Abstract
Background:
Traumatic brain injury (TBI) induces major insult to the normal cerebral physiology. The anesthetic agents may infrequently produce deleterious effects and further aggravate damage to the injured brain. This study was conducted to evaluate the effects of propofol and sevoflurane on cerebral oxygenation, brain relaxation, systemic hemodynamic parameters and levels of interleukin-6 (IL-6) in patients with severe TBI undergoing decompressive craniectomy.
Methods:
A prospective randomized comparative study was conducted on 42 patients undergoing surgery for severe TBI. Patients were randomized into two groups, Group P received propofol and Group S received sevoflurane for maintenance of anesthesia. All patients were induced with fentanyl, propofol, and vecuronium. The effect of these agents on cerebral oxygenation was assessed by jugular venous oxygen saturation (SjVO2). Hemodynamic changes and quality of intraoperative brain relaxation were also assessed. The serum levels of IL-6 were quantitated using enzyme-linked immunosorbent assay technique.
Results:
SjVO2 values were comparable and mean arterial pressure (MAP) was found to be significantly lower in Group P as compared to those in Group S (P < 0.05). Brain relaxation scores were comparable between the groups. The level of IL-6 decreased significantly at the end of surgery compared to baseline in patients receiving sevoflurane (P = 0.040).
Conclusions:
Cerebral oxygenation measured by SjVO2 was comparable when anesthesia was maintained with propofol or sevoflurane. However, significant reduction in MAP by propofol needs attention in patients with severe TBI. The decrease in IL-6 level reflects anti-inflammatory effect and probable neuroprotective potential of propofol and sevoflurane.
Keywords: Jugular venous oxygenation, propofol, traumatic brain injury
Introduction
Traumatic brain injury (TBI) in the present day scenario is a major public health problem resulting in long-term disability and death especially in young adults. Primary injury or initial impact results in initiating an inflammatory cascade, edema formation, and excitotoxicity thus causing increase in intracranial pressure (ICP) and decrease in cerebral perfusion pressure (CPP).[1,2] Secondary systemic insults occurring thereafter in the form of hypoxia, hypotension, hypercarbia, hyperglycemia, hyperthermia, anemia, etc., are preventable.[3,4] Neuroanesthesiolgists are actively involved in resuscitation of TBI patients, thereby playing an imperative role in prevention secondary brain injuries and improving their overall outcome. The drugs used for induction and maintenance of anesthesia have a direct effect on cerebral blood flow (CBF), cerebral metabolic requirement of oxygen (CMRO2), ICP, and CPP.[5] Jugular venous oxygen saturation (SjVO2) is an indirect assessment of cerebral oxygenation, which reflects the global cerebral balance between cerebral oxygen demand and supply.[6,7] It provides an early diagnosis of ischemia resulting from either intracranial or systemic causes. The anesthetic agents can provide neuroprotection by maintaining an adequate balance between cerebral oxygen demand and supply. Various inhalational anesthetic agents have demonstrated promising results as cerebral protectants through their preconditioning effect in animal models.[8] The superiority of one anesthetic agent over the other has yet not been established despite the difference in their neurophysiological properties due to lack of substantial evidence favoring one over the other. Sevoflurane and propofol are both being increasingly used in neurosurgery due to their property of rapid onset and emergence from anesthesia aiding in early assessment of neurosurgical status following surgery. However, the intravenous anesthetic agents maintain the CBF-metabolism coupling as against the inhalational counterparts which disrupt it at higher maximum additive concentration (MAC) values and thus increase cerebral blood volume and thereby, ICP, which may prove detrimental to the already compromised brain function.[9] Thus, intravenous anesthetic agents are given a preference over inhalational anesthetics to provide adequate brain relaxation by reducing intracranial blood volume in moderate-to-severe TBI. Sevoflurane may prove to be equally beneficial in maintaining cerebral oxygenation and hemodynamics compared to propofol in TBI patients and may have an additional advantage of providing neuroprotection by virtue of its preconditioning effects.
Interleukin-6 (IL-6) is a pro-inflammatory cytokine that is sensitive for brain injury and can be easily detected in serum.[10] The anesthetic agents may have anti-inflammatory properties and consequently neuroprotective effects which can influence the serum IL-6 levels.
