Abstract
Background:
The present era is of new tools and technique. Handling of new challenges require, better understanding of microscopic anatomy, which requires better magnification and light. Microscope has played significant role in this, use of endoscope and introduction of exoscope have given new dimensions to this field.
Aim:
This study aims to compare and see the advantages, disadvantages of endoscope with exoscope, will analyze the difference in terms of ergonomics, learning curve, opportunities for training, operating time, magnification, and image quality.
Materials and Methods:
This study was conducted in the Department of Neurosurgery, Bantane Hospital Fujita Health University, Japan. Apart from comparing the specifications of available systems, we conducted a worldwide survey of the two systems through sending questionnaire through mail collected responses and analyzed them.
Results:
Learning curve, magnification, image quality, and ergonomics favors exoscope but depth perception and maneuverability, hand eye coordination, tactile sensation, and usage of different angulation tubes favored endoscope to be superior to exoscope.
Conclusion:
There is more scope for modifications and research in both the instruments. These instruments are not replacement of either and should be used according to their indications.
Keywords: Endoscope, exoscope, survey
Introduction
Optics has played a significant role in the evolution of neurosurgery. The use of magnification came in around 800BC.[1] We started using operating microscope in 20th century. Neurosurgeons throughout the 1960s also began to formally teach and disseminate the techniques of the surgical microscope. Donaghy and Yasargil organized the first microvascular symposium in October 1966.[2,3] With passage of time, we started using improved magnification, with better light system, better maneuverability. Simultaneously, we started using endoscopes. First experiences with the use of this new method in different fields of medicine began in the early 20th century. The development of neuroendoscopy was related to the treatment of hydrocephalus.[4]
A significant advantage of endoscopy includes improvements in surgeon's comfort, lesser fatigue, and less morbidity.[5,6] As compared to operating microscopes focal length is much shorter in endoscopes, thus needs to be placed in close proximity to the intracranial structures which limits the usage of instruments around the scope and frequent obstruction of the lens by blood and tissue obstructed the work flow which limited the neurosurgical application of endoscopy. Latest in the series exoscope, this is a high definition extracorporeal telescope. Exoscope system was developed over the past decade, appears to be an answer to the limitations of microscope and endoscope.[6,7]
Video telescopic operating monitor works on the principle of telescopic surgery with familiar microsurgical instrument; thus, it acts as a bridge between microneurosurgery and endoneurosurgery as well as it improves surgeon comfort, minimizes fatigue, and reduces surgical morbidity and patient discomfort. This system was also used successfully in various cranial and spinal microneurosurgery in place of the microscope as well as in another specialty. In comparison to the endoscope, the exoscope has a broad field of view (600 vs. 25 mm) and greater mean focal distance (200–300 vs. 3–20 mm), allowing the access of neurosurgical instruments without much difficulty. In addition, it is easier to setup exoscope. With the use of exoscope both the surgeon and assistant gets to see the same view. And also allows the rest of operating room (OR) team to follow the procedure with ease. Stereopsis was a matter of concern with initial exoscope. New 3-D 4K-HD exoscope system has significantly solved this issue.
Materials and Methods
This study was conducted in the Department of Neurosurgery, Bantane Hospital Fujita Health University, Japan. Apart from comparing the specifications of available systems, we conducted a worldwide survey of the two systems through sending questionnaire through mail [Table 1], collected responses and analyzed them.
Table 1.
