Abstract
Osteomas of the paranasal sinuses rarely lead to intracranial manifestations. We present an unusual case of a giant frontal sinus osteoma leading to subdural empyema formation. Determine the origin and the optimal surgical approach of these unusual lesions by analyzing giant osteomas of the frontal and ethmoidal sinuses in the literature. We report a rare case of giant frontoethmoidal osteoma with intracranial extension in a 34-year-old man, revealed by seizures. Neuroradiological studies revealed frontoparietal subdural empyema associated to a large osteoma in the right frontal sinus. The patient underwent surgical evacuation of the empyema and resection of the osteoma in one stage operation of decompressive craniotomy. The patient recovered very well after surgery and postoperative antibiotic therapy. This case represents in the literature only the third-reported case of subdural empyema complicating frontoethmoidal osteoma. The surgical treatment options, including open surgery techniques and endoscopic approaches, as well as pathogenesis are discussed according to the relevant literature.
Keywords: Fronto-ethmoidal, giant, osteoma, subdural empyema, surgery
Introduction
Frontoethmoidal osteomas represent slow-growing benign tumors with potentially serious complications. They are rare with an incidence of 0.43% in the general population.[1] These encapsulated bony tumors are most commonly asymptomatic or may remain silent without causing neurological deficit, and are detected incidentally in 3% of computed tomography (CT) scans and 1% of plain sinus radiographs.[2] However, depending on their size and location, they may become symptomatic due to direct mass effect or erosion of the posterior sinus wall.[3] Thus, surgery is necessary as the main treatment option for symptomatic frontal osteomas and intracranial complication.
We conducted a focused literature review of PubMed and MEDLINE databases for similar contemporary cases of osteoma, restricting our focus to frontal sinus osteomas complicating subdural empyema requiring surgical management. To the best of our knowledge, only two cases of frontal osteoma complicated by subdural empyema have been reported in the literature.[4,5] Through this observation and the review of the literature, we aim to discuss the etiology of intracranial infection, complicating sinusal osteomas, their pathogenesis, and the treatment strategy.
Case Report
A 34-year-old man presented with a prolonged history of progressive right frontal bony swelling, headaches, and new-onset seizure. The patient denied any history of fever, chills, or nasal liquorrhea. On physical examination, he was afebrile, alert, and oriented without focal neurologic deficit. Initial CT scan demonstrated a large bony lesion of the right frontal bone, growing inside the right frontal sinus, breaking the posterior wall of the sinus cavity and compressing the frontal lobe. The osseous lesion was associated to right frontobasal pneumocephalus. The CT scan patterns suggested a giant fronto-ethmoidal osteoma [Figure 1]. Subsequently, the patient was advised that the lesion was most likely present from birth, and given the lesion's apparent growth and risk of further seizures, surgical resection was recommended. During a prolonged hospitalization, the patient presented a progressive left hemiparesis 4/5 strength, with 38.5°C of fever, and he complained aggravation of headache. Brain magnetic resonance imaging (MRI) was performed in emergency and revealed a right fronto-parietal subdural empyema causing a noticeable mass effect to the midline structures. It demonstrated also the known giant right fronto-ethmoidal osteoma [Figure 2]. Because of the presence of subdural empyema, surgery was performed in emergency.
Figure 1.
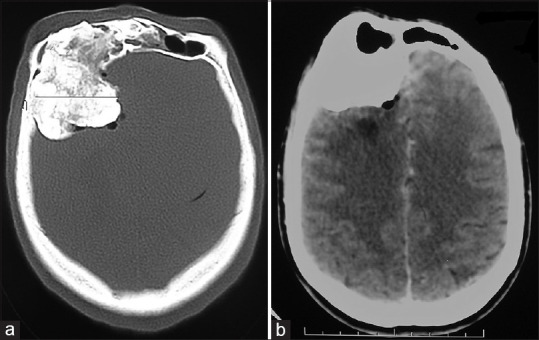
Axial cerebral computed tomography scan (in bony and parenchymal windows) showing a large right fronto-ethmoidal osseous lesion (a), compressing the frontal lobe with pneumocephalus (b)
Figure 2.
