Abstract
Introduction
Since its inception, laparoscopic surgery has evolved and new techniques have been developed due to technological advances. This requires a different and more complex skill set in comparison with open surgery. Reduced working hours, less training time and patient safety factors demand that such skills need to be achieved outside the operating theatre environment. Several studies have been published and have determined the effectiveness of virtual reality training.
We aimed to compare virtual reality training with the traditional apprenticeship method of training and determine whether it can supplement or replace the traditional apprenticeship model. We also aimed to perform a meta-analysis of the literature and develop conclusions with respect to the benefits achieved by adding virtual reality training on a regular basis to surgical training programmes.
Methods
A literature search was carried out on PubMed, MEDLINE, EMBASE and Google Scholar academic search engines using the MESH terms ‘randomised controlled trials’, ‘virtual reality’, ‘laparoscopy’, ‘surgical education’ and ‘surgical training’. All randomised controlled trials published to January 2018 comparing virtual reality training to apprenticeship training were included. Data were collected on improved dexterity, operative performance and operating times. Each outcome was calculated with 95% confidence intervals and with intention-to-treat analysis; 24 randomised controlled trials were analysed.
Findings
Meta-analytical data were extracted for time, path length, instrument handling, tissue handling, error scores and objective structure assessment of technical skills scoring. There was significant improvement in individual trainee skill in all meta-analyses (p < 0.0002).
Conclusion
This meta-analysis shows that virtual reality not only improves efficiency in the trainee’s surgical practice but also improves quality with reduced error rates and improved tissue handling.
Keywords: Laparoscopy, Virtual reality, Randomised controlled trials, Patient safety, Apprenticeship training
Introduction
Laparoscopic surgery and the advent of robotic surgery has modernised surgical care, encouraging hospital and health authorities to shift toward a minimally invasive system of performing surgical procedures.1 Thus, surgical trainees must acquire the skills and level of proficiency in laparoscopic surgery.2 Setbacks and health policies safeguarding patient safety threaten and limit the exposure of surgical trainees to laparoscopic surgery.3–7 To tackle this problem, surgical training centres provide opportunities through simulation and virtual reality.1,4
In contrast to the Halstedian mantra, simulation and technology safeguard patient safety and provide trainee feedback during their performance.1 Unfortunately, there is no recent literature comparing virtual reality with apprenticeship training.4,7 However, several randomised controlled trials (RCTs) have shown a positive attitude towards the implementation of simulation in surgical training programmes. Current literature reports a general agreement regarding the superiority in the proficiency of virtual reality to the apprenticeship model among trainees.1,3,8,9
The typical virtual reality setup is an enclosed device attached to a monitor with ports for insertion of instruments connected to a software-based system.4,10,11,29 Different devices use different systems, some using tracking of motion for simulation.7,11 Others use items directed at training individual skills (eg knotting).7,9
This meta-analysis had two aims: comparing virtual reality training with apprenticeship training to determine whether it replaces or supplements the latter, and providing data to develop conclusions about the benefits achieved by adding virtual reality training routinely for surgical trainees.
Methods
We carried out a literature search of PubMed, MEDLINE, EMBASE, Cochrane Library and Google Scholar academic search engines using the ‘Advanced Search’ setting and the medical subject headings ‘randomised controlled trial’, ‘virtual reality’, ‘laparoscopy’, ‘surgical education’ and ‘surgical training’. To obtain specific studies, Boolean characters ‘OR’ and ‘AND’ were used, with wildcards such as ‘+’, “” and ‘?’. All RCTs published to January 2018 comparing virtual reality training to apprenticeship training were included. Unfortunately, the literature search did not provide any randomised controlled studies between 2015 and 2019.
Additional inclusion criteria were the use of validated virtual reality simulators and studies with objective scoring methods. We excluded RCTs using endoscopic techniques other than laparoscopy. Studies that fitted the inclusion criteria allocated their participants into a virtual reality training group (case) and an apprenticeship training group (control).
Three groups of participants were enrolled:
naïve – participants with no exposure to laparoscopic surgery including medical students
novice – surgical residents with some experience in laparoscopic surgery (ie still training)
expert – laparoscopic surgeons who finished training programme.
The initial literature search yielded 32 RCTs fitting the inclusion criteria and provided sufficient data for the meta-analysis. Studies were analysed to ensure random sequence generator and blinding of participants; assessors and benchmark measurements were used to eliminate performance bias and eliminate selection bias, respectively. Using these criteria, eight studies were excluded, leaving 24 RCTs included in this meta-analysis. Data were collected on six parameters: operative time, path length, instrument handling, tissue handling, error scores and objective structured assessment of technical skills (OSATS) scoring.