Our primary aim was to compare the effects of sevoflurane and propofol on cerebral oxygenation measured using jugular venous oximetry. Secondary aims were to determine the effect of these drugs on intraoperative heart-rate, blood pressure, brain relaxation score, and attenuation of cerebral inflammatory response by analyzing IL-6 in moderate-to-severe TBI patients undergoing decompressive craniectomy.
Methods
This prospective, randomized, double-blind study was conducted after approval from Institution Ethics Committee and registration with the clinical trial registry of India (Regn. no-CTRI/2018/02/012139). Written informed consent was obtained from participants' relatives and all the procedures were performed in accordance with the Helsinki declaration. The CONSORT recommendations for reporting randomized trials were followed [Figure 1].
Figure 1.
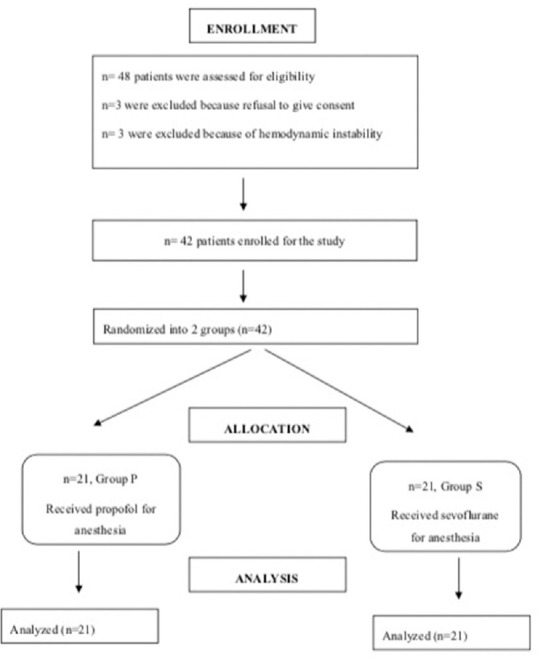
Consort diagram
We enrolled 42 American Society of Anesthesiologists physical status IE-IIE patients aged 18–60 years with severe head injury who underwent decompressive hemicraniectomy. Patients with mild-to-moderate head injury (Glasgow Coma Scale >8), patients in shock (systolic blood pressure [SBP] <90 mm of Hg) even after resuscitation, any comorbidity other than hypertension or diabetes (i.e., coronary artery disease, chronic obstructive pulmonary disease, hepatic, or renal impairment) were excluded. Randomization was done using computer-generated random numbers table and patients were divided equally into two groups - Group P received propofol and Group S received sevoflurane for maintenance of anesthesia.
Each patient underwent preanesthetic check-up prior to shifting the patient inside the operation theatre. Preinduction monitoring included electrocardiography, noninvasive blood pressure, entropy, neuromuscular transmission, pulse oximetry (SpO2), and invasive blood pressure using 20 G intra-arterial catheter in radial artery. Patients were induced with fentanyl 2 μg/kg and propofol 1–2 mg/kg administered in titrated doses. Vecuronium (0.1 mg/kg) was used for tracheal intubation and lignocaine 1.5 mg/kg was administered around 90 s prior to laryngoscopy to prevent intubation response. All patients were administered a continuous infusion of fentanyl at the rate of 1 μg/kg/h for intraoperative analgesia. After intubation, both the groups were mechanically ventilated with oxygen-air mixtures (50:50) and an I/E ratio of 1:2. The tidal volume was set to 6–8 ml/kg and the respiratory rate was adjusted to maintain a PaCO2 (partial pressure of carbon dioxide in arterial blood) value between 32 and 35 mm Hg. Anesthesia was maintained by continuous infusion of propofol 75–150 μg/kg/h in Group P and with sevoflurane 0.8–1 MAC in Group S to titrate the entropy values between 40 and 60.
