Supplemental Digital Content is available in the text.
Background:
The prevalence of alcohol use disorder (AUD) and alcohol-associated liver disease is increasing in the United States. Efficacious AUD pharmacotherapies, while available, are, for protean reasons, underutilized. Hepatology providers may be in a position to bridge the pharmacotherapeutic gap between availability and utilization of AUD pharmacotherapies. Our aim was to ascertain the current practice, knowledge and attitudes of hepatology physicians in the United States, and identify opportunities on how to increase AUD medication prescribing.
Methods:
A web-based survey, developed by an expert panel, was administered to hepatology physicians working at all transplant centers in the United States.
Results:
The survey response rate was 131/658 (20%). There was significant support (two-thirds of respondents) for hepatology providers prescribing AUD medications; however, only 1 in 4 was comfortable prescribing these medications. The majority felt additional education is needed to prescribe AUD medications. The practice of hepatology providers prescribing AUD medications is common, with >50% of respondents having done so. Baclofen was the most popular medication prescribed. Hepatology providers perceived suboptimal ancillary addiction services. Although AUD prescribers had higher rates of AUD pharmacotherapy knowledge compared with nonprescribers, approximately 50% still had inadequate knowledge.
Conclusions:
AUD medication prescribing is a common practice among hepatology providers who appear eager to increase this practice through more education as they attempt to bridge the pharmacotherapeutic gap. This informative survey provides guidance for professional societies on how best to disseminate the requisite education required to optimize the care of patients with AUD.
INTRODUCTION
Alcohol use disorder (AUD) is a chronic relapsing disorder manifesting as compulsive alcohol use, loss of control over alcohol consumption, continued use despite mounting consequences, and a negative emotional state during periods of abstinence. The diagnosis of AUD is based on criteria set forth by the Fifth Edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), with the term AUD superseding prior conceptualizations of “alcohol abuse” and “alcohol dependence.”1 The prevalence of AUD has been increasing in the United States over time, with 15.1 million adults in the United States (5.6%) meeting the diagnostic criteria for AUD and 6% of the US population engaged in heavy drinking in 2016.2 Consequently, alcohol-associated liver disease (ALD) is now the leading cause of mortality from cirrhosis and the leading indication for liver transplantation in the United States.3-6
Guidelines from the American Association for the Study of Liver Diseases recommend that patients with advanced ALD and who are still drinking be referred to AUD treatment professionals for evaluation of possible approved pharmacotherapies that increase abstinence and reduce relapse rates.7 There are 3 FDA-approved medications for AUD treatment: disulfiram, naltrexone, and acamprosate. The number needed to treat to prevent return to any drinking is estimated to be around 12 for acamprosate and 20 for naltrexone, emphasizing their efficacy.8 To provide some context, the number needed to treat for statins for primary prevention of atherosclerotic cardiovascular disease in statin-eligible patients has been found to be 49.9 Tailored treatment is necessary given their adverse effects profile, such as hepatotoxicity with naltrexone, due to its hepatic metabolism. In addition, there are non-FDA-approved medications which have been found to have some benefit in AUD, such as gabapentin, baclofen, topiramate, and varenicline.10-14 Notably, baclofen has been the only medication to be studied in AUD patients with cirrhosis. Although it is clear that a combined treatment approach with behavioral therapy is the optimal strategy,15 pharmacotherapy is a vital component.16
Despite the increased recognition of the ALD epidemic fueled by AUD, pharmacotherapy of patients with AUD remain relatively underutilized in the context of established efficacy. A recent Veteran Affairs healthcare system study highlighted the extent of this deficiency, reporting that only 0.4% of AUD patients received pharmacotherapy alone and 1% received both behavioral and pharmacotherapy over a 180-day period after initial diagnosis.17 Importantly, in this study, pharmacotherapy-based AUD treatment alone (versus no AUD treatment) was associated with a significant reduction in incident hepatic decompensation (5.5% versus 11.6%) and in mortality (0.6% versus 3.9%).17 Further studies are needed to confirm this mortality benefit. The reasons for underutilization of AUD pharmacotherapy appear multifactorial, with a significant factor undoubtedly being the shortage of addiction specialist physicians in the United States. There are only approximately 4400 actively practicing certified addiction specialist physicians in the United States, which is far below the 6000 that were needed based on an estimate in 2009.18 Considering that this projection was made over a decade ago and we have now experienced an opioid epidemic in addition to a rise in AUD, it is now likely that this disparity is even greater.