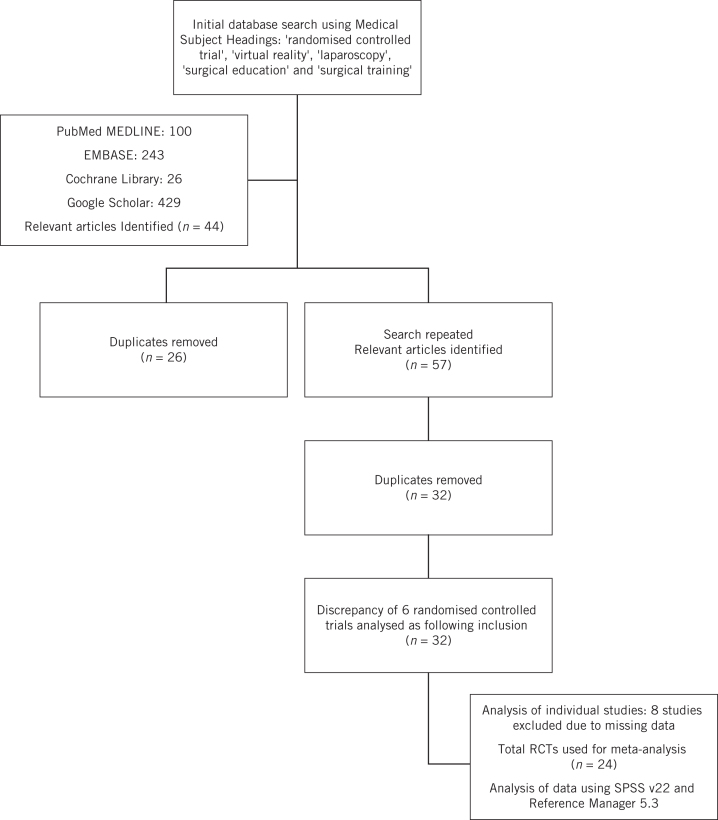
The meta-analysis was performed following the recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-Analysis statement and the Cochrane Collaboration statement (Fig 1).
Figure 1.
Flow diagram illustrating the studies included
The data were tabulated using Microsoft Excel and the analysis was done using Reference Manager 5.3 and SPSS 24.0. For each outcome, the mean difference was calculated with 95% confidence interval and with intention-to-treat analysis. Study heterogeneity was assessed by the I-square (I2) and Chi-square (χ2) tests.
Findings
The objectives were finalised by six meta-analyses for each of the six data sets mentioned above. For each of the six meta-analyses we used the data available depending on the six parameters we set out to analyse. For example, if four papers studied and compared the operative time in virtual reality training compared with apprenticeship training these were included (Tables 1 and 2).
Table 1.
Summary of characteristics of included studies
| Study | Participants (n) | Benchmark measurements | Level of expertise | VR training modality | VR training performed | Control group | Assessment method | Recorded results |
| Aggarwal et al (2007)10 | 19 | 10 experienced surgeons completed 2 laparoscopic cholecystectomies | Novice | LapSim® (Surgical Sciences Sweden AB) | Proficiency based: Calot’s triangle dissection + 3 porcine laparoscopic cholecystectomies | 5 cadaveric porcine laparoscopic cholecystectomies | 5 porcine laparoscopic cholecystectomies | ROVIMAS; time taken, total path length, total number of movements, video rating scores |
| Ahlberg et al (2007)39 | 13 | 5 experienced surgeons performed 6 tasks in recorded results | Novice | LapSim | Proficiency based: 6 tasks performed under supervision until expert level attained | No additional training | 10 laparoscopic cholecystectomies performed per trainee | Errors in exposure, clipping and tissue division, dissection errors, total errors, surgical time |
| Ahlborg et al (2013)3 | 28 | Nil (No benchmark measurement) | Novice | LapSim | 2-day practice on simulator | No additional training | 3 supervised laparoscopic tubal occlusions | Visuospatial ability, flow scores, time |
| Ali et al (2014)11 | 60 | Nil | Novice and expert | LapSim | LapSim group: camera navigation, instrument navigation, coordination, grasping, cutting, lifting, suturing, dissection. Box model group: excise a drawn circle, move pegs, cut the outer balloon, grasp and throw beans, peel an orange, suture and tie a knot, introduce an epidural catheter into an intravenous infusion tube. |
No additional training | Supervised laparoscopic tubal occlusions | OSA-LS; operation time, total score, economy of movements, movements/instrument handling, economy of time, respect of tissue |
| Andreatta et al (2006)12 | 19 | Nil | Novice | Lap Mentor™ (3D Systems) | Proficiency based: camera navigation, eye-hand coordination, clipping and grasping, cutting, electrocautery and translocation of objects | No additional training | Laparoscopic skills exercises on anaesthetised male pigs | Camera navigation, eye–hand coordination, time, efficiency of motion, instrument handling, perceptual ability, safe electrocautery, safe clipping |
| Calatayud et al (2010)13 | 10 | Nil | Novice and expert | LapSim | Preoperative VR training termed as ‘warm-up’ | No additional training | Supervised laparoscopic cholecystectomy | OSATS; respect for tissue, time and motion, instrument handling, knowledge of instruments, use of assistants, flow of operation, knowledge |
| Cosman et al (2007)14 | 10 | 10 experienced surgeons performed clipping task on the simulator | Novice | LapSim | Proficiency based: clipping task + training protocol for a maximum of 1 hour/day | No additional training | Supervised application of clips and divide cystic duct or cystic artery during a laparoscopic cholecystectomy | Errors, global score, time |
| Hogle et al (2009)27 | 33 | Nil | Novice and expert | LapSim | Proficiency based: novice – camera navigation, instrument navigation, coordination, grasping, lifting and grasping, cutting and clip applying; expert – training on a laparoscopic simulator for 5 weeks | No additional training | Supervised laparoscopic cholecystectomy | GOALS; Depth perception, bimanual dexterity, efficiency, efficiency, tissue handling, autonomy, operative time |
| Hung et al (2012)28 | 24 | Nil | Novice | DaVinci® Skills Simulator (Mimic Technologies Inc.) | 17 simulator exercises over 10 weeks | No additional training | Porcine bowel resection, cystotomy and repair and partial nephrectomy using robotic system | GOALS; objects dropped, motion economy, excessive instrument force, instrument collisions, missed targets, time, broken vessels, blood loss |
| Hyltander et al (2002)5,22 | 24 | Nil | Naïve | LapSim | 4 simulator exercises: camera navigation, instrument navigation, instrument handling, manipulating items for 2 hours/week for 5 weeks | No additional training | Laparoscopic surgery on two anaesthetised pigs | Camera navigation, instrument navigation, combination, extended combination, time |
