Abstract
Air pollution has been labelled the ‘new smoking’, with news articles bearing titles such as ‘If You Live in a Big City You Already Smoke Every Day’ and ‘The Air Is So Bad in These Cities, You May As Well Be Smoking’. Dr Tedros Adhanom Ghebreyesus, WHO Director-General, highlighted this attention-catching comparison, saying, ‘The world has turned the corner on tobacco. Now it must do the same for the ‘new tobacco’ – the toxic air that billions breathe every day’ and ‘Globally, with smoking on the decline, air pollution now causes more deaths annually than tobacco’ at the First Global Conference on Air Pollution and Health in 2018. The suggestion that the world has turned the corner on tobacco control and the reference to air pollution as the ‘new smoking’ raise a number of concerns. We generate outputs from GBD Compare (the online data visualisation tool of the Global Burden of Diseases and Injuries (GBD) Study) to demonstrate historical disease burden trends in terms of disability-adjusted life years and age-standardised mortality attributable to air pollution and tobacco use from 1990 to 2017 across the globe. We find that the disease burden caused by ambient air pollution declined significantly faster than the burden caused by tobacco use. We conclude that the world is still far from turning the corner on the tobacco endemic. Further, the suggestion that air pollution is as bad as actual smoking is not only inaccurate but also potentially dangerous to public health.
Keywords: new smoking, attributable deaths, tobacco control, ambient air pollution
The rise in the use of facemasks and indoor air purifiers whether effective or not, is a sign of public concern about ambient air pollution, which recently has been labelled the ‘new smoking’ in news articles bearing titles such as ‘If You Live in a Big City You Already Smoke Every Day’1 and ‘The Air Is So Bad in These Cities, You May As Well Be Smoking’.2 An article in the Economist titled ‘Mapping the Invisible Scourge’ claimed that spending 1 day in Beijing is equivalent to smoking 40 cigarettes.3 Adding to this, an app called ‘S**t! I Smoke!’ measures real-time air pollution in terms of the equivalent number of cigarettes smoked. At the First Global Conference on Air Pollution and Health held in Geneva in November 2018, Dr Tedros Adhanom Ghebreyesus, WHO Director-General, highlighted this attention-catching comparison: ‘The world has turned the corner on tobacco. Now it must do the same for the ‘new tobacco’—the toxic air that billions breathe every day.’ He continued, ‘Globally, with smoking on the decline, air pollution now causes more deaths annually than tobacco.’4
Analogising other health risks as ‘the new smoking’ to highlight their danger is not new. This equivalence has been made for several other risk factors that received momentary media prominence, including prolonged sitting, obesity, high-protein diets and diets high in processed meats.5 However, most of the ‘new smoking’ hypes have been short-lived,6 and ‘old smoking’ continues to be the unresolved, second-largest cause of death worldwide.7 Since this analogy is common, it is essential to consider how such a comparison could potentially affect global tobacco control and aspects of daily life such as outdoor physical activity.
There are a number of concerns raised by suggestions that the world has turned the corner on the tobacco endemic and that air pollution is the ‘new smoking’.