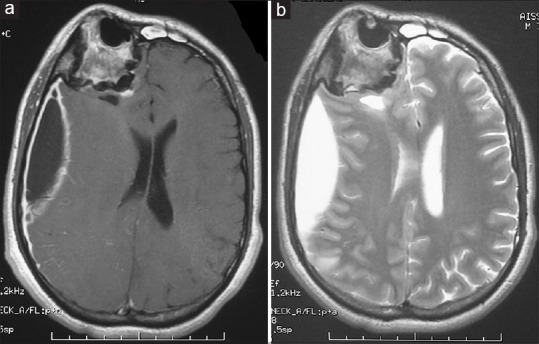
Axial brain magnetic resonance imaging weighted T1 with gadolinium (a) and weighted T2 (b), demonstrating a right frontoparietal compressive subdural empyema associated to giant right fronto-ethmoidal osteoma
Operation
The patient underwent right decompressive fronto-parietal craniotomy, with en bloc resection of the fronto-ethmoidal osteoma which was sent for frozen and permanent pathology [Figure 3]. At operation, it was noted that the bony tumor had eroded the posterior wall of the frontal sinus and the basal dura, with extension into the frontal brain parenchyma. The right frontal sinus cavity was fully cranialized by resecting all remaining respiratory mucosa, and the residual sinus cavity was packed with a pedunculated periosteal flap. The dura mater in contact with the osteoma was expanded and thin harboring a large dural defect behind surrounding inflammatory changes, and adhered closely to the brain surface. After dural incision, meticulous removal of yellowish pus with irrigation was done. The dural defect was then reconstructed with an autologous periosteal flap and fibrin glue.
Figure 3.
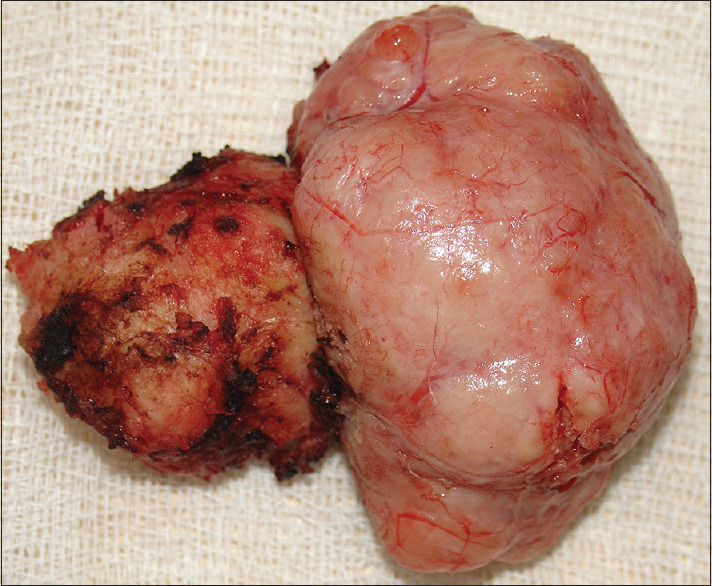
Intraoperative picture of the giant osteoma totally resected
Postoperative course
Surgical pathology revealed bony tumor consistent with mixed osteoma, cortical, and cancellous type [Figure 4]. In addition, the bacteriological examination and culture of pus were negative. Thereby, the patient received intravenous antibiotics ceftriaxone (200 mg/Kg/day) and metronidazole (1.5 g/day) for 3 weeks associated to antiepileptic treatment. His neurological status improved to baseline after the surgery, and the patient experienced no postoperative complications with total recovery at 2 months postoperatively. At the last follow-up, the patient is doing well but had epilepsy well equilibrated by 400 mg of carbamazepin well taken three times daily.
Figure 4.