| Larsen et al (2009)23 | 21 | Nil | Novice | LapSim | Oral introduction on simulator + simulator training in lifting and grasping and cutting + completion of a simulated right sided salpingectomy. Training cycles of 45–60 minutes. | No additional training | Supervised laparoscopic salpingectomy | Duration of training, time, score |
| Lucas et al (2008)25 | 32 | Nil | Naïve | Lap Mentor | 8 simulator exercises: camera manipulation, hand–eye coordination, clipping, grasping, 2-handed manoeuvres, cutting, fulguration and object translocation. 6 unsupervised training sessions of 30 minutes each. | No additional training | Porcine laparoscopic nephrectomy | OSATS; respect for tissue, time and motion, instrument handling, knowledge of instruments, use of assistants, flow of operation, knowledge |
| Lucas et al (2008)24 | 32 | Nil | Naïve | Lap Mentor | 8 simulator exercises: camera manipulation, hand–eye coordination, clipping, grasping, 2-handed manoeuvres, cutting, fulguration and object translocation. 6 unsupervised training sessions of 30 minutes each. | No additional training | Supervised simple laparoscopic cholecystectomy | OSATS; respect for tissue, time and motion, instrument handling, knowledge of instruments, use of assistants, flow of operation, knowledge |
| Madan & Frantzides (2007)40 | 65 | Nil | Naïve | MIST-VR | Simulator exercises: acquire and place, transfer and place, transversal, withdraw and insert, diathermy, manipulate and diathermy. 10 sessions of 20 minutes each for both simulator and box-trainer groups. | No additional training | Four tasks assessed in a porcine laboratory | Tissue handling, placing bowel in retrieval bag, liver biopsy, stapling, ‘running’ the bowel |
| Maschuw et al (2011)15 | 50 | Nil | Novice | LapSim | Proficiency based simulator exercises + virtual laparoscopic cholecystectomy for twice a week sessions for 3 months | No additional training | VR simulation assessing predefined criteria | Time, path length, angular path, tissue damage, economy of motion |
| McClusky et al (2004)6 | 12 | Experienced surgeons performed laparoscopic cholecystectomy | Novice | MIST-VR | Simulator exercises: manipulation and diathermy | No additional training | Supervised laparoscopic cholecystectomy | OSATS; time, path length, angular path, operative steps, score |
| Palter et al (2012)21 | 25 | Nil | Novice | LapSim | Proficiency based: simulator exercises + video instruction for a duration of 5 months | No additional training | Supervised laparoscopic right hemicolectomy | OSATS; respect for tissue, time and motion, instrument handling, knowledge of instruments, use of assistants, flow of operation, knowledge |
| Palter et al (2013)16 | 18 | Nil | Novice | LapSim | Theoretical training + case-based learning + simulator training for 6 months | No additional training | 5 laparoscopic cholecystectomies in operating theatre, VR assessment and simulated crisis scenario | Time, path length, angular path, number of errors |
| Sergio et al (2014)26 | 14 | Nil | Naïve | Lap Mentor | Virtual sigmoid colectomy: 2-hour training on simulator | No additional training | Laparoscopic sigmoid resection on anaesthetised pig | Tissue handling, dexterity, instrument handling, exposure, haemostasis, flow of tasks, technical skills score |
| Seymour et al (2002)29 | 16 | 4 experienced surgeons performed the 10 trials in recorded results | Novice | MIST-VR | Proficiency based: two trials performed with both hands. Training sessions lasted approx. 1 hour. | No additional training | Supervised laparoscopic cholecystectomy | Number of errors |
| Tanoue et al (2005)18 | 30 | Nil | Naïve | MIST-VR | 1 simulator exercise - one stitch and two ties including left- and right-hand repetitions for 2 hours/day for 2 days | No additional training | One stitch and two ties including left and right repetitions in a box trainer | Improvement rate |
| Tanoue et al (2008)17 | 35 | Nil | Naïve | MIST-VR | 3 simulator/box trainer exercises: suturing, knot tying and diathermy including left- and right-hand repetitions for 2 hours/day for 2 days | Watched an educational video for 30 minutes | Stitch needle to place one stitch and two ties between dots printed on a rubber sheet in a box trainer | Time, speed |
| Verdaasdonk et al (2008)19 | 20 | Nil | Novice | Simendo® | Proficiency based: knot-tying repeated for 10 times | No additional training | Laparoscopic knot on an anaesthetised porcine model | Instrument handling, needle and suture drops, attempted loops, knot tightening |
| Youngblood et al (2005)20 | 46 | Experienced surgeons performed laparoscopic techniques | Naïve | LapSim and tower trainer | 3 simulator tasks: grasping and placing gallstones in endo bag, running the bowel, clipping and cutting an artery. 4 supervised, 45-minute training sessions. | No additional training | Laparoscopic assessment in porcine laboratory | Time, accuracy |
GOALS, global operative assessment of laparoscopic skills; MIST-VR, minimally invasive surgery trainer – virtual reality; OSA-LS, objective structured assessment – laparoscopic salpingectomy; OSATS, objective structured assessment of technical skills; ROVIMAS, RObotics VIdeo and Motion Assessment Software; VR, virtual reality
Table 2.