Many patients with AUD are inevitably assessed regularly in hepatology clinics, providing an excellent opportunity for hepatology providers to bridge this gap and prescribe appropriate pharmacotherapy and potentially help obviate patients from the associated mortality and morbidity. The extent of this practice among hepatology providers in the United States is unknown. Ascertaining this information is essential to better understand the optimal approach to improving the treatment of patients with AUD and liver disease in the future. Thus, the aim of this study was to ascertain the current practice, knowledge and attitudes of hepatology providers at liver transplant centers in the United States, where the key patterns of this practice are captured, with regard to treatment of patients with AUD with pharmacotherapy.
MATERIALS AND METHODS
Survey Development and Recruitment
In collaboration with the University of Chicago Survey Lab, a survey was developed by an expert panel encompassing of hepatologists with expertise in ALD and AUD pharmacotherapy and an addiction specialist with expertise in AUD. The language of survey questions was edited and finalized by experts on survey administration from the University of Chicago Survey Lab to ensure the optimal comprehension and answering of questions. This survey instrument was programmed into Qualtrics online survey platform. Text of the questionnaire can be found in Appendix S1 A (SDC, http://links.lww.com/TXD/A280). Institutional Review Board approval was obtained before study onset (IRB20-0288—The Division of Social Sciences, The University of Chicago, Chicago, IL).
Inclusion criteria included board-certified/board-eligible transplant hepatologists or gastroenterologists caring for patients with liver disease at all US liver transplant centers (including Hawaii and Puerto Rico) that performed at least one liver transplant in 2019, as ascertained from the Organ Procurement and Transplantation Network database.19 Exclusion criteria included inability to obtain contact information, or voluntary withdrawal from survey after initial contact. A comprehensive email address list was compiled of the relevant physicians ascertained from publicly accessible resources, professional society membership directories and from direct contact with personnel in the respective institutions. There were 662 physicians identified as meeting the study inclusion criteria, and email addresses were available on the majority of them (658/662, 99%).
The survey response collection period was from February 27, 2020 to March 21, 2020. The survey was prospectively administered via an initial invitational email sent on February 27, 2020, and 3 subsequent emails were sent to those who neither responded nor opted out at the date of the prompt. The text of these emails is found in Appendix S1 B (SDC, http://links.lww.com/TXD/A280). There were 65 respondents to the first email, 35 to the second, 21 to the third, and 11 to the fourth, resulting in a total sample size of 131. The overall response rate using standard American Association for Public Opinion Research Response Rate 2 was 20%.20 This is summarized in Table 1. Ninety out of 131 (68.7%) respondents wished to be entered into a drawing for one of four $250 Amazon gift cards.
Table 1.
Summary of the survey response
| N | Percent of total (%) | Percent of received (%) | Percent of opened (%) | |
|---|---|---|---|---|
| Emails sent | 658 | 100.0 | ||
| Received | 656 | 99.7 | ||
| Email not deliverable | 2 | |||
| Opted out | 12 | 1.8 | 1.8 | |
| Did not open the survey | 467 | 71.0 | 71.2 | |
| Opened the survey | 166 | 25.2 | 25.3 | |
| Did not complete | 35 | 5.3 | 5.3 | 21.1 |
| Completed partially | 2 | 0.3 | 0.3 | 1.2 |
| Completed fully | 129 | 19.6 | 19.7 | 77.7 |
Statistical Analysis
The data analysis was largely descriptive with comparative analysis, including stratified analysis, performed where appropriate. Continuous variables were summarized with means and standard deviations, and frequencies and percentages were used for categorical variables. Comparative analysis of categorical variables was based on the two-sided chi-square test. A P-value of <0.05 was considered significant for all statistical methods used. The statistical analyses were completed using the Stata statistical package (Stata Statistical Software: Release 16; StataCorp LLC, College Station, TX).
