Abstract
Introduction
Both the COVID-19 pandemic and its management have had a negative impact on mental health worldwide. There is a growing body of research on mental health as it relates to the pandemic. The objective of this study is to use bibliometric analyses to assess the mental health research output related to the COVID-19 pandemic and compare it to that of the West Africa Ebola and H1N1 outbreaks.
Methodology
We performed comprehensive searches in Embase, PubMed, and Scopus databases, and included all types of documents related to the three outbreaks published since the respective beginnings up to August 26, 2020.
Results
Despite the shorter time since the beginning of the COVID-19 pandemic, relative to Ebola and H1N1, we found a much greater number of mental health documents related to COVID-19 (n = 3070) compared to the two other outbreaks (127 for Ebola and 327 for H1N1). The proportion of documents in the top 10% journals was 31% for COVID-19, 24% for Ebola, and 40% for H1N1. Authors affiliated with institutions located in high-income countries published or contributed to 79% of all documents followed by authors from upper-middle-income countries (23%), lower-middle-income countries (10%), and low-income countries (2%). Approximately 19% of the documents reported receiving funding and 23% were the product of international collaboration.
Conclusion
Mental health research output is already greater for COVID-19 compared to Ebola and H1N1 combined. A minority of documents reported funding, was the product of international collaboration, or was published by authors located in low-income countries during the three outbreaks in general, and the COVID-19 pandemic in particular.
Keywords: Mental health, Psychiatry, COVID-19, Ebola, H1N1, Bibliometrics
1. Introduction
After the emergence of pneumonia of unknown causes in late 2019 in Wuhan, China, a new coronavirus, SARS-COV2, was identified. On March 11, 2020, the World Health Organization (WHO) announced alarming concerns regarding the new virus and characterized it as the COVID-19 pandemic (Neilson et al., 2020; WHO, 2020c). As of August 26, 2020, 216 countries, areas, or territories were swept by the pandemic, 23,752,965 people have been infected, and 815,038 died as a result of the virus (WHO) (WHO, 2020a). The death rate reached 15% in some countries (Worldmeter, 2020b). Distribution of confirmed cases varies by continent and countries, but the bulk extends over the Americas and Asia, with 13,885,026 and 7,365,080 infected individuals, respectively (Worldmeter, 2020d). According to the Scopus database, on August 26, 2020, there were over 43,000 articles, letters, editorials, notes, reviews, and case reports published on COVID-19 and, per PubMed, thousands more were accepted for publication.
The impact of the COVID-19 pandemic on mental health has been of immense interest to international health organizations (WHO, 2020b), national health agencies (CDC, 2020), and psychiatric and other mental health researchers. Recently published studies reported an increasing rate of psychological distress, traumatization, and suicide in relation to COVID-19 (Reger et al., 2020). For example, in an online survey in China, 29% of respondents reported moderate to severe anxiety symptoms, while 17% reported depressive symptoms (Wang et al., 2020).
Research has also found a negative impact of COVID-19 public health interventions on mental health. For example, the strictly implemented measures of social distancing led to various negative psychological consequences associated with a prolonged quarantine duration, fear of catching the infection, disturbed routine, and lack of adequate supplies and information about the virus (Brooks et al., 2020). The post-pandemic phase is even more unsettling due to the increasing rates of post-traumatic stress disorder (PTSD) and other mental health sequelae (Dutheil et al., 2020).
Mental health researchers have also been interested in the impact of other infectious disease outbreaks on mental health and the mental health response to those outbreaks. Two prominent examples are the H1N1 influenza outbreak in 2009 and the Ebola virus disease (EVD) outbreak in 2014. For example, one study reported on fear and anxiety as common reactions during the H1N1 pandemic (Taha et al., 2014) and another study related to EVD reported that the burden of the disease on mental health continued to linger in the aftermath (Reardon, 2015). Interestingly, while a high level of H1N1-related anxiety was associated with compliance to preventive measures (Bults et al., 2011), fear of exposure or stigmatization during the EVD epidemic prevented individuals from seeking help and thus hastened viral transmission (O'Leary et al., 2018).
COVID-19, H1N1, and EVD vary in their epidemiological characteristics and general prevalence of associated mental distress and disorders. We have summarized these differences in Table 1 .
Table 1.