First, the world has not turned the corner on the tobacco endemic
Smoking remains one of the top preventable causes of death and disability despite decades of tobacco control efforts and some promising successes. However, currently only two countries—Brazil and Turkey—have implemented all MPOWER measures at best-practice level as recommended by WHO.8 Many countries with a high-disease burden from tobacco, such as China, Indonesia and even high-income countries like Germany, have seen limited progress in controlling the smoking and tobacco endemic. Sales of cigarettes continue to soar in China9 as well as in many low-income and middle-income countries.10 Judging by a chronically underfunded global tobacco control unit at the WHO, it would be devastating to global tobacco control if WHO were to divert its attention and resources from tobacco control at this stage. The world needs more resources for global tobacco control in order to reach the sustainable development goals in the next few decades.11
Second, smoking causes more premature deaths and devastating disability than air pollution, despite being completely avoidable
Deaths, disability and human suffering caused by smoking often come at an earlier age and are more painful in terms of symptoms and outcomes than those caused by outdoor air pollution. Recent analyses from the 2017 Global Burden of Disease and Injuries Study indicate that between 2007 and 2017, the number of deaths due to outdoor particulate matter (PM2.5) air pollution increased from 2.42 million to 2.94 million.7 Despite these increases, the same study shows that tobacco use, combined with the harms from secondhand smoke, remains the second-largest risk factor for death and disability globally; responsible for 8.3 million deaths in 2017, nearly three times that of outdoor air pollution.7 According to Doll et al’s milestone study, smoking kills half of all long-term users, an estimate endorsed by WHO.12 More recently, the death toll was estimated to be as high as two-thirds for smokers who start at a young age.13 Overall, life expectancy for smokers is about 10 years less than for non-smokers14 while lifetime exposure to air pollution in a mildly (15 µg/m3 mean PM2.5) or moderately polluted city (25 µg/m3 mean PM2.5) results in an estimated reduction of life expectancy by 0.8 or 1.6 years, respectively.15
In addition, disability-adjusted life years (DALYs) due to air pollution, across all countries and social development levels, exhibited a general decline from 1990 to 2017 (figure 1). For the USA, a recent study found that deaths attributable to air pollution decreased by 47% from 1990 to 2010, dropping from about 135 000 to 71 100, which translates to one of every 35 deaths.16 In contrast, smoking causes one of every five deaths in the USA, totalling around 480 000 deaths each year.17 China, which is infamous for its poor air quality and has the greatest disease burden due to air pollution in the world, accounted for about 25% of global deaths from air pollution in 2016.18 Yet even in China, 2.5 times more deaths are caused by smoking than by ambient air pollution, a trend that has not changed significantly since 1990.19 In our recent commentary, we investigated the contribution of air pollution and smoking to chronic obstructive pulmonary disease (COPD). We concluded that while nearly 100% of the global population is exposed to some degree of air pollution and only a fraction smokes, the bulk of COPD diagnoses (70%) are linked to smoking—10 times more than those attributed to ambient PM2.5.20
Figure 1.
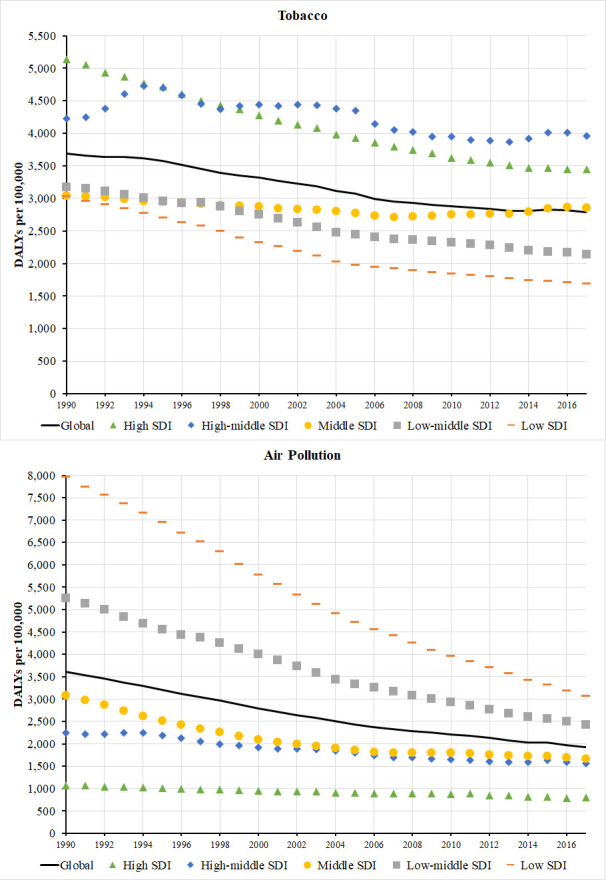
Loss of disability-adjusted life years (DALYs) due to tobacco use and air pollution across social development levels, extracted from the GBD Compare Visualisation Tool, IHME, University of Washington, 2017.19
Third, from 1990 to 2017, cleaning up air pollution to reduce associated harms has been more successful than stubbing out tobacco-related harms
As figure 1 indicates, since 1990, across countries with varying social development levels, more gains have been made from reducing air pollution than from controlling the tobacco endemic in terms of reduction in DALYs. The numbers of age-standardised deaths per 100 000 people attributable to air pollution have declined significantly across diverse countries according to GBD estimates (figure 2).