Survey questionnaire
| 1. Which type of institution you are affiliated with |
| (a) Government hospital |
| (b) Private hospital |
| (c) Visiting consultant |
| 2. How frequently you use exoscope and endoscope |
| (a) Frequently |
| (b) Occasionally |
| (c) Rarely |
| (d) Use only endoscope |
| (e) Use only exoscope |
| (f) Does not use either of these |
| 3. Opportunities for training of endoscope |
| (a) Easily available |
| (b) Available at some places |
| (c) Available at few places only |
| 4. Opportunities for training of exoscope |
| (a) Easily available |
| (b) Available at some places |
| (c) Available at few places only |
| 5. In your opinion which instrument is better for depth perception |
| (a) Endoscope |
| (b) Exoscope |
| (c) Both equally good |
| (d) Both have limitations |
| (e) Microscope is better than both |
| 6. Ease of maneuverability |
| (a) Better with exoscope |
| (b) Better with endoscope |
| (c) Both are equal |
| (d) Both have limitations |
| 7. Learning curve |
| (a) No difference |
| (b) Steep learning curve for both |
| (c) Endoscope is easy in comparison to exoscope |
| (d) Exoscope is easy in comparison to endoscope |
| 8. Image quality |
| (a) No significant difference |
| (b) Exoscope gives better image |
| (c) Endoscope gives better image |
| 9. Which instrument you find magnification is better |
| (a) Endoscope is better |
| (b) Exoscope is having better magnification |
| (c) No significant difference |
| (d) Depends on case to case |
| 10. Duration of surgery |
| (a) Similar in both the instruments with minimal difference |
| (b) Significant difference endoscope takes less time |
| (c) Significant difference exoscope takes less |
| (d) Depends on case to case |
Analyzing instruments
EXOSCOPE
(Discussed here are, VITOM, KINEVO, ORBEYE).
VITOM
The Storz VITOM (Storz, Tuttlingen, Germany) was the first neurosurgical exoscope, freeing the surgeon from the need to interface directly with the magnifying device.
Initial version:
Length: 14 cm, outer diameter of 10 mm
Light source: 300-W xenonfiberoptic light box
Image: 23-inch, high-definition monitor
Working distance: 25–60 cm
Limitation: Steep learning curve,[8] fixed pneumatic holder, two-dimensional (2D) view. Now improved to 3D VITOM (Karl Storz, Tuttlingen, Germany).
KINEVO
To combine the advantages of both the standard microscope and the 3D exoscope, the KINEVO (Carl Zeiss AG, Oberkochen, Germany) was designed with the idea of creating a robotic, navigational microscope that can be converted into an exoscope.
Advantages: Kinematics/mobility through mouthpiece adjustment, 3D 4 K resolution, indocyanine green video angiography are integrated into the optics to allow the dye runs to be viewed directly through the microscope, rather than looking away to the monitor.[9]
Limitations: Heavy footprint/size and impaired workflow.[9]
ORBEYE
3D 4 K (Olympus, Tokyo, Japan).
Advantages: 3D 4 K ultra-high-definition imaging. The use of 55-inch 4K 3D monitor contributes to a reduction of surgeon fatigue and facilitates team surgery.
Significant reduction in size (95% smaller than the conventional model).
Limitations: One subjective disadvantage has been the visualization of
Bleeding tissue particularly in muscle or white matter. Image quality degrades and is inferior to that of the microscope in these situations.[9]
Neuroendoscopes
A 0-degree angled eyepiece olympus endoscope for endoscope-assisted
Microneurosurgery Figure 1
Figure 1.
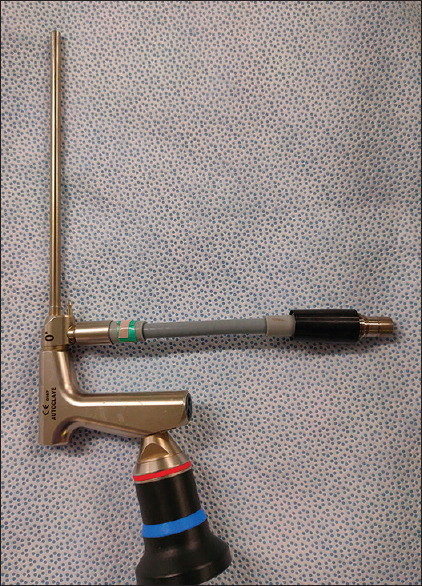
Zero degree endoscope
The use of a microelectro mechanical system has improved light discrimination to view different structures of the brain when obtaining an image.[10]
(KARL STORZ GmbH and Co., Tuttlingen, Germany).
