Abstract
One in three Cambodian children under 5 years of age are stunted. This study adopted a multidimensional approach to understand the influence of a series of contextual factors on the nutritional status of Cambodian children. In this study, we use a multidimensional poverty framework to identify a combination of interventions likely to achieve reductions in child stunting, in Cambodia. We used the UNICEF Multiple Overlapping Deprivation Analysis tool and data from the Cambodia Demographic and Health Survey 2014 to assess children's multidimensional poverty across nutrition, health, early childhood development, water, sanitation, and housing dimensions. We found that 80% of children under age five were deprived in at least two poverty dimensions. Multivariate logistic regression analysis revealed that reducing the likelihood of being deprived in three or more poverty dimensions was associated with a significant reduction of the probability of being stunted, after controlling for potential confounders. The combined probability of nondeprivation in nutrition, sanitation, and health dimensions had the largest effect on reducing the probability of stunting. The results of this study highlight the multiple, intersecting needs of children and their associated explanatory factors. Targeted and integrated cross‐sectoral policies that reinforce comprehensive early childhood interventions are needed for improving nutritional status as part of a wider set of child poverty reduction measures in Cambodia.
Keywords: Cambodia, early childhood, multidimensional poverty, nutrition, stunting
Key messages.
Most Cambodian children are multidimensionally deprived with the highest degree of deprivation in the nutrition, health, water, sanitation, and housing dimensions.
Stunting is strongly linked to multidimensional poverty and requires nutrition‐specific and nutrition‐sensitive interventions as part of broad packages of cross‐sectoral programmes during the first 1,000 days—from conception to age 2 years—to improve children's direct environments.
Understanding children's deprivations across multiple dimensions is necessary to identify entry points for integrated high‐impact early childhood interventions to address growth and development.
Long‐term implications of stunting, along with necessary conditions for catch‐up growth, should be explored among school‐age children in Cambodia.
1. INTRODUCTION
Good nutrition is a crucial component of children's well‐being during the foundational years of early childhood. The far‐reaching consequences of unmet nutritional needs in utero and during early childhood influence on chronic and intergenerationally transmitted poverty experienced by children (Harper, Marcus, & Moore, 2003; Hulme & Shepherd, 2003; Minujin, Delamonica, Davidziuk, & Gonzalez, 2016). Stunting, or low “height‐for‐age” (World Health Organization, 2008), is used as an indicator of chronic undernutrition with potentially irreversible consequences for children's long‐term physical and cognitive development, which altogether extend to household, community, and societal levels (Campisi, Cherian, & Bhutta, 2017; De Neubourg & de Neubourg, 2012; Khasnutdinova & Grjibovski, 2010; de Onis & Branca, 2016). Timely interventions to prevent stunting and protect early childhood development (ECD) yield the highest rates of return to human capital investment and are especially critical in the first 1,000 days, from conception to age 2 years.
Cambodia is the second‐poorest country in Southeast Asia, with more than one third of the population living under the poverty threshold of USD 1.90/day. Despite rapid economic growth in recent years and a reduction in the prevalence of stunting from 44.6% in 2000 to 32.0% in 2014 (National Institute of Statistics [NIS], Directorate General for Health, & ICF International [ICF], 2015; NIS, Directorate General for Health, & ORC Macro, 2001), the economic burden of maternal and child undernutrition is high and estimated to amount to 1.7% of Cambodia's gross domestic product (GDP) (Moench‐Pfanner et al., 2016). Although positive progress has been made in reducing child stunting in Cambodia, approximately one in every three children has stunted growth and therefore risks not meeting his or her developmental potential (Ministry of Planning, Cambodia, & NIS, 2017).
The drivers of child stunting in Cambodia have been well explored. Several studies explicate the association of child stunting with life‐cycle sensitive maternal undernutrition, repeated child parasitic infection, low levels of parental education, intergenerationally transmitted poverty, inadequate sanitation, and the nutrient inadequacy of traditional Cambodian diets coupled with early uptake of complementary foods (Anderson, Cornwall, Jack, & Gibson, 2008; Ikeda, Irie, & Shibuya, 2013; Perignon et al., 2014; Sunil & Sagna, 2015). Our study seeks to identify the interventions that could directly and immediately prevent stunting, by analysing the effects of simultaneous deprivations, as revealed by a multidimensional poverty analysis, on the likelihood of stunting among children. We investigate the multiple deprivations that contribute to child stunting in early childhood, and how overlaps between them point to opportunities for improved integration of effective interventions in early childhood to reduce child stunting. Our study aims to generate new insights into the pathways for reducing child stunting by analysing children's nutritional status as a function of multiple and concurrent deprivations within a multidimensional poverty, or deprivation, framework.
We measure children's multidimensional poverty in terms of their simultaneously experienced deprivations of conditions or material resources, independent of income, that are essential for well‐being and development, following the framework of multidimensional child poverty and deprivation as developed by Alkire and Roche (2012), De Neubourg, de Milliano, and Plavgo (2014), and Gordon, Nandy, Pantazis, Pemberton, and Townsend (2003). We define multidimensional child poverty as multidimensional deprivation, and the terms are used interchangeably in our study, following the convention in this field of research.
2. DATA AND METHODS
2.1. Study design and sample
We conducted a secondary analysis of Cambodia's 2014 Demographic and Health Survey (CDHS, 2014) data. Comprehensive information on the sampling technique and survey procedures applied for data collection in the CDHS have been published in detail elsewhere (NIS et al., 2015). In summary, the CDHS collected individual‐level data on anthropometry for children under age five, maternal and infant health services, infant and young child feeding practices, early childhood education and development indicators, and household‐level data on water, sanitation, and housing conditions.
2.2. Analytical methods
The multidimensional deprivation analysis used in this study was based on the Multiple Overlapping Deprivation Analysis (MODA) methodology by De Neubourg, Chai, de Milliano, Plavgo, and Wei (2013). It is designed to be sensitive to children's life cycle and to the incidence and intensity of deprivations, reflecting the extent to which children's rights and needs are fulfilled. Using MODA, we first analysed children's deprivations by (a) calculating the percentage headcount rates of children deprived in six single dimensions (nutrition, health, ECD, water, sanitation, and housing) and (b) analysing children's multiple deprivations by calculating three multidimensional poverty indices based on those developed by Alkire and Foster (2011). The child deprivation headcount ratio by single indicator and dimension was calculated using the formula:
where hj, r is the headcount ratio of children deprived in a dimension, j, of the reference child population, r; qj, r is the number of children who are deprived in a dimension j of the reference child population r; nr is the total reference child population r; yj is the deprivation status of a child i in a dimension j, where yj = 1 if xj < Zj (deprivation) and yj = 0 if xj ≥ Zj (no deprivation); xj is the value of dimension j for child i; Zj is the threshold of deprivation for the dimension j. The formula was also applied to calculate headcount ratios for each indicator. Indicators were chosen to minimise values treated as missing in the single‐dimension analysis. Children with missing values in an indicator were excluded from the deprivation headcount of that indicator, to ensure that the analysis is specific to the deprivation status of the individual child for whom the indicator or dimension is relevant.
