The pandemic of coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is rapidly evolving worldwide and is now face-to-face with another major pandemic ― diabetes mellitus. Both these pandemics are having enormous negative health, economic, and social consequences throughout the world. Emerging data consistently show that diabetes mellitus is associated with increased morbidity and mortality in COVID-19 patients [1], [2], recently confirmed in a very large epidemiological study of the UK General Practice population [3]. On the other hand, there have been reports of deterioration of glycemic control, including episodes of ketosis, ketoacidosis, or hyperosmolar hyperglycaemic state in type 2 diabetes patients with COVID-19, requiring exceptionally high doses of insulin [1], [4]. Further, recent reports show an increase in new-onset type 1 diabetes, possibly linked to COVID-19, firstly in a US-based population [5] and subsequently, in a cohort of children living in North West London [6]. These clinical observations provide new evidence for new-onset diabetes in COVID-19 patients.
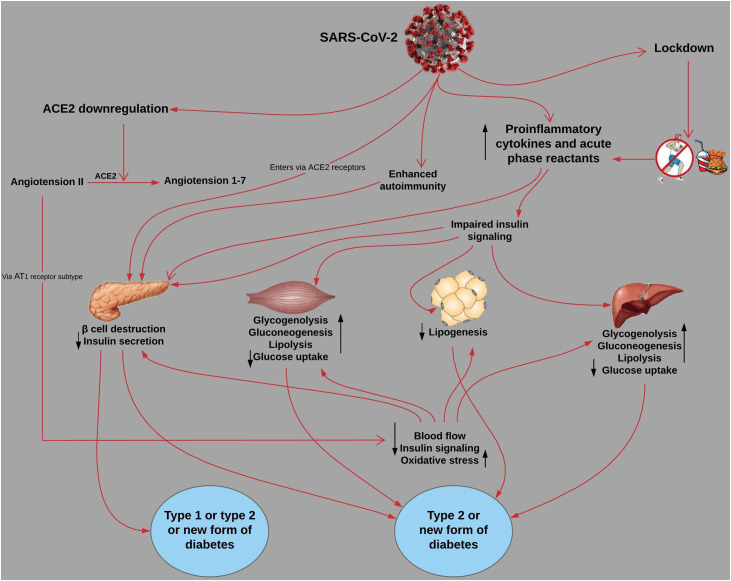
As a result, there is a pressing need to characterize not only the clinical but also the pathophysiological phenotype of COVID-19-related diabetes. Here, we discuss potential pathways whereby COVID-19 might increase the risk of developing diabetes. This includes, but not limited to, injury to the pancreatic β cells, an exaggerated proinflammatory cytokine response, activation of the renin-angiotensin system (RAS), and changes in health behaviours during this pandemic (Fig. 1 ). None of these possibilities is exclusive on its own, and as we discuss below, several of these factors may combine to play a role for either the development or progression of type 1 or 2 diabetes or, in fact, result in a new form of diabetes.
Fig. 1.
Potential metabolic and inflammatory pathways between COVID-19 and new-onset diabetes. ACE2, angiotension-converting enzyme.2.
SARS-CoV-2 uses angiotensin-converting enzyme 2 (ACE2) as its receptor to gain entry into human cells [7]. ACE2 is expressed widely in metabolic organs and tissues, including the pancreatic β cells, as reported more than 15 years ago [8]. A recent organoid study showed that pancreatic β cells are permissive to SARS-CoV-2 [9], and an autopsy study on three deceased COVID-19 patients in China found degeneration of some islet cells in the pancreas [10]. SARS-CoV-2 could further damage the β cells by triggering a plethora of proinflammatory cytokines (e.g., Interleukin-6) and acute phase reactants (e.g., C-reactive protein) [11], or by enhancing autoimmunity in genetically predisposed individuals. This destruction of β cells by SARS-CoV-2 presumably via ACE2 is relevant to both type 1 and type 2 diabetes where insulin deficiency plays a key role. Whereas in type 1 diabetes, insulin deficiency occurs at least in part as a result of autoimmune processes, in type 2 diabetes, insulin deficiency can be the predominant abnormality as recently described by several groups [12], [13] or can develop as a result of glucotoxicity to β cells after a period of hyperglycaemia induced by insulin resistance [14].