Angulation 15–90 degree
Source of light: Light-emitting diode
The most novel is the introduction of the “insect eye” technology,
Developed by Visionsense Corp., (New York, New York, USA), where a 3D
lens system is attached to the endoscope.
Hopkins' endoscopic systems and optics have proved to be the most influential in the field of neuroendoscopy and provide the basis of the endoscopes that are used to the present day.
Results
Specification of endoscope and exoscope, comparison is show in Table 2. Of the 280 surveys that were received at the recipient e-mail addresses, Graphical distribution of the responses are shown in Figures 2-11 and Table 3.
Table 2.
Comparing specifications of Endoscope with Eexoscope
| Instrument | Endoscope | Exoscope |
|---|---|---|
| Working distance | 3-20 mm | 250-750 |
| Field of view | Small 25 mm | Large 600 mm |
| Depth perception | Better | Limitation |
| Image type | 2D/3D | 2D/3D |
| Chance of damage to intracranial structures | Possibility | Nil |
| Blood obscuring the field | Does happen | Never happens |
| Neck position of surgeon | Neutral | Neutral |
| Comfort to the assistant | Yes | Yes |
| Operating time | Varies from case to case | Varies from case to case |
| Learning curve | Long | Easy |
| Availability | Commonly available | Few places only |
| Advantages | Angled view | Not possible |
| Feasibility in access to small regions | ||
| Disadvantages | Blind surgical corridor | Difficult to re-position |
| Use limited to some procedures |
Figure 2.
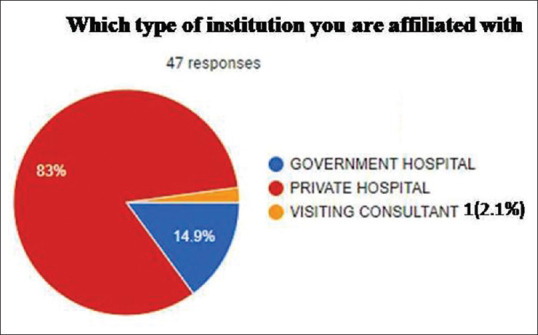
Which type of institution you are affiliated with
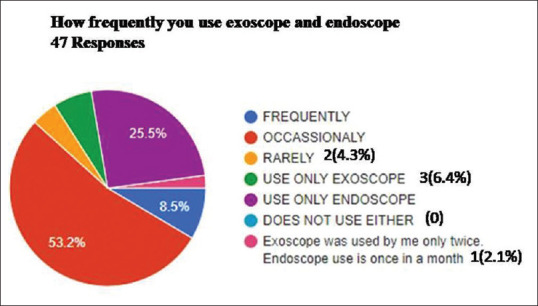
Figure 11.
Duration of surgery
Table 3.