Second, we summed the number of deprivations experienced per child and calculated a deprivation headcount ratio of the total number of children deprived at each level of poverty intensity according to the poverty cut‐off, k, presenting the overall multidimensional poverty distribution. Missing values in individual dimensions were assigned a value of “0” (nondeprived), to ensure all dimensions had the same number of observations, following the approach as used by De Neubourg et al. (2013). Resulting deprivation headcount rates in the multidimensional analysis represent a slight underestimation of the single‐dimension analysis. An overlap analysis calculated the headcount rate of children concurrently deprived in all permutations of any two or more dimensions at a time. The Alkire–Foster indices calculated are the deprivation headcount (H), the average intensity of deprivation (A), and the adjusted deprivation headcount (M 0).
Nutrition, health, and ECD dimensions and indicators were evaluated at the level of the individual child. Deprivation in water, sanitation and housing dimensions, and indicators are constructed from variables measured at the household level, and therefore use the household as the unit of measurement and the individual child as the unit of analysis (i.e., a child is considered deprived if it is living in a household that is considered deprived in these dimensions).
2.3. Analysis parameters
The selection of indicators, dimensions, and thresholds of deprivation was based on the MODA protocols as specified in the guidelines by De Neubourg et al. (2013) to capture children's unmet needs and rights based on the International Convention on the Rights of the Child (UN General Assembly, 1989), national and international standards, and was finalised through consultation with national stakeholders. The dimensions, indicators, and thresholds applied in this study therefore reflect the nationally contextualised adaptation of or adherence to international standards on the necessary conditions for child well‐being and development, as specified in the International Convention on the Rights of the Child and by national and international nutrition, health, housing, and children's institutions. The six dimensions and 14 indicators used to assess the deprivation status of children age 0–59 months are presented in Table 1.
Table 1.
Analysis parameters: Dimensions, indicators, and deprivation thresholds
| Dimension | Indicator | Indicator deprivation threshold |
|---|---|---|
| Nutrition | Unexclusive breastfeeding | Child under 6 months not exclusively breastfed (WHO, 2008). |
| No minimum acceptable diet | Child age 6–23 not meeting standards for minimum meal frequency or minimum dietary diversity (WHO, 2008). | |
| Wasting | Child's weight‐for‐height Z‐score < −2 SD from median of WHO reference population, considered thin (wasted) and acutely malnourished (WHO, 2008). | |
| Underweight | Child's weight‐for‐age Z‐score standard deviations −2 SD from median of the WHO reference population, considered underweight (WHO, 2008). | |
| Health | Unskilled birth attendance | Child's mother not assisted or assisted by unskilled birth attendant in 5 years preceding the survey (NIS et al., 2015). |
| Missing immunisations | Child not received all routine immunisations according to recommended schedule (NIS et al., 2015). | |
| Early childhood development (ECD) | No early childhood education (ECE) attendance | Child 36–59 months not attending early childhood education or preschool programme. |
| No books or toys (support for learning) | Child does not have access to any books or homemade or manufactured toys. | |
| Water | Unimproved drinking water source | Household main source of drinking water is unimproveda. |
| No handwashing | Soap and water not observed at a place of handwashing or no observed place for handwashing (WHO & United Nations Children's Fund, 2017). | |
| Sanitation | Unimproved toilet | Household uses unimproved toilet facilityb. |
| Housing | Overcrowding | Household has >4 persons per sleeping roomc (UN‐HABITAT, 2007). |
| Inadequate floor, roof, walls | Roof, floor, or exterior walls made of natural materials not considered permanent (NIS et al., 2001). | |
| Indoor pollution from solid cooking fuel | Household uses solid cooking fuel and cooking takes place inside the house (Rees, 2016). |
The NIS et al. (2015), referring to World Health Organization (WHO) and United Nations Children's Fund (UNICEF) (2017) classify unimproved drinking water sources during both rainy and dry seasons as unprotected/dug well; unprotected spring; tanker truck/cart with small tank; surface water; and other. Toilet facilities as flush/pour flush not to sewer/septic tank/pit latrine; pit latrine without slab/open pit; bucket; hanging toilet/hanging latrine; and no facility/bush/field.
Unimproved toilet facilities are classified by WHO and UNICEF (2017) and NIS et al. (2015) as flush/pour flush not to sewer/septic tank/pit latrine; pit latrine without slab/open pit; bucket; hanging toilet/hanging latrine; and no facility/bush/field.
Children have a weight of 0.5.
Children were considered deprived in a particular dimension if they were deprived in any indicators assigned to the respective dimension, per the union approach described by De Neubourg et al. (2013). Deprivation status in an indicator or dimension was measured using a binary variable, with a value of “1” for deprivation exists and “0” for no deprivation. Children who are not part of the indicator reference population, but who are included within the age group of children under age 5 years, are considered to be nondeprived to limit the bias of the deprivation headcount calculations. For example, in the case of the nutrition indicators that span different age groups to be both sensitive and relevant to life‐cycle needs, children age 6 months and above are not considered in the single deprivation headcount of the unexclusive breastfeeding indicator. The aggregated indicators of the nutrition dimension therefore reflect different facets of the age‐specific nutrition situation for all children under age 5 years in the sample.
2.4. Statistical analysis
Multiple multivariate logistic models were developed to examine the relationship between stunting, various individual and household characteristics, and the results of the multidimensional poverty analysis, including dimensions considered entry points for stunting reduction. We estimated the following models:
Model 1 estimates the relationship between various individual and household characteristics and children's probability of being stunted, to examine which of children's characteristics predict their likelihood of being stunted.
Model 2a–c examines the relationship between being nondeprived in three or more dimensions at a time (reference category: being deprived in 0, 1, or 2 dimensions) and being stunted, holding constant the covariates used in Model 1. Model 2a–c estimates the same model separately at the national, urban, and rural levels, respectively.
