Abstract
Background Microvascular decompression (MVD) has been widely accepted as a definitive therapy for primary trigeminal neuralgia (TN). However, some patients may not experience relief of TN symptoms following surgery. In this study, the findings of redo MVD are discussed.
Methods Between 2015 and 2017, 205 patients with primary TN underwent MVD surgery in Shanghai Tongren Hospital. Among these patients, 187 had immediate complete relief of symptoms, 8 improved apparently, and 10 reported no symptom relief. Of the 10 patients without relief, 6 underwent reoperation within 5 days, 2 underwent reoperation 3 months after the first procedure, and 2 refused to undergo reoperation.
Results The symptoms of those patients who received reoperation disappeared immediately after the surgery. In the second operations, new conflict sites at the motor roots were found in five cases. The real offending vessels were the superior cerebellar artery (SCA) or branch of the SCA in seven cases and the petrosal vein in one case. The nerve was not decompressed completely in either of the two cases. At the 12-month follow-up, no recurrence was found. For the other two patients who did not have reoperation, their symptom persisted. Postoperative complications showed no significant differences between the first and second operations.
Conclusion Compression of the motor roots might be one of the causes of TN. Thorough exploration of both sensory and motor roots of the trigeminal nerve is essential to performing a successful MVD operation. Early reoperation for resistant TN after MVD does not increase the incidence of complications.
Keywords: trigeminal neuralgia, microvascular decompression, reoperation, motor root, offending vessel
Introduction
Microvascular decompression (MVD) has been widely accepted as an effective treatment for trigeminal neuralgia (TN) because it is less invasive and preserves vascular and neural functions. 1 2 3 However, the cure rate of MVD for TN has varied from 79.6 to 89.1%. 4 5 6 7 Not all patients experience relief of TN symptoms after MVD. Some authors believe that there may still be “delay relief” within 1 year of surgery. 8 Yet, the factors that contribute to the “delay relief” have not been well studied. To improve MVD surgery and increase the cure rate, re-explorations were performed for patients who did not have immediate relief. The intraoperative findings and experiences were reviewed in this study.
Methods
Patients
From January 2015 to June 2017, 205 idiopathic TN patients who underwent MVD at the Department of Neurosurgery, Shanghai Tongren Hospital were included in this study. All patients were treated by MVD. The patients who underwent reoperation due to the unimproved symptoms were the focus of this study. All the patients were followed up for at least 12 months.
Surgical Procedure
The operation was performed via a suboccipital retrosigmoid approach. After the dura was opened, cerebrospinal fluid (CSF) was drained slowly. The cerebellar-fissures approach was adopted to avoid the petrosal vein (PV) and the arachnoid membranes were opened sharply. Then, the entire trigeminal nerve root was exposed. The neurovascular relationship was carefully studied and the offending vessel was removed. Small pieces of shredded Teflon sponge were placed between the vessel and the trigeminal nerve.
For the patients who underwent reoperation, the previous conflict site was double checked. Then, the whole trigeminal nerve root was dissected thoroughly (both motor and sensory roots), and any artery relevant to the nerve was removed. A Teflon sponge was placed between them.
Follow-up and Outcome Evaluation
All patients were evaluated by either an interview in the clinic or telephone interview after discharge. A comprehensive analysis of surgical outcomes, including complications, was performed at 1 day, 3 months, and 6 months postoperation. The Barrow Neurological Institute (BNI) pain intensity scale was used 9 ( Table 1 ). The efficiency of the surgery was evaluated by this scale: excellent (BNI pain score I), good (BNI pain scores II and III), and poor (BNI pain scores IV and V).
Table 1. Barrow Neurological Institute pain intensity score.
| Score | |
|---|---|
| I | No trigeminal pain, no medication |
| II | Occasional pain, not requiring medication |
| III | Some pain, adequately controlled with medication |
| IV | Some pain, not adequately controlled with medication |
| V | Severe pain/no pain relief |
Source : Adapted from Rogers et al. 9
Results
Surgical Outcome
Of all the 205 patients, 187 had immediate complete relief (excellent), 8 improved apparently (good), and 10 reported no relief (poor). Among the 10 patients without relief, 6 underwent reoperation within 5 days, 2 underwent reoperation 3 months after the first procedure, and 2 were observed (refused to undergo reoperation). After reoperation, all of the eight patients had an “excellent” outcome. For the two patients who refused to undergo reoperation, their symptoms persisted.