Proinflammatory pathways leading to chronic low-grade inflammation in sites such as adipose tissue are considered to play increasingly important roles in the pathogenesis and progression of type 2 diabetes [15]. The inflammatory molecules activated by SARS-CoV-2 infection could impair insulin signalling as has been reported for numerous cytokines such as tumour necrosis factor-α [16], albeit not yet proven in the COVID-19 context. Indeed, this could, in turn, inhibit insulin-stimulated glycogen synthesis and glucose uptake in the skeletal muscle and liver, as well as lipogenesis in the adipose tissue, thereby conferring hyperglycaemia and insulin resistance [16].
ACE2 is a key enzyme in the RAS, where it catalyzes the conversion of angiotensin II, the classical effector molecule of this pathway and a powerful vasoconstrictor, to the vasodilator, angiotensin 1–7. After endocytosis, SARS-CoV-2 downregulates ACE2 expression [7], resulting in unopposed deleterious actions of angiotensin II (primarily through the AT1 receptor subtype). These effects include reduction in blood flow to tissues, impairment of insulin signalling, and an increase in oxidative stress. Consequently, insulin secretion decreases, and lipolysis, glycogenolysis, and gluconeogenesis increase in the liver and skeletal muscle, leading to insulin resistance [16], [17]. It remains uncertain as to the pathophysiological relevance of the effects of angiotensin II on glucose homeostasis with only modest beneficial effects on reducing susceptibility to diabetes with drugs that interrupt the RAS such as ACE inhibitors and angiotensin II receptor blockers [16], [17].
The COVID-19 pandemic has disrupted the ongoing prevention and control efforts for non-communicable diseases (NCDs) at the individual, community, and health system level in many countries. A recent survey by the World Health Organization among 155 countries shows that more than half (53%) have stopped their preventive and treatment services for NCDs either partially or completely [18]. Stay-at-home orders, self-isolation, and social distancing measures are crucial to flatten the curve of this disease. However, these measures are having negative impacts, including reduced physical activity, unhealthy eating, and weight gain [19]. These changes in lifestyle have numerous pathophysiological effects, including promoting insulin resistance via a range of well-described mechanisms (e.g., triggering inflammatory pathways), which would presumably increase the risk of new-onset diabetes in high-risk individuals.
It is crucial to establish a full understanding of the impact of COVID-19 on the risk of developing diabetes in order to inform clinical care because countries that are currently severely affected by COVID-19 have a large number of at-risk people for diabetes, including the USA, UK, India, and Brazil [20]. The global registry of patients with COVID-19-related diabetes (covidiab.e-dendrite.com) should help in leading to a better understanding of the natural course of the onset of COVID-related diabetes and assist in providing clues as to which underlying mechanisms should be further elucidated [21]. There is still much that we need to learn about COVID-19, and there may yet be other mechanisms that come into play to explain the association between COVID-19 and new-onset diabetes. We now have the situation of arguably the two major pandemics of the 21st Century colliding!
Conflicts of interests
None.
References
- 1.Bornstein S.R., Rubino F., Khunti K., Mingrone G., Hopkins D., Birkenfeld A.L. Practical recommendations for the management of diabetes in patients with COVID-19. Lancet Diabetes Endocrinol. 2020;8:546–550. doi: 10.1016/S2213-8587(20)30152-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Targher G., Mantovani A., Wang X.B., Yan H.D., Sun Q.F., Pan K.H. Patients with diabetes are at higher risk for severe illness from COVID-19. Diabetes Metab. 2020;46:335–337. doi: 10.1016/j.diabet.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barron E., Bakhai C., Kar P., Weaver A., Bradley D., Ismail H. Associations of type 1 and type 2 diabetes with COVID-19-related mortality in England: a whole-population study. Lancet Diabetes Endocrinol. 2020;8:813–822. doi: 10.1016/s2213-8587(20)30272-2. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Scheen A.J., Marre M., Thivolet C. Prognostic factors in patients with diabetes hospitalized for COVID-19: findings from the CORONADO study and other recent reports. Diabetes Metab. 