Introduction
Lipodermatosclerosis (LDS) is a sclerosing panniculitis that commonly occurs on the legs in middle-aged women and is associated with chronic venous insufficiency. The spectrum of clinical presentations includes an acute inflammatory phase and a chronic fibrotic phase.1 Acute inflammation in LDS can mimic cellulitis and may be very painful; the chronic phase is characterized by hyperpigmentation and hardening of the skin and subcutaneous tissue. The pathogenesis is thought to be associated with superficial venous hypertension, resulting in fibrin deposition and tissue hypoxia, leading to increased levels of transforming growth factor β with subsequent type 1 collagen deposition.2 Management of LDS is similar to that of chronic venous insufficiency and involves compression therapy and leg elevation. Oral agents such as pentoxifylline, hydroxychloroquine, and others are also found to be helpful in some cases.3
May-Thurner syndrome (MTS) is a common but underdiagnosed condition in which the left common iliac vein is compressed between the overlying right common iliac artery and the lumbar vertebrae. Although there are other locations in the body in which an artery apposes a vein, the unique positioning of the iliac vein between the iliac artery and lumbar vertebral body leads to compression. Chronic compression may lead to endovascular intimal proliferation and venous spur formation, leading to irreversible luminal narrowing. Patients with venous spurs may remain asymptomatic for an extended period; however, endoluminal narrowing may eventually lead to iliac venous obstruction and contribute to severe symptoms of chronic venous disease of the left lower extremity. Rare cases of MTS affecting the right iliac vein have also been reported in the literature.4 We present a case of a 63-year-old woman with severe LDS refractory to conventional therapy, found to have MTS, and treated with an endovascular intervention that led to dramatic improvement of her symptoms.
Case report
A 63-year-old woman with a history of hypertension and diabetes was evaluated by the inpatient dermatology service for a 3-week history of severe left lower extremity swelling, tenderness, and evolving erythema and hyperpigmentation. The patient had a 10-year history of venous insufficiency, left lower extremity swelling, and discomfort. She had undergone endovenous ablation of the left great saphenous vein several years before with some symptom improvement at the time; however, her symptoms had recently worsened. On admission, physical examination of the left leg found significant hyperpigmentation, erythema, tenderness, and edema (Fig 1) along with intact strength and sensation and strong distal pulses. Venous duplex studies found no deep venous thromboses, minimal deep venous reflux, and some superficial varicose veins. The patient was treated for acute LDS with a prednisone taper and completed a course of antibiotics for possible cellulitis, with improvement during her hospital stay.
Fig 1.
A, Initial clinical appearance of the left lower extremity. B, Clinical appearance of the left lower extremity 1 year after left iliac vein venoplasty and stenting.
At outpatient follow-up, the patient reported continued severe left lower extremity pain and swelling and poor ambulatory function. She did not tolerate compression therapy because of pain. She completed her prednisone course and was started on pentoxifylline. She was referred to a vascular surgeon who recommended a venogram study be performed by the interventional radiology department to assess the venous drainage of her left lower extremity.
She subsequently required another hospitalization for severe left lower extremity pain, swelling, and erythema greatly affecting her ability to ambulate. She improved with leg elevation, antibiotics, and prednisone. Hydroxychloroquine was added to her regimen of pentoxifylline, 400 mg 3 times a day. Notably, during both of her admissions, she had no fevers, normal white blood cell counts, and negative blood cultures. Magnetic resonance imaging of the left lower extremity found diffuse mild subcutaneous edema and fluid and skin thickening predominantly in the mid to lower calf, both concerning for possible cellulitis.
Lower extremity and inferior vena cava venography and intravascular ultrasound scan by the interventional radiology department found left iliac vein compression consistent with MTS. The patient underwent left common and external iliac vein angioplasty and stenting (Fig 2). Subsequently, the patient reported significant improvement in her left lower extremity swelling and pain and was able to ambulate farther without the assistance of her walker. In the year and a half since her intervention, she has not suffered any further acute inflammatory episodes requiring antibiotics or systemic steroids. She continues to have mild swelling of her left leg with improved hyperpigmentation and chronic sclerotic changes.
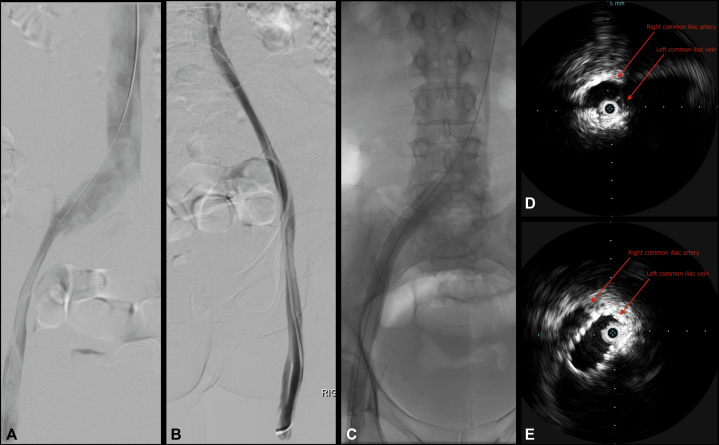
Fig 2.