Intraoperative findings in Reoperation
The eight patients who underwent reoperation were the focus of this study. The demographic data are shown in Table 2 . In the previous operation, the superior cerebellar artery (SCA) had been regarded as the offending artery in five patients, the PV in two patients, and the anterior inferior cerebellar artery in one patient. The conflict site had been believed to be in the caudal area of the trigeminal nerve in five patients and in the dorsal area in three patients.
Table 2. Clinical features of patients who underwent second MVD surgery.
| No. | Sex | Age (y) | Duration (y) | Side | Division affected | Final outcome | Complication | Follow-up (mo) |
|---|---|---|---|---|---|---|---|---|
| 1 | M | 45 | 6 | L | V1 | Excellent | None | 12 |
| 2 | M | 69 | 3 | R | V2 | Excellent | None | 18 |
| 3 | F | 76 | 8 | R | V1, V2 | Excellent | None | 12 |
| 4 | F | 55 | 3 | R | V2, V3 | Excellent | None | 15 |
| 5 | F | 63 | 10 | L | V1, V2, V3 | Excellent | Numbness | 24 |
| 6 | F | 51 | 5 | L | V3 | Excellent | None | 18 |
| 7 | M | 66 | 6 | R | V2, V3 | Excellent | None | 15 |
| 8 | F | 57 | 0.5 | L | V2, V3 | Excellent | Dizziness | 24 |
Abbreviation: MVD, microvascular decompression.
In the second operation, new conflict sites at the motor roots were found in five cases. The real offending vessels were the SCA or a branch of the SCA in seven cases and the PV in one case. The nerve was not decompressed completely in two cases because not enough Teflon was inserted ( Table 3 ).
Table 3. The intraoperative findings for patients who underwent second MVD surgery.
| No. | Finding at first MVD | Finding at second MVD | Failure reason | ||
|---|---|---|---|---|---|
| Offending vessel | Conflict site | Offending vessel | Conflict site | ||
| 1 | SCA | Caudal of the fifth (sensory root) | Branch of SCA | Ventral of the fifth (motor root) | Zone missed |
| 2 | SCA | Caudal of the fifth (sensory root) | SCA | Caudal of the fifth (sensory root) | Incomplete decompression |
| 3 | PV | Dorsal of the fifth (sensory root) | PV | Dorsal of the fifth (sensory root) | Incomplete decompression |
| 4 | SCA | Caudal of the fifth (sensory root) | Branch of SCA | Rostral of the fifth (motor root) | Zone missed |
| 5 | AICA | Dorsal of the fifth (sensory root) | SCA | Rostral of the fifth (motor root) | Zone missed |
| 6 | SCA | Caudal of the fifth (sensory root) | Branch of SCA | Rostral of the fifth (motor root) | Zone missed |
| 7 | SCA | Caudal of the fifth (sensory root) | SCA | Rostral of the fifth (motor root) | Zone missed |
| 8 | PV | Dorsal of the fifth (sensory root) | Branch of SCA | Rostral of the fifth (sensory root) | Zone missed |
Abbreviations: AICA, anterior inferior cerebellar artery; MVD, microvascular decompression; PV, petrosal vein(s); SCA, superior cerebellar artery.
Complications
Of all the 205 cases, postoperative complications contained facial numbness in six, dizziness/vertigo in eight, partial hearing loss in three, and CSF leakage in two. There was no mortality or intracranial infection noted in any of the cases ( Table 4 ). At the 12-month follow-up, no recurrence was found.
Table 4. Comparison of transient postoperative complications between the patients who underwent MVD and re-MVD.
| Symptoms | First operation ( n ) | Second operation ( n ) | p -Value |
|---|---|---|---|
| Numbness | 5 | 1 | 0.2074 |
| Dizziness/vertigo | 7 | 1 | 0.2677 |
| Hearing loss | 3 | 0 | 1.0000 |
| CSF leakage | 2 | 0 | 1.0000 |
Abbreviation: MVD, microvascular decompression.