For jugular bulb oximetry, a 5 Fr, 15 cm long central venous catheter was inserted in the side of predominant injury or right internal jugular vein in case of diffuse axonal injury requiring decompression along the retrograde direction toward the jugular bulb by Seldinger's technique. The length of insertion was estimated from the point of insertion to the mastoid prominence or till the resistance was felt near the mastoid at which point the catheter was pulled back by 1 cm. Confirmation of correct placement was done using C-arm by lateral neck radiography to position the tip of the catheter between C1 and C2 vertebra. The blood samples were withdrawn slowly at a rate not more than 2 mlmin-1. Sampling of jugular bulb blood was done three times, and the values were recorded to find any episodes of desaturation (<50%) or hyperemia (>75%). Baseline SjVO2 values were recorded just after insertion of catheter into the jugular bulb. Arterial and jugular bulb blood samples were withdrawn simultaneously after catheter insertion (baseline value), at the end of surgery, and 12 h after completion of surgery.
The muscle relaxation was achieved with intermittent boluses of vecuronium (0.01mg/kg) in intraoperative period to maintain a train of four count <2. The packed red blood cells were administered in case the hematocrit readings were below 30. All patients received mannitol (0.5 g/kg), phenytoin (5mg/kg), and antibiotics as per the institutional protocol.
The hemodynamic parameters (heart rate [HR], SBP, diastolic blood pressure, and mean arterial pressure [MAP]) were recorded prior to induction of anesthesia as baseline values, intraoperatively at every 10 min interval till the end of surgery and 12 h after completion of surgery. The MAP was kept above 65 mm of Hg. In case of hypotension (MAP <65 mm Hg), crystalloid fluid bolus of 3–5 ml/kg was given initially followed by boluses of intravenous mephentermine 3 mg or phenylephrine (50–100 μg). If MAP persisted at <65 mm of Hg for more than 5 min, an infusion of nor-adrenaline was started at the rate of 0.05–0.1 μg/kg/min. In case of hypertension (MAP >110 mmHg), intravenous 2–3 esmolol boluses (0.3–0.5 mg/kg) were administered. In case of any bradycardia of <50/min, intravenous atropine (0.5 mg) was administered. All rescue drugs used to maintain hemodynamic were recorded and urinary bladder was catheterized in all the patients to monitor intraoperative urine output.
Interleukin-6 assay
The blood samples for IL-6 were taken twice, one sample before induction of anesthesia which was considered the baseline value and other two, at the end of surgery. Levels of IL-6 were measured in duplicate in plasma by enzyme-linked immunosorbent assay method. A volume of 3–5 ml of blood sample was taken and centrifuged to obtain an adequate amount of serum which was then stored at −20°C–−40°C and was analyzed in duplicate by TECAN (Infinite M200 pro, 2014) analyzer.
The surgery was conducted by an experienced neurosurgeon (>2 year experience in neurosurgery) who was blinded to the agent used for maintenance of anesthesia and were asked to assess and grade the brain relaxation after the elevation of bone flap using a four-point grade.[11] Grade I - excellent with no brain swelling, Grade II - minimal but acceptable brain swelling, Grade III - moderate brain swelling but no specific change required in management, and Grade IV - severe brain swelling requiring some intervention such as change in position, a further reduction in PaCO2, additional dose of mannitol and/or furosemide.
Fentanyl infusion was stopped at the beginning of skin closure whereas the maintenance agents were stopped following completion of skin closure. None of the patients were extubated at the end of surgery and were shifted to neurosurgical intensive care unit.
Statistical analysis
The sample size of total 42 patients (21 in each group) was calculated on the basis of a previous study,[12] taking an alpha error of 0.05% at 80% power and considering SjVO2 values <50% as significant cerebral hypoperfusion. Statistical analysis was carried out using statistical package for social sciences (SPSS Inc., Chicago, IL, USA, version 21.0). The continuous data were presented as mean ± standard deviation for normally distributed data; two groups were compared using Student's t-test. Categorical and nominal data were described as proportions and Chi-square test or Fischer's exact test was used to look at significant associations. Paired sample t-test was also used for baseline comparisons. A P < 0.05 was considered statistically significant.
Results
A total of 48 patients were assessed for decompressive hemicraniectomy for severe TBI. Six patients were excluded due to refusal of consent and hemodynamic instability. A total of 42 patients were finally analyzed [Figure 1].
Demographic data and other characteristics were comparable in both the groups [Table 1].
Table 1.