Summary of characteristics of excluded studies
| Study | Participants (n) | Benchmark measurements | Level of expertise | VR Training Modality | VR Training Performed | Control group | Assessment method | Recorded results | Reason for exclusion |
| Clevin & Grantcharov (2008)41 | 16 | Nil | Novice | LapSim® (Surgical Sciences Sweden AB) | Simulator exercises: camera navigation, instrument navigation, coordination, grasping, lifting, cutting and clip applying. Box training exercises: moving pegs, cutting, introducing an epidural catheter in an infusion tube, applying clips, cutting for 5-minute didactic hands-on instruction on simulator followed by 3 hours on a box model trainer. | No additional training | Simulator exercises | Time, misses, drift, path length, angular path | No documentation of specific mean results other than p-value |
| Gallacher et al (2013)42 | 225 | Nil | Novice and expert | MIST-VR | Simulator exercises: experts and novices: holding items, instrument manipulation | No additional training | Simulator exercises - cutting, grasping, instrument manipulation, object manipulation | Correct incisions, errors | No documentation of specific mean results other than p -value |
| Grantcharov et al (2004)43 | 16 | Nil | Novice | MIST-VR | 6 simulator exercises | No additional training | Simulated laparoscopic cholecystectomy | Errors, economy of movement | No documentation of specific mean results other than p -value |
| Hiemstra et al (2011)8 | 50 | Nil | Naïve | Simendo® | Simulator exercises | No additional training | Simulator exercises | Time, path length, motion | Evaluation of data showed comparison done between VR, box-trainer and control. data inadequate for the study |
| Munz et al (2004)44 | 24 | Nil | Naïve | LapSim | Simulator exercises: instrument navigation, coordination, grasping, cutting, precision, speed for 3 weekly sessions of 30 minutes each | No additional training | Simulator exercises | Distance, time, economy of movement, errors | No documentation of specific mean results other than p -value |
| Pearson et al (2002)9 | 43 | Nil | Naïve | MIST-VR | Simulator exercises: knot tying | No additional training | 10 knot-tying trials | Economy of movement, errors, time | No documentation of specific mean results other than p -value |
| Torkington et al (2000)45 | 30 | Nil | Naïve | MIST-VR | 6 simulator tasks: minimal-access training tasks performed over a period of one hour | No additional training | Drills performed using the Imperial College Surgical Assessment Device | Distance, movements, speed, time | Data compared values for both right- and left-handed use of laparoscopic tools. No overall data was recorded. Excluded to avoid bias. |
| Van Bruwaene et al (2015)46 | 30 | Nil | Novice | Lap Mentor™ (3D Systems) | Proficiency based: simulator exercises and box trainer exercises: laparoscopic cholecystectomy exercises for 5 hours | No additional training | Laparoscopic cholecystectomy on an anaesthetised pig | Time, performance score | No documentation of specific mean results other than p-value |
MIST-VR, minimally invasive surgery trainer – virtual reality; VR, virtual reality
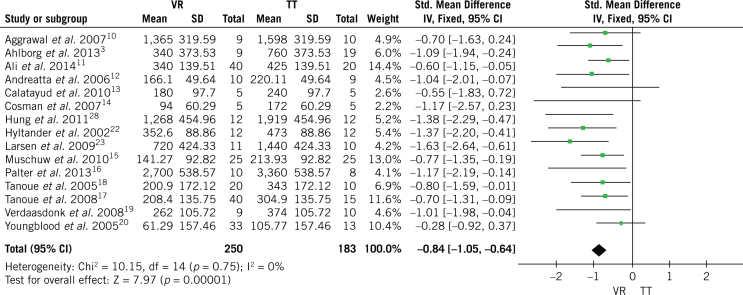
Operative time
Operative time is the time taken to complete the assessment task planned on the individual RCTs. A total of 15 RCTs were included in the meta-analysis involving 433 participants: 250 in the virtual reality training group compared with 183 in the control traditional training group. The meta-analysis for the outcome operative time fell in favour of virtual reality training (Fig 2). The mean difference of operative time for virtual reality compared with traditional training was 0.84 minutes with 95% confidence intervals (CI) of –1.05 and –0.64 The results were statistically significant since CI did not include zero. The heterogeneity value was χ2 = 10.15 (p < 0.00001) I2 = 0%.3,10–23
Figure 2.
Forrest plot for operative time of virtual reality (VR) compared with traditional training (TT)
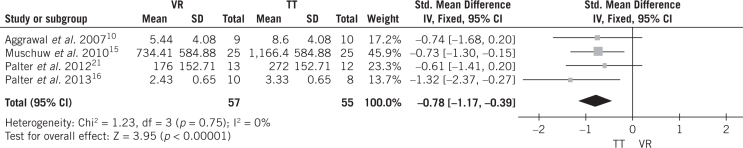
Path length
Path length is the score performed for the recording of the economy of movement. Four randomised controlled trials were chosen involving a total of 112 participants: 57 (virtual reality training) compared with 55 (control traditional training). The meta-analysis for the path length outcome fell in favour of virtual reality training (Fig 3). The mean difference of path length for virtual reality compared with traditional training was 0.78 metres with confidence intervals of –1.17 and –0.39. The results were statistically significant since the confidence intervals did not include zero. The heterogeneity value was χ2 = 1.23 (p < 0.0001) I2 = 0%.10,15,21,22
Figure 3.