Discussion
Vascular compression of the trigeminal nerve is the most common cause of primary TN. 10 11 Based on this hypothesis, MVD has been widely accepted as the only etiological therapy for TN with a high success rate and low risk of complications. 6 However, there is a large difference between the efficiencies reported by various hospitals. Some patients still suffer from residual or recurrent pain. According to previous reports, the main causes of recurrence include: inadequate separation of vessel and nerve, adhesion of the interposed Teflon material, and Teflon-induced granuloma. 12 13 Re-MVD has been previously reported to have good success in managing recurrent TN. 12 13 14 In this study, wrong identification of the offending vessels, neglect of the conflict site, and inadequate separation of vessel and nerve are the main causes of the failed surgeries. No Teflon shifting, adhesion, or shedding was found in this series, probably because of the early reoperation ( Fig. 1 ).
Fig. 1.
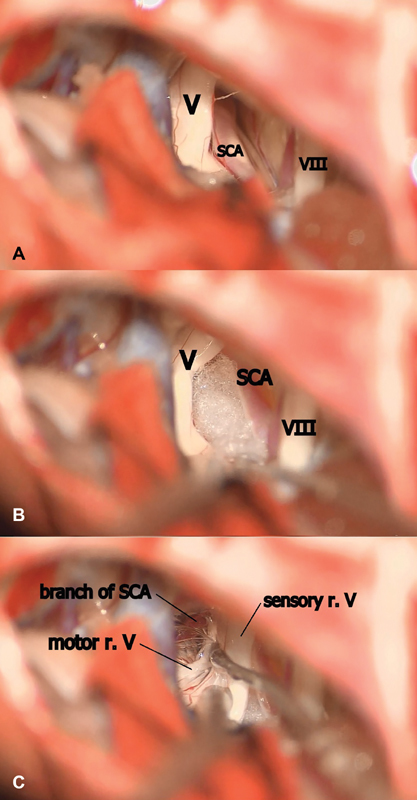
Intraoperative findings in an early redo MVD for TN. ( A) During the first MVD surgery, SCA was found to be compressing the caudal area of the trigeminal nerve (V). ( B) A Teflon sponge was placed between the offending vessel and the trigeminal nerve. ( C) As the symptoms persisted, the patient underwent redo MVD 3 days later. During the reoperation, the trigeminal nerve was fully exposed. A new conflict site at the motor branch of trigeminal nerve compressed by a branch of the SCA was found. MVD, microvascular decompression; SCA, superior cerebellar artery; TN, trigeminal neuralgia; V, trigeminal nerve; VIII, acoustic nerve.
The trigeminal nerve is formed by motor and sensory roots. It has been wildly believed that the compression of the sensory root was the main cause of TN. However, in this study, we found new conflict sites at the motor root in five of the eight patients who underwent re-MVD. After decompression of the motor root in the second operation, symptoms were completely relieved. Therefore, we wondered if TN can also be caused by the compression of the motor root.
To address this question, we have reviewed the microscopic anatomy of the trigeminal nerve. Generally, there are one or multiple motor roots. They emerge from the pons anterosuperomedial to the entry point of the large sensory root. 15 16 When there are more than one motor roots, the most cephalic motor root is defined as the superior motor root and the remaining ones are defined as inferior motor roots, which are also called “accessory fibers.” 17 Numerous communicants were found between the sensory root and both of these motor roots. 15 16 It was even found that some accessory fibers join the sensory root instead of the superior motor root. 16 17 Young reported that afferent sensory fibers were found in motor roots and these fibers may form accessory sensory roots in 12 to 20% of cases. 18 19 It was reported that touch sensation remained after rhizotomy of the sensory root at the pons in some cases. 15 16 This concept might explain why patients with TN still suffered from pain after decompression of the sensory roots of the trigeminal nerve in this study. Considering that any compressions along the full lengths of the trigeminal nerve roots might result in TN, it was found that the motor roots had an even higher chance of neurovascular contacts than the sensory root by magnetic resonance imaging studies. 20
To avoid missing the conflict site and offending vessels, “five-zone exploration” has been proposed by Feng et al. 21 According to this theory, the trigeminal nerve root at the cisternal segment can be divided into five zones (from Meckel's cave to the pons): Zone 1 is located at the rostral area of the root entry zone (REZ). Zone 2 is located at the caudal area of the REZ. Zone 3 is located at the ventral area of the fifth nerve and Zone 4 is located at the dorsal of the nerve. According to this method, a new conflict site was found during the second exploration in the six cases in this study. The offending vessels were found at the rostral area of the trigeminal nerve in five of these six cases. After complete decompression of the sensory and motor rootlets, the patients' symptoms disappeared. Thus, we propose that both sensory and motor roots should be explored during MVD surgery. Any portion of the trigeminal root can be the conflict site and any suspicious vessels compressing the trigeminal nerve should be removed. 21