Figure 2.
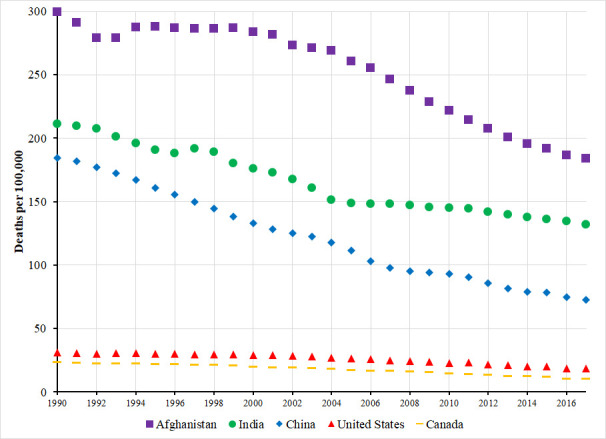
Age-standardised deaths per 100 000 people due to air pollution in Afghanistan, India, China, the USA, Canada, extracted from the GBD Compare Visualization Tool, IHME at University of Washington, 2017.19
Studies on secondhand smoke have found that PM2.5 concentrations were often much higher in the restaurants and bars where smoking was allowed than at the side of outdoor roadways.21 For instance, in Copenhagen, higher concentration of PM2.5 (165.1±8.5 µg m3) were found in smoking areas than along adjacent motorways (4.6±0.7 µg m3).22
Fourth, stating that air pollution is the new smoking undermines tobacco control efforts and the promotion of physical activity
If air pollution really is the new smoking, some smokers may conversely think that breathing air is equally as bad as smoking. Among the more than one billion current smokers worldwide, this equivalence may lead some to wonder why they should even bother to quit. Paradoxically, some nonsmokers may consider smoking since they believe that breathing urban air is the same.
The tobacco industry would likely welcome the comparison of air pollution and smoking, as this will create a perception that using their products is ‘only as bad as breathing polluted air’. The ubiquitous presence of outdoor air pollution is a common justification used by adolescents who have begun smoking and by smokers who are uncertain about quitting.23 However, breathing polluted air is not highly addictive nor is it heavily marketed by a notorious industry. No industry deliberately produces toxic and addictive ambient air as a commodity, in stark contrast to the tobacco industry, which produces and aggressively markets a toxic and addictive commodity—cigarettes. The success of the tobacco industry depends on generating as many nicotine-dependent customers as possible.24 In addition, unlike smoking, measures to improve air quality have tremendous public support, in part because people are not addicted to toxic air in the same way that smokers are dependent on nicotine. In China, for example, public outrage about air quality and the resulting decline in foreign investment has led the government to take drastic measures to improve air quality. As a result of these measures, air quality in major Chinese cities has improved significantly in only a few years.25 In contrast, despite China's more than decade-long commitment to tobacco control and ratification of the WHO Framework Convention on Tobacco Control, tobacco consumption is increasing. Notwithstanding a slight decline in 2016 due to a tax hike, consumption again increased in 2017 and 2018.9
Due to the fear of outdoor air pollution, some have suggested never exercising at rush hours.26 However, this suggestion may cause more harms than gains, as the potential benefits of exercise almost always trump the potential harm from air pollution.27 A study found that for 99% of cities in the WHO air quality database, the health benefits gained from cycling 2 hours each day outweighed the extra risk due to air pollution for most people.28
In conclusion, we believe that the importance of improving air quality should not be emphasised in a way that potentially undermines the risks of tobacco use. The public should not be advised that air pollution is as bad as smoking, because it is not. Instead, it is important to scale up action on both tobacco control and air pollution. WHO must continue its commitment to tobacco control and hope that an actual ‘new smoking’, with similar devastating effects as those caused by the tobacco industry, never emerges.