Comparison of COVID-19, EVD, and H1N1 outbreaks’ characteristics.
| H1N1 (2009) | EVD (2014–2016) | COVID (2019 – ongoing) | |
|---|---|---|---|
| Duration of outbreaks | Mid-April 2009 (CDC, 2009) – August 10, 2010 (WHO) | December 2013–June 2016 (CDC, 2019b) | December 2019 – ongoing |
| Reproduction Number R0 | 1.46–1.48 (Eisenberg, 2020) | 1.51–2.53 (Eisenberg, 2020) | 1.5–3.5 (Eisenberg, 2020) |
| Case fatality rate | 2–3% (Sarukhan, 2016) | 70% (Sarukhan, 2016) | <0.1% - >25% (WHO, 2020) |
| Total number of cases and total number of deaths | 60.8 million cases and 12,469 deaths (CDC, 2019a) | >28,600 cases and 11,325 deaths (CDC, 2019b) | 24,654,965 cases and 836,112 deaths (Worldmeter, 2020c) |
| Incubation period (days) | 1–4 (Siddiqui, 2020) | 2–21 (Sarukhan, 2016) | 2- 14 (Worldmeter, 2020a) |
| Number of affected countries | >214 countries (CDC, 2010) | 10 countries (CDC, 2019b) | 216 (WHO, 2020a) |
| General prevalence of mental disorders | Emotional distress: 6% (Lau et al., 2010) | Depression 12–75%, Anxiety 27.5–83.3%, PTSD 40% (Cénat et al., 2020) | Depression 17%,- 28%, Anxiety 21–32%, Insomnia 7–24% (Rossi et al., 2020; Shi et al., 2020) |
Before the COVID-19 outbreak, humanity faced two other coronavirus epidemics; namely, SARS in 2002 and MERS in 2012. Out of the five outbreaks that occurred during the past two decades, COVID-19, EVD, and H1N1 have infected more people worldwide as compared to SARS and MERS which were associated with elevated case fatality rates of 11% and 35%, respectively (Sarukhan, 2016).
The current study focuses on the most recent coronavirus outbreak (i.e., COVID-19), and EVD and H1N1. Our objective is to use bibliometric analyses to assess the mental health research output related to the COVID-19 pandemic and compare it to that of EVD and H1N1 outbreaks. We specifically aimed to identify the publications’ numbers, types, venues, origins, levels of funding, and levels of collaboration.
2. Methodology
2.1. Database selection
We used Embase, PubMed, and Scopus databases to identify relevant documents. Embase and PubMed are the two largest biomedical databases in the world, indexing, as of August 26, 2020, over 15,000,000 documents since 2010: 93.5% in English and the remaining in Chinese (1.6%), German (1.1%), Spanish (0.8%), French (0.8%), and over 50 other languages (2.2%). Scopus is the largest multidisciplinary bibliographic and citation database in the world, indexing, as of August 26, 2020, approximately 30,500,000 documents since 2010: 90.8% in English and the remaining in Chinese (3.3%), German (1.1%), Spanish (1.1%), French (0.9%), and over 50 other languages (2.7%).
2.2. Search strategy
To be as inclusive as possible, we carried out comprehensive searches for documents that included in the title, abstract, or keywords fields both terms and phrases related to mental health and the infectious outbreaks in question. We made use of controlled vocabularies in Embase (Emtree) and PubMed (MeSH) and assumed that all retrieved documents are relevant. Please see Appendix I for the search queries in each database. We included all document types retrieved from the databases in all languages covered in the databases from the beginning of each outbreak until August 26, 2020 (from 2009 on in the case of H1N1, 2014 in the case of EVD, and 2019 on in the case of COVID-19). We excluded 20 documents classified as corrections. Our searches retrieved 3524 documents in total, including 1912 articles, 798 letters, 309 editorials, 248 reviews, 233 notes, 18 short surveys, and 6 chapters (all referred to hereafter as documents).
2.3. Indicators
For each of the three infectious diseases, we extracted the following data:
-
1
Number of documents by disease;
-
2
Number of documents published in Open Access format, as a measure of accessibility;
-
3
Number of documents by country, based on affiliation information provided for each document. We gave equal full credit for each country represented in each document. We also specified the number of documents by country for each outbreak alone as well as the total number of documents by country for the three outbreaks together;
-
4
Number of documents by countries' income. We categorized countries into four groups according to the World Bank classification: high-income countries, upper-middle-income countries, lower-middle-income countries, and low-income countries. We then calculated for each outbreak, the total number of documents in each of the four income categories;
-
5
Proportion of documents in high impact journals, defined as the top 10% journals in their respective fields per Scopus's CiteScore;
-
6
Proportion of documents with authors from more than one country, as a measure of international collaboration; and
-
7
Percentage of documents receiving internal or external funding as recorded by the Scopus database.