RESULTS
Demographics
The demographics and practice setting of the respondents are outlined in Table 2. Of note, there was no statistical difference observed in sex distribution between responders and non-responders (P = 0.898). All 11 United Network for Organ Sharing (UNOS) regions were represented. The majority of respondents were non-Hispanic White (55%). Almost half of respondents (45%) had less than 10 years of practice post-fellowship, and 75% were aged between 36 and 55 years of age. The vast majority worked at a University Hospital (90%), and 61% were at a high-volume transplant center (>80 transplants annually). On average, each respondent evaluated 6 patients with active AUD per week in their scope of practice.
Table 2.
Demographics and practice setting of survey respondents (N = 131)
| Variable | n (%) |
|---|---|
| GI or Hepatology board-certified | 126 (96.2) |
| Years of practice post-fellowship: 0–10 y | 59 (45.0) |
| 11–20 y | 38 (29.0) |
| >20 y | 34 (26.0) |
| UNOS regions: 1 (3.7%a) | 4 (3.2) |
| 2 (11.5%a) | 15 (11.5) |
| 3 (16.2%a) | 11 (8.4) |
| 4 (10.4%a) | 7 (5.3) |
| 5 (15.8%a) | 16 (12.2) |
| 6 (2.8%a) | 4 (3.1) |
| 7 (7.8%a) | 34 (26.0) |
| 8 (6.4%a) | 7 (5.3) |
| 9 (5.7%a) | 10 (7.6) |
| 10 (9.9%a) | 10 (7.6) |
| 11 (9.8%a) | 13 (9.9) |
| Male sex | 90 (68.7) |
| Age range: 25–35 y | 12 (9.2) |
| 36–45 y | 57 (43.5) |
| 46–55 y | 29 (22.1) |
| 56–65 y | 24 (18.3) |
| >65 y | 7 (5.3) |
| Race/ethnicity: non-Hispanic White | 72 (55.0) |
| Asian | 31 (23.7) |
| Hispanic | 15 (11.5) |
| Other | 13 (9.9) |
| Hospital setting: university-based or -affiliated | 118 (90.1) |
| Community | 10 (7.6) |
| Number of liver transplants in 2019: 1–40 | 23 (17.6) |
| 40–80 | 28 (21.4) |
| >80 | 80 (61.0) |
| Average number of patients with liver disease per weekb | 33.5 ± 16.6 |
| Average number of patients with ALD per weekb | 11.8 ± 7.6 |
| Average number of patients with active AUD per weekb | 6.0 ± 5.5 |
aPercent of overall liver transplants in the United States in 2019.
bEvaluated by each respondent.
ALD, alcohol-associated liver disease; AUD, alcohol use disorder; GI, gastroenterology; UNOS, United Network for Organ Sharing.
Practice Habits
Among respondents, 78 (59.5%) have treated a patient with ALD with a first- or second-line AUD medication to prevent relapse or reduce cravings. There was notable geographic variation with this practice being most prevalent in the Northeast and least prevalent in the Northwest (Figure 1A). There was no difference in this practice when stratified by level of experience (ie, years post-fellowship) (P = 0.724), age (P = 0.538), transplant center volume (>80 liver transplants versus <80 liver transplants per year) (P = 0.336), or by AUD patient volume (≥5 AUD patients versus <5 AUD patients per week) (P = 0.069). Of these 78 respondents, only 2 (2.6%) have received what they would consider formal training in AUD treatment, although this was not an addiction medicine fellowship or training course or AUD training course. Over the past 12 months, 22 (16.8%) of respondents have treated greater than 20% of their active AUD patient population with AUD medications, with 4 (4.6%) treating more than 40% of their active AUD patient population.
FIGURE 1.