Model 3a–g estimates the relationship between being nondeprived in each of the measured single dimensions of deprivation and being stunted, holding constant the covariates in Model 1. Model 3g includes all dimensions as additional covariates to study the joint relationship of deprivation in these dimensions with the stunting variable. Model 3a–g is estimated separately at the national, urban, and rural level. The dimensions are considered potential intervention entry points to reduce stunting.
The explanatory variables in the models include being in the poorest two wealth quintiles ; no or primary maternal education; maternal age at first birth under 18; maternal height under 145 cm; male child gender; child's age; the number of household members by age group; rural area of residence; and residence in the north‐eastern region. Child's age and household composition were continuous, whereas all other variables were categorical and binary. The variables denoting maternal height under 145 cm and maternal age at first birth were converted from continuous into categorical variables to control for the effects of early pregnancy and maternal stunting. All other categorical variables could only be expressed in their original categorical form. The model covariates were chosen based on theoretical and empirical literature review of risk factors for child stunting, data availability, and statistical association with higher rates of stunted children during the secondary data analysis in this study. The covariates were chosen and eliminated based on bivariate correlation tests for statistically significant association with the probability of being stunted. All regressors were then tested for collinearity and had a Pearson's correlation coefficient of r < 0.5. All statistically significant subgroup differences in the single and multidimensional analyses are based on pairwise t‐tests and are denoted with asterisks. The marginal effect is expressed as a percentage point change in the probability of being stunted given a one‐unit change in the regressor, in the adjusted models.
3. RESULTS
3.1. Single‐dimension analysis
The final sample in this study consists of 7,906 children under age five, with the majority in rural areas (86.4%), compared with urban (13.6%) areas. Table 2 presents the deprivation headcount ratio of children under five for each indicator in each dimension, as a proportion of the reference population. A general high rate of deprivation was observed across all measured dimensions with 37.1% for water, 47.4% for nutrition, 60.5% for sanitation, and 62.5% for housing. Nutrition deprivation was driven by the high percentage (54.8%) of children 0–23 months not meeting minimum acceptable diet standards. Deprivation rates among children living in rural areas were higher than in urban areas across all dimensions, though the percentage of children with nutrition deprivation was almost similar in urban (42.6%) and rural (48.1%) areas, largely due to the high rate (61.7%) of nonexclusive breastfeeding among children under 6 months in urban areas.
Table 2.
Deprivation headcount rates by indicator and dimension
| Indicator deprivation headcount (%)a | Dimension deprivation headcount (%)b | ||||||
|---|---|---|---|---|---|---|---|
| Dimension | Indicator | National | Urban | Rural | National | Urban | Rural |
| Nutrition | Unexclusive breastfeeding | 35.1 | 61.7* | 30.8* | 47.4 | 42.6* | 48.1* |
| No minimum acceptable diet | 54.8 | 55.3 | 54.7 | ||||
| Wasting | 9.3 | 7.4 | 9.6 | ||||
| Underweight | 23.5 | 14.8 | 24.9 | ||||
| Health | Unskilled birth attendance | 10.6 | 1.5* | 12.1* | 25.2 | 11.6* | 27.4* |
| Missing immunisations | 18.9 | 10.4* | 20.3* | ||||
| ECD | No ECE attendance | 81.8 | 58.3* | 85.3* | 71.1 | 47.7* | 74.9* |
| No books or toys | 46.7 | 24.3* | 50.3* | ||||
| Water | Unimproved drinking water source | 37.1 | 7.1* | 41.8* | 37.1 | 7.1* | 41.8* |
| Sanitation | No handwashing | 34.0 | 8.5* | 38.0* | 60.5 | 16.1* | 67.5* |
| Unimproved toilet | 49.2 | 10.6* | 55.3* | ||||
| Housing | Inadequate floor, roof, walls | 14.6 | 4.2* | 16.2* | 62.5 | 40.4* | 66.0* |
| Indoor pollution from solid cooking fuel | 34.1 | 15.1* | 37.1* | ||||
| Overcrowding | 38.2 | 29.6* | 39.6* | ||||
| Total | 100.0 | 13.6 | 86.4 | 100.0 | 13.6 | 86.4 | |
| Total in numbersc | 1,372,994 | 186,864 | 1,186,130 | 1,372,994 | 186,864 | 1,186,130 | |
Note. ECD: early childhood development; ECE: early childhood education.
Headcount ratios are calculated for the reference population only. For example, 35.1% of children under 6 months were deprived in exclusive breastfeeding.
Headcount ratios are calculated with the reference population being all children under 5 years.
Estimated using official population projections for 2014 (Ministry of Planning, Cambodia, & NIS, 2017).
P < 0.05.
3.2. Multidimensional analysis
Most children under five had multiple deprivations (Table 3). Children in rural areas experienced a significantly higher level of average deprivation intensity among the deprived children, than children in urban areas, at every level of increasing deprivation intensity. More than half (57.1%) of children aged 0–59 months were concurrently deprived in at least three dimensions, and these children experience, on average, 65.0% of the total possible deprivations. The adjusted deprivation headcount (M 0) index was also significantly higher in rural (0.41) compared with urban (0.11) areas at every deprivation intensity level.
Table 3.
Multidimensional deprivation ratios by national and subnational level
| Number of deprivations | Multidimensional deprivation headcount (H) % | Average intensity of deprivations among the deprived (A) % | Adjusted deprivation headcount (M 0) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| National | Urban | Rural | National | Urban | Rural | National | Urban | Rural | |
| 1–6* | 93.0 | 76.0 | 95.7 | 49.9 | 32.7 | 52.1 | 0.46 | 0.25 | 0.50 |
| 2–6* | 77.9 | 44.4 | 83.1 | 56.4 | 44.1 | 57.4 | 0.44 | 0.20 | 0.48 |
| 3–6* | 57.1 | 18.7 | 63.2 | 64.8 | 59.0 | 65.0 | 0.37 | 0.11 | 0.41 |
| 4–6* | 33.6 | 7.1 | 37.8 | 75.1 | 73.5 | 75.2 | 0.25 | 0.05 | 0.28 |
| 5–6* | 14.1 | 2.7 | 15.8 | 86.9 | 84.8 | 86.9 | 0.12 | 0.02 | 0.14 |
| 6* | 3.0 | 0.2 | 3.4 | 100.0 | 100.0 | 100.0 | 0.03 | 0.00 | 0.03 |
P < 0.05.