2.4. Data analysis
We exported the data and analyzed them using Microsoft Excel and Access 2016. We analyzed all indicators using frequency analysis and cross-tabulations where necessary. We compared findings for the three outbreaks, then compared them by country income level and funding, and finally assessed the patterns of collaboration between countries. The assessment of international collaboration included the proportion of documents with authors from more than one country and social network analyses using the VOSviewer software. Where necessary, we supported our claims by comparing results of outbreak-related mental health research against those of the larger fields of “psychiatry and mental health” and “medicine” as defined by Scopus. In Scopus, the field of “psychiatry and mental health” is composed of 501 active journals and “medicine” of 6452 such journals.
3. Results
3.1. Number of publications overall, by country, and by income level
The number of documents published on mental health aspects of the three outbreaks was as follows: 3070 on COVID-19 in less than a year since the first case was officially reported, 127 on West African Ebola since late 2013, and 327 documents on H1N1 since 2009. When examining research productivity by country (Table 2 ), we observed the following:
-
-
The United States and the United Kingdom have contributed the most to research on all three outbreaks;
-
-
The United States, the United Kingdom, Canada, China, and France rank among the top 10 contributors on all three outbreaks;
-
-
Australia, Germany, Italy, and Switzerland are the only other four countries that rank among the top 10 most published on two of the three outbreaks; and
-
-
As of August 26, 2020, there were publications from 108 countries on mental health aspects of COVID-19, compared to 39 on Ebola, and 52 on H1N1 (see Appendix II)
Table 2.
Research productivity by country.
| COVID-19 | Ebola | H1N1 | |||
|---|---|---|---|---|---|
| United States | 950 (31%) | United States | 60 (48%) | United States | 101 (31%) |
| United Kingdom | 425 (14%) | United Kingdom | 29 (24%) | United Kingdom | 36 (11%) |
| China | 363 (12%) | Sierra Leone | 16 (13%) | Sweden | 30 (9%) |
| Italy | 290 (9%) | France | 10 (8%) | Germany | 24 (7%) |
| India | 206 (7%) | Switzerland | 10 (8%) | Finland | 24 (7%) |
| Australia | 174 (6%) | Liberia | 9 (7%) | Italy | 24 (7%) |
| Canada | 170 (6%) | Canada | 9 (7%) | France | 21 (6%) |
| Spain | 127 (4%) | Uganda | 6 (6%) | Canada | 18 (6%) |
| France | 116 (4%) | Australia | 6 (5%) | China | 18 (6%) |
| Germany | 103 (3%) | China | 6 (5%) | Switzerland | 14 (4%) |
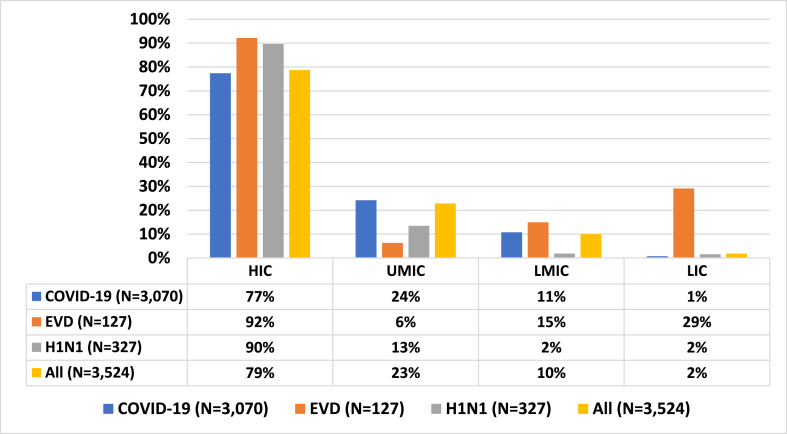
As far as income is concerned, authors affiliated with institutions located in high-income countries (HIC) published or contributed to 79% of all documents, followed by authors from upper-middle-income countries (UMIC) (23%), lower-middle-income countries (LMIC) (10%), and low-income countries (LIC) (2%).
