Abstract
Background
Telehealth may be an important care delivery modality in reducing dropout from bariatric surgery programs which is reported globally at approximately 50%.
Methods
In this convergent mixed methods case study of a large, US healthcare system, we examine the impact of telehealth implementation in 2020 on pre-operative bariatric surgery visits and provider perspectives of telehealth use.
Results
We find that telehealth was significantly associated with a 38% reduction in no-show rate compared with the prior year. Additionally, providers had positive experiences with regard to the appropriateness and feasibility of using telehealth in the pre-operative bariatric surgery process.
Conclusions
Telehealth use in the pre-operative bariatric surgery process may lead to greater efficiency in healthcare resource utilization. Insurance providers and bariatric accreditation bodies globally should consider accepting telehealth visits and self-reported weights when determining coverage decisions to ensure access for patients.
Keywords: Telehealth, Bariatric surgery
Introduction
Despite bariatric surgery being the only effective method for sustainable weight loss, it remains underutilized at less than 1% of eligible persons [1]. Even more concerning is that of those who initiate the bariatric surgery process; globally, nearly 50% will drop out prior to completing surgery [2–7]. Required time intensive workup and number of visits are two of the important factors associated with increased dropout [2, 8].
Telehealth allows patients to access care from their chosen location which can help incorporate health into the lives of patients, especially those who have other household and work responsibilities or who for other reasons have difficulty attending in-person visits. Thus, mechanisms of healthcare delivery like telehealth, which can potentially reduce the burden of visits, may improve follow-through.
The COVID-19 pandemic provided a natural experiment to assess telehealth’s impact on pre-operative bariatric visits. First, best practices limited in-person visits, leading to a large increase in the number of telehealth visits completed globally [9, 10]. This allowed clinicians and patients to become familiar with telehealth as a care delivery modality. Second, countries [10–12] and large insurers [13] instituted policies covering telehealth to continue to provide care access without risk of exposure to COVID-19. In this context, we sought to understand telehealth’s impact on pre-operative bariatric visit utilization and provider telehealth experience using a US healthcare system as a case study.
Methods
This study was performed at a large healthcare system caring for a diverse patient population. Using convergent mixed methods design to understand telehealth use (video visits and phone visits) from a healthcare system standpoint, we simultaneously collected data on visit type and provider perspectives [14]. The University of Michigan Institutional Review Board deemed this study exempt given the use of de-identified data.
We quantitatively examined pre-operative workup visits, which are completed in this system by advanced practice providers (APPs) and dieticians. APPs include physician assistants and nurse practitioners who are able to ensure patients are medically, psychologically, and socially optimized for surgery. APPs complete the full initial surgical evaluation; conduct physical exams; order and evaluate testing; refer to specialists such as cardiologists, pulmonologists, psychologists, and social workers when appropriate; and prescribe medications. Dieticians provide longitudinal dietary counseling for patients during the pre-operative process. Visits were classified as an office visit (in-person), phone visit, video visit, or no show. We used Epic Clarity, a reporting database extracted from electronic medical records and validated against manual data pulls, to collect data on visits. We assess contemporary no-show rates versus historical controls (March/April 2020 vs March/April 2019) using chi-square analysis.
For qualitative analysis, all APPs, dieticians, and surgeons were first invited to participate in a focus group to develop an interview guide (Appendix). They were then invited to individual interviews. Interviews were transcribed and then iteratively coded and analyzed using MaxQDA20 (VERBI Software). An inductive method was used to develop themes. All data were collected May-July 2020.
Results
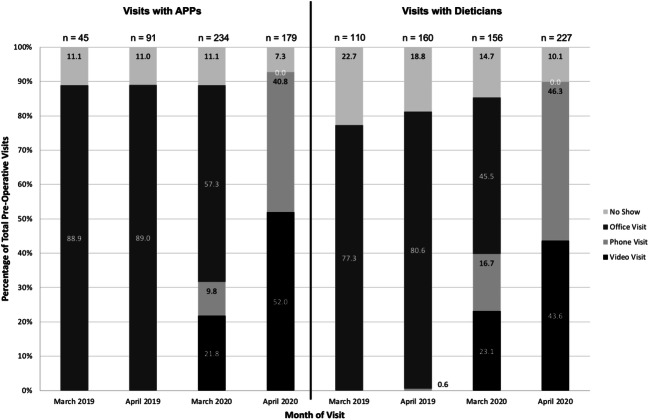
There were 413 APPs and 383 dietician pre-operative visits scheduled in March/April 2020. Figure 1 shows the number and proportion of patient visit types that occurred in March/April 2019 and 2020. No-show rates for all pre-operative visits were 17.2% (2019) and 10.7% (2020), representing a -37.8% difference. Chi-square analysis showed that telehealth implementation in 2020 was significantly associated with decreased no-show rates when compared with 2019 rates (χ2, 10.3; P = .001).
Fig. 1.