Some authors believe that delayed relief might occur from several months to 1 year. 8 However, the rate of delayed relief is very rare in our experience. In the present study of 205 TN patients, no delayed relief was observed. On the contrary, the eight patients who underwent re-MVD had excellent outcome after the second operation. Furthermore, the incidence of complications after re-MVD was not increased. Of course, reoperation is not suitable for all patients, although it has previously been reported as having good outcomes in management of recurrent TN. 14 Before re-MVD, the video of the previous operation should be reviewed repeatedly and suspicious causes of failure should be discussed. In order not to increase surgical complications, the manipulation should be more tenderly and more carefully during the re-MVD. All the Teflon was removed to find the real offending vessel and conflict site in this study. The entire nerve root was explored, especially the rostral and ventral parts of the trigeminal nerve near Meckel's cave. Even very small branches of the SCA could be the offending vessels. If no clear compression or distortion was found at the time of re-exploration, neurolysis was suggested in addition to the MVD. 14
Conclusion
The compression of the motor roots might be one of the causes of TN. Thorough exploration of both sensory and motor roots of the trigeminal nerve is essential to performing a successful MVD operation. Early reoperation for resistant TN after MVD does not increase the incidence of complications.
Funding Statement
Funding This study was supported by the grant from Shanghai Municipal Commission of Health and Family Planning (201540299, to Li Xinyuan) and by Medical Engineering Cross Fund of Shanghai Jiaotong University (YG2016MS67, to Li Xinyuan).
Conflict of Interest This article has not been published or presented elsewhere in part or in entirety and is not under consideration by another journal. All study participants provided informed consent, and the study design was approved by the appropriate ethics review board. We have read and understood your journal's policies, and we believe that neither the article nor the study violates any of these. There are no conflicts of interest to declare.
Ethical Approval
The clinical data were retrospectively reviewed. For this type of study, formal consent is not required.
These authors contributed equally to this study.
References
- 1.Sindou M, Leston J M, Decullier E, Chapuis F.Microvascular decompression for trigeminal neuralgia: the importance of a noncompressive technique--Kaplan-Meier analysis in a consecutive series of 330 patients Neurosurgery 2008630402341–350., discussion 350–351 [DOI] [PubMed] [Google Scholar]
- 2.Sekula R F, Jr, Frederickson A M, Jannetta P J, Quigley M R, Aziz K M, Arnone G D. Microvascular decompression for elderly patients with trigeminal neuralgia: a prospective study and systematic review with meta-analysis. J Neurosurg. 2011;114(01):172–179. doi: 10.3171/2010.6.JNS10142. [DOI] [PubMed] [Google Scholar]
- 3.Zhong J, Li S T, Zhu J. A clinical analysis on microvascular decompression surgery in a series of 3000 cases. Clin Neurol Neurosurg. 2012;114(07):846–851. doi: 10.1016/j.clineuro.2012.01.021. [DOI] [PubMed] [Google Scholar]
- 4.Barker F G, II, Jannetta P J, Bissonette D J, Larkins M V, Jho H D. The long-term outcome of microvascular decompression for trigeminal neuralgia. N Engl J Med. 1996;334(17):1077–1083. doi: 10.1056/NEJM199604253341701. [DOI] [PubMed] [Google Scholar]