When we looked at the distribution of publications per countries’ income during each of the three outbreaks, we found a decrescendo pattern during COVID-19 and H1N1 contrasting with a bimodal distribution during EVD. HIC contributed to 77% and 90% of the total research output during COVID-19 and H1N1, respectively, followed by a contribution from UMIC of 24% and 13%. HIC participated in 92% of mental health research output, maintaining by that a leading position during the EVD epidemic, while LMICs and LICs were found to have a noticeable rate of contribution of 15% and 29%, respectively, during EVD, despite their negligible contribution during all outbreaks in general. UMIC participated in only 6% of mental health research output related to EVD. Finally, only on Ebola, there are LIC countries represented among the top 10 most published countries, including Sierra Leone, Liberia, and Uganda and no LMIC country is among the topmost published on any outbreak (see Table 2).
We should emphasize here that about 12% of the total publication on the mental health aspects of COVID-19 were about health care workers as compared to 25% of the EVD publications and 2% of publications on H1N1 (see Fig. 1 ).
Fig. 1.
Proportion of documents by countries' income levels.
3.2. Characteristics of publications
The proportion of outbreak-related mental health documents published in the top 10% journals per Scopus's CiteScore was 31% for COVID-19, 24% for EVD, and 40% for H1N1. These percentages for outbreak-related mental health were, in the cases of COVID-19 and H1N1, considerably higher than the percentages for “psychiatry and mental health” and “medicine” overall research fields (see Table 3 ).
Table 3.
Proportion of documents in the top 10% journals.
| Time-period | Outbreak-related mental health | Psychiatry and mental health | Medicine |
|---|---|---|---|
| 2020 | 31% (COVID-19) | 21% | 23% |
| 2014–2020 | 24% (EVD) | 21% | 22% |
| 2009–2020 | 40% (H1N1) | 22% | 23% |
Source: SciVal (August 2020).
Concerning research accessibility, the proportion of outbreak-related mental health documents published in Open Access format was 81% for COVID-19, 57% for Ebola, and 32% for H1N1. These percentages for outbreak-related mental health were remarkably larger than the proportions for psychiatry, mental health, and medicine research fields in general (see Table 4 ).
Table 4.
Proportion of documents published in Open Access format.
| Time-period | Outbreak-related mental health | Psychiatry and mental health | Medicine |
|---|---|---|---|
| 2020 | 81% (COVID-19) | 30% | 41% |
| 2014–2020 | 57% (EVD) | 24% | 35% |
| 2009–2010 | 32% (H1N1) | 20% | 30% |
Source: Scopus (August 2020).
As shown in Table 5 , of all published documents, the proportion of outbreak-related mental health documents reporting funding was 18% for COVID-19, 20% for EVD, and 22% for H1N1. During COVID-19 particularly, the percentage of funded “outbreak-related mental health research” was remarkably lower than the funding received for “psychiatry and mental health” research (35%) and “medicine” research (32%).
Table 5.
Proportion of documents reporting funding.
| Time-period | Outbreak-related mental health | Psychiatry and mental health | Medicine |
|---|---|---|---|
| 2020 | 18% (COVID-19) | 35% | 32% |
| 2014–2020 | 20% (EVD) | 32% | 24% |
| 2009–2020 | 22% (H1N1) | 26% | 18% |
3.3. Collaboration
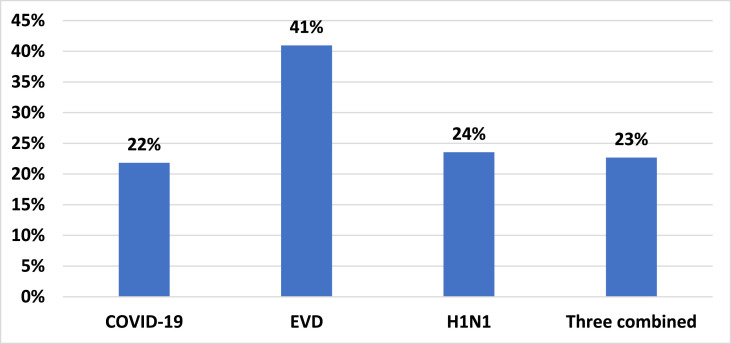
In terms of the proportion of documents with authors from more than one country, 23% of mental health research related to all three diseases had multinational co-authorship. While 41% of EVD mental health publications were the product of international collaboration, only 22% of the total COVID-19 mental health research and 24% H1N1 mental health-related publications resulted from such collaboration (Fig. 2).
