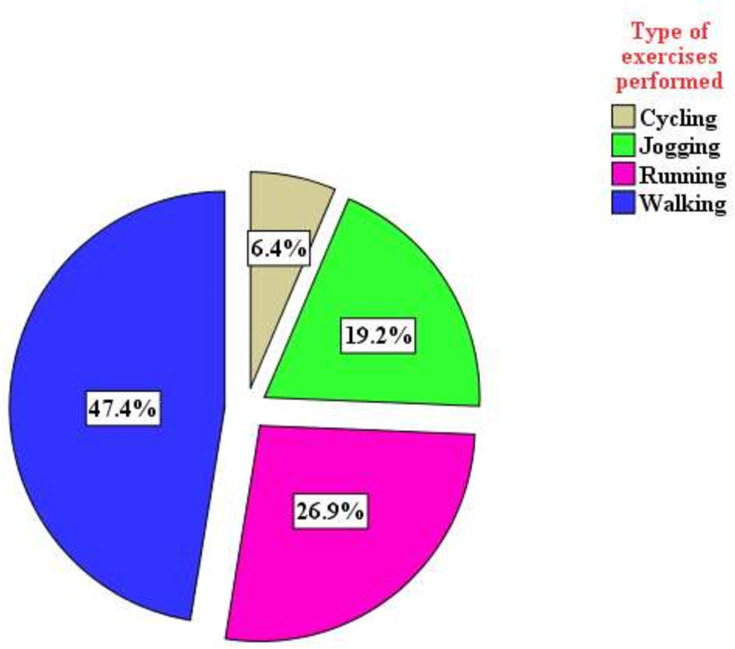
Adherence to Exercise
Approximately half (156; 51.8%) of the hypertensive patients performed physical exercise; of them 136 (87.2%) exercised three or greater than three times per a week and 126 (80.8%) participants exercised for at least 30 minutes per session. As shown in Figure 3, among 156 respondents who performed exercise walking was the dominant type (74; 47.5%) followed by running (42; 26.9%).
Figure 3.
Type of exercise performed by hypertensive patients attending chronic follow-up units at Dessie referral hospital, North East Ethiopia, 2020.
Adherence to Cessation of Smoking
About 9.6% of the patients had ever used tobacco; of these 37.9% were still smokers. Among 11 respondents who still smoked cigarettes five had tried to quit smoking.
Moderation of Alcohol
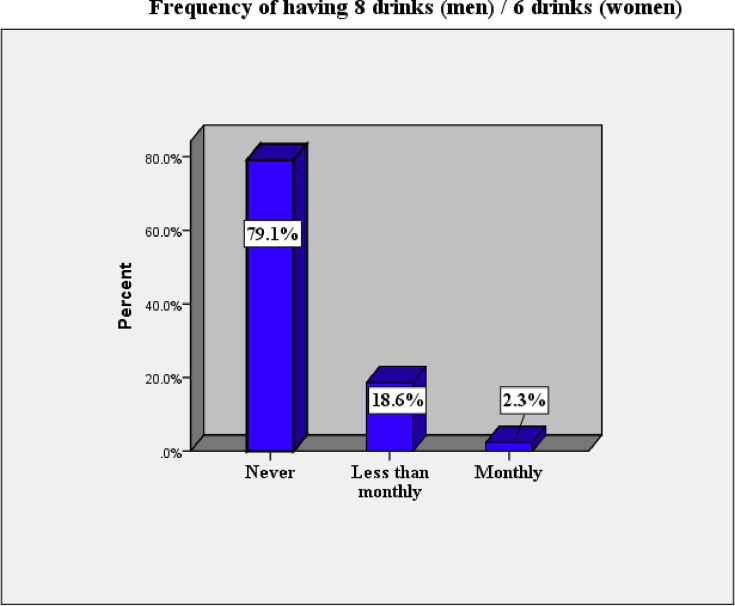
Based on the FAST score 283 (94%) hypertensive patients were FAST negative or adherent to moderation of alcohol consumption (Table 2). Figure 4 shows that 79.1% of the respondents never engaged in harmful drinking (>8 drinks for men and >6 for women) on one or more occasions. The remaining 18.6% and 2.3% of respondents engaged in harmful drinking less than monthly and monthly respectively. Out of the 63 respondents who reported that they consumed alcohol, the majority never had a history of inability to remember what happened after drinking the night before (91.7%) or failure to do what was expected from them in the last year (95%). Around 11.3% of these respondents confirmed that a relative/friend/doctor/health worker was concerned about their drinking and advised them to cut down on their drinking; 1.7% of them were advised before the last year and 9.6% during the last year.