Comparison of demographic data (n=21)
| Parameters | Group P | Group S | P |
|---|---|---|---|
| Age (years) | 39.29±9.809 | 36.71±13.138 | 0.477 |
| Weight (kg) | 70.00±6.301 | 68.57±4.986 | 0.420 |
| Sex (male/female)# | 18/3 | 16/5 | 0.348 |
| ASA status (I/II)# | 18/3 | 18/3 | 1.000 |
| Duration of surgery (min) | 107.14±14.280 | 113.57±16.594 | 0.186 |
| Duration of anesthesia (min) | 135.71±13.990 | 140.95±17.001 | 0.282 |
Values expressed as mean±SD; #Presented as number. SD – Standard deviation; ASA – American Society of Anesthesiologists
The neurological diagnosis of patients is described in Table 2.
Table 2.
Type of traumatic brain injury (n=21)
| Diagnosis | Group P, n (%) | Group S, n (%) | P |
|---|---|---|---|
| Acute SDH | 7 (33.33) | 6 (28.57) | 0.896 |
| Acute SDH with contusion | 11 (52.38) | 11 (52.38) | |
| Cerebral contusions | 3 (14.28) | 4 (19.05) |
Values expressed as numbers (%). SDH – Sub dural haemorrhage
Values of SjVO2 were comparable between Group P and Group S at baseline, end of surgery, and at 12 h after surgery [Table 3].
Table 3.
Intergroup comparison of jugular venous oxygen saturation (n=21) (%)
| Time period | Group P | Group S | P |
|---|---|---|---|
| Postinduction | 73.67±14.14 | 76.84±8.41 | 0.382 |
| End of surgery | 76.53±14.37 | 75.68±9.49 | 0.822 |
| 12 h after surgery | 74.54±8.21 | 74.72±5.84 | 0.937 |
Values expressed as mean±SD. SD – Standard deviation
HR was recorded prior to induction as well at various intervals intraoperatively. The baseline (pre-induction) HR was comparable in both the groups (P = 0.867). The difference in HR was not found statistically significant at any point of time and was comparable in both the groups [Figure 2].
Figure 2.
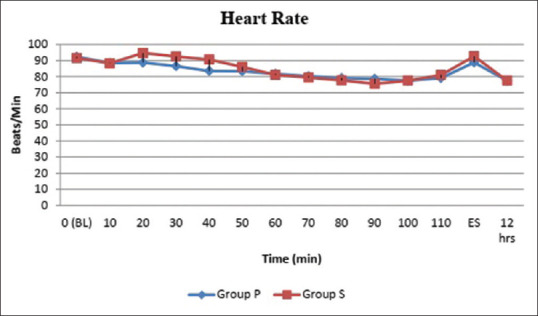
Comparison of intraoperative heart rate among the two groups
Baseline values of MAP were comparable in both the groups (P = 0.569), but after the start of surgery, there was a significant difference (P < 0.05) in MAP at various time intervals intraoperatively, end of surgery and even after 12 h of surgery. This shows that MAP was on lower range in Group P as compared to Group S [Figure 3]. A statistically significant difference was found with mean IV fluid infused - 2800 ml in Group P and 2385.71 ml of fluid in Group S (P < 0.001). More intravenous fluid requirement was seen in Group P as compared to Group S to maintain hemodynamics.
Figure 3.
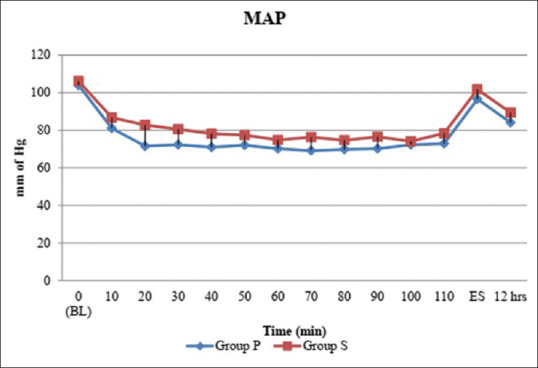
Comparison of intraoperative mean bp among the two groups
The total urine output was compared in both groups and a statistically significant difference was found with total urine output values of 1352.38 ml in Group P and 1166.66 ml of fluid in Group S (P < 0.001) [Table 4].