Fig. 2.
Percent of documents with international collaboration.
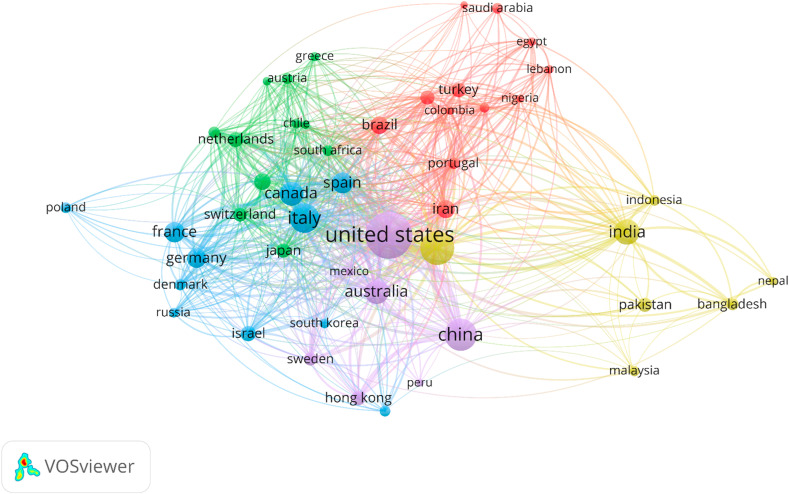
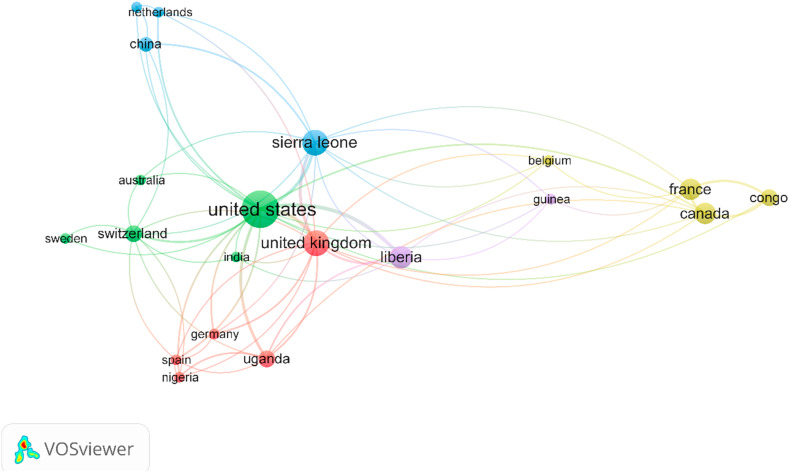
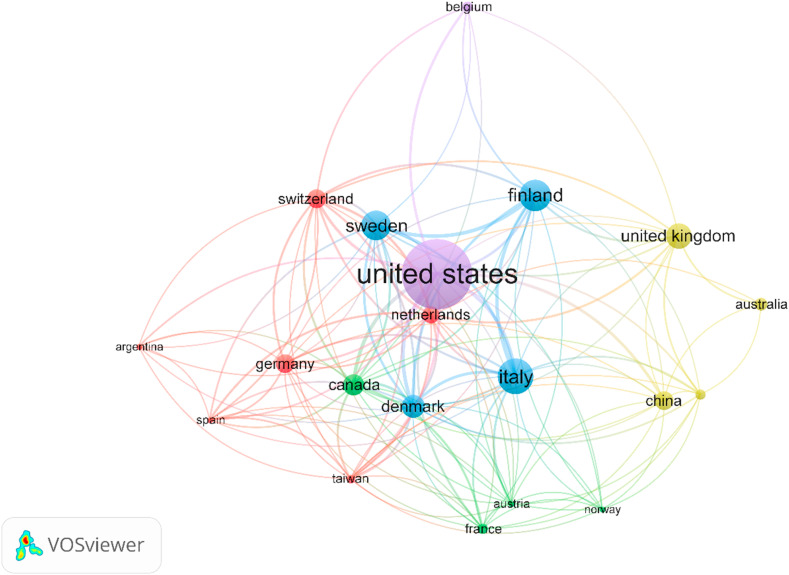
Fig. 3, Fig. 4, Fig. 5 represent the network analysis of international collaboration in mental health research during COVID-19, EVD, and H1N1, respectively. In these figures, each node corresponds to the country contributing to mental health research, and its density is relative to the amount of research from the corresponding country. Countries with shared co-authorship are connected with lines of the same color as the node. The line's density is relative to the intensity of multinational collaboration.