A, Prone left iliac and inferior vena cava digital subtraction venography shows anteroposterior compression of left common iliac vein. B, Contralateral right iliac digital subtraction venography shows normal caliber. C, Native left iliac venography after venoplasty and stenting. D, Preintervention intravascular ultrasound scan shows May-Thurner compression of left common iliac vein by overlying right common iliac artery. E, Poststenting intravascular ultrasound scan shows improved left common iliac vein caliber.
Discussion
This is a case of LDS with recurrent severe acute episodes, found to be associated with MTS with significant improvement from an endovascular intervention. Patients with MTS may have a variety of clinical presentations, ranging from asymptomatic to recurrent deep vein thrombosis.5 Patients with acute symptoms of MTS may present with lower extremity venous thrombosis, whereas chronic symptoms such as swelling and pain may follow a more insidious course. Patients with chronic symptoms may present as in chronic venous insufficiency, with leg swelling, pain, LDS, varicose veins, or superficial thrombophlebitis. This patient presented with severe, recurrent, unilateral inflammatory symptoms mimicking recurrent cellulitis. Interestingly, she showed minimal signs of venous hypertension on duplex ultrasound scan. A proximal outflow obstruction thus cannot be ruled out by a normal venous duplex ultrasound study.
It has been reported that patients with severe symptoms of chronic venous disease have a higher incidence of compression of the iliocaval system when studied with intravascular ultrasound scan6; patients may more commonly present with nonthrombotic iliac vein lesions (including venous webs and spurs). A single-center prospective observational study found that limbs with LDS or with healed or active venous ulceration, especially in the left limb, had a high prevalence of iliocaval venous obstruction.7 The population prevalence of MTS has yet to be defined, although one study of asymptomatic patients found a prevalence of common iliac vein compression in up to 24%, most commonly caused by compression between the common iliac artery and lumbar vertebral body.8 This finding has implications for patients suffering from either LDS or chronic venous insufficiency, particularly when disease is limited unilaterally to the left lower extremity. In the case of a patient with severe and refractory left-sided LDS, it is important to consider the possibility of the presence of MTS.
Footnotes
Funding sources: None.
Conflicts of interest: None disclosed.
References
- 1.Kirsner R.S., Pardes J.B., Eaglstein W.H., Falanga V. The clinical spectrum of lipodermatosclerosis. J Am Acad Dermatol. 1993;28(4):623–627. doi: 10.1016/0190-9622(93)70085-8. [DOI] [PubMed] [Google Scholar]
- 2.Miteva M., Romanelli P., Kirsner R.S. Lipodermatosclerosis. Dermatol Ther. 2010;33:375–388. doi: 10.1111/j.1529-8019.2010.01338.x. [DOI] [PubMed] [Google Scholar]
- 3.Chaowattanapanit S., Choonhakarn C. Lipodermatosclerosis: improvement noted with hydroxychloroquine and pentoxifylline. J Am Acad Dermatol. 2012;66(6):1013–1014. doi: 10.1016/j.jaad.2011.11.942. [DOI] [PubMed] [Google Scholar]
- 4.Abboud G., Midulla M., Lions C. “Right-sided” May-Thurner syndrome. Cardiovasc Intervent Radiol. 2009;33(5):1056–1059. doi: 10.1007/s00270-009-9654-z. [DOI] [PubMed] [Google Scholar]
- 5.Esposito A., Charisis N., Kantarowsky A., Uhl J.F., Lapropoulos N. A comprehensive review of the pathophysiology and clinical importance of iliac vein obstruction. Eur J Endovasc Surg. 2020;60(1):118–125. doi: 10.1016/j.ejvs.2020.03.020. [DOI] [PubMed] [Google Scholar]
- 6.Raju S., Neglen P. High prevalence of nonthrombotic iliac vein lesions in chronic venous disease: a permissive role in pathogenicity. J Vasc Surg. 2006;44:136–143. doi: 10.1016/j.jvs.2006.02.065. discussion 144. [DOI] [PubMed] [Google Scholar]
- 7.Sermsathanasawadi N., Pruekprasert K., Pitaksantayothin W. Prevalence, risk factors, and evaluation of iliocaval obstruction in advanced chronic venous insufficiency. J Vasc Surg Venous Lymphat Disord. 2019;7:441–447. doi: 10.1016/j.jvsv.2018.10.021. [DOI] [PubMed] [Google Scholar]
- 8.Kibbe M.R., Ujiki M., Goodwin A.L., Eskandari M., Yao J., Matsumara J. Iliac vein compression in an asymptomatic patient population. J Vasc Surg. 2004;39(5):937–943. doi: 10.1016/j.jvs.2003.12.032. [DOI] [PubMed] [Google Scholar]