Table 2.
Adherence to Recommended Lifestyle Modifications Among Hypertensive Patients Attending Chronic Follow-up Units at Dessie Referral Hospital, North East Ethiopia, 2020 (n=301)
| Variables | Category | Frequency (n=301) | Percentage (100%) |
|---|---|---|---|
| Adherence to diet | Non adherent | 71 | 23.6 |
| Adherent | 230 | 76.4 | |
| Adherence to exercise | Non adherent | 181 | 60.1 |
| Adherent | 120 | 39.9 | |
| Adherence to cessation of smoking | Non adherent | 31 | 10.3 |
| Adherent | 270 | 89.7 | |
| Moderation of alcohol | Not moderated | 18 | 6.0 |
| Moderated | 283 | 94.0 | |
| Overall adherence rate to lifestyle modifications | Non adherent | 230 | 76.4 |
| Adherent | 71 | 23.6 |
Figure 4.
Harmful drinking engagement habits based on Fast Alcohol Screening Test of respondents attending chronic follow-up units at Dessie referral hospital, North East Ethiopia, 2020.
Adherence to Recommended Lifestyle Modifications
The overall adherence (including diet, exercise, smoking cessation and moderation of alcohol consumption) in this study was only 23.6% with 95% CI of 18.6 – 28.4%. Around 76.4% of the total respondents were adherent to diet-related recommendations. Out of the total 301 participants only 120 (39.9%) were adherent to recommended physical activities. Around 270 hypertensive patients did not smoke or ceased smoking and 94% of respondents were adherent to moderation of alcohol consumption (Table 2).
Bivariable and Multivariable Analysis
The association of dependent and independent variables was investigated using bivariable and multivariable logistic regression models. Table 3 showed that age, sex, marital status, education level, occupational status, monthly income, having co-morbidities, knowledge level and self-efficacy were significantly associated with adherence to recommended lifestyle modifications from the bivariable binary logistic regression analysis model at P ≤ 0.2. After controlling the effect of other factors (confounders) in multivariable logistic regression, marital status, education level, monthly income, having co-morbidities, knowledge level and self-efficacy were found to be statistically significant predictors of adherence to recommended lifestyle modifications at P ≤ 0.05.
Table 3.
Factors Associated with Adherence to Recommended Lifestyle Modifications Among Hypertensive Patients Attending Chronic Follow-up Units at Dessie Referral Hospital, North East Ethiopia, 2020 (n=301)
| Variables | Adherence to Lifestyle Modifications | COR (95% CI) | AOR (95% CI) | P –value | ||
|---|---|---|---|---|---|---|
| Adherent (n=71) | Non-Adherent (n=230) | |||||
| Sex | Male | 43 | 111 | 1.00 | ||
| Female | 28 | 119 | 0.61 (0.35–1.04)* | |||
| Age in years | 18–35 | 16 | 51 | 1.85 (0.86–3.95)* | ||
| 36–45 | 21 | 48 | 2.57 (1.25–5.32)* | |||
| 46–55 | 17 | 31 | 3.23 (1.47–7.06)* | |||
| >55 | 17 | 100 | 1.00 | |||
| Marital status | Married | 53 | 120 | 1.00 | ||
| Not married | 6 | 22 | 0.62 (0.24–1.61)* | |||
| Divorced | 6 | 39 | 0.35 (0.14–0.87)* | 0.35 (0.13–0.94)** | 0.038 | |
| Widowed | 6 | 49 | 0.28 (0.11–0.69)* | 0.27 (0.10–0.75)** | 0.012 | |
| Educational status | Cannot read and write | 7 | 60 | 1.00 | 1.00 | |
| Read and write only | 6 | 37 | 1.39 (0.43–4.46) | 1.40 (0.40–4.94) | ||
| Primary | 12 | 56 | 1.84 (0.68–4.99) | 1.89 (0.63–5.71) | ||
| Secondary | 16 | 19 | 7.22 (2.58–20.16)* | 4.85 (1.54–15.22)** | 0.007 | |
| College/University | 30 | 58 | 4.43 (1.81–10.89)* | 1.62 (0.54–4.81) | ||
| Occupational status | Employed | 43 | 105 | 1.83 (1.06–3.14)* | ||
| Unemployed | 28 | 125 | 1.00 | |||
| Monthly income | No regular income | 9 | 50 | 0.82 (0.37–1.83)* | 0.22 (0.08–0.65)** | 0.006 |
| < 3000 ETB | 35 | 160 | 1.00 | 1.00 | ||
| ≥ 3000 ETB | 27 | 20 | 6.17 (3.11–12.23)* | 5.58 (2.46–12.66)** | 0.001 | |
| Presence of co-morbidities | Yes | 28 | 155 | 3.17 (1.83–5.50)* | 2.37 (1.23–4.57)** | 0.010 |
| No | 43 | 75 | 1.00 | 1.00 | ||
| Knowledge level | Good | 50 | 125 | 2.00 (1.13–3.54)* | 1.83 (0.92–3.65)** | 0.045 |
| Poor | 21 | 105 | 1.00 | 1.00 | ||
| Self-efficacy | Good efficacy | 57 | 109 | 4.52 (2.39–8.57)* | 3.64 (1.75–7.55)** | 0.001 |
| Poor Efficacy | 14 | 121 | 1.00 | |||