Survey results
| Questions of the survey | Percent distribution of responses | Graphical representation of the responses |
|---|---|---|
| 1. Which type of institution you are affiliated with | ||
| Government | 14.9 | Image 2 |
| Private | 83 | |
| Visiting consultant | 2.1 | |
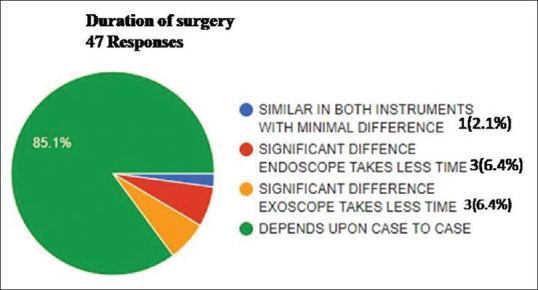
| 2. How frequently you use exoscope and endoscope | ||
| Frequently | 8.5 | Image 3 |
| Occasionally | 53.2 | |
| Rarely | 4.3 | |
| Use only endoscope | 25.5 | |
| Use only exoscope | 6.4 | |
| Does not use either of these | 2.1 | |
| 3. Opportunities for training of endoscope | ||
| Easily available | 17 | Image 4 |
| Available at some places | 66 | |
| Available at few places only | 17 | |
| 4. Opportunities for training of exoscope | ||
| Easily available | 6.4 | Image 5 |
| Available at some places | 21.3 | |
| Available at few places only | 70.2 | |
| Do not know | 2.1 | |
| 5. In your opinion which instrument is better for depth perception (46 response) | ||
| Endoscope | 67.4 | Image 6 |
| Exoscope | 19.6 | |
| Both equally good | 4.3 | |
| Both have limitations | 2.2 | |
| Microscope is better than both | 2.2 | |
| 6. Ease of maneuverability (46 response) | ||
| Better with exoscope | 19.6 | Image 7 |
| Better with endoscope | 76.1 | |
| Both are equal | 4.3 | |
| Both have limitations | - | |
| 7. Learning curve | ||
| No difference | 6.4 | Image 8 |
| Steep learning curve for both | 6.4 | |
| Endoscope is easy in comparison to exoscope | 4.3 | |
| Exoscope is easy in comparison to endoscope | 80.9 | |
| Not used exoscope | 2.1 | |
| 8. Image quality (46 responses) | ||
| No significant difference | 8.7 | Image 9 |
| Exoscope gives better image | 76.1 | |
| Endoscope gives better image | 13 | |
| Endoscope is good but not used exoscope | 2.2 | |
| 9. Which instrument you find magnification is better | ||
| Endoscope is better | 10.6 | Image 10 |
| Exoscope is better | 74.5 | |
| No significant difference | 4.3 | |
| Depends upon case to case | 10.6 | |
| 10. Duration of surgery | ||
| Similar in both the instruments with minimal difference | 2.1 | Image 11 |
| Significant difference endoscope takes less time | 6.4 | |
| Significant difference exoscope takes less | 6.4 | |
| Depends on case to case | 85.1 |
Figure 3.
How frequently you use exoscope and endoscope
Figure 4.
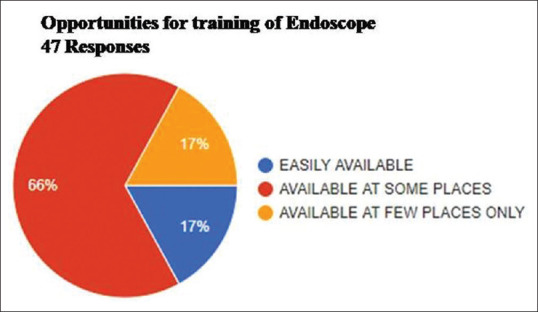
Opportunities for training of Endoscope
Figure 5.
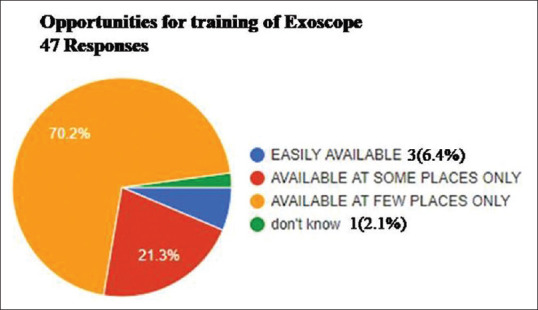
Opportunities for training of Exoscope
Figure 6.
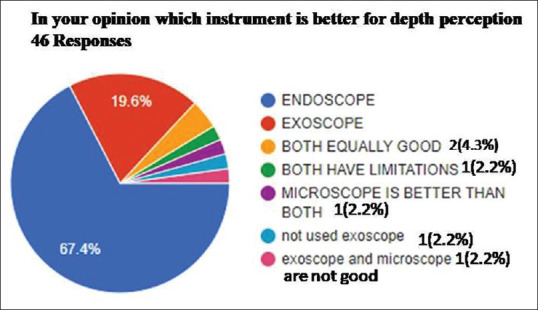
Which instrument is better for depth perception
Figure 7.