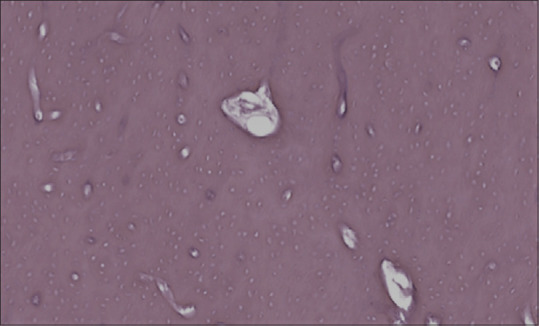
Histologic features of osteoma: higher-power view with compact cortical bone with Haversian-like systems evident, consistent with mixed osteoma, cortical and cancellous type
Discussion
Epidemiology, clinical symptoms, and histology
Giant osteomas are uncommon slow-growing tumors, defined as being larger than 3 cm, with an overall growth rate estimated at 1.84 mm2 per year.[6,7] Ocular and neurological symptoms result from the proliferation of osteomas located in the frontoethmoidal region and causing exophthalmia, dacryorrhea, even lead to intracranial complications such as meningitis, pneumocephalus, mucocele, cerebral abscess, or subdural empyema.[3,8,9,10,11]
The etiology of osteomas still remains unclear. Indeed, three theories have been suggested as cause of osteomas; infectious, traumatic, and genetic.[12] Osteomas occur more commonly in men with a male-to-female ratio of 2,[8] and a peak incidence in the 4th to 6th decades of life.[1] This greater prevalence of osteomas in men is attributed to the larger size of their sinuses and more frequent exposure to injuries. Histologically, four acknowledged pathological types of osteomas have been described: the ivory osteoma dense and mature bone; the compact osteoma with small Haversian canals, the osteoma spongiosum; and finally the mixed osteoma.[2]
Pathogenesis
The pathogenesis of subdural empyema associated to osteoma is unclear. However, some authors have proposed the role of osteoma in the development of intracranial infection.[4,5] In fact, a giant osteoma may progress to trigger bone crack in the posterior wall of the sinus concomitantly with traumatism, leading thus to meningeal erosion. Although rarely reported, the tumor may also grow gradually intradurally with dural defect, resulting in a fistula between the sinuses and the intracranial compartment.[10] In up to 50% of cases, osteomas are associated with the secondary growth of mucoceles because they can cause chronic obstruction of outlet ostia.[13] The intracranial rupture of these mucoceles through bony and dural defect can lead to severe complications such as meningitis, cerebrospinal fluid fistula, seizures, abscesses, and subdural empyema. Another suggestion is that the cranial infection may occur directly or indirectly, via the venous system giving rise to a life-threatening evolution of this benign entity. In our case, we believe that the occurrence of subdural empyema was caused by the break of the posterior wall of the sinus generated by the huge volume of the osteoma. The illustrative CT scan and MRI of our patient are supporting our hypothesis.
Surgery
Many authors agreed with the “wait-and-see policy” for asymptomatic osteomas, small sized or those discovered accidently. Nevertheless, surgery is recommended for significant tumor growth associated to the appearance of clinical symptoms or in cases of orbital involvement and/or intracranial extension.[12] Depending on the location and extension of the tumor, open surgery techniques as well as endoscopic transnasal approaches might be considered. Conversely, the surgical method seems to be independent of the osteoma size thereby, the decision is rather based on the past surgeon's experience and operator skill, knowledge of different surgical techniques and available equipment.[2,14] In case of giant frontal osteomas or associated with intracranial extensions, as reported in our case, the transfrontal approach is safer, more effective, and remains the standard treatment.[15] However, endoscopy can be considered for all fronto ethmoidal neoplasms with median localization.[16,17] Some authors suggest that combined surgical treatment associating endoscopy and open surgery in one stage allowing the frontal sinus obliteration followed by osteoma and empyema removal through craniotomy may be a good treatment strategy.[4,18] Matter of course, postoperative antibiotics therapy for sufficient period has to follow surgical intervention.
Conclusion
Although osteomas are usually considered as benign slow-growing lesions, they may cause neurological and/or ophthalmological complications whenever they reach sizeable volume. Subdural empyema should be taken in mind in a giant fronto ethmoidal osteoma presented with seizure and neurological deficit. We emphasize the importance of early operative management of giant osteoma before endocranial complications.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Ishii T, Sakamoto Y, Miwa T, Yoshida K, Kishi K. A giant osteoma of the ethmoid sinus. J Craniofac Surg. 2018;29:661–2. doi: 10.1097/SCS.0000000000004206. [DOI] [PubMed] [Google Scholar]