Notes: NB: *Variables having a (p≤ 0.2) in bivariable analysis, **Statistically significant at p≤ 0.05 in the multivariable analysis.
Compared with married adult hypertensive patients, divorced and widowed patients were 65% and 73% less likely to be adherent to recommended lifestyle modifications [AOR=0.35; 95% CI (0.13–0.94)] and [AOR=0.27; 95% CI (0.10–0.75)] respectively. Patients with educational status of secondary (Grades 9–12) were almost 5 times more likely to be adherent than respondents who were illiterate [AOR=4.85; 95% CI (1.54–15.22)]. Respondents who had no regular income were around 78% less likely to be adherent [AOR=0.22; 95% CI (0.08–0.65)], similarly those who had monthly income of 3000 ETB and greater were almost 6 times more likely to be adherent than those with less than 3000 ETB [AOR=5.58; 95% CI (2.46–12.66)]. The odds of being adherent to recommended lifestyle modifications by adult hypertensive patients who had co-morbidities were 2 [(AOR=2.37); CI (1.23–4.57)] times more as compared with patients without co-morbidities. Respondents with good knowledge were almost twice more likely to be adherent than those with poor knowledge [(AOR=1.83); CI (0.92–3.65)]. The participants who had good self-efficacy were approximately 4 [(AOR=3.64); CI (1.75–7.55)] times more likely to be adherent than those who had poor self-efficacy.
Discussion
Hypertension is one of the most important public health challenges in which patients’ outcomes are disability and death if it is not effectively prevented and controlled. Non-pharmacological management requires great attention in addition to pharmacological treatment to control hypertension and its complications. This study aimed to investigate adherence to recommended lifestyle modifications and associated factors among hypertensive patients attending chronic follow-up units of Dessie referral hospital, North East Ethiopia.
In this study the overall adherence (including diet, exercise, smoking cessation and moderation of alcohol consumption) among hypertensive patients was 23.6%. This finding was similar to studies in Iran (27.79%),17 SNNPR region of Ethiopia (27.3%)18 and Addis Ababa (23%).8 This might be due to the similarities of some parts of the standard tool as well as the study design used in all studies.
The adherence rate of the current study was lower than studies in India (54.7),9 Nepal (54%),19 and Ghana (72%).20 The possible reasons for this discrepancy might include tool differences, age differences in the study population (in this study patients were ≥18 years but in India patients were above 30 years of age), dietary habit difference between the countries,9 sample size and study period difference,19 tool quality difference and study area setup difference.20
In contrast this study’s adherence result was higher than findings from studies in the Kingdom of Saudi Arabia (4.2%)7 and Eastern Nigeria (16.4%).21 The possible justification for this difference might be due to variances in the study participants’ knowledge and awareness about the disease and lifestyle modification, living standard differences and gender inclusion (this study included men and women but the study in Saudi Arabia included only men),7 socio-cultural variation that influences lifestyle of individuals, methodological differences and low level of education and low level of awareness related to risk of hypertension complications.21
The prevalence of diet-related adherence of respondents in this study was 76.4%. This finding was higher than the study conducted in Saudi Arabia (11.8%).7 This discrepancy might be due to the study population gender proportion variance (only men were included in Saudi Arabia). Similarly our study finding on adherence to consumption of vegetables, fruits, unsaturated oil and reduction in dairy food intake in the control of high blood pressure was higher than the study in Nigeria (20%);10 this might be due to the current study having used a larger sample size, as well as socio-cultural differences. This result was also higher than that from a study done in Addis Ababa (69.1%).8 The possible reason for this variation might be due to a time difference in which the increment of the disease prevalence alerts people to be vegetarian and to eat the recommended healthy diet.