- 5.Zhang X, Xu L, Zhao H. Long-term efficacy of nerve combing for patients with trigeminal neuralgia and failed prior microvascular decompression. World Neurosurg. 2017;108:711–715. doi: 10.1016/j.wneu.2017.09.081. [DOI] [PubMed] [Google Scholar]
- 6.Xia L, Zhong J, Zhu J. Effectiveness and safety of microvascular decompression surgery for treatment of trigeminal neuralgia: a systematic review. J Craniofac Surg. 2014;25(04):1413–1417. doi: 10.1097/SCS.0000000000000984. [DOI] [PubMed] [Google Scholar]
- 7.Chakravarthi P S, Ghanta R, Kattimani V. Microvascular decompression treatment for trigeminal neuralgia. J Craniofac Surg. 2011;22(03):894–898. doi: 10.1097/SCS.0b013e31821a07b7. [DOI] [PubMed] [Google Scholar]
- 8.Sandell T, Eide P K.Effect of microvascular decompression in trigeminal neuralgia patients with or without constant pain Neurosurgery 2008630193–99., discussion 99–100 [DOI] [PubMed] [Google Scholar]
- 9.Rogers C L, Shetter A G, Fiedler J A, Smith K A, Han P P, Speiser B L. Gamma knife radiosurgery for trigeminal neuralgia: the initial experience of the Barrow Neurological Institute. Int J Radiat Oncol Biol Phys. 2000;47(04):1013–1019. doi: 10.1016/s0360-3016(00)00513-7. [DOI] [PubMed] [Google Scholar]
- 10.Jannetta P J. Arterial compression of the trigeminal nerve at the pons in patients with trigeminal neuralgia. 1967. J Neurosurg. 2007;107(01):216–219. doi: 10.3171/JNS-07/07/0216. [DOI] [PubMed] [Google Scholar]
- 11.Petty P G, Southby R, Siu K. Vascular compression: cause of trigeminal neuralgia. Med J Aust. 1980;1(04):166–167. doi: 10.5694/j.1326-5377.1980.tb134736.x. [DOI] [PubMed] [Google Scholar]
- 12.Gu W, Zhao W. Microvascular decompression for recurrent trigeminal neuralgia. J Clin Neurosci. 2014;21(09):1549–1553. doi: 10.1016/j.jocn.2013.11.042. [DOI] [PubMed] [Google Scholar]
- 13.Matsushima T, Yamaguchi T, Inoue T K, Matsukado K, Fukui M. Recurrent trigeminal neuralgia after microvascular decompression using an interposing technique. Teflon felt adhesion and the sling retraction technique. Acta Neurochir (Wien) 2000;142(05):557–561. doi: 10.1007/s007010050469. [DOI] [PubMed] [Google Scholar]
- 14.Hussain M A, Konteas A, Sunderland G. Re-exploration of microvascular decompression in recurrent trigeminal neuralgia and intraoperative management options. World Neurosurg. 2018;117:e67–e74. doi: 10.1016/j.wneu.2018.05.147. [DOI] [PubMed] [Google Scholar]
- 15.Lang J. [Neuroanatomy of the optic, trigeminal, facial, glossopharyngeal, vagus, accessory and hypoglossal nerves (author's transl)] Arch Otorhinolaryngol. 1981;231(01):1–69. doi: 10.1007/BF00465556. [DOI] [PubMed] [Google Scholar]
- 16.Saunders R L, Sachs E., Jr Relation of the accessory rootlets of the trigeminal nerve to its motor root. A microsurgical autopsy study. J Neurosurg. 1970;33(03):317–324. doi: 10.3171/jns.1970.33.3.0317. [DOI] [PubMed] [Google Scholar]
- 17.Gudmundsson K, Rhoton A L, Jr, Rushton J G. Detailed anatomy of the intracranial portion of the trigeminal nerve. J Neurosurg. 1971;35(05):592–600. doi: 10.3171/jns.1971.35.5.0592. [DOI] [PubMed] [Google Scholar]
- 18.Young R F. Unmyelinated fibers in the trigeminal motor root. Possible relationship to the results of trigeminal rhizotomy. J Neurosurg. 1978;49(04):538–543. doi: 10.3171/jns.1978.49.4.0538. [DOI] [PubMed] [Google Scholar]
- 19.Young R F, Kruger L. Axonal transport studies of the trigeminal nerve roots of the cat. With special reference to afferent contributions to the portio minor. J Neurosurg. 1981;54(02):208–212. doi: 10.3171/jns.1981.54.2.0208. [DOI] [PubMed] [Google Scholar]
- 20.Yousry I, Moriggl B, Holtmannspoetter M, Schmid U D, Naidich T P, Yousry T A. Detailed anatomy of the motor and sensory roots of the trigeminal nerve and their neurovascular relationships: a magnetic resonance imaging study. J Neurosurg. 2004;101(03):427–434. doi: 10.3171/jns.2004.101.3.0427. [DOI] [PubMed] [Google Scholar]
- 21.Feng B H, Zheng X S, Liu M. Microvascular decompression for trigeminal neuralgia: zone exploration and decompression techniques. J Craniofac Surg. 2015;26(08):2381–2384. doi: 10.1097/SCS.0000000000002147. [DOI] [PubMed] [Google Scholar]