Fig. 3.
Network analysis of International collaboration during COVID-19 outbreak.
Fig. 4.
Network analysis of International collaboration during the Ebola outbreak.
Fig. 5.
Network analysis of International collaboration during the H1N1 outbreak.
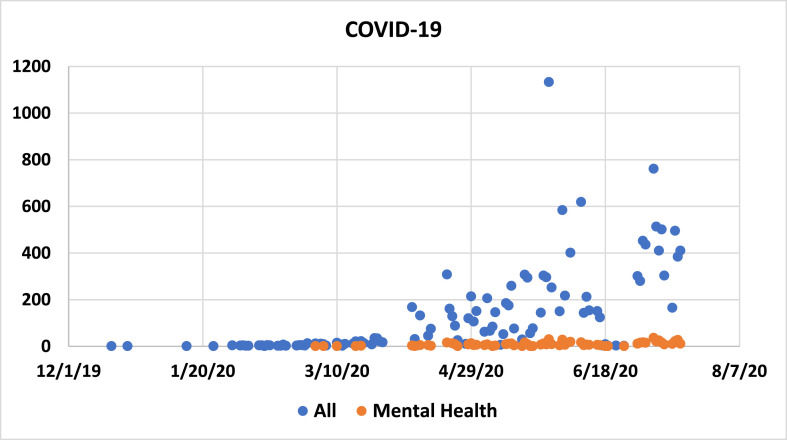
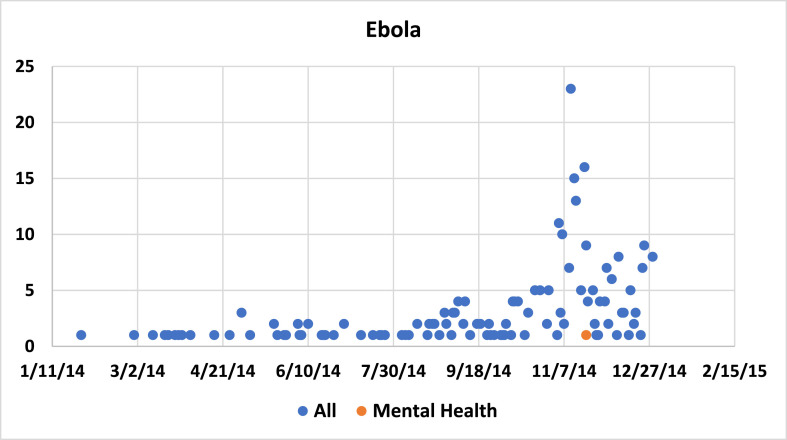
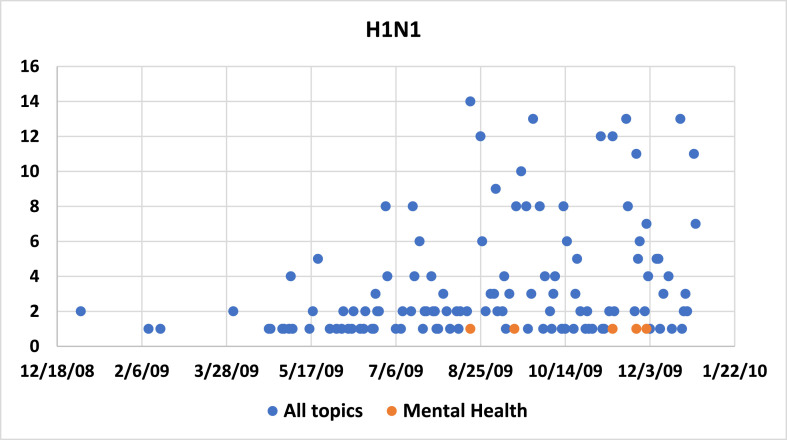
3.4. Timeframe of research output onset
Graph 1, Graph 2, Graph 3 represent the timeframe difference between the onset of research in mental health as compared to all other non-mental health research following the outbreak of each of the three infectious diseases COVID-19, EVD, and H1N1, respectively. The onset and rate of mental health publications lagged behind the onset of publications in other fields during all three outbreaks. Eleven and eight months had passed before the first mental health publications appeared after the onset of EVD and H1N1 outbreaks, respectively. However, the first COVID-19 related mental health paper was published only three months following the onset of the outbreak.