Children deprived in the nutrition, ECD, water, sanitation, or housing dimensions were more likely to be deprived in at least three other dimensions simultaneously, with consistently higher rates of three‐way overlap in rural areas. The highest incidence of three‐way overlap occurred for nutrition, housing, and sanitation dimensions (Figure S2).
3.3. Stunting
More than 30% of children under 5 years of age were stunted, with the highest prevalence in rural areas (33.0%) and in the north‐east region (37.2%). Deprivation incidence was higher among stunted children than among nonstunted children at all levels of deprivation intensity (see Figure S3). At the national level, 22.8% of children with at least three deprivations were both stunted and multidimensionally deprived, 34.6% were only deprived, and 9.4% were only stunted, meaning that most children who are stunted are also multidimensionally deprived (Figure S4). Stunted children consistently showed a larger overlap of deprivations across dimensions than nonstunted children, particularly across the water, housing, nutrition, and sanitation dimensions. Figure 1 shows that 20.8% of stunted children were deprived in nutrition, water, and sanitation at the same time, compared with only 9.5% of notstunted children.
Figure 1.
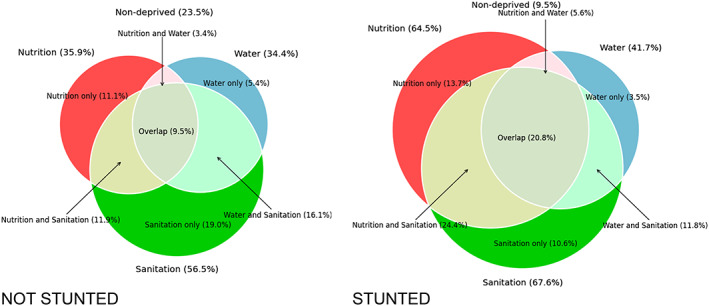
Three‐way overlap of deprivation in the nutrition, water, and sanitation dimensions for not stunted and stunted children. Source: author's calculations using CDHS 2014
To investigate the role of household wealth in the prevalence of stunting, we plotted the headcount ratios of deprivation in nutrition, health, ECD, and stunting against the CDHS 2014 household asset‐wealth index (Figure S5). Compared with a relatively steep decline in the prevalence of children deprived in health and ECD between the first and third wealth quintiles, the prevalence of stunting and nutrition deprivation decreased only slightly between the first and fourth wealth quintiles in urban and rural areas.
As shown in Table 4, being deprived in less than three‐dimensions had a sizeable negative marginal effect on the probability of being stunted. Factors significantly associated with being stunted included maternal height < 145 cm (average marginal effect [AME]: 0.196, CI: 0.134, 0.258, P < 0.01); being in the poorest two wealth quintiles (AME: 0.099; CI: 0.067, 0.130, P < 0.01); an additional year of child's age (AME: 0.048, CI: 0.39, 0.057, P < 0.01), residence in the north‐east and rural areas, and presence of an additional child aged 5–14 years in the household (AMEs less than 0.05).
Table 4.
Average marginal effects on the probability of child stunting
| (1)a | (2a)a | (2b)a | (2c)a | |
|---|---|---|---|---|
| Variables | Stunting | National | Urban | Rural |
| Not deprived in ≥3 deprivations | −0.159*** | −0.163*** | −0.155*** | |
| (0.0148) | (0.0474) | (0.0164) | ||
| Household in the poorest 2 wealth quintiles | 0.0985*** | |||
| (0.0160) | ||||
| Mother has no or primary education | 0.0139 | 0.00375 | 0.0146 | 0.00134 |
| (0.0166) | (0.0163) | (0.0366) | (0.0183) | |
| Mother's age at first birth <18 | 0.00655 | 0.00144 | −0.0298 | 0.00549 |
| (0.0231) | (0.0228) | (0.0598) | (0.0247) | |
| Mother's height <145 cm | 0.191*** | 0.196*** | 0.205* | 0.195*** |
| (0.0318) | (0.0316) | (0.105) | (0.0333) | |
| Child is a boy | 0.0148 | 0.0126 | 0.0260 | 0.0109 |
| (0.0137) | (0.0136) | (0.0328) | (0.0149) | |
| Child's age | 0.0479*** | 0.0493*** | 0.0295** | 0.0524*** |
| (0.00479) | (0.00473) | (0.0120) | (0.00514) | |
| No. of children 0–4 years in household | 0.00754 | −0.000744 | −0.00506 | 0.000795 |
| (0.0112) | (0.0111) | (0.0247) | (0.0124) | |
| No. of children 5–14 years in household | 0.0263*** | 0.0225*** | 0.0337** | 0.0207*** |
| (0.00646) | (0.00642) | (0.0152) | (0.00707) | |
| No. of children 15–17 years in household | −0.0159 | −0.0203 | −0.00493 | −0.0239 |
| (0.0168) | (0.0167) | (0.0365) | (0.0185) | |
| No. of adults 18–59 years in household | −0.00161 | −0.00171 | −0.0115 | 0.00172 |
| (0.00535) | (0.00525) | (0.00979) | (0.00612) | |
| No. of adults over age 60 in the household | 0.0138 | 0.00801 | 0.0392* | 0.00174 |
| (0.0122) | (0.0120) | (0.0231) | (0.0137) | |
| Rural area | 0.0430** | |||
| (0.0218) | ||||
| North‐east region | 0.0442** | 0.0485*** | 0.0202 | 0.0514*** |
| (0.0190) | (0.0188) | (0.0592) | (0.0199) | |
| Total | 4,389 | 4,389 | 1,195 | 3,194 |
AME ± SE. Standard errors in parentheses.
P < 0.1.
P < 0.05.
P < 0.01.
Model 2a–c presents the association between having a low deprivation intensity (0, 1, or 2 deprivations) and the likelihood of being stunted. At the national level, not being deprived in at least three dimensions was significantly associated with a −15.9‐percentage point change in the probability of being stunted (P < 0.01), controlling for no or primary maternal education, maternal age at first birth under 18, maternal height under 145 cm, male child gender, child's age, the number of household members by age group, rural area of residence, and residence in the north‐eastern region. In rural areas, not being deprived in three or more dimensions was also negatively associated with being stunted (AME: −0.155, CI: −0.187, −0.122, P < 0.01), in the adjusted model.