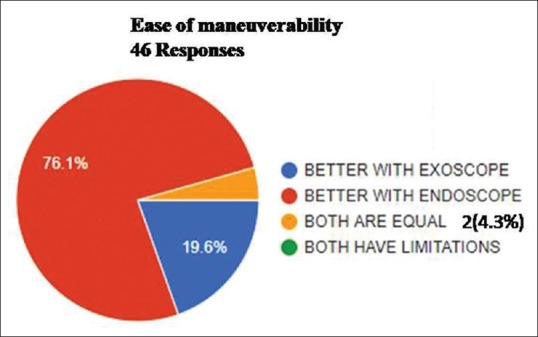
Ease of maneuverability
Figure 8.
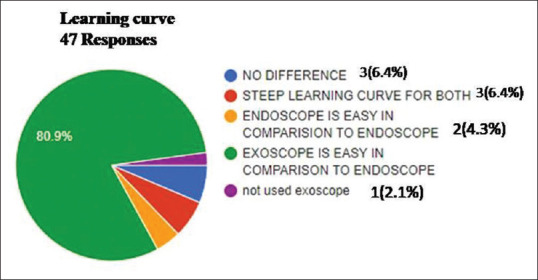
Learning curve
Figure 9.
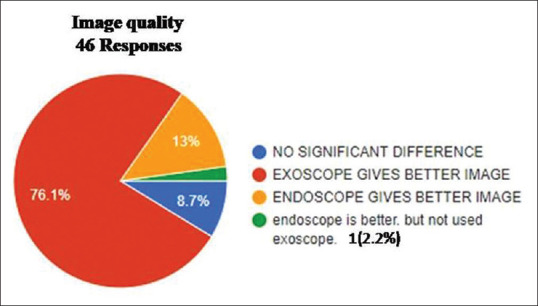
Image quality
Figure 10.
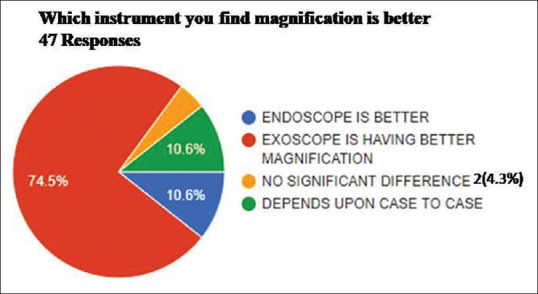
Which instrument you find magnification is better
Forty-seven were returned and thus response rate was 16.78%; therefore, the study is based on the analysis of specifications of various available instruments through available literature and opinion of 47 neurosurgeons working in different parts of the world.
Place of work
Which type of institution you are affiliated with?
Out of 47 responders, majority of people were working in private hospital (83%). 14.9% were working in government hospitals, and 2.1% working as visiting consultant.
Usage of the two instruments
How frequently you use exoscope and endoscope.
Forty-seven people responded.
53.2% people mentioned frequent usage, 25.5% use only endoscope, 6.4% surgeons used only exoscope, and 4.3% mentioned rarely using either of the instruments.
Training opportunities
We received 47 responses, majority of the people said training for endoscope is available at some places only and for exoscope it is available at few places only.
Depth perception
Received 46 responses
Majority of the surgeons (67.4%) felt endoscope is better for depth perception. Only 19.6% felt exoscope is better for depth perception.
Ease of maneuverability
Forty-six responses
76.1% feel endoscope has got better maneuverability, 19.6% feel its better with exoscope.
Learning curve
Forty-seven responses
Majority of the surgeons, 80.9% said exoscope is easy to learn and work.