The current study found that around 39.9% were adherent to recommended physical activities . This result was comparable with a study conducted in the USA which reported 36.6% of hypertensive patients engaged in physical activity.22 However this result was lower than those from other studies in the USA (52.2%)6 and in the Aseer Region of Saudi Arabia (96.3%).23 The discrepancies in the adherence rate might be due to study population and methodological differences, and measuring instrument difference. The rate of physical exercise adherence in this study was also higher than studies in Nigeria (6.2%),24 12.9%,10 and Addis Ababa (31.4%).8 The possible justification for these discrepancies is the fact that adherence to physical exercise is a patient personal behavior and attitude that varies between different communities and cultures. It could be due to socio-economic status variation in which those people who live in low socio-economic areas are obligated to be pedestrians.
Regarding recommended moderation of alcohol consumption, the current study revealed around 94% of respondents were adherent. Some studies reported low levels of adherence to alcohol consumption as compared with our study finding; Nigeria (87.6%)24 and Addis Ababa (74.8%).8 The possible reasons might be socio-cultural differences and differences in study participants’ dominant religion (in our case more than half of participants were Muslim and thus do not consume alcohol due to their religious direction, but in the other studies most participants were not Islam).
The results of this study indicated that 89.7% of hypertensive patients did not smoke or ceased smoking. This finding was similar with study reports in Israel that stated 87% of study participants were adherent to smoking related recommendations.25 On the other hand the current study finding was lower than a study conducted in Eastern Nigeria (100.0%);21 this might be due to socio-cultural reasons, difference in patient education about the adverse effect of smoking and sample size variation. Moreover this finding was higher than studies done in USA (75%),6 Turkey (49.0%),26 and Addis Ababa (85.9%).8 This might be due to religious reasons, socio-cultural variance and methodological differences.
According to the multivariable analysis, marital status, education level, monthly income, having co-morbidities, knowledge level and self-efficacy were strongly associated with adherence to recommended lifestyle modifications. Our study concluded that compared with married adult hypertensive patients, divorced and widowed patients were 65% and 73% less likely to be adherent to recommended lifestyle modifications. This finding was supported by studies in Ghana20 - married patients were twice as likely to adhere to recommended lifestyle modifications than widowed patients, Addis Ababa27- married respondents were twice as likely to adhere to self-care practice compared with divorced respondents. This was possibly explained as married respondents give more concern for the choice of the recommended lifestyle by sharing ideas about its importance with each other. Also, a widowed or divorced individual’s life might not be stable enough for a lifestyle modification due to the absence of their partner.
Patients with educational status of secondary school were almost five times more likely to be adherent than illiterate respondents. This finding was consistent with findings of studies in China,28 Kingdom of Saudi Arabia,7 Ghana,20 Ayder Hospital-Tigray29 and Harar.30 The possible explanation might be related to an increment of patients’ awareness on the importance of recommended lifestyle modifications to prevent hypertension and its complications as formal education level rises. In addition it might be because illiterate respondents cannot read written information about the disease and recommended lifestyle modification.
Another finding of this study was respondents who had monthly income of 3000 ETB and greater were almost six times more likely to be adherent than those with less than 3000 ETB, which was supported by study findings in Kingdom of Saudi Arabia7 and Southern Ethiopia.18 The explanation might be that those patients with low monthly income cannot afford all domains of the recommended lifestyle and also they might not ever think about the modifications.
This study indicated that the odds of being adherent to recommended lifestyle modifications by adult hypertensive patients who had co-morbidities were two times higher compared with patients without co-morbidities. This result was mirrored by findings of studies in Saudi Arabia7 and Addis Ababa.8 The possible justification might be that the presence of other co-morbidities and their multiple burdens may incentivize patients to modify their lifestyle based on the recommendations. Also, lifestyle changes are easier to afford than medication, since medication is expensive.