Table 4.
Comparison of intravenous fluids and urine output (n=21)
| Parameter | Group P | Group S | P |
|---|---|---|---|
| Total fluid (ml) | 2800±158.11 | 2385.71±159.01 | <0.001* |
| Total urine output (ml) | 1352.38±103.05 | 1166.66±127.80 | <0.001* |
*P<0.001 (highly significant)-for both the variables.
The brain relaxation was assessed by the operating surgeon who was blinded to the randomization of groups before opening of dura and was noted using four-point grades. most patients had a brain relaxation score of Grade-II in both the groups, none of the patients had Grade-IV brain relaxation score. No statistical difference in brain relaxation was noted between the groups (P = 0.626) [Figure 4].
Figure 4.
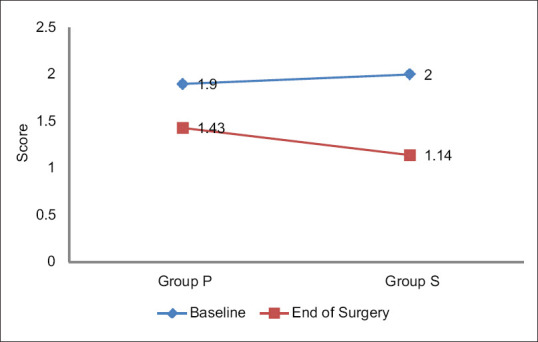
Brain relaxation score comparison between the two groups
The values of IL-6 were compared within the groups and between the groups. Both the baseline IL-6 levels and IL-6 levels at end of surgery were comparable between the two groups. A significant difference was found between the baseline value and value at the end of surgery in Group S (P = 0.040) [Table 5].
Table 5.
Intergroup comparison of interleukin-6 Levels (in pg/ml) (n=21)
| Time period | Group P | Group S | P |
|---|---|---|---|
| Baseline | 105.19±73.99 | 96.05±64.96 | 0.673 |
| End of surgery | 98.91±63.97 | 78.42±57.41 | 0.338 |
Values expressed as mean±SD. SD – Standard deviation
Discussion
Administering general anesthesia to the patients with moderate-to-severe head injury is a challenge as these patients commonly have hemodynamic instability, neurological complications as well as respiratory compromise. Resuscitation, prevention of further damage to brain cells and providing neuroprotection are the goals of neuroanesthesia in these patients posted for decompressive craniectomy. Optimal neuroprotective strategies include appropriate patient positioning, management of systemic as well as cerebral hemodynamics.[13] Anesthetic agents may provide neuroprotection by keeping a balance between cerebral oxygen demand and supply.
In the study, SjVO2 was comparable in patients receiving either propofol or sevoflurane at baseline value or at the end of surgery and 12 h after surgery. In patients receiving propofol SjVO2 values were a little on higher side compared to those receiving sevoflurane, though the difference was not statistically significant. Higher SjVO2 may be due to decrease in CMRO2 by propofol. The values were similar at 12 h after surgery to that of baseline values suggesting that both propofol and sevoflurane are short acting agents and effects do not last longer.
However, SjVO2 as a marker of cerebral oxygenation has its drawbacks. SjVO2 is a global oxygenation parameter, which cannot detect regional ischemia. SjVO2 monitoring has a high specificity but low sensitivity for the detection of regional ischemia. In other words, a normal SjVO2 does not guarantee against regional ischemia but a low SjVO2 is a definitive indicator of global ischemia and/or focal ischemia.[14] Nevertheless, we must emphasize that a low SjVO2 not always equates with cerebral anoxia, but can indicate an increase in oxygen extraction, which may be an early warning sign of possible ischemia. In this study, none of the SjVO2 values were less than lower normal limit (<50%).