2020;46:265–271. doi: 10.1016/j.diabet.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ebekozien O.A., Noor N., Gallagher M.P., Alonso G.T. Type 1 diabetes and COVID-19: preliminary findings from a multicenter surveillance study in the U.S. Diabetes Care. 2020;43:e83–e85. doi: 10.2337/dc20-1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Unsworth R., Wallace S., Oliver N.S., Yeung S., Kshirsagar A., Naidu H. New-onset type 1 diabetes in children during COVID-19: multicenter regional findings in the U.K. Diabetes Care. 2020;43:e170–e171. doi: 10.2337/dc20-1551. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 7.Hoffmann M., Kleine-Weber H., Schroeder S., Krüger N., Herrler T., Erichsen S. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271–280. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tikellis C., Wookey P.J., Candido R., Andrikopoulos S., Thomas M.C., Cooper M.E. Improved islet morphology after blockade of the renin- angiotensin system in the ZDF rat. Diabetes. 2004;53:989–997. doi: 10.2337/diabetes.53.4.989. [DOI] [PubMed] [Google Scholar]
- 9.Yang L., Han Y., Nilsson-Payant B.E., Gupta V., Wang P., Duan X. A human pluripotent stem cell-based platform to study SARS-CoV-2 tropism and model virus infection in human cells and organoids. Cell Stem Cell. 2020;27:125–136. doi: 10.1016/j.stem.2020.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yao X.H., Li T.Y., He Z.C., Ping Y.F., Liu H.W., Yu S.C. A pathological report of three COVID-19 cases by minimal invasive autopsies. Zhonghua Bing Li Xue Za Zhi. 2020;49:411–417. doi: 10.3760/cma.j.cn112151-20200312-00193. [DOI] [PubMed] [Google Scholar]
- 11.Ahlqvist E., Storm P., Käräjämäki A., Martinell M., Dorkhan M., Carlsson A. Novel subgroups of adult-onset diabetes and their association with outcomes: a data-driven cluster analysis of six variables. Lancet Diabetes Endocrinol. 2018;6:361–369. doi: 10.1016/S2213-8587(18)30051-2. [DOI] [PubMed] [Google Scholar]
- 12.Kahn S.E., Cooper M.E., Del Prato S. Pathophysiology and treatment of type 2 diabetes: perspectives on the past, present, and future. Lancet. 2014;383:1068–1083. doi: 10.1016/S0140-6736(13)62154-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zaharia O.P., Strassburger K., Strom A., Bönhof G.J., Karusheva Y., Antoniou S. Risk of diabetes-associated diseases in subgroups of patients with recent-onset diabetes: a 5-year follow-up study. Lancet Diabetes Endocrinol. 2019;7:684–694. doi: 10.1016/S2213-8587(19)30187-1. [DOI] [PubMed] [Google Scholar]
- 14.Sell H., Habich C., Eckel J. Adaptive immunity in obesity and insulin resistance. Nat Rev Endocrinol. 2012;8:709–716. doi: 10.1038/nrendo.2012.114. [DOI] [PubMed] [Google Scholar]
- 15.Hotamisligil G.S., Shargill N.S., Spiegelman B.M. Adipose expression of tumor necrosis factor-alpha: direct role in obesity-linked insulin resistance. Science. 1993;259:87–91. doi: 10.1126/science.7678183. [DOI] [PubMed] [Google Scholar]
- 16.Jandeleit-Dahm K.A., Tikellis C., Reid C.M., Johnston C.I., Cooper M.E. Why blockade of the renin-angiotensin system reduces the incidence of new-onset diabetes. J Hypertens. 2005;23:463–473. doi: 10.1097/01.hjh.0000160198.05416.72. [DOI] [PubMed] [Google Scholar]
- 17.Scheen A.J. Renin-angiotensin system inhibition prevents type 2 diabetes mellitus. Part 2. Overview of physiological and biochemical mechanisms. Diabetes Metab. 2004;30:498–505. doi: 10.1016/s1262-3636(07)70147-7. [DOI] [PubMed] [Google Scholar]
- 18.World Health Organization COVID-19 significantly impacts health services for noncommunicable diseases. 2020. https://www.who.int/news-room/detail/01-06-2020-covid-19-significantly-impacts-health-services-for-noncommunicable-diseases [Accessed 16 June 2020]
- 19.Ammar A., Brach M., Trabelsi K., Chtourou H., Boukhris O., Masmoudi L. Effects of COVID-19 home confinement on eating behaviour and physical activity: results of the ECLB-COVID19 international online survey. Nutrients. 2020;12:1583. doi: 10.3390/nu12061583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.International Diabetes Federation . 9th ed. Brussels; Belgium: 2019. IDF diabetes atlas. [Google Scholar]
- 21.Rubino F., Amiel S.A., Zimmet P., Alberti G., Bornstein S., Eckel R.H. New-onset diabetes in Covid-19. N Engl J Med. 2020;383:789–790. doi: 10.1056/NEJMc2018688. [DOI] [PMC free article] [PubMed] [Google Scholar]