According to our study result respondents with good knowledge of the disease were almost twice as likely to be adherent than those with poor knowledge. This was supported by studies done in the USA,31 Korea,32 Nigeria,33 Ayder hospital-Tigray29 and Addis Ababa.8 This is probably because knowledgeable patients might know about the disease, its severity, its complications and how it can be prevented, controlled and managed and asks health care providers about ambiguous information about it. Those participants who had good self-efficacy were approximately four times more likely to be adherent than those who had poor self-efficacy, which was supported by studies done in China,34 Addis Ababa8 and Jimma, Southwest Ethiopia.35 The possible explanation might be that the more confident patients are that they will be motivated and have emotional well‐being to modify their lifestyle based on the recommendations, the more likely they are to be adherent.
Strength of the Study
Since there were no similar studies conducted in this area, this study can offer ideas and information for further studies. The study uses appropriate descriptive and inferential statistics.
Limitations of the Study
The quantitative questionnaire might be prone to social desirability bias, because individuals do not want to expose any inability, and the cross-sectional nature of the design makes it difficult to draw causal relationships. The chosen participants might be less representative of other hypertensive patients since the selection process was completely consecutive due to the change of hypertensive patients’ appointment schedules from one month to three months because of the COVD 19 pandemic. There might be selection bias. It was very difficult to collect data due to the pandemic of COVD 19.
Conclusion
In this study we tried to identify the pattern of adherence to recommended lifestyle modifications and associated factors. The overall adherence to recommended lifestyle modifications among hypertensive patients in this study was very low. Independent predictors of adherence to lifestyle modifications were: marital status, educational level, monthly income, having co-morbidities, knowledge level, and self-efficacy.
Recommendations
Based on the findings of the study, the following recommendations were forwarded to the concerned body engaged in this area about adherence to life style modifications: Amhara Regional Health Bureau should create programs to increase hypertensive clients’ adherence capacity for lifestyle modifications and health-care facility managers should facilitate training for health-care professionals about lifestyle modifications to manage hypertension. Health-care providers should give special attention for the proper practice of lifestyle modifications. Health- care facilities should provide health education to hypertensive clientsabout recommended lifestyle modifications. It is important to increase information access to patients about risk factors, signs and symptoms of hypertension and the management as well as the recommendations of lifestyle modifications. More studies should be conducted on a larger scale especially at regional levels or nationwide to identify gaps in hypertensive patients’ adherence to lifestyle modifications and should consider qualitative aspects of the issue.
Acknowledgments
We acknowledge Wollo University for creating an opportunity to run this study. We also extend our gratitude to study participants, data collectors and supervisors.
Funding Statement
Wollo University fully covered the financial issues to handle this research.
Abbreviations
ADH, Adult Health Nursing; AUDIT, Alcohol Use Disorders Identification Test; BSc, Bachelor of Science; DASH, Dietary Approach to Stop Hypertension; DRH, Dessie Referral Hospital; DUSOCS, Duke Social Support and Stress Scale; FAST, Fast Alcohol Screening Test; HELM, Hypertension Evaluation of Lifestyle and Management; MPH, Master of Public Health; MSC, Master of Science; RCS, Research and Community Service; RH, reproductive health; SNNPR, Southern Nation and Nationality People Representative.
Data Sharing Statement
The datasets generated or analyzed during this study are available from the corresponding author but will be shared for only reasonable request in order to protect participants’ anonymity.
Ethics and Consent to Participate
Ethical clearance and supportive letter were obtained from Wollo University, College of Medicine and Health Sciences Research and Community Service (RCS) office in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. A supportive letter was given to the hospital and permission was obtained to start data collection. After gaining written consent from each respondent by telling each the objective of the study and assuring confidentiality, data collection was commenced anonymously.
Author Contributions
All authors made a significant contribution to the work reported; whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no conflicts of interest for this work.