Forrest plot for path length of virtual reality (VR) compared with traditional training (TT)
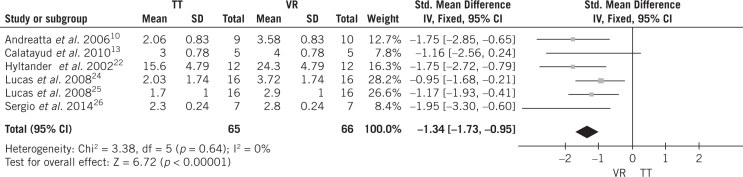
Instrument handling
Instrument handling is the score obtained from blinded assessors for manipulation of instruments. Six RCTs were chosen, with a total of 131 participants (66 in the virtual reality training group vs 65 in the control traditional training group). The meta-analysis for instrument handling outcome was in favour of virtual reality training (Fig 4). The mean difference of the instrument handling score for virtual reality compared with traditional training was 1.34 (95% CI –1.73 and –0.95). The results were statistically significant since the confidence intervals did not include zero. The heterogeneity value was χ2 = 3.38 (p < 0.00001) I2 = 0%.12,13,22,24–26
Figure 4.
Forrest plot for instrument handling of virtual reality (VR) compared with traditional training (TT)
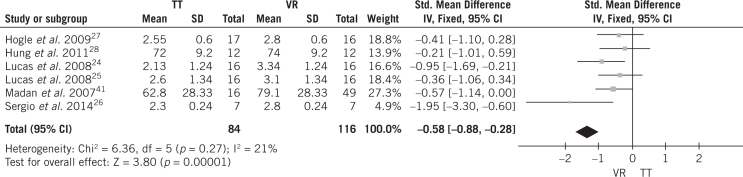
Tissue handling
Tissue handling is the score obtained from blinded assessors for handling of tissues during the test. Six RCTs were chosen including a total of 200 participants (116 in the virtual reality training group vs 84 in the control group). The meta-analysis for the tissue handling outcome fell in favour of virtual reality training (Fig 5). The mean difference of tissue handling score for virtual reality compared with traditional training was 0.58 (95% CI –0.88 and –0.28). The results were statistically significant since the confidence intervals did not include zero. The heterogeneity value was χ2 = 6.36 (p < 0.0001) I2 = 21%.6,24–28
Figure 5.
Forrest plot for tissue handling of virtual reality (VR) compared with traditional training (TT)
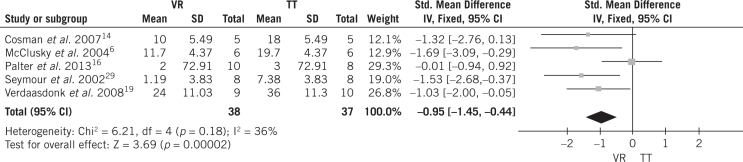
Error score
The error score is the score obtained from blinded assessors for errors for each test RCT or total number of errors recorded in the assessment process. Five RCTs were chosen consisting of a total of 75 participants (38 in the virtual reality training group vs 37 in the control group). The meta-analysis for the error scores outcome fell in favour of virtual reality training (Fig 6). The mean difference of error scores for virtual reality compared with traditional training was 0.95 (95% CI –1.45 and –0.44). The results were statistically significant since the confidence intervals did not include zero. The heterogeneity value was χ2 = 6.21 (p < 0.0002) I2 = 36%.6,14,16,19,29
Figure 6.
Forrest plot for error scores of virtual reality (VR) compared with traditional training (TT)
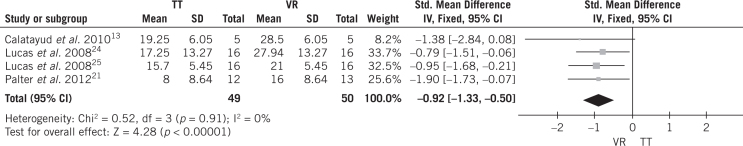
OSATS score
The OSATS score is the total of seven parameters including respect for tissue, time and motion, instrument handling, knowledge of instruments, flow of operation, formed planning, and knowledge of the specific procedure. Four RCTs were chosen consisting of a total of 99 participants (50 in the virtual reality training group vs 49 in the control group). The meta-analysis for the OSATS outcome was in favour of virtual reality training (Fig 7). The mean difference of OSATS score for virtual reality compared with traditional training was 0.92 (95% CI –1.33 and –0.50). The results were statistically significant since the confidence intervals did not include zero. The heterogeneity value was χ2 = 0.52 (p < 0.0001).
Figure 7.
Forrest plot for objective structured assessment of technical skills score of virtual reality (VR) compared with traditional training (TT)
Discussion
This study aimed to compare virtual reality training with the traditional apprenticeship approach of teaching and to establish whether it can supplement or replace the latter training model.
A thorough literature search highlighted 24 RCTs, which provided the essential numerical data to carry out separate meta-analyses within the six recorded parameters as described in the methodology. For the purpose of this study, a p-value of less than 0.5 was considered as being statistically significant and this was applied to each meta-analysis.