What this paper adds.
Labelling emerging health risks, such as prolonged sitting, as the new smoking is, according to previous studies, unwarranted and could have negative impacts on tobacco control.
Ambient air pollution has also been analogised as the ‘new smoking’, but comparing the historical trends of disease burdens attributable to ambient air pollution and to tobacco use, we conclude that ambient air pollution should not be called the new smoking because its attributable burden not only is significantly smaller but also has declined faster than that attributable to tobacco use in the last three decades.
Footnotes
Contributors: WG conceived the idea and drafted the manuscript. CPW conceived the idea and critically reviewed and revised the manuscript. MS re-organised the data, and critically reviewed and revised the manuscript. MH was involved in the early drafts, and critically reviewed and revised the manuscript. MH and MS helped with new revisions in response to referees’ comments and questions. All the authors approved the final manuscript as submitted, and agreed to be accountable for all aspects of the work.
Funding: MH is supported by a National Heart Foundation Australia Postdoctoral Fellowship, award number 101938. CPW is supported in part by Taiwan Ministry of Health and Welfare Clinical Trial Center (MOHW108-TDU-B-212-133004), China Medical University Hospital, Academia Sinica Stroke Biosignature Project (BM10701010021), MOST Clinical Trial Consortium for Stroke (MOST 108-2321-B-039-003-), Tseng-Lien Lin Foundation, Taichung, Taiwan and Katsuzo and Kiyo Aoshima Memorial Funds, Japan.
Disclaimer: The funding source had no role in study design, data collection, data analysis, data interpretation, writing of the report, or the decision to submit the paper for publication. The corresponding author had full access to all data in the study and had final responsibility for the decision to submit for publication.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Gray A. If you live in a big city you already smoke every day: World Economic Forum, 2018. Available: https://www.weforum.org/agenda/2018/05/if-you-live-in-a-big-city-you-already-smoke-every-day/
- 2. Biba E. The air is so bad in these cities, you may as well be smoking. Daily Beast 28 June 2018. [Google Scholar]
- 3. Mapping the Invisible Scourge The Economist London 2015.
- 4. Carrington D, Taylor M. Air pollution is the ‘new tobacco’, warns WHO head. The Guardian 27 October 2018. [Google Scholar]
- 5. Chau JY, Reyes-Marcelino G, Burnett AC, et al. Hyping health effects: a news analysis of the 'new smoking' and the role of sitting. Br J Sports Med 2019;53:1039–40. 10.1136/bjsports-2018-099432 [DOI] [PubMed] [Google Scholar]
- 6. Vallance JK, Gardiner PA, Lynch BM, et al. Evaluating the evidence on sitting, smoking, and health: is sitting really the new smoking? Am J Public Health 2018;108:1478–82. 10.2105/AJPH.2018.304649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Stanaway JD, Afshin A, Gakidou E, et al. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet 2018;392:1923–94. 10.1016/S0140-6736(18)32225-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ghebreyesus TA. Progress in beating the tobacco epidemic. Lancet 2019;394:548–9. 10.1016/S0140-6736(19)31730-1 [DOI] [PubMed] [Google Scholar]
- 9. Euromonitor International Tobacco in China 2019;36. [Google Scholar]
- 10. Campaign for Tobacco-Free Kids The global cigarette industry. Industry Watch 2018. [Google Scholar]
- 11. Vogel L. Antitobacco programs underfunded, WHO says. Can Med Assoc J 2011;183:E769–70. 10.1503/cmaj.109-3946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. WHO Report on the global tobacco epidemic, 2008: the MPOWER package. Geneva (Switzerland: World Health Organization, 2008. [Google Scholar]