References
- 1.Campbell NR, Lackland DT, Lisheng L, Niebylski ML, Nilsson PM, Zhang XH. Using the Global Burden of Disease study to assist development of nation‐specific fact sheets to promote prevention and control of hypertension and reduction in dietary salt: a resource from the World Hypertension League. J Clin Hypertension. 2015;17(3):165–167. doi: 10.1111/jch.12479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mills KT, Bundy JD, Kelly TN, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016;134(6):441–450. doi: 10.1161/CIRCULATIONAHA.115.018912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Organization WH. A Global Brief on Hypertension: Silent Killer, Global Public Health Crisis: World Health Day 2013. World Health Organization; 2013. [Google Scholar]
- 4.Abebe S, Yallew WW. Prevalence of hypertension among adult outpatient clients in hospitals and its associated factors in Addis Ababa, Ethiopia: a hospital based cross-sectional study. BMC Res Notes. 2019;12(1):87. doi: 10.1186/s13104-019-4127-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Finkelstein R, Kamber T, Mollenkopf JH. The Aging City. CUNY: Graduate Center; 2013. [Google Scholar]
- 6.Warren-Findlow J, Seymour RB. Prevalence rates of hypertension self-care activities among African Americans. J Natl Med Assoc. 2011;103(6):503–512. doi: 10.1016/S0027-9684(15)30365-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Elbur AI. Level of adherence to lifestyle changes and medications among male hypertensive patients in two hospitals in Taif; Kingdom of Saudi Arabia. Int J Pharm Pharm Sci. 2015;7(4):168–172. [Google Scholar]
- 8.Tibebu A, Mengistu D, Negesa L. Adherence to recommended lifestyle modifications and factors associated for hypertensive patients attending chronic follow-up units of selected public hospitals in Addis Ababa, Ethiopia. Patient Prefer Adherence. 2017;11:323. doi: 10.2147/PPA.S126382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Verma P, Srivastava M, Ratan K. Assessment of extent of lifestyle modification among diagnosed patients of hypertension attending tertiary care hospital. Int J Med Health Sci. 2015;4(2):196–201. [Google Scholar]
- 10.Okwuonu C, Emmanuel C, Ojimadu N. Perception and practice of lifestyle modification in the management of hypertension among hypertensives in south-east Nigeria. Int J Med Biomed Res. 2014;3(2):121–131. doi: 10.14194/ijmbr.3.2.8 [DOI] [Google Scholar]
- 11.Ademe S, Aga F, Gela D. Hypertension self-care practice and associated factors among patients in public health facilities of Dessie town, Ethiopia. BMC Health Serv Res. 2019;19(1):51. doi: 10.1186/s12913-019-3880-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ghezelbash S, Ghorbani A. Lifestyle modification and hypertension prevention. ARYA Atheroscler. 2012:202–207. [Google Scholar]
- 13.Parkerson G. Duke Social Support and Stress Scale (DUSOCS). Vol. 2 Nueva York: Oxford University Press; 2007:252–254. [Google Scholar]
- 14.Schapira MM, Fletcher KE, Hayes A, et al. The development and validation of the hypertension evaluation of lifestyle and management knowledge scale. J Clin Hypertens. 2012;14(7):461–466. doi: 10.1111/j.1751-7176.2012.00619.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hu H, Li G, Arao T. Validation of a Chinese version of the self-efficacy for managing chronic disease 6-item scale in patients with hypertension in primary care. ISRN Public Health. 2013:2013. [Google Scholar]
- 16.Hodgson R, Alwyn T, John B, Thom B, Smith A. The FAST alcohol screening test. Alcohol Alcoholism. 2002;37(1):61–66. doi: 10.1093/alcalc/37.1.61 [DOI] [PubMed] [Google Scholar]
- 17.Akbarpour S, Khalili D, Zeraati H, Mansournia MA, Ramezankhani A, Fotouhi A. Healthy lifestyle behaviors and control of hypertension among adult hypertensive patients. Sci Rep. 2018;8(1):1–9. doi: 10.1038/s41598-018-26823-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Buda ES, Hanfore LK, Fite RO, Buda AS. Lifestyle modification practice and associated factors among diagnosed hypertensive patients in selected hospitals, South Ethiopia. Clin Hypertens. 2017;23(1):26. doi: 10.1186/s40885-017-0081-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bhandari B, Bhattarai M, Bhandari M, Jha N. Awareness of disease and self care among hypertensive patients attending Tribhuvan University Teaching Hospital, Kathmandu, Nepal. J Nobel Med Coll. 2011;1(2):29–35. doi: 10.3126/jonmc.v1i2.7296 [DOI] [Google Scholar]