The results from each respective meta-analysis suggested a significant concordance towards a positive effect observed from supplementing the laparoscopic trainee with virtual reality simulations. Furthermore, this study emphasised that virtual reality training accentuated aspects crucial to adequate surgical performance. As noted, participants in the virtual reality training model completed the assessment in a shorter time compared with the control group. In addition, the participants scored better overall in the OSATS and showed good technical ability throughout instrument/tissue handling. The economy of movement was better and the participants did not succumb to the same number of mistakes of the control group. An exception was the study by Pater et al, which showed a borderline result.16
Unfortunately, this meta-analysis could not prevent the existence of systematic bias. Some studies did not specify whether individuals who had the opportunity to pre-train on virtual reality systems were excluded from their study groups. This could have made an unfair comparison when virtual reality training was used as the assessment of the traditional apprenticeship model of training among these participants.
It was evident that the virtual reality training model assisted surgical trainees to exercise safer and more efficient tissue/instrument handling techniques with a minimal chance of error. All the meta-analyses performed within their respective subsections/parameters tended towards a more favourable outcome for virtual reality training. In the parameters, subjective scoring was an issue. Thus, we included studies involving multiple expert observers to reduce the risk of observer bias.
Virtual reality training models permit the laparoscopic trainee to acquire the fundamental skills required from surgeons such as camera navigation, grasping, cutting and suturing. Different virtual reality systems provide different levels of difficulty, permitting staggered training possibilities. Similarly, to a virtual reality setup, box trainers offer the trainee the possibility to develop basic laparoscopic skills.30 Newer virtual reality systems also provide statistical data, such as time and path length and provide the trainee with a baseline to evaluate improvement.1
However, the virtual reality training model also has some limitations and issues which need to be addressed to ensure an effective training programme for surgical trainees. In comparison with the traditional approach of training, the virtual reality training setup fails to produce haptic feedback to the trainee. This feedback would allow for a proper understanding of the force required to avoid tissue damage and would provide real time correction of the errors if they were to happen.8 Thus, it was noted that simulation training should be accompanied with feedback, evaluation and formal assessment via methods (eg global operative assessment of laparoscopic skills and OSATS). Literature reviews confirm that both tests are valid in providing formal feedback, but, to date, no study has been identified to compare both scoring systems.13,21,24,25,27,28,31
Despite many RCTs being performed and published, no quantitative meta-analytical study has highlighted the benefit of virtual reality training.30,31 The virtual reality system requires a relatively high-tech setup requiring expensive maintenance and level of functioning. Fortunately, alternatives have been identified, such as box trainers.32 This necessitates meta-analytical data to enable hospitals to properly evaluate such investment decisions.30
This study did not explore the cost–benefit of the two training models, and many variables have been identified that could affect the economic burden of the healthcare sector. Virtual reality simulation equipment is more expensive than box trainer equipment.10,32,33 Although the price of simulators may vary depending upon the techniques, equipment and learning outcomes, apprenticeship training is not without costs. Bridges and Diamond observed that the operating time increased significantly among surgical trainees in comparison with more senior peers.33 In fact, this increased operating time amounted to US$12,000/year for every surgical trainee.33–35
Moreover, in addition to operating times, complication rates were noted to be higher in junior surgeons.10,34–36 This negatively impacts the length of stay of patients, and thus ultimately increases the economic burden on medical institutions. Studies suggest that the cost of virtual reality training systems needs to be balanced against the cost of the longer operating time and complication rates through traditional surgical training.33,36
Despite the new technology incorporated within the virtual reality setup, instruments need to be tested for face and construct validity. This should encourage more software developers to invest in equipment that would provide the trainee with statistical data of their performance in the virtual reality training programme, allowing an overall improvement in psychomotor skills.
Policies implemented in European and American institutions, such as reduced working hours (time constraints), and the importance of safeguarding patient safety are a detriment to the quality of teaching in the operating theatre environment.3,4,7,22,23 Thus, virtual reality training offers an alternative to the teaching opportunities within the operating theatre and ensures appropriate levels of safety.1,26
In contrast to the apprenticeship model of training, virtual reality training cannot fully prepare the surgical trainee for any anatomical variations they might encounter in real-life surgery. These variations are common within the human body and thus skills acquired on this single computer simulation program may not be applicable in practice.35–37
In summary, this meta-analysis has further confirmed that virtual reality training improves efficiency and quality of tissue handling, with reduced error rates, when used in conjunction with the laparoscopic surgeon’s individual ability and knowledge.
Conclusion
Although the 24 studied RCTs did not demonstrate actual evidence of improved patient safety and improved cost–benefit when comparing the virtual reality training model to the apprenticeship model, the participants using virtual reality simulations produced significant results in most parameters. Reduced operation time, better instrument and tissue handling technique and minimal errors were observed throughout the results. If such parameters were to be translated into practice, we believe that the virtual reality training model would allow for a reduced economic burden, improved patient safety system and a decrease in operation time and the incidence of surgical complications within the operating theatre.
We suggest that a separate study should focus on performing a cost–benefit analysis. This would quantify the impact of virtual reality training on patient outcomes, hospital stay and, ultimately, on the medical institutions themselves. Furthermore, it would also be possible to provide an average cost per trainee undergoing such a training programme.
Finally, virtual reality training should not replace the experience of a surgical trainee acquired in the theatre setting. Therefore, it should be used as a supplement throughout the surgical training programme. To improve the validity of virtual reality training tools, one should make use of other formal assessment methods which allow adequate feedback to provide the trainee with an individual baseline for further development.