- 13. Banks E, Joshy G, Weber MF, et al. Tobacco smoking and all-cause mortality in a large Australian cohort study: findings from a mature epidemic with current low smoking prevalence. BMC Med 2015;13:38 10.1186/s12916-015-0281-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. U.S. Department of Health and Human Services The health consequences of smoking—50 years of progress: a report of the surgeon General. 943 Atlanta, Georgia (USA): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Diseasese Prevention and Health Promotion, Office on Smoking and Health, 2014. [Google Scholar]
- 15. Dockery DW, Pope III CA. Lost life expectancy due to air pollution in China. Risk Dialogue Magazine 2014;17:5–11. [Google Scholar]
- 16. Zhang Y, West JJ, Mathur R, et al. Long-term trends in the ambient PM2.5- and O3-related mortality burdens in the United States under emission reductions from 1990 to 2010. Atmos Chem Phys 2018;18:15003–16. 10.5194/acp-18-15003-2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Centers for Disease Control and Prevention QuickStats: number of deaths from 10 leading causes — national vital statistics system, United States, 2010. Available: https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6208a8.htm?s_cid=mm6208a8_w
- 18. Cohen AJ, Brauer M, Burnett R, et al. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the global burden of diseases study 2015. Lancet 2017;389:1907–18. 10.1016/S0140-6736(17)30505-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Global Burden of Disease Study 2017 Global burden of disease study 2017 (GBD 2017) results. Seattle, Washington (United States of America): Institute for health metrics and evaluation (IHME), 2018. Available: https://http://vizhub.healthdata.org/gbd-compare/ [Accessed Apr 2019].
- 20. Wen CP, Gao W. PM2.5: an important cause for chronic obstructive pulmonary disease? Lancet Planet Health 2018;2:e105–6. 10.1016/S2542-5196(18)30025-1 [DOI] [PubMed] [Google Scholar]
- 21. Repace JL. Enemy No.1: Waging the war on Secondhand smoke: Repace associates, Inc 2019.
- 22. Boffi R, Ruprecht A, Mazza R, et al. A day at the European respiratory Society Congress: passive smoking influences both outdoor and indoor air quality. Eur Respir J 2006;27:862–3. 10.1183/09031936.06.00148505 [DOI] [PubMed] [Google Scholar]
- 23. Invernizzi G, Ruprecht A, Mazza R, et al. Particulate matter from tobacco versus diesel CAR exhaust: an educational perspective. Tob Control 2004;13:219–21. 10.1136/tc.2003.005975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Gao W, Sanna M, Branston JR, et al. Exploiting a low Tax system: non-tax-induced cigarette price increases in Taiwan 2011–2016. Tob Control 2019;28(e2:e126–32. 10.1136/tobaccocontrol-2018-054908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Greenpeace East Asia PM2.5 in Beijing down 54%, but nationwide air quality improvements slow as coal use increases. Beijing (China): Greenpeace International Press Desk, 2018. [Google Scholar]
- 26. Saner E. Never exercise at rush hour: six ways to avoid air pollution. The Guardian 8 October 2018. [Google Scholar]
- 27. Woodward A, Samet J. Active transport: exercise trumps air pollution, almost always. Prev Med 2016;87:237–8. 10.1016/j.ypmed.2016.03.027 [DOI] [PubMed] [Google Scholar]
- 28. Tainio M, de Nazelle AJ, Götschi T, et al. Can air pollution negate the health benefits of cycling and walking? Prev Med 2016;87:233–6. 10.1016/j.ypmed.2016.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]