Quality of the image
Forty-six responses
Majority of the surgeons said that 76.1% said exoscope gives better image while only 13% found endoscope to give better image quality in comparison to exoscope.
Magnification
Forty-seven responses
Majority of the surgeons, 74.5% feel exoscope gives better magnification in comparison to the endoscope; only 10.6% said that endoscope is better.
Duration of surgery
Forty-seven responses
85.1% said that it depends on case to case, 2.1% said it is similar in both the instruments with minimal difference.
Discussion
This study has compared the two operative scope endoscope and exoscope which is actually extension of the preexisting microscope. The use of particular instrument depends on the requirement of case, and capabilities of the instrument. In this study, we have analyzed the specific details of the available endoscope and exoscope system, through survey we gathered the opinion of neurosurgeons working in different parts of the world. Both the endoscope and exoscopes have their advantages and limitations. Exoscopy is a newly emerging technique
for neurosurgery allowing visualization of the intracranial structures from outside of the body rather than inside, the way the endoscope does.[7,11,12,13]
Neuroendoscopes utilize long, narrow-diameter rod lenses with short focal lengths and “direct in-line” visual trajectories, resulting in a relatively fixed, narrow field of view that is easily obscured with the introduction of surgical instruments or with moderate to brisk bleeding.[14]
Due to the limitation of 2D images, endoscopes generally used for limited procedures such as transsphenoidal, endonasal skull base, or intraventricular procedures.[13]
With the development of image guided systems which improves the surgical precision and gives better outcome.[13,15]
Exoscope has a wide and larger working distance as compared to neuroendoscopes, thus permits efficient usage of surgical instruments. Being familiar to the traditional operating microscopes learning curve is much smaller. In addition, there are no issues of lens fogging or cleaning, problems frequently encountered with the endoscopy.[16,17]
Neuroendoscopes
Advantages
Good maneuverability
Depth perception
Minimal brain retraction
Minimal access
Access to blind areas using adequate angulation
Availability
Good opportunities for training.
Disadvantages
Steep learning curve
Use limited to certain procedures only
Chance of damage to intracranial structures
Blood frequently obstructs the vision.
Exoscope
Advantages
Latest exoscope system gives following advantages
4K 3D visualization
Precise images for seeing more
Anatomical details and tissue structure
4K 3D visualization
No image latency
Super high ×26
More comfortable and natural working posture
Comfortable heads-up posture
Freedom from ocular lenses
Positioning flexibility
Ample operative space
Larger working distance
Wider field of view
Familiarity with conventional microscopes
Same picture for surgeon, assistant side-by-side, and other staff.
No obscuration of surgical field with blood.
Disadvantages
Light does not focus in deeper parts
Not good for minimally invasive procedures
Lack of easy availability.
Conclusion
The 3-D 4K-HD is a novel exoscope system aimed at improving visualization and overall operative experience of the entire team. Learning curve, magnification, image quality, and ergonomics favor exoscope but depth perception and maneuverability favors endoscope. Hand eye coordination, tactile sensation, and usage of different angulation tubes favored endoscope to be superior to exoscope. As there is more scope for modifications and research in both the instruments, these instruments are not replacement of either and should be used according to the indications.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Bradbury S. The Evolution of the Microscope. London: Pergam on Press; 1965. [Google Scholar]