References
- 1.Alaker M, Wynn GR, Arulampalam T. Virtual reality training in laparoscopic surgery: a systematic review and meta-analysis. Int J Surg 2016; : 85–94. [DOI] [PubMed] [Google Scholar]
- 2.Bjerrum F, Soerensen JL, Konge L et al. Randomised trial to examine procedure-to-procedure transfer in laparoscopic simulator training. Br J Surg 2016; : 44–50. [DOI] [PubMed] [Google Scholar]
- 3.Ahlborg L, Hedman L, Nisell H et al. Simulator training and non-technical factors improve laparoscopic performance among OBGYN trainees. Acta Obstet Gynecol Scand 2013; : 1194–1201. [DOI] [PubMed] [Google Scholar]
- 4.Gallacher AG, McClure N, McGuigan J et al. Virtual reality training in laparoscopic surgery: a preliminary assessment of minimally invasive surgical trainer virtual reality (MIST virtual reality). Endoscopy 1999; : 310–313. [DOI] [PubMed] [Google Scholar]
- 5.Hyltander A, Liljegren E, Rhodin PH et al. The transfer of basic skills learned in a laparoscopic simulator to the operating room. Surg Endosc 2002; : 1324–1328. [DOI] [PubMed] [Google Scholar]
- 6.McClusky DA, Gallacher AG, Ritter EM et al. Virtual reality training improves junior residents’ operating room performance: results of a prospective, randomized, double-blinded study of the complete laparoscopic cholecystectomy. J Am Coll Surg 2004; : S73. [Google Scholar]
- 7.Nagendran M, Gurusamy KS, Aggarwal R et al. Virtual reality training for surgical trainees in laparoscopic surgery. Cochrane Database Syst Rev 2013; : CD006575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hiemstra E, Terveer EM, Chmarra MK et al. Virtual reality in laparoscopic skills training: is haptic feedback replaceable?. Minim Invasive Ther Allied Technol 2011; : 179–184. [DOI] [PubMed] [Google Scholar]
- 9.Pearson AM, Gallacher AG, Rosser JC et al. Evaluation of structured and quantitative training methods for teaching intracorporeal knot tying. Surg Endosc 2002; : 130–137. [DOI] [PubMed] [Google Scholar]
- 10.Aggarwal R, Ward J, Balasundaram I et al. Proving the effectiveness of virtual reality simulator training in laparoscopic surgery. Ann Surg 2007; : 771–779. [DOI] [PubMed] [Google Scholar]
- 11.Ali A, Sendag F, Oztekin MK. Laparoscopic virtual reality simulator and box trainer in gynecology. Int J Gyn Obstet 2014; : 181–185. [DOI] [PubMed] [Google Scholar]
- 12.Andreatta PB, Woodrum DT, Birkmeyer JD et al. Laparoscopic skills are improved with LapMentor training. Ann Surg 2006; : 854–863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Calatayud D, Arora S, Aggarwal R et al. Warm-up in a virtual reality environment improves performance in the operating room. Ann Surg 2010; : 1181–1185. [DOI] [PubMed] [Google Scholar]
- 14.Cosman PH, Hugh TJ, Shearer CJ et al. Skills acquired on virtual reality laparoscopic simulators transfer into the operating room in a blinded, randomised controlled trial. Stud Health Tech Inf 2007; : 76–81. [PubMed] [Google Scholar]
- 15.Maschuw K, Schlosser K, Kupietz E et al. Do soft skills predict surgical performance? a single-center randomised controlled trial evaluating predictors of skill acquisition in virtual reality laparoscopy. World J Surg 2011; : 480–486. [DOI] [PubMed] [Google Scholar]
- 16.Palter VN, Orzech N, Reznick RK et al. Validation of a structured training and assessment curriculum for technical skill acquisition in minimally invasive surgery: a randomised controlled trial. Ann Surg 2013; : 224–230. [DOI] [PubMed] [Google Scholar]
- 17.Tanoue K, Ieiri S, Konishi K et al. Effectiveness of endoscopic surgery training for medical students usinga virtual reality simulator versus a box trainer: a randomized controlled trial. Surg Endosc 2008; : 985–990. [DOI] [PubMed] [Google Scholar]
- 18.Tanoue K, Yasunaga T, Konishi K et al. Effectiveness of training for endoscopic surgery using a simulator with virtual reality: Randomized study. Int Congr Ser 2005; : 515–520. [Google Scholar]
- 19.Verdaasdonk EGG, Dankelman J, Lange JF et al. Transfer validity of laparoscopic knot-tying training on a virtual reality simulator to a realistic environment: a randomized controlled trial. Surg Endosc 2008; : 1636–1642. [DOI] [PubMed] [Google Scholar]
- 20.Youngblood PL, Srivastava S, Curet M et al. Comparison of training on two laparoscopic simulators and assessment of skills transfer to surgical performance. J Am Coll Surg 2005; : 546–551. [DOI] [PubMed] [Google Scholar]
- 21.Palter VN, Grantcharov TP. Development and validation of a comprehensive curriculum to teach an advanced minimally invasive procedure. Ann Surg 2012; : 25–32. [DOI] [PubMed] [Google Scholar]
- 22.Hyltander A, Liljegren E, Rhodin PH et al. The transfer of basic skills learned in a laparoscopic simulator to the operating room. Surg Endosc 2002; : 1324–1328. [DOI] [PubMed] [Google Scholar]