- 20.Obirikorang Y, Obirikorang C, Acheampong E, et al. Adherence to lifestyle modification among hypertensive clients: A descriptive cross-sectional study. Open Access Libr J. 2018;5(2):1–13. [Google Scholar]
- 21.Iloh GUP, Amadi AN, Okafor GOC, Ikwudinma AO, Odu FU, Godswill-Uko EU. Adherence to lifestyle modifications among adult hypertensive Nigerians with essential hypertension in a primary care clinic of a tertiary hospital in resource-poor environment of Eastern Nigeria. J Adv Med Res. 2014;3478–3490. doi: 10.9734/BJMMR/2014/9439 [DOI] [Google Scholar]
- 22.Kim H, Andrade FC. Diagnostic status and age at diagnosis of hypertension on adherence to lifestyle recommendations. Prev Med Rep. 2019;13:52–56. doi: 10.1016/j.pmedr.2018.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Al-Gelban KS, Khan MY, Al-Khaldi YM, et al. Adherence of primary health care physicians to hypertension management guidelines in the Aseer region of Saudi Arabia. Saudi J Kidney Dis Transpl. 2011;22(5):941. [PubMed] [Google Scholar]
- 24.Ayodapo A, Olukokun T. Lifestyle counselling and behavioural change: role among adult hypertensives in a rural tertiary institution. S Afr Fam Pract. 2019;61(3):91–96. doi: 10.1080/20786190.2019.1569453 [DOI] [Google Scholar]
- 25.Heymann AD, Gross R, Tabenkin H, Porter B, Porath A. Factors associated with hypertensive patients’ compliance with recommended lifestyle behaviors. IMAJ. 2011;13(9):553. [PubMed] [Google Scholar]
- 26.Selçuk KT, Çevik C, Mercan Y, Koca H. Hypertensive patients’ adherence to pharmacological and non-pharmacological treatment methods, in Turkey. Int J Community Med Public Health. 2017;4(8):2648. doi: 10.18203/2394-6040.ijcmph20173308 [DOI] [Google Scholar]
- 27.Hareri HA, Abebe M, Asefaw T. Assessments of adherence to hypertension managements and its influencing factors among hypertensive patients attending black lion hospital chronic follow up unit, Addis Ababa, Ethiopia-a cross-sectional study. Int J Pharm Sci Res. 2013;4(3):1086. [Google Scholar]
- 28.Tam HL, Wong EML, Cheung K. Effectiveness of educational interventions on adherence to lifestyle modifications among hypertensive patients: an integrative review. Int J Environ Res Public Health. 2020;17(7):2513. doi: 10.3390/ijerph17072513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gebremichael GB, Berhe KK, Beyene BG, Gebrekidan KB. Self-care practices and associated factors among adult hypertensive patients in Ayder Comprehensive Specialized Hospital, Tigray, Ethiopia, 2018. BMC Res Notes. 2019;12(1):489. doi: 10.1186/s13104-019-4502-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nadewu AN, Geda B. Adherence to healthy lifestyle among hypertensive patients in Harar Region, Eastern Ethiopia. Primary Health Care. 2018;8(4):1–7. [Google Scholar]
- 31.Abu HO, Aboumatar H, Carson K, Goldberg RJ, Cooper L. Hypertension knowledge, heart healthy lifestyle practices and medication adherence among adults with hypertension. Eur J Pers Cent Healthc. 2018;6:108. doi: 10.5750/ejpch.v6i1.1416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shim J-S, Heo JE, Kim HC. Factors associated with dietary adherence to the guidelines for prevention and treatment of hypertension among Korean adults with and without hypertension. Clinical Hypertension. 2020;26(1):1–11. doi: 10.1186/s40885-020-00138-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Iyalomhe GB, Iyalomhe SI. Hypertension-related knowledge, attitudes and life-style practices among hypertensive patients in a sub-urban Nigerian community. J Public Health Epidemiol. 2010;2(4):71–77. [Google Scholar]
- 34.Hu H, Li G, Arao T. The association of family social support, depression, anxiety and self-efficacy with specific hypertension self-care behaviours in Chinese local community. J Hum Hypertens. 2015;29(3):198–203. [DOI] [PubMed] [Google Scholar]
- 35.Labata BG, Ahmed MB, Mekonen GF, Daba FB. Prevalence and predictors of self care practices among hypertensive patients at Jimma University Specialized Hospital, Southwest Ethiopia: cross-sectional study. BMC Res Notes. 2019;12(1):86. doi: 10.1186/s13104-019-4125-3 [DOI] [PMC free article] [PubMed] [Google Scholar]