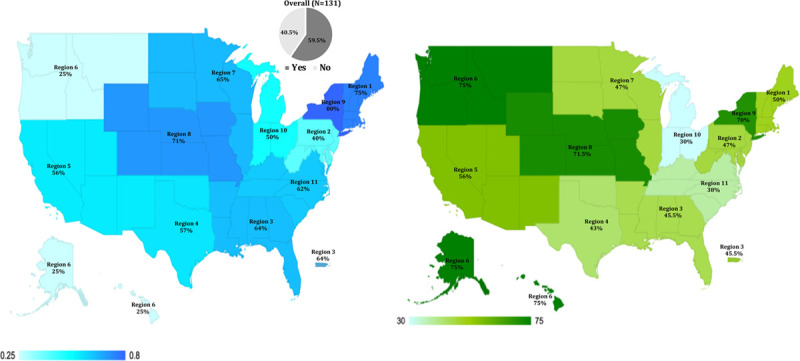
A, The geographic variation of hepatology providers who have prescribed alcohol use disorder (AUD) medications. The percentage of hepatology providers who have ever prescribed AUD medication over the total number of respondents in each UNOS geographic regions is shown. Darker color indicates higher percentage of AUD prescribers. B, The geographic variation of hepatology providers perceived access to Addiction Psychiatry services. The percentage of hepatology providers who have adequate access to Addiction Psychiatry (defined as being able to have suitable patients evaluated by Addiction Psychiatry in a timely manner at least half of the time, or better) over the total number of respondents in each UNOS geographic region is shown. Darker color indicates higher percentage of AUD prescribers. Source: Microsoft PowerPoint Version 16.16.22. UNOS, United Network for Organ Sharing.
Among the respondents who prescribed AUD medications over the previous 12 months, baclofen (37/69 = 53.6%) was the most commonly prescribed medication, followed by naltrexone (15/69, 21.7%), acamprosate (9/69, 13.0%), and gabapentin (7/69, 10.1%). Disulfiram was not used by any of the respondents as first line, but 4/69 (5.8%) reported prescribing it as their second most commonly prescribed AUD medication.
The availability of ancillary addiction services (Addiction Psychiatry, Psychotherapy, AUD Rehabilitation Programs) was perceived by hepatology providers as inadequate (Figure 2). Among the 119 respondents who have referred patients with AUD to Addiction Psychiatry, the majority (82, 69%) were unable to have these patients evaluated in a timely manner, that is, within 4 weeks. The reasons for this deficiency included poorly resourced (59/82, 72.0%) or absent addiction psychiatry services (23/82, 28.0%). One respondent described lack of interest of the liver transplant team in addiction services. Forty-two (35%) respondents reported they were rarely or never able to have their patients evaluated by Addiction Psychiatry in a timely manner. Over half (67/131, 51.1%) of respondents reported that AUD-specific psychotherapy services were only available less than half the time or rarely/never at their institutions, whereas 78/131 (59.5%) found it somewhat to very difficult for their patients with AUD to gain access to AUD rehabilitation programs. There was no difference in perceived accessibility to these ancillary services when stratified by liver transplant volume or by AUD patient volume (all P values >0.5). The geographic variation of hepatology providers who perceived themselves to have adequate access to Addiction Psychiatry, by UNOS region, is displayed in Figure 1B.
FIGURE 2.
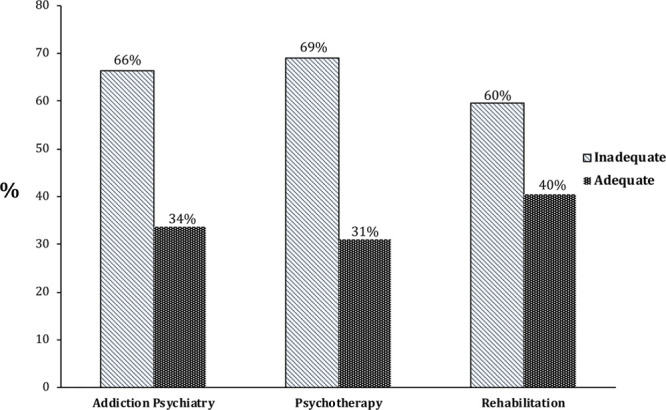
The accessibility of timely ancillary AUD services (ie, Addiction Psychiatry, Psychotherapy, and AUD Rehabilitation Programs) as perceived by hepatology providers. The majority of hepatology providers feel that they have inadequate access to these services (defined as having patients seen in a timely manner either half the time, less than half the time, or rarely or never). AUD, alcohol use disorder.