Intravenous agents are considered to produce more brain relaxation compared to inhalational anesthetic agents. In our study, brain relaxation was assessed by the blinded experienced neurosurgeon not involved in study, after elevation of bone flap, using brain relaxation grades of I to IV and it was observed that the degree of brain relaxation was comparable in the two groups. Chui et al., in the meta-analysis and systematic review compared intravenous with inhalational agents in 1819 patients and observed that sevoflurane is as good a maintenance agent as propofol to maintain brain relaxation at <1MAC and controlled ventilation.[15]
Hypotension is one of the major causes of secondary brain injury and poor outcome in patients with TBI. In our study, the MAP in Group P was found to be comparable to Group S (P = 0.569) at the start of surgery. After induction of anesthesia, there was fall in MAP significantly in Group P compared to Group S throughout the surgery. This decrease in MAP may be attributed to decrease in systemic vascular resistance caused by propofol. In contrary to our observation, Sneyd et al. observed increased number of hypotensive episodes in sevoflurane group compared to propofol.[16] They justified their findings by demonstrating greater depth of anesthesia in sevoflurane group as compared to propofol group. In our study, the depth of anesthesia was maintained by titrating the doses of anesthetic agent's propofol and sevoflurane at an entropy value of 40–60. The end tidal carbon dioxide, temperature, and fraction of inspired oxygen were similar in both the groups.
The total intravenous fluid used was significantly higher in propofol group than sevoflurane group (P < 0.001) which might be explained by increased fluid requirement to maintain MAP values in the normal range in the group receiving propofol.
IL-6 is a pro-inflammatory biomarker and in our study, we estimated the levels of IL-6 in serum observing that the values were comparable between both the groups. Intragroup comparison revealed that the levels of IL-6 decreased significantly in the sevoflurane group at the end of surgery compared to the baseline (P = 0.040). This may be explained by the anti-inflammatory effects of sevoflurane which might demonstrate a beneficial neuroprotective effect in patients with TBI. A similar beneficial effect of sevoflurane was also demonstrated in the study by Potočnik et al. where the authors observed decreased levels of IL-6 with sevoflurane compared to propofol in patients undergoing one lung ventilation for lung surgery, thus predicting its anti-inflammatory role.[17] Markovic-Bozic et al. studied effect of propofol and sevoflurane on the inflammatory response of patients undergoing craniotomy.[18] They found that neither propofol nor sevoflurane had any significant impact on the occurrence of postoperative complications and suggested to incite future studies to prove a potential medically important anti-inflammatory role of propofol in neuroanesthesia.
Limitations
We did not measure SjVO2 continuously, and hence, we could have missed a few desaturation or hyperemic episodes during the intraoperative period which could have better elucidated the effects of intravenous or inhalational agents as real-time monitor, which would have aided in an earlier prevention of secondary brain insults. And second, we did not follow-up these patients to assess their long-term outcomes in relation to the secondary insults, that they might have had during perioperative period and hospital stay. Furthermore, we did not assess their long-term outcome in terms of cognitive dysfunctions, neurological morbidity and mortality to evaluate neuroprotective potential of propofol or sevoflurane.
Conclusions
The effects of propofol and sevoflurane used for maintenance of anesthesia are similar in regards to cerebral oxygenation as measured by jugular venous oximetry and brain relaxation scores. Significant reduction in MAP by propofol needs a caution in the intraoperative period for its judicious and careful use. Hypotension should be prevented at all costs as it might be detrimental to the overall outcome of these patients. Decrease in level of IL-6 at the end of surgery compared to baseline values may suggest a neuroprotective potential of sevoflurane which needs to explore further by larger randomized controlled studies on patients with severe TBI.