Telehealth use in pre-operative bariatric surgery visits
Interviews with APPs (n = 3), a dietician (n = 1), and surgeons (n = 4) revealed the following themes. (1) Providers felt that telehealth allowed adequate patient-provider communication. (2) Regarding policy, providers expressed concern that insurance providers would deny authorization for surgery because of the telehealth modality despite unchanged visit content. (3) Providers identified resource limitations for weight measurements. Table 1 demonstrates representative quotes.
Table 1.
Provider interview themes and participant quotes
| Providers… | Participant quotes |
|---|---|
| felt they had the tools to adequately convey details of the process and operations, including risks and benefits. |
Participant 2 (APP): “You know, bariatrics can be a sensitive subject with weight and obesity. They seemed pretty open to talking about it. And it might be even better nowadays because they can see our facial expressions, clearly and not behind a mask because sometimes those can be uncomfortable conversations like with “How long have you struggled with your weight?” or things like that. So, in terms of having a video avenue is helpful. Yeah, I think overall it went great!” Participant 5 (Surgeon): Yeah, we have had, I mean for the bariatric ones, we have had really good conversations. It’s been all great. Same sort of kind of questions, and people just really intrigued and interested in the process, and also like why it works and how it works. |
| were concerned over the insurance authorization process for patients if weight loss or pre-operative visits were conducted with telehealth rather than in office. |
Participant 1 (APP): Yeah. My only concern is insurance coverage. If we just had you know the information that they would be willing to accept these visits, then I would be 100% on board with only doing virtual visits.” Participant 3 (APP): For our program specifically, we were worried more whether that insurance companies would accept video visits as their monthly weight loss appointments, and whether that would still satisfy their criteria for bariatric surgery. And so, to be honest, we still have not had an answer on that, and I know we are starting to submit people who had you know video, video visits, and it’s gonna be, be kind of a testing process to see which ones get through and which ones do not.” |
| were concerned about patients who did not have access to scales, but they also felt that weight measurements could be completed at a number of other touchpoints in the pre-surgical process. |
Participant 2 (APP): “Yeah, I think that for some of um the heavier patients, some scales do not go as high at home. I mean um, we have people 3, 400 pounds. And their scales. I remember a patient whose PCP scale would not even measure his weight.” Participant 7 (Surgeon): “It would depend how the bariatric program was set up. I think an intake visit virtually is very reasonable. At some point, I would want to see people in person. But, you know, we interact with the bariatric patients for six months, so…” |
Discussion
This study found that telehealth implementation was associated with decreased no-show rates compared with prior year data and identifies positive provider experiences in appropriateness and feasibility of telehealth use. Combined, these findings support continued telehealth use which may mitigate patient dropout from the bariatric surgery process, a global phenomenon.
Possible implementation barriers identified by providers were that patient-reported weights may not be reliable and insurance providers would reject data not obtained in-person. However, prior research has found self-reported weights reliable within 1.3 kg (2.7 lbs) among bariatric patients [15]. Thus, our study demonstrates the importance of alternatives like patient-reported weights to maximize telehealth’s potential.
There are several limitations. First, patients participating in telehealth may have been more willing to use telehealth and show than those who chose in-office or delayed care. Second, this study focused on providers. Future analyses are needed of patient perspectives after pandemic precautions resolve. Patient broadband and equipment limitations are also important to consider to ensure equitable access [16]. However, barriers like childcare, work hours, and long travel distances will remain, so telehealth will continue to be an important option for patient care.
Telehealth has the important potential to increase follow-through to surgery by lowering barriers to bariatric care for patients around the globe. The decrease in no-show rate also holds positive implications for healthcare system efficiency in resource utilization. Thus, continued coverage for telehealth is needed. How telehealth impacts insurance authorization for surgery, a major component of feasibility of telehealth use in bariatric surgery, remains unknown. Insurance providers and bariatric accreditation bodies globally should consider accepting telehealth visits and self-reported weights when determining coverage decisions to ensure access for patients.
Appendix. Interview Guide
| No. | Question | Domain | Prompts |
|---|---|---|---|
| 1 | What were difficulties in patient-provider communication using telehealth? | Patient-provider communication |
Tell me about a typical video/phone visit. Did you feel you were effective in communicating details about care? Did you feel like your patients engaged similarly as before? |
| 2 | Were there any important aspects of an in-person office visit that were lost through telehealth modalities? | Patient-provider communication | How did you feel about connecting with patients through telehealth? |
| 3 | Did you feel that patients understood what was being discussed? | Patient-provider communication | What were indications that patients understood or did not understand what you were saying? |
| 4 | What types of institutional policy made using telehealth easy? Difficult? | Policy | What were the protocol elements? What are areas of uncertainty regarding regulations or policies? |
| 5 | What elements of policy would need to be changed to make telehealth more usable? | Policy | What was the process like of using telehealth? Who did you learn from? |
| 6 | Were care aspects outside of verbal communication lacking in the telehealth visit? | Resources | Were you able to do what you would consider a standard visit? What was missing? |
| 7 | How were these differences addressed? | Resources | When you were not able to do something you typically would do in an office visit, how did you and the patient work through this? |
Funding
Dr. Chao receives funding from the Veterans Affairs Center for Clinical Management Research, VA Ann Arbor Healthcare System. Dr. Telem receives funding from AHRQ K08 HS025778-01A1. Dr. Dimick receives grant funding from the NIH, AHRQ, and BlueCross BlueShield of Michigan Foundation.