- 2.Humeniuk-Arasiewicz M, Stryjewska-Makuch G, Janik MA, Kolebacz B. Giant fronto-ethmoidal osteoma – Selection of an optimal surgical procedure. Braz J Otorhinolaryngol. 2018;84:232–9. doi: 10.1016/j.bjorl.2017.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Umredkar AB, Disawal A, Anand A, Gaur P. Frontal sinus osteoma with pneumocephalus: A rare cause of progressive hemiparesis. Indian J Radiol Imaging. 2017;27:46–8. doi: 10.4103/0971-3026.202972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cho SY, Kim JW, Kim CY. Osteoma of the frontal sinus with secondary subdural empyema formation. J Korean Neurosurg Soc. 2006;40:202–5. [Google Scholar]
- 5.Semmler M, Keck T. Osteoma of the frontal sinus leading to acute sinusitis with the complication of subdural empyema. Laryngorhinootologie. 2007;86:794–7. doi: 10.1055/s-2007-966519. [DOI] [PubMed] [Google Scholar]
- 6.Halawi AM, Maley JE, Robinson RA, Swenson C, Graham SM. Craniofacial osteoma: Clinical presentation and patterns of growth. Am J Rhinol Allergy. 2013;27:128–33. doi: 10.2500/ajra.2013.27.3840. [DOI] [PubMed] [Google Scholar]
- 7.Kolcun JPG, Richardson AM, Gernsback JE, Rosenberg A, Komotar RJ. Frontal sinus osteoma presenting with meningitis and epilepsy. World Neurosurg. 2019;123:216–20. doi: 10.1016/j.wneu.2018.12.031. [DOI] [PubMed] [Google Scholar]
- 8.Dominguez IB, Alvarez AV, Gonzalez LM, Garcia-Rubio BM, Iglesias GF, Garcia JR. Fron-toethmoidal osteoma with orbital extension. A case report. Arch Soc Esp Oftalmol. 2016;91:349–52. doi: 10.1016/j.oftal.2016.01.025. [DOI] [PubMed] [Google Scholar]
- 9.Kamide T, Nakada M, Hayashi Y, Hayashi Y, Uchiyama N, Hamada J. Intraparenchymal pneumocephalus caused by ethmoid sinus osteoma. J Clin Neurosci. 2009;16:1487–9. doi: 10.1016/j.jocn.2009.01.016. [DOI] [PubMed] [Google Scholar]
- 10.Summers LE, Mascott CR, Tompkins JR, Richardson DE. Frontal sinus osteoma associated with cerebral abscess formation: A case report. Surg Neurol. 2001;55:235–9. doi: 10.1016/s0090-3019(01)00344-5. [DOI] [PubMed] [Google Scholar]
- 11.Nabeshima K, Marutsuka K, Shimao Y, Uehara H, Kodama T. Osteoma of the frontal sinus complicated by intracranial mucocele. Pathol Int. 2003;53:227–30. doi: 10.1046/j.1320-5463.2003.01459.x. [DOI] [PubMed] [Google Scholar]
- 12.Mansour AM, Salti H, Uwaydat S, Dakroub R, Bashshour Z. Ethmoid sinus osteoma presenting as epiphora and orbital cellulitis: Case report and literature review. Surv Ophthalmol. 1999;43:413–26. doi: 10.1016/s0039-6257(99)00004-1. [DOI] [PubMed] [Google Scholar]
- 13.Manaka H, Tokoro K, Sakata K, Ono A, Yamamoto I. Intradural extension of mucocele complicating frontoethmoid sinus osteoma: Case report. Surg Neurol. 1998;50:453–6. doi: 10.1016/s0090-3019(97)00162-6. [DOI] [PubMed] [Google Scholar]
- 14.Karunaratne YG, Gunaratne DA, Floros P, Wong EH, Singh NP. Frontal sinus osteoma: From direct excision to endoscopic removal. J Craniofac Surg. 2019;30:e494. doi: 10.1097/SCS.0000000000005371. [DOI] [PubMed] [Google Scholar]
- 15.Fanchette J, Faucon B, Cartry F, Ratajczak M. Reconstruction of the anterior wall of the frontal sinus by a custom-made titanium prosthesis after resection of a giant osteoma of the frontal sinus. Eur Ann Otorhinolaryngol Head Neck Dis. 2019;136:33–6. doi: 10.1016/j.anorl.2018.07.003. [DOI] [PubMed] [Google Scholar]
- 16.Panagiotopoulos V, Tzortzidis F, Partheni M, Iliadis H, Fratzoglou M. Giant osteoma of the frontoethmoidal sinus associated with two cerebral abscesses. Br J Oral Maxillofac Surg. 2005;43:523–5. doi: 10.1016/j.bjoms.2005.01.020. [DOI] [PubMed] [Google Scholar]
- 17.Rivera T, Rodríguez M, Pulido N, García-Alcántara F, Sanz L. Current indications for the osteoplastic flap. Acta Otorrinolaringol Esp. 2016;67:33–9. doi: 10.1016/j.otorri.2015.01.006. [DOI] [PubMed] [Google Scholar]
- 18.Licci M, Zweifel C, Hench J, Guzman R, Soleman J. Frontoethmoidal osteoma with secondary intradural mucocele extension causing frontal lobe syndrome and pneumocephalus: Case report and review of literature. World Neurosurg. 2018;115:301–8. doi: 10.1016/j.wneu.2018.04.071. [DOI] [PubMed] [Google Scholar]