Financial support and sponsorship
This study was supported by PGIMER, Chandigarh.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Greve MW, Zink BJ. Pathophysiology of traumatic brain injury. Mt Sinai J Med. 2009;76:97–104. doi: 10.1002/msj.20104. [DOI] [PubMed] [Google Scholar]
- 2.Werner C, Engelhard K. Pathophysiology of traumatic brain injury. Br J Anaesth. 2007;99:4–9. doi: 10.1093/bja/aem131. [DOI] [PubMed] [Google Scholar]
- 3.Chesnut RM. Secondary brain insults after head injury: Clinical perspectives. New Horiz. 1995;3:366–75. [PubMed] [Google Scholar]
- 4.Unterberg AW, Stover JF, Kress B, Kiening KL. Edema and brain trauma. Neuroscience. 2004;129:1021–9. doi: 10.1016/j.neuroscience.2004.06.046. [DOI] [PubMed] [Google Scholar]
- 5.Tameem A, Krovvidi H. Cerebral physiology. Contin Educ Anaesth Crit Care Pain. 2013;13:113–118. [Google Scholar]
- 6.Feldman Z, Robertson CS. Monitoring of cerebral hemodynamics with jugular bulb catheters. Crit Care Clin. 1997;13:51–77. doi: 10.1016/s0749-0704(05)70296-7. [DOI] [PubMed] [Google Scholar]
- 7.De Deyne C, Van Aken J, Decruyenaere J, Struys M, Colardyn F. Jugular bulb oximetry: Review on a cerebral monitoring technique. Acta Anaesthesiol Belg. 1998;49:21–31. [PubMed] [Google Scholar]
- 8.Bhuiyan MI, Kim YJ. Mechanisms and prospects of ischemic tolerance induced by cerebral preconditioning. Int Neurourol J. 2010;14:203–12. doi: 10.5213/inj.2010.14.4.203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bazin JE. Effects of anesthetic agents on intracranial pressure. Ann Fr Anesth Reanim. 1997;16:445–52. doi: 10.1016/s0750-7658(97)81477-3. [DOI] [PubMed] [Google Scholar]
- 10.Woiciechowsky C, Schöning B, Cobanov J, Lanksch WR, Volk HD, Döcke WD. Early IL-6 plasma concentrations correlate with severity of brain injury and pneumonia in brain-injured patients. J Trauma. 2002;52:339–45. doi: 10.1097/00005373-200202000-00021. [DOI] [PubMed] [Google Scholar]
- 11.Todd MM, Warner DS, Sokoll MD, Maktabi MA, Hindman BJ, Scamman FL, et al. A prospective, comparative trial of three anesthetics for elective supratentorial craniotomy.Propofol/fentanyl, isoflurane/nitrous oxide, and fentanyl/nitrous oxide. Anesthesiology. 1993;78:1005–20. doi: 10.1097/00000542-199306000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Muñoz HR, Núñez GE, de la Fuente JE, Campos MG. The effect of nitrous oxide on jugular bulb oxygen saturation during remifentanil plus target-controlled infusion propofol or sevoflurane in patients with brain tumors. Anesth Analg. 2002;94:389–92. doi: 10.1097/00000539-200202000-00030. [DOI] [PubMed] [Google Scholar]
- 13.El Beheiry H. Protecting the brain during neurosurgical procedures: Strategies that can work. Curr Opin Anaesthesiol. 2012;25:548–55. doi: 10.1097/ACO.0b013e3283579622. [DOI] [PubMed] [Google Scholar]
- 14.De Georgia MA, Deogaonkar A. Multimodal monitoring in the neurological intensive care unit. Neurologist. 2005;11:45–54. doi: 10.1097/01.nrl.0000149993.99956.09. [DOI] [PubMed] [Google Scholar]
- 15.Chui J, Mariappan R, Mehta J, Manninen P, Venkatraghavan L. Comparison of propofol and volatile agents for maintenance of anesthesia during elective craniotomy procedures: Systematic review and meta-analysis. Can J Anaesth. 2014;61:347–56. doi: 10.1007/s12630-014-0118-9. [DOI] [PubMed] [Google Scholar]
- 16.Sneyd JR, Andrews CJ, Tsubokawa T. Comparison of propofol/remifentanil and sevoflurane/remifentanil for maintenance of anaesthesia for elective intracranial surgery. Br J Anaesth. 2005;94:778–83. doi: 10.1093/bja/aei141. [DOI] [PubMed] [Google Scholar]
- 17.Potočnik I, Novak Janković V, Šostarič M, Jerin A, Štupnik T, Skitek M, et al. Antiinflammatory effect of sevoflurane in open lung surgery with one-lung ventilation. Croat Med J. 2014;55:628–37. doi: 10.3325/cmj.2014.55.628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Markovic-Bozic J, Karpe B, Potocnik I, Jerin A, Vranic A, Novak-Jankovic V. Effect of propofol and sevoflurane on the inflammatory response of patients undergoing craniotomy. BMC Anesthesiol. 2016;16:18. doi: 10.1186/s12871-016-0182-5. [DOI] [PMC free article] [PubMed] [Google Scholar]