- 23.Larsen CR, Soerensen JL, Grantcharov TP et al. Effects of virtual reality training on laparoscopic surgery: randomized controlled trial. BMJ 2009; : b1802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lucas S, Tuncel A, Bensalah K et al. Virtual reality training improves simulated laparoscopic surgery performance in laparoscopy naïve medical students. J Endourol 2008; : 1047–1051. [DOI] [PubMed] [Google Scholar]
- 25.Lucas S, Zeltser IS, Bensalah K et al. Training on a virtual reality laparoscopic simulator improves performance of an unfamiliar live laparoscopic procedure. J Urol 2008; : 2588–2591. [DOI] [PubMed] [Google Scholar]
- 26.Sergio EA, Delaney CP, Seid VE et al. Short-duration virtual reality simulation training positively impacts performance during laparoscopic colectomy in animal model: results of a single-blinded randomized trial. Surg Endosc 2014; : 2547–2554. [DOI] [PubMed] [Google Scholar]
- 27.Hogle NJ, Chang VEM, Strong AOU et al. Validation of laparoscopic surgical skills training outside the operating room: a long road. Surg Endosc 2009: ; 1476–1482. [DOI] [PubMed] [Google Scholar]
- 28.Hung AJ, Patil MB, Zehnder P et al. Concurrent and predictive validation of a novel robotic surgery simulator: a proscpective, randomised study. J Urol 2012; : 630–637. [DOI] [PubMed] [Google Scholar]
- 29.Seymour NE, Gallacher AG, Roman SA et al. Virtual reality training improves operating room performance – results of a randomised double-blinded study. Ann Surg 2002: : 458–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fried GM, Feldman LS, Vassiliou MC et al. Proving the value of simulation in laparoscopic surgery. Ann Surg 2004; : 518–525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Torricelli FCM, Barbosa JABA, Marchini GS. Impact of laparoscopic surgery training laboratory on surgeon’s performance. World J Gastrointest Surg 2016; : 735–743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ikonen TS, Antikainen T, Silvennoinen M et al. Virtual reality simulator training of laparoscopic cholecystectomies: a systematic review. Scand J Surg 2012; : 5–12. [DOI] [PubMed] [Google Scholar]
- 33.Bridges M, Diamond DL. The financial impact of teaching surgical residents in the operating room. Am J Surg 1999; : 28–32. [DOI] [PubMed] [Google Scholar]
- 34.Gurusamy KS, Aggarwal R, Palanivelu L, Davidson BR. Virtual reality training for surgical trainees in laparoscopic surgery. Cochrane Database Syst Rev 2009; : CD006575. [DOI] [PubMed] [Google Scholar]
- 35.Nagendran M, Rajesh,Gurusamy KS Aggarwal R et al. Virtual reality training for surgical trainees in laparoscopic surgery. Cochrane Database Syst Rev 2013; : CD006575.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Thompson JR, Leonard AC, Doarn, Doarn CR et al. Limited value of haptics in virtual reality laparoscopic cholecystectomy training. Surg Endosc 2011; : 1107–1114. [DOI] [PubMed] [Google Scholar]
- 37.Khan R, Plahouras C, Johnston B et al. Virtual reality simulation training for health professions trainees in gastrointestinal endoscopy. Cochrane Database Syst Rev 2018; : CD008237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wilkiemeyer M, Pappas TN, Giobbie-Hurder A et al. Does resident post graduate year influence the outcomes of inguinal hernia repair?. Ann Surg 2005; : 879–884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ahlberg G, Enochssohn L, Gallagher AG et al. Proficiency-based laparoscopic simulator training leads to improved operating room skill that is resistant to decay. Surg Innov 2008; : 69–73. [DOI] [PubMed] [Google Scholar]
- 40.Madan AK, Frantzides CT. Prospective randomized controlled trial of laparoscopic trainers for basic laparoscopic skills acquisition. Surg Endosc 2007; : 209–213. [DOI] [PubMed] [Google Scholar]
- 41.Clevin L, Grantcharov T. Does box model training improve surgical dexterity and economy of movement during virtual reality laparoscopy? A randomised trial. Acta Obstet Gynecol 2008; : 99–103. [DOI] [PubMed] [Google Scholar]
- 42.Gallagher AG, Seymour NE, Jordan-Black et al. Prospective, randomised assessment of transfer of training (ToT) and transfer effectiveness ratio (TER) of virtual reality simulation training for laparoscopic skill acquisition. Ann Surg 2013; : 1025–1031. [DOI] [PubMed] [Google Scholar]
- 43.Grantcharov T, Kristiansen V, Bendix J et al. Randomized clinical trial of virtual reality simulation for laparoscopic skills training. Br J Surg 2004; : 146–150. [DOI] [PubMed] [Google Scholar]
- 44.Munz Y, Kumar B, Moorthy K et al. Laparoscopic virtual reality and box trainers: is one superior to the other?. Surg Endosc 2004; : 485–494. [DOI] [PubMed] [Google Scholar]
- 45.Torkington J, Smith SGT, Rees BI, Darzi A. Skill transfer from virtual reality to a real laparoscopic task. Surg Endosc 2001; : 1076–1079. [DOI] [PubMed] [Google Scholar]
- 46.Van Bruwaene S, Schijven MP, Napolitano D, et al. Porcine cadaver organ or virtual-reality simulation training for laparoscopic cholecystectomy: a randomized, controlled trial. J Surg Educ 2015; : 483–490. [DOI] [PubMed] [Google Scholar]