Compliance with Ethical Standards
This article does not contain any studies with human participants or animals performed by any of the authors. Informed consent was obtained from all individual participants included in the study.
Disclaimer
This work does not represent the views of the US government.
Conflict of Interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Grace F. Chao, Email: grace.f.chao@yale.edu
Anne P. Ehlers, Email: aehlers@med.umich.edu
Chad Ellimoottil, Email: cellimoo@med.umich.edu.
Oliver A. Varban, Email: ovarban@med.umich.edu
Justin B. Dimick, Email: jdimick@med.umich.edu
Dana A. Telem, Email: dtelem@med.umich.edu
References
- 1.Campos GM, Khoraki J, Browning MG, Pessoa BM, Mazzini GS, Wolfe L. Changes in utilization of bariatric surgery in the United States from 1993 to 2016. Ann Surg. 2020;271(2):201–209. doi: 10.1097/SLA.0000000000003554. [DOI] [PubMed] [Google Scholar]
- 2.Alvarez R, Matusko N, Stricklen AL, Ross R, Buda CM, Varban OA. Factors associated with bariatric surgery utilization among eligible candidates: who drops out? Surg Obes Relat Dis. 2018;14(12):1903–1910. doi: 10.1016/j.soard.2018.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jakobsen GS, Hofso D, Roislien J, Sandbu R, Hjelmesaeth J. Morbidly obese patients--who undergoes bariatric surgery? Obes Surg. 2010;20(8):1142–1148. doi: 10.1007/s11695-009-0053-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Taylor T, Wang Y, Rogerson W, Bavin L, Sharon C, Beban G, Evennett N, Gamble G, Cundy T. Attrition after acceptance onto a publicly funded bariatric surgery program. Obes Surg. 2018;28(8):2500–2507. doi: 10.1007/s11695-018-3195-y. [DOI] [PubMed] [Google Scholar]
- 5.Pitzul KB, Jackson T, Crawford S, Kwong JC, Sockalingam S, Hawa R, et al. Understanding disposition after referral for bariatric surgery: when and why patients referred do not undergo surgery. Obes Surg. 2014;24(1):134–140. doi: 10.1007/s11695-013-1083-z. [DOI] [PubMed] [Google Scholar]
- 6.Gill RS, Karmali S, Hadi G, Al-Adra DP, Shi X, Birch DW. Predictors of attrition in a multidisciplinary adult weight management clinic. Can J Surg. 2012;55(4):239–243. doi: 10.1503/cjs.035710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Benediktsdottir A, Halldorsson TI, Bragadottir GJ, Gudmundsson L, Ramel A. Predictors of dropout and bariatric surgery in Icelandic morbidly obese female patients. Obes Res Clin Pract. 2016;10(1):63–69. doi: 10.1016/j.orcp.2015.03.009. [DOI] [PubMed] [Google Scholar]
- 8.Diamant A, Milner J, Cleghorn M, Sockalingam S, Okrainec A, Jackson TD, Quereshy FA. Analysis of patient attrition in a publicly funded bariatric surgery program. J Am Coll Surg. 2014;219(5):1047–1055. doi: 10.1016/j.jamcollsurg.2014.08.003. [DOI] [PubMed] [Google Scholar]
- 9.Mehrotra A, Chernew M, Linetsky D, Hatch H, Cutler D. The impact of the COVID-19 pandemic on outpatient visits: practices are adapting to the new Normal. The Commonwealth Fund. 2020 25, 2020.
- 10.Anonymous Shanghai. The smartphone will see you now. The Economist. 2020 March 7, 2020;434(9184):64.
- 11.Insurance Regulatory and Development Authority of India. Guidelines on telemedicine. 2020.
- 12.Kwinda M. Notice to amend telemedicine guidelines during COVID-19. In: Health Professions Council of South Africa, editor. South Africa; 2020.
- 13.Centers for Medicare and Medicaid Services. Medicare telemedicine health care provider fact sheet. 2020 [updated July 2, 2020]; Available from: https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet. Accessed 21 Aug 2020.
- 14.Dossett LA, Kaji AH, Dimick JB. Practical guide to mixed methods. JAMA Surg. 2020;155(3):254–55. doi: 10.1001/jamasurg.2019.4388. [DOI] [PubMed] [Google Scholar]
- 15.Chao GF, Bonham AJ, Ross R, Stricklen A, Ghaferi AA. Patient-reported comorbidity assessment after bariatric surgery: a potential tool to improve longitudinal follow-up. 2020; Under Review. Presented at the Michigan Bariatric Surgical Collaborative Tri-Annual Meeting February 2, 2018.
- 16.Velazquez D, Mehrotra A. Ensuring the growth of telehealth during COVID-19 does not exacerbate disparities in care. Health Aff. 2020; 10.1377/hblog20200505.591306/full/.