Table 5 presents the results of Model 3a–g for rural areas, estimating the probability change to being stunted given the likelihood of a nondeprived status in respectively nutrition, health, ECD, water, sanitation, housing, and all dimensions jointly (holding constant deprivation status in other dimensions), controlling for key characteristics used in Model 2a–c. In rural areas, nondeprivation in all dimensions except ECD were significantly associated with a reduction in the probability of being stunted without controlling for deprivation in other dimensions. Not being deprived in nutrition was associated with the highest average marginal effect of a −26.2‐percentage point change in the predicted probability of being stunted (AME: −0.262, CI: −0.291, −0.233, P < 0.01). Controlling for nondeprivation in all dimensions, in addition to the other covariates, showed that in the joint relationship of the dimensions and their effect on the predicted probability of stunting, the effect of nondeprivation in health became less significant (AME: −0.031, CI: −0.064, 0.002, P < 0.1), whereas the effects of nondeprivation in housing became insignificant (P = 0.123). The significance and magnitude of the effects of nondeprivation in nutrition (AME: −0.258, CI: −0.287, −0.229, P < 0.01) and sanitation (AME: −0.050, CI: −0.084, −0.171, P < 0.01) remained robust. Comparing the same model 3g estimated for urban areas (Table S8) showed only nondeprivation in nutrition and housing were associated with a negative change to the probability of being stunted, respectively −23.0 (CI: −0.302, −0.157, P < 0.01) and −7.9 (CI: −0.152, −0.007, P < 0.05) percentage points.
Table 5.
Average marginal effects of the probability of being deprived in single and multiple dimensions, in rural areas
| (3a)a | (3b)a | (3c)a | (3d)a | (3e)a | (3f)a | (3g)a | |
|---|---|---|---|---|---|---|---|
| Variables | Nutrition | Health | ECD | Water | Sanitation | Housing | All dimensions |
| Not deprived in nutrition | −0.262*** | −0.258*** | |||||
| (0.0146) | (0.0147) | ||||||
| Not deprived in health | −0.0585*** | −0.0314* | |||||
| (0.0179) | (0.0170) | ||||||
| Not deprived in ECD | −0.0147 | 0.00257 | |||||
| (0.0189) | (0.0183) | ||||||
| Not deprived in water | −0.0372** | −0.0249* | |||||
| (0.0155) | (0.0150) | ||||||
| Not deprived in sanitation | −0.0745*** | −0.0504*** | |||||
| (0.0168) | (0.0170) | ||||||
| Not deprived in housing | −0.0411** | −0.0255 | |||||
| (0.0168) | (0.0165) | ||||||
| Mother has no or primary education | 0.0298* | 0.0276 | 0.0353** | 0.0333* | 0.0193 | 0.0324* | 0.00880 |
| (0.0170) | (0.0179) | (0.0177) | (0.0177) | (0.0182) | (0.0177) | (0.0178) | |
| Mother's age at first birth <18 | 0.00460 | 0.00821 | 0.0141 | 0.0119 | 0.00967 | 0.0145 | −0.00235 |
| (0.0240) | (0.0251) | (0.0252) | (0.0251) | (0.0250) | (0.0252) | (0.0238) | |
| Mother's height <145 cm | 0.170*** | 0.199*** | 0.198*** | 0.196*** | 0.193*** | 0.195*** | 0.165*** |
| (0.0324) | (0.0335) | (0.0336) | (0.0336) | (0.0336) | (0.0336) | (0.0324) | |
| Child is a boy | 0.0186 | 0.0120 | 0.0119 | 0.0130 | 0.0129 | 0.0106 | 0.0195 |
| (0.0144) | (0.0150) | (0.0151) | (0.0151) | (0.0150) | (0.0151) | (0.0144) | |
| Child's age | 0.0649*** | 0.0513*** | 0.0502*** | 0.0507*** | 0.0514*** | 0.0513*** | 0.0653*** |
| (0.00502) | (0.00522) | (0.00530) | (0.00522) | (0.00521) | (0.00522) | (0.00511) | |
| No. of children 0–4 years in household | −0.00967 | 0.0120 | 0.0132 | 0.0144 | 0.0113 | 0.0128 | −0.0153 |
| (0.0120) | (0.0125) | (0.0127) | (0.0124) | (0.0124) | (0.0125) | (0.0123) | |
| No. of children 5–14 years in household | 0.0245*** | 0.0243*** | 0.0258*** | 0.0257*** | 0.0254*** | 0.0228*** | 0.0204*** |
| (0.00687) | (0.00716) | (0.00715) | (0.00713) | (0.00712) | (0.00726) | (0.00701) | |
| No. of children 15–17 years in household | −0.00899 | −0.0237 | −0.0214 | −0.0224 | −0.0177 | −0.0226 | −0.0101 |
| (0.0182) | (0.0187) | (0.0187) | (0.0187) | (0.0187) | (0.0187) | (0.0182) | |
| No. of adults 18–59 years in household | −0.00482 | −0.00358 | −0.00309 | −0.00316 | 0.00120 | −0.00484 | −0.00179 |
| (0.00590) | (0.00614) | (0.00621) | (0.00616) | (0.00624) | (0.00617) | (0.00606) | |
| No. of adults over age 60 in the household | −0.00290 | 0.00271 | 0.000351 | −0.000555 | 0.00683 | −0.00144 | 0.000629 |
| (0.0133) | (0.0139) | (0.0139) | (0.0139) | (0.0139) | (0.0139) | (0.0134) | |
| North‐east region | 0.0631*** | 0.0518** | 0.0657*** | 0.0609*** | 0.0615*** | 0.0607*** | 0.0463** |
| (0.0195) | (0.0206) | (0.0204) | (0.0204) | (0.0203) | (0.0204) | (0.0198) | |
| Total | 3,194 | 3,194 | 3,194 | 3,194 | 3,194 | 3,194 | 3,194 |
Note. ECD: early childhood development.
AME ± SE. Standard errors in parentheses.
P < 0.1.
P < 0.05.
P < 0.01.
4. DISCUSSION
This study is the first to construct a comprehensive multidimensional child poverty analysis for Cambodian children aged 0–59 months using the most recent 2014 CDHS. It applies UNICEF's rights‐based MODA toolbox to measure deprivation in the nutrition, health, ECD, water, sanitation, and housing dimensions, and in the combinations of these dimensions.
The findings reveal that in Cambodia, most children are multidimensionally deprived (78% having ≥2 deprivations), with a high average intensity of deprivation among the deprived children. The greatest overlap occurred among deprivation in nutrition, health, water, sanitation, and housing dimensions, suggesting that children who are not deprived in these dimensions, through access to safe water, adequate age‐specific nutrition, and suitable living environments, are less likely to be stunted. Not only are most Cambodian children multidimensionally deprived but they are particularly vulnerable because of the high intensity of their deprivation, especially in rural areas and among stunted children. Holding constant key background characteristics, being deprived in less than three dimensions had a consistently large negative marginal effect on the probability of being stunted. Maternal height under 145 cm was also strongly associated with child stunting, which is consistent with a pooled analysis of maternal height and child growth patterns from five birth cohorts in Brazil, Guatemala, India, the Philippines, and South Africa that showed a 1‐cm increase in maternal height predicts a 0.02 SD increase in conditional height of children at 2 years of age (Addo et al., 2013).
Although housing and water, sanitation and hygiene (WASH)‐related deprivations were concentrated in rural areas, the high nationwide deprivation headcount for nutrition suggests poor infant and young child feeding practices and inadequate growth are both prevalent in all regions of the country. Although the poorest children had the highest prevalence of nutrition deprivation and stunting, the fact that children in the highest wealth quintiles also exhibited these conditions indicates that nonresource barriers to good child nutrition are at play, which is consistent with other findings from Southeast Asia (Bloem et al., 2013). Infant and child undernutrition in Cambodia is attributed to inadequate macronutrient and micronutrient intake, including suboptimal breastfeeding and complementary feeding practices, and insufficient intake of complementary foods of animal origin (dairy, eggs, fish, and meat protein sources), compounded by the low nutrient density of traditional Cambodian diets (Anderson et al., 2008; Ministry of Health, Cambodia, 2011).
Although nutrition‐specific strategies that combine interventions before conception, during pregnancy, and in the first 2 years of life effectively improve child growth, the impact of reducing nutrition deprivation on stunting will be substantially higher in combination with nutrition‐sensitive interventions in WASH conditions, and to a lesser extent in health services, simultaneously implemented at the earliest possible stage of the child's life cycle, as supported by Bloem et al. (2013) and by evidence from South Asia in Aguayo and Menon (2016). Water, sanitation, and housing inadequacies have been widely studied as risk factors for child stunting, due to factors such as increased exposure to microbial and diarrhoeal disease (Cumming & Cairncross, 2016; Dearden et al., 2017). Children who have access to safe water, adequate age‐specific nutrition, and healthy housing conditions, simultaneously implemented at the earliest possible stage of the child's life, are less likely to be stunted. There is broad consensus that nutrition‐sensitive interventions such as “baby‐WASH interventions” to improve sanitation, water, and hygiene and thereby ensure a safe environment for infant feeding and development could be instrumental to eliminating stunting in low‐resource settings (Mbuya & Humphrey, 2016; Ngure et al., 2014).
The study builds on existing research on determinants of stunting in Cambodia and its socio‐economic burden on the population (Ikeda et al., 2013; Moench‐Pfanner et al., 2016; Zanello, Srinivasan, & Shankar, 2016). Our study underscores the linkages between child stunting and multidimensional deprivations, principally rooted in poverty.
5. LIMITATIONS
Our analysis focused on children with at least three chosen deprivations and therefore excludes the children with some scarcity who are also likely to be undernourished. Further, data were not representative at the provincial level, thereby limiting our ability to identify pockets of extreme child poverty and assess the role of provincial geography on stunting prevalence. The lack of data on characteristics of fathers limited the ability to understand paternal influences on child poverty and stunting such as associations between paternal age, occupation and decision‐making power, and child undernutrition observed in other studies (Deshmukh, Sinha, & Dongre, 2013). Finally, the analysis is limited to the sample of children covered by the CDHS which, by definition of a household survey, excludes some of the most vulnerable groups of children who are not living in regular households. Our analysis faces the common measurement limitations of studies that use a household survey with self‐reported data on child feeding practices, for which there is insufficient information to assess any bias in over or under‐reporting.
6. FUTURE RESEARCH
Several questions, not addressed in this analysis, are relevant to understanding the determinants of child stunting in Cambodia. Future analyses could benefit from studying the modifying role of child age at 1 or 2‐year intervals to discern which specific interventions would be most beneficial during these time points. Also, the likelihood of catch‐up growth and recovery from early stunting in Cambodian school‐age children should be examined. Finally, as social participation and environmental pollution are becoming more relevant in the Cambodian context, these dimensions should be considered for inclusion in future multidimensional analyses.
7. CONCLUSION
An understanding of the overlap of children's deprivations in early childhood is important for identifying opportunities for improved integration of high‐impact early childhood interventions. We have presented pathways for reducing stunting in Cambodia by addressing children's multiple and overlapping needs within a multidimensional framework. The high degree of overlap in nutrition, health, water, sanitation, and housing deprivations, particularly for rural and stunted children, supports the need for nutrition‐specific and nutrition‐sensitive interventions in health and living environments during the first 1,000 days. Helping families move out of poverty requires moving beyond solely increasing incomes towards greater social investments in human capital.
CONFLICTS OF INTEREST
The authors declare no conflict of interest. The opinions and statements in this article are those of the authors and may not reflect official policies or opinion of the organisations that they belong.
CONTRIBUTIONS
JK and CdN developed the study and analysed the data. JK, CdN, AL, and EP interpreted the data and drafted the manuscript. All authors reviewed and approved the final manuscript.
Supporting information
Data S1. Appendix
Table 6. Disaggregation of geographical regions
Table 7. Average marginal effects of the probability of being deprived in single and multiple dimensions, at the national level
Table 8. Average marginal effects of the probability of being deprived in single and multiple dimensions, in urban areas
Figure S2. Three‐way overlap of deprivations in the Nutrition, Sanitation and Housing dimensions in urban and rural areas. Source: Author's calculations, CDHS 2014.
Figure S3. Adjusted deprivation headcount (M0) of stunted and not stunted children at all deprivation cut‐off levels. Source: Author's calculations, CDHS 2014.
Figure S4. Two‐way overlap between stunting and multidimensional deprivation, with a threshold of k = 3 dimensions, at the national level. Source: Author's calculations, CDHS2014.
Figure S5. Deprivation incidence, stunting and the wealth index for children under age 5 years in rural and urban areas. Source: Author's calculations, CDHS 2014.
ACKNOWLEDGMENTS
We thank UNICEF Cambodia, Ministry of Planning of Cambodia, and the National Institute of Statistics of Cambodia for their participation in the consultative process to determine the analysis parameters.
Karpati J, de Neubourg C, Laillou A, Poirot E. Improving children's nutritional status in Cambodia: Multidimensional poverty and early integrated interventions. Matern Child Nutr. 2020;16(S2):e12731 10.1111/mcn.12731
Footnotes
The prevalence of stunting for children under five is reported by the World Bank as 49.2% in 2000 (2017).
Observed missing values were largely due to the sample design and did not show observable bias given the random sample selection process of the CDHS. Controlling for key individual and household characteristics including the geographical location, sex, and wealth quintiles of the child, we did not find statistically significant differences (P < 0.05) between the sample of children with missing values who were excluded from the analysis and those with nonmissing values.
H is the poverty headcount at each selected deprivation cut‐off, k. A measures the breadth of deprivation among those who are multidimensionally deprived according to the cut‐off k and is the sum of all deprivations among children counted as deprived, as a share of the sum of all possible deprivations among those deprived in at least k dimensions. As a product of H and A, M 0 calculates a poverty index that is sensitive to both the incidence and breadth of children's poverty.
The threshold of k = 3, with children deprived in three or more dimensions considered multidimensionally poor, was decided through a national consultative validation process to reflect the Cambodian context and to account for variance among the sample of children. We tested the same model using different values of k, and the outcomes remain robust.
The CDHS 2014 wealth index provides a proxy for measuring household expenditure and income to assess socio‐economic status, as explained by National Institute of Statistics et al. (2015).
See regional disaggregation by province in Table S6.
Variables such as the child's gender and household composition, although not statistically significant in the bivariate analysis, were kept as regressors due to conceptual relevance and possible importance in the multivariate regression analysis.
Anthropometric data on mothers and children were collected for a nationally representative smaller sample, making up 4,991 children under age five in the final sample used for all analyses involving the stunting variable.
The water, sanitation, and housing dimensions share certain variables used in the construction of the indicators with the construction of the wealth index and have therefore been omitted from this part of the analysis.
Tables S7 and S8 present the national and urban‐level results of Model 3a–g.
Due to the large volume of analytical output, not all potential deprivation overlaps can be reported within the scope of this article.
REFERENCES
- Addo, O. Y. , Stein, A. D. , Fall, C. H. , Gigante, D. P. , Guntupalli, A. M. , Horta, B. L. , … Martorell, R. (2013). Maternal height and child growth patterns. The Journal of Pediatrics, 163(2), 549–554. 10.1016/j.jpeds.2013.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aguayo, V. M. , & Menon, P. (2016). Stop stunting: Improving child feeding, women's nutrition and household sanitation in South Asia. Maternal & Child Nutrition, 12(Suppl 1), 3–11. 10.1111/mcn.12283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alkire, S. , & Foster, J. (2011). Counting and multidimensional poverty measurement. Journal of Public Economics, 95(7–8), 476–487. 10.1016/j.jpubeco.2010.11.006 [DOI] [Google Scholar]
- Alkire, S. , & Roche, J. M. (2012). Beyond headcount: Measures that reflect the breadth and components of child poverty In Minujin A., & Nandy S. (Eds.), Global child poverty and well‐being: Measurement, concepts, policy and action (pp. 103–134). Bristol: Policy Press. [Google Scholar]
- Alkire, S. , & Santos, M. E. (2010). Acute multidimensional poverty: A new index for developing countries. Working paper/Oxford Poverty & Human Development Initiative: Vol. 38. Oxford: Oxford Poverty & Human Development Initiative. Retrieved from http://www.ophi.org.uk/wp‐content/uploads/ophi‐wp38.pdf
- Anderson, V. P. , Cornwall, J. , Jack, S. , & Gibson, R. S. (2008). Intakes from non‐breastmilk foods for stunted toddlers living in poor urban villages of Phnom Penh, Cambodia, are inadequate. Maternal & Child Nutrition, 4(2), 146–159. 10.1111/j.1740-8709.2007.00120.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bloem, M. W. , Pee, S. D. , Le Hop, T. , Khan, N. C. , Laillou, A. , Minarto, … Theary, C. (2013). Key strategies to further reduce stunting in Southeast Asia: Lessons from the ASEAN countries workshop. Food and Nutrition Bulletin, 34(Suppl 2), S8–S16. 10.1177/15648265130342S103 [DOI] [PubMed] [Google Scholar]
- Campisi, S. C. , Cherian, A. M. , & Bhutta, Z. A. (2017). World perspective on the epidemiology of stunting between 1990 and 2015. Hormone Research in Paediatrics. Advance Online Publication. 88, 70–78. 10.1159/000462972 [DOI] [PubMed] [Google Scholar]
- Cumming, O. , & Cairncross, S. (2016). Can water, sanitation and hygiene help eliminate stunting? Current evidence and policy implications. Maternal & Child Nutrition, 12(Suppl 1), 91–105. 10.1111/mcn.12258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Neubourg, C. , Chai, J. , de Milliano, M. , Plavgo, I. , & Wei, Z. (2013). Step‐by‐step guidelines to the multiple overlapping deprivation analysis (MODA). (Innocenti Working Paper No. 2012‐10). Florence.
- De Neubourg, C. , de Milliano, M. , & Plavgo, I. (2014). Lost (in) dimensions: Consolidating progress in multidimensional poverty research (Innocenti Working Paper No. 2014‐04). Florence.
- De Neubourg, E. , & de Neubourg, C. (2012). The impact of malnutrition and post traumatic stress disorder on the performance of working memory in children (UNU‐MERIT Working Paper Series). Maastricht.