Knowledge
There were 3 questions included in the study that all members of the expert panel agreed were standard knowledge items expected of regular prescribers of AUD medications (Appendix A S1, SDC, http://links.lww.com/TXD/A280). For the first question, nearly half of respondents, 57/129 (44.2%), failed to identify that gabapentin is not FDA-approved for treatment of AUD. For the second item, the majority, 75/129 (58.1%), failed to correctly choose baclofen as the only AUD medication that has been studied in patients with advanced liver disease. Finally, for the third question, over half of respondents, 68/129 (52.7%), did not correctly select naltrexone as having an FDA black box warning for hepatotoxicity. Respondents who reported prescribing AUD medications had a higher proportion of correct answers compared with respondents who did not prescribe AUD medications for the questions on baclofen and naltrexone, whereas no difference was observed for the gabapentin question (Figure 3).
FIGURE 3.
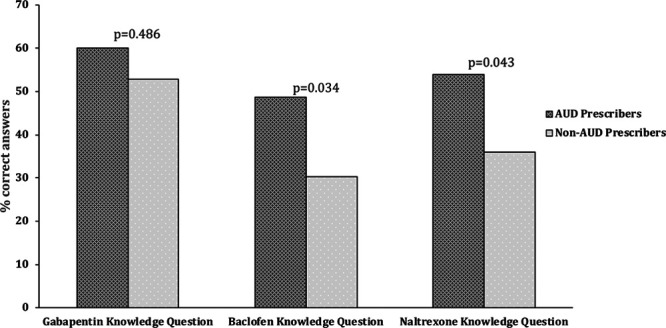
Comparison of alcohol use disorder (AUD) medication knowledge between hepatology providers who prescribe them and those who do not. Prescribers of AUD medications have higher rates of knowledge of AUD medications, however, around half of them still failed to get the correct answers.
Attitudes
Almost one-third of hepatology providers (84/129, 65.1%) endorsed the prescribing AUD medications by hepatology providers, whereas only 18/129 (14.0%) opposed this practice. Providers at higher volume centers (versus lower volume) (P = 0.023) and physicians who had a higher AUD patient volume (vs lower volume) (P = 0.028) were more likely to support hepatology providers prescribing AUD medications. There was no difference in hepatology provider support for prescribing AUD medications when stratified by experience (P = 0.938), age (P = 0.910). Of the 18 respondents who did not support hepatology providers prescribing AUD medications, there were 17 responses that deemed it not to be part of a hepatology provider’s job, 12 responses citing perceived inadequate clinic resources, and finally, 12 responses endorsing inadequate AUD medication knowledge.
Less than one-third of respondents (35/129, 27.1%) reported being mostly or very comfortable with prescribing AUD medications. Providers working at a higher volume liver transplant center (versus lower volume) (P = 0.025) and who had higher AUD patient volume (versus lower volume) (P = 0.020) were more likely to be comfortable prescribing AUD medications. However, there was no difference in providers’ comfort level when stratified by experience (P = 0.327), age (P = 0.910) or by perception of Addiction Psychiatry availability (P = 0.885). Not surprisingly, respondents who have prescribed AUD medications had higher rates of being mostly or very comfortable with prescribing AUD medications compared with those who have never prescribed AUD medications (41.0% versus 5.7%, P < 0.001).
Slightly over half of respondents (67/129, 51.9%) felt that additional training should be required beyond medicine/gastroenterology (GI)/hepatology boards to prescribe AUD medications. The most highly endorsed popular option selected for increasing provider’s awareness of AUD pharmacotherapy was integration into fellowship as an option for trainees, endorsed by 85/129 (65.9%) of respondents. Online modules were next most popular (81/129, 62.7%), followed by webinars (71/129, 55%), and in-person didactics (66/129, 51%). The least popular modality was formal certification for prescribing AUD medications, with only 33/129 (25.5%) of respondents selecting this option.