Graph 1.
Timeframe difference between the onset of research in mental health and those of other fields during COVID-19.
Graph 2.
Timeframe difference between the onset of research in mental health and those of other fields during Ebola.
Graph 3.
Timeframe difference between the onset of research in mental health and those of other fields during H1N1.
4. Discussion
This is the first bibliometric analysis of mental health research output during three major infectious disease outbreaks that took place over the last decade or so, namely H1N1, Ebola, and COVID-19. Although it has been less than a year since the beginning of the COVID-19 outbreak, we found that the number of related publications on mental health has by far exceeded the number of publications on the mental health aspects of the other two outbreaks combined. There was a higher proportion of documents on mental health during infectious disease outbreaks that were published in the top 10% journals as compared to documents in medicine or mental health in general. Conversely, mental health research related to COVID-19 received considerably less funding compared to medical research in general, whereas mental health research related to Ebola and H1N1 received considerably less funding compared to psychiatry and mental health research in general. In addition, less than a quarter of the publications were the product of international collaboration among all three outbreaks together. While high-income countries contributed to the overwhelming majority of publications, there was, not surprisingly, some correlation between the publishing country and the geographical origin of the outbreak. There was also a higher proportion of publications on health care workers and mental health in relation to EVD as compared to the two other outbreaks.
The bibliometric approach used in the current study is comprehensive as we included all types of documents available in any language from three distinct, comprehensive databases: Embase, PubMed, and Scopus. Additionally, the choice of phrases and terms related to mental health and each of the outbreaks was exhaustive. Unlike prior analyses of the scientific literature on coronaviruses, ours did not limit to records in English (Liu et al., 2020; Nowakowska et al., 2020; Tao et al., 2020; Zhai et al., 2020) or English and Chinese only (Yu et al., 2020). We additionally extracted records from more than two databases (Haghani et al., 2020; Liu et al., 2020) and included editorials, commentaries, letters, case reports, news, and narrative reviews (Liu et al., 2020; Yu et al., 2020). In addition to looking at the number and countries of origin of publications, we also examined indicators related to international collaboration, funding, and research visibility.
Recently published bibliometric analyses either looked at research output on various scientific and medical topics of all coronavirus outbreaks including the Severe Acute Respiratory Syndrome (SARS) and the Middle East Respiratory Syndrome (MERS) (Bonilla-Aldana et al., 2020; Haghani et al., 2020; Liu et al., 2020; Tao et al., 2020; Yu et al., 2020; Zhai et al., 2020) or were limited to the current COVID-19 pandemic overall (De Felice and Polimeni, 2020; Nowakowska et al., 2020). Our study is unique in that it examined an underexplored area in the COVID-19 research (Liu et al., 2020), namely, the trend in mental health research, and compared the findings with two prior distinct viral outbreaks.
Our study, however, has a couple of limitations. Although we tried to be as inclusive as possible using three different databases, there may be publications that are not captured by Embase, PubMed, and Scopus. Also, since the COVID-19 pandemic is still evolving, our results do not represent the complete course of the fast-growing literature of the current pandemic.
It was not surprising that the number of publications on COVID-19 related mental health publications was much higher than that of the other two outbreaks combined. These results are explained by the relative magnitude of the different outbreaks. For example, the death toll registered for COVID-19 during the first six months of the outbreak exceeded the total deaths during the first two years of the EVD epidemic and is close to the estimated death toll during 18 months of the H1N1 pandemic (CDC, 2009; 2010; 2019a; 2019b; Worldmeter, 2020c). Furthermore, unlike the more localized EVD epidemic (CDC, 2019b), the transcontinental spread of the current COVID-19 pandemic (Worldmeter, 2020b), although similar in its geographical distribution to the H1N1 pandemic (CDC, 2010), has precipitated an unusual global economic, social, and geopolitical crises (Nicola et al., 2020). These have resulted in mental health distress among the general public (Alradhawi et al., 2020). The proportion of publications about health care workers was higher for EVD as compared to the other two outbreaks. This may be