- de Onis, M. , & Branca, F. (2016). Childhood stunting: A global perspective. Maternal & Child Nutrition, 12(Suppl 1), 12–26. 10.1111/mcn.12231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dearden, K. A. , Schott, W. , Crookston, B. T. , Humphries, D. L. , Penny, M. E. , & Behrman, J. R. (2017). Children with access to improved sanitation but not improved water are at lower risk of stunting compared to children without access: A cohort study in Ethiopia, India, Peru, and Vietnam. BMC Public Health, 17(1), 110 10.1186/s12889-017-4033-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deshmukh, P. R. , Sinha, N. , & Dongre, A. R. (2013). Social determinants of stunting in rural area of Wardha, Central India. Medical Journal Armed Forces India, 69(3), 213–217. 10.1016/j.mjafi.2012.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon, D. , Nandy, S. , Pantazis, C. , Pemberton, S. , & Townsend, P. (2003). Child poverty in the developing world In Studies in poverty, inequality and social exclusion. Bristol: Policy Press. [Google Scholar]
- Harper, C. , Marcus, R. , & Moore, K. (2003). Enduring poverty and the conditions of childhood: Lifecourse and intergenerational poverty transmissions. Chronic Poverty and Development Policy, 31(3), 535–554. 10.1016/S0305-750X(03)00010-X [DOI] [Google Scholar]
- Hulme, D. , & Shepherd, A. (2003). Conceptualizing chronic poverty. World Development, 31(3), 403–423. 10.1016/S0305-750X(02)00222-X [DOI] [Google Scholar]
- Ikeda, N. , Irie, Y. , & Shibuya, K. (2013). Determinants of reduced child stunting in Cambodia: Analysis of pooled data from three demographic and health surveys. Bulletin of the World Health Organization, 91(5), 341–349. 10.2471/BLT.12.113381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khasnutdinova, S. L. , & Grjibovski, A. M. (2010). Prevalence of stunting, underweight, overweight and obesity in adolescents in Velsk district, north‐west Russia: A cross‐sectional study using both international and Russian growth references. Public Health, 124(7), 392–397. 10.1016/j.puhe.2010.03.017 [DOI] [PubMed] [Google Scholar]
- Mbuya, M. N. , & Humphrey, J. H. (2016). Preventing environmental enteric dysfunction through improved water, sanitation and hygiene: An opportunity for stunting reduction in developing countries. Maternal & Child Nutrition, 12(Suppl 1), 106–120. 10.1111/mcn.12220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of Health, Cambodia . (2011). National policy and guidelines for micronutrient supplementation to prevent and control deficiencies in Cambodia. Cambodia: Phnom Penh. [Google Scholar]
- Ministry of Planning, Cambodia, & National Institute of Statistics . (2017). Population project of Cambodia 2013–2023: Based on Cambodia Inter‐Censal Population Survey 2013 and Cambodia Demographic and Health Survey 2014. Phnom Penh. Retrieved from http://hismohcambodia.org/public/fileupload/PopulationProjection_2023.pdf
- Minujin, A. , Delamonica, E. , Davidziuk, A. , & Gonzalez, E. D. (2016). The definition of child poverty: A discussion of concepts and measurements. Environment and Urbanization, 18(2), 481–500. 10.1177/0956247806069627 [DOI] [Google Scholar]
- Moench‐Pfanner, R. , Silo, S. , Laillou, A. , Wieringa, F. , Hong, R. , Hong, R. , … Bagriansky, J. (2016). The economic burden of malnutrition in pregnant women and children under 5 years of age in Cambodia. Nutrients, 8(5). 10.3390/nu8050292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute of Statistics, Directorate General for Health, & ICF International . (2015). Cambodia Demographic and Health Survey 2014. Phnom Penh, Cambodia. Retrieved from National Institute of Statistics (NIS); Directorate General for Health; ICF International (ICF) website: http://dhsprogram.com/pubs/pdf/FR312/FR312.pdf
- National Institute of Statistics, Directorate General for Health, & ORC Macro . (2001). Cambodia Demographic and Health Survey , 2000: Cambodia Demographic and Health Survey 2000 Phnom Penh, Cambodia: National Institute of Statistics; Directorate General for Health; ORC Macro. Retrieved from http://dhsprogram.com/pubs/pdf/FR124/FR124.pdf
- Ngure, F. M. , Reid, B. M. , Humphrey, J. H. , Mbuya, M. N. , Pelto, G. , & Stoltzfus, R. J. (2014). Water, sanitation, and hygiene (WASH), environmental enteropathy, nutrition, and early child development: Making the links. Annals of the New York Academy of Sciences, 1308, 118–128. 10.1111/nyas.12330 [DOI] [PubMed] [Google Scholar]
- Perignon, M. , Fiorentino, M. , Kuong, K. , Burja, K. , Parker, M. , Sisokhom, S. , … Wieringa, F. T. (2014). Stunting, poor iron status and parasite infection are significant risk factors for lower cognitive performance in Cambodian school‐aged children. PLoS One, 9(11), e112605 10.1371/journal.pone.0112605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rees, N. (2016). Clear the air for the children: The impact of air pollution on children. New York: United Nations Children's Fund. [Google Scholar]
- Sunil, T. S. , & Sagna, M. (2015). Decomposition of childhood malnutrition in Cambodia. Maternal & Child Nutrition, 11(4), 973–986. 10.1111/mcn.12029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The World Bank . (2017). World development indicators. Retrieved from https://data.worldbank.org/indicator/SH.STA.STNT.ZS?locations=KH&page=4
- UN General Assembly . (1989). Convention on the Rights of the Child, 20 November 1989. Retrieved from http://www.ohchr.org/EN/ProfessionalInterest/Pages/CRC.aspx [PubMed]
- UN‐HABITAT . (2007). Enhancing urban safety and security: Global report on human settlements 2007/ United Nations human settlements programme. London: Earthscan. [Google Scholar]
- UNICEF Office of Research . (2014). CC‐MODA analysis for Cambodia (DHS 2010–2011). Retrieved from www.unicef‐irc.org/MODA.
- World Health Organization . (2008). Indicators for assessing infant and young child feeding practices: Conclusions of a consensus meeting held 6–8 November 2007 in Washington D.C., USA. Washington, D.C.: World Health Organization (WHO).
- World Health Organization, & United Nations Children's Fund . (2017). Progress on drinking water, sanitation and hygiene: 2017 update and SDG baselines. Geneva. [Google Scholar]
- Zanello, G. , Srinivasan, C. S. , & Shankar, B. (2016). What explains Cambodia's success in reducing child stunting‐2000‐2014? PLoS One, 11(9), e0162668 10.1371/journal.pone.0162668 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Appendix
Table 6. Disaggregation of geographical regions
Table 7. Average marginal effects of the probability of being deprived in single and multiple dimensions, at the national level
Table 8. Average marginal effects of the probability of being deprived in single and multiple dimensions, in urban areas
Figure S2. Three‐way overlap of deprivations in the Nutrition, Sanitation and Housing dimensions in urban and rural areas. Source: Author's calculations, CDHS 2014.
Figure S3. Adjusted deprivation headcount (M0) of stunted and not stunted children at all deprivation cut‐off levels. Source: Author's calculations, CDHS 2014.
Figure S4. Two‐way overlap between stunting and multidimensional deprivation, with a threshold of k = 3 dimensions, at the national level. Source: Author's calculations, CDHS2014.
Figure S5. Deprivation incidence, stunting and the wealth index for children under age 5 years in rural and urban areas. Source: Author's calculations, CDHS 2014.