DISCUSSION
The practice of hepatology providers prescribing AUD medications for their patients is common, with over half of respondents having done so, despite no formal training. There is geographic variation with AUD medication prescribing particularly prevalent in the Northeast. Among prescribers, baclofen is the most endorsed first-line option. As expected, hepatology providers perceived suboptimal availability of ancillary addiction services. Approximately 50% of AUD prescribers failed to answer standard AUD medication questions correctly about gabapentin, baclofen, and naltrexone. Although two-thirds of respondents prescribed AUD medications to suitable patients, only 1 in 4 reported being comfortable prescribing such medications. Importantly, the majority of respondents endorsed the prescribing of AUD medications by hepatology providers but did feel that additional training should be required. These factors should serve as strong impetus for tailored training programs for all providers who manage patients with liver disease to help address the underutilization of AUD medications.18
Despite minimal formal training in addiction medicine, the practice of prescribing AUD medications among hepatology providers is relatively high, with 3 in every 5 respondents having done so in the past. Age, experience, volume of transplants, and AUD patient volume did not affect prescribing rates. Almost 1 in 5 of respondents have treated >20% of their active AUD patient population over the past 12 months, with 1 in 20 treating >40%. This is encouraging and indicates a relatively solid platform to build upon to increase AUD prescribing rates. Concordance with high rates of AUD prescribers in UNOS regions 3 and 8 (Southern United States) and this region’s high rates of binge drinking was also noted.21 The Northeast of the United States reported the highest rates of AUD medication prescribing. Interestingly, the Northeast is the region with the highest rates of liver transplantation for alcoholic hepatitis, a severe consequence of AUD.6 Evidently, providers in this region may be more attuned to AUD medication prescribing than other areas.
As has been established previously,18 hepatology providers generally perceived inadequate access to ancillary addiction services. Although there are other specialties such as addiction medicine-trained internal medicine doctors who help manage patients with AUD, addiction psychiatrists are putatively the most highly trained to treat and manage such patients. Interestingly, the patterns of accessibility to addiction psychiatry tracked to some degree with hepatology providers who prescribed AUD medications. For example, the Northeast and UNOS region 8 (the Mountain West and Midwest regions) had higher rates prescribing AUD medications and also had the highest perceived “adequate” accessibility to Addiction Psychiatry services. This may reflect the interchange of education and information that occurs between specialties working close together. This trend was not observed in the Northwest; however, this region had the least number of respondents (ie, 4), limiting inference validity. The ongoing addiction services shortage highlights the need for hepatology providers to bridge the pharmacotherapeutic gap while making simultaneous attempts to link to additional addiction behavioral services such as behavioral therapies.
There is little existing information on hepatology provider’s AUD medication preferences. Although tailored medication selection is necessary,7 baclofen was the most endorsed first-line therapy. Baclofen has been shown to be effective12-14 and is the only AUD medication studied in advanced liver disease, making it a viable option for hepatology providers. Of note, baclofen is not FDA-approved for AUD treatment, and thus, it is being prescribed off-label. The suboptimal knowledge of AUD medications observed from AUD prescribers highlights the need for education. This study also emphasizes that although overall enthusiasm exists among hepatology providers to AUD prescribing, the willingness to prescribe pharmacotherapies for AUD may be hampered by comfort level, mainly attributed to inadequate knowledge. The majority of respondents felt that additional training should be required beyond fellowship training such as integration into fellowship as an option for trainees and online modules for post-graduate training. This information should serve to help guide professional societies how best to disseminate the requisite education needed to help increase provider competence in providing AUD medication to suitable patients. A particular effort should also be made to extend this education to all GI and advanced practice practitioners in community-based practices where many of the AUD patient population are regularly managed.
The strengths of this study include a well-defined study population at every liver transplant center in the United States with a valid response rate and full accountability of the population ensuring good internal validity. Our response rate of 20% compares favorably to other transplant center survey studies which achieved a response rate of 14%.22 There has been another survey among liver transplant centers with a higher response rate; however, this study utilized a more selective criteria to define their population (70% of our total study population).23 We are confident that the key patterns of AUD medication prescribing among hepatology providers are captured at liver transplant centers who manage patients with ALD both in the transplant and nontransplant realms. We reached our target sample in this study, that is, providers managing patients with AUD, with >96% of respondents board-certified in transplant hepatology and/or GI and >90% practicing at university or university-affiliated centers, which accurately represents the nature of the transplant centers. There was an appropriate sex ratio and good distribution of age and years of experience. All 11 UNOS geographic regions were represented, enhancing external validity (ie, generalizability).
However, there were also some limitations that merit consideration. Overall transplant volume and response rates in respective UNOS regions were largely similar (Table 2). It is worth noting, however, that 1 region did account for a somewhat disproportionate response rate, compared with their transplant volume, which may have introduced some bias. Capturing respondents from non-transplant center-based hepatology practices and more community-based GI providers (inclusive of physician and advanced practice providers) would have been desirable in terms of a larger and broader sample. Widening the external validity would, however, come at the considerable cost of decreasing the internal validity as study population accountability and response rates would be extremely challenging to report reliably. In any case, it is conceivable that any training initiative introduced to hepatology providers at transplant centers, should be largely applicable to providers at nontransplant centers and in the community setting, as baseline medical knowledge is similar. Finally, there may also have been a response bias towards providers who are engaged in treating patients with AUD and providing them with medications to help them maintain abstinence. Therefore, the proportion of hepatology providers who support this practice may be somewhat lower in the real world. However, it is evident that there is still a strong core of hepatology providers who are willing to prescribe AUD medications. Studies with greater compensation for participation or staffing to provide outreach to nonresponders may help mitigate this concern in the future.
In summary, AUD medication prescribing is a common practice among hepatology providers who report an eagerness to increase this practice through more education and training. There are some knowledge deficiencies which are imminently addressable by relevant professional societies. Access to ancillary addiction services remains a pervasive limitation for hepatology providers, highlighting the need for hepatology providers to bridge the pharmacotherapeutic gap between availability and utilization of AUD pharmacotherapies while making concerted efforts to obtain concomitant behavioral therapy to optimize patient care. Increasing the practice of AUD medication use is expected to become even more crucial in the coming months, considering the anticipated surge in AUD and ALD instigated by the COVID-19 pandemic.24
ACKNOWLEDGMENTS
The authors would like to thank the staff at the University of Chicago Survey Lab for their contribution in the design and administration of the survey.
Supplementary Material
Footnotes
Published online 17 September, 2020.
Supplemental digital content (SDC) is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (www.transplantationdirect.com).
Supported by a grant from the Gastro-intestinal Research Foundation Associates’ Board, Chicago, IL.
A.C.K. has received grant/research support and consultant fees from Pfizer, Inc. K.G.R. has received grant/research support from Durect, Pilant, Gilead, Genfit, Intercept, and Target PharmaSolutions. M.C. has received grant/research support from Gilead, Conatus, and Galectin; consultant fees from Gilead, Metacrine, Enterome, Novartis, AbbVie, Intercept, and NGM Bio. T.G.C. and F.A. have no relevant disclosures.
T.G.C. involved in study concept and design; collection, analysis and interpretation of data; drafting and critical revision of the manuscript for important intellectual content; F.A., A.C.K., K.G.R., and MC involved in study design, critical revision of the manuscript for important intellectual content. All authors approved final version to be published.
REFERENCES
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 20135th ed, Washington, DC: American Psychiatric Association [Google Scholar]
- 2.Substance Abuse and Mental Health Services Administration (SAMHSA). National survey on drug use and health (NSDUH). 2016. 2016. Available at https://www.samhsa.gov/data/sites/default/files/NSDUH-FFR1-2016/NSDUH-FFR1-2016.htm. Accessed April 3, 2020 [PubMed]
- 3.Kim D, Li AA, Perumpail BJ, et al. Changing trends in etiology-based and ethnicity-based annual mortality rates of cirrhosis and hepatocellular carcinoma in the United States. Hepatology. 2019; 69:1064–1074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tapper EB, Parikh ND. Mortality due to cirrhosis and liver cancer in the United States, 1999-2016: observational study. BMJ. 2018; 362:k2817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cotter TG, Paul S, Sandikçi B, et al. Improved graft survival after liver transplantation for recipients with hepatitis C virus in the direct-acting antiviral era. Liver Transpl. 2019; 25:598–609 [DOI] [PubMed] [Google Scholar]
- 6.Cotter TG, Sandikçi B, Paul S, et al. Liver transplantation for alcoholic hepatitis in the US: excellent outcomes with profound temporal and geographic variation in frequency Am J Transplant. 2020. Jun 12. doi: 10.1111/ajt.16143. [Online ahead of print] [DOI] [PubMed] [Google Scholar]
- 7.Crabb DW, Im GY, Szabo G, et al. Diagnosis and treatment of alcohol-related liver diseases: 2019 practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2020; 71:306–333 [DOI] [PubMed] [Google Scholar]
- 8.Jonas DE, Amick HR, Feltner C, et al. Pharmacotherapy for adults with alcohol use disorders in outpatient settings: a systematic review and meta-analysis. JAMA. 2014; 311:1889–1900 [DOI] [PubMed] [Google Scholar]
- 9.2013 ACC/AHA cholesterol guideline and implications for healthy people 2020 cardiovascular disease prevention goals. J Am Heart Assoc. 2016; 5:e003558 doi: 10.1161/JAHA.116.003558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.de Bejczy A, Löf E, Walther L, et al. Varenicline for treatment of alcohol dependence: a randomized, placebo-controlled trial. Alcohol Clin Exp Res. 2015; 39:2189–2199 [DOI] [PubMed] [Google Scholar]
- 11.Johnson BA, Ait-Daoud N, Bowden CL, et al. Oral topiramate for treatment of alcohol dependence: a randomised controlled trial. Lancet. 2003; 361:1677–1685 [DOI] [PubMed] [Google Scholar]
- 12.Leggio L, Ferrulli A, Zambon A, et al. Baclofen promotes alcohol abstinence in alcohol dependent cirrhotic patients with hepatitis C virus (HCV) infection. Addict Behav. 2012; 37:561–564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yamini D, Lee SH, Avanesyan A, et al. Utilization of baclofen in maintenance of alcohol abstinence in patients with alcohol dependence and alcoholic hepatitis with or without cirrhosis. Alcohol Alcohol. 2014; 49:453–456 [DOI] [PubMed] [Google Scholar]
- 14.Addolorato G, Leggio L, Ferrulli A, et al. Effectiveness and safety of baclofen for maintenance of alcohol abstinence in alcohol-dependent patients with liver cirrhosis: randomised, double-blind controlled study. Lancet. 2007; 370:1915–1922 [DOI] [PubMed] [Google Scholar]
- 15.Klimas J, Fairgrieve C, Tobin H, et al. Psychosocial interventions to reduce alcohol consumption in concurrent problem alcohol and illicit drug users. Cochrane Database Syst Rev. 2018; 12:CD009269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Addolorato G, Mirijello A, Barrio P, et al. Reply to “Treatment of alcohol use disorders in patients with liver disease”. J Hepatol. 2016; 65:1271. [DOI] [PubMed] [Google Scholar]
- 17.Rogal S, Youk A, Zhang H, et al. Impact of alcohol use disorder treatment on clinical outcomes among patients with cirrhosis. Hepatology. 2020; 71:2080–2092. doi: 10.1002/hep.31042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.The President’s commission on combating drug addiction and the opioid crisis. 2017 doi: 10.1002/cpt.1050. Available at https://www.whitehouse.gov/sites/whitehouse.gov/files/images/Final_Report_Draft_11-1-2017.pdf. Accessed April 3, 2020. [DOI] [PubMed]
- 19.Organ Procurement and Transplantation (OPTN). National data. 2020. Available at https://optn.transplant.hrsa.gov/data/view-data-reports/national-data/. Accessed January 10, 2020
- 20.The American Association for Public Opinion Research Standard definitions: final dispositions of case codes and outcome rates for surveys. 20167th edAAPOR [Google Scholar]
- 21.Centers for Disease Control and Prevention (CDC). Behavioral risk factor surveillance system. Age-adjusted intensity of binge drinking among adults aged 18 years and older, by state, United States, 2015. 2015. Available at https://www.cdc.gov/alcohol/data-stats.htm. Accessed November 12, 2019
- 22.Couri T, Katz J, Stoeckle K, et al. Provider attitudes toward the use of hepatitis C virus-positive organs in kidney transplantation. Am J Nephrol. 2019; 50:168–176 [DOI] [PubMed] [Google Scholar]
- 23.Rich NE, Yang JD, Perumalswami PV, et al. Provider attitudes and practice patterns for direct-acting antiviral therapy for patients with hepatocellular carcinoma. Clin Gastroenterol Hepatol. 2020; 18:974–983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Da BL, Im GY, Schiano TD. COVID-19 hangover: a rising tide of alcohol use disorder and alcohol-associated liver disease. Hepatology. 2020. May 5. doi: 10.1002/hep.31307. [Online ahead of print] [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