- 2.Buncke HJ. Forty years of microsurgery: What's next? J Hand Surg Am. 1995;20:S34–45. doi: 10.1016/s0363-5023(95)80168-5. [DOI] [PubMed] [Google Scholar]
- 3.Buncke HJ. Microsurgery-retrospective. Clin Plast Surg. 1986;13:315–8. [PubMed] [Google Scholar]
- 4.Stachura K, Libionka W. An outline of the history of neuroendoscopy. Przegl Lek. 2007;64:118–20. [PubMed] [Google Scholar]
- 5.Quilici PJ, Greaney EM, Jr, Quilici J, Anderson S. Laparoscopic inguinal hernia repair results: 131 cases. Am Surg. 1993;59:824–30. [PubMed] [Google Scholar]
- 6.Mamelak AN, Nobuto T, Berci G. Initial clinical experience with a high-definition exoscope system for microneuro surgery. Neurosurgery. 2010;67:476–83. doi: 10.1227/01.NEU.0000372204.85227.BF. [DOI] [PubMed] [Google Scholar]
- 7.Mamelak AN, Danielpour M, Black KL, Hagike M, Berci G. A high-definition exoscope system for neurosurgery and other microsurgical disciplines: Preliminary report. Surg Innov. 2008;15:38–46. doi: 10.1177/1553350608315954. [DOI] [PubMed] [Google Scholar]
- 8.Parihar V, Yadav YR, Kher Y, Ratre S, Sethi A, Sharma D. Learning neuroendoscopy with an exoscope system (video telescopic operating monitor): Early clinical results. Asian J Neurosurg. 2016;11:421–6. doi: 10.4103/1793-5482.145551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Langer DJ, White TG, Schulder M, Boockvar JA, Labib M, Lawton MT. Advances in intraoperative optics: A brief review of current exoscope platforms. Oper Neurosurg (Hagerstown) 2019;0:1–10. doi: 10.1093/ons/opz276. [DOI] [PubMed] [Google Scholar]
- 10.Chamot SR, Depeursinge C. MEMS for enhanced optical diagnostics in endoscopy. Minim Invasive Ther Allied Technol. 2007;16:101–8. doi: 10.1080/13645700701267022. [DOI] [PubMed] [Google Scholar]
- 11.Di Ieva A, Komatsu M, Komatsu F, Tschabitscher M. Endoscopic telovelar approach to the fourth ventricle: Anatomic study. Neurosurg Rev. 2012;35:341–8. doi: 10.1007/s10143-011-0371-0. [DOI] [PubMed] [Google Scholar]
- 12.Di Ieva A, Tschabitscher M, Galzio RJ, Grabner G, Kronnerwetter C, Widhalm G, et al. The veins of the nucleus dentatus: Anatomical and radiological findings. Neuroimage. 2011;54:74–9. doi: 10.1016/j.neuroimage.2010.07.045. [DOI] [PubMed] [Google Scholar]
- 13.Mamelak AN, Nobuto T, Berci G. Initial clinical experience with a high-definition exoscope system for microneurosurgery. Neurosurgery. 2010;67:476–83. doi: 10.1227/01.NEU.0000372204.85227.BF. [DOI] [PubMed] [Google Scholar]
- 14.Cruvinel MG, Duarte JB, Castro CH, Costa JR, Kux P. Multimodal approach to rapid discharge after endoscopic thoracic sympathectomy. Acta Anaesthesiol Scand. 2005;49:238–42. doi: 10.1111/j.1399-6576.2004.00558.x. [DOI] [PubMed] [Google Scholar]
- 15.Spiotta AM, Fiorella D, Vargas J, Khalessi A, Hoit D, Arthur A, et al. Initial multicenter technical experience with the Apollo device for minimally invasive intracerebral hematoma evacuation. Neurosurgery. 2015;11(Suppl 2):243–51. doi: 10.1227/NEU.0000000000000698. [DOI] [PubMed] [Google Scholar]
- 16.Carlucci C, Fasanella L, Ricci Maccarini A. Exolaryngoscopy: A new technique for laryngeal surgery. Acta Otorhinolaryngol Ital. 2012;32:326–8. [PMC free article] [PubMed] [Google Scholar]
- 17.Snyderman CH, Pant H, Kassam AB, Carrau RL, Prevedello MD, Gardner PA. The learning curve for endonasal Surgery of the cranial base: A systematic approach to training. In: Kassam AB, editor. Endoscopic Approaches to the Skull Base: Progessin Neurological Surgery. 1st ed. Basel: Karger; 2012. pp. 222–31. [Google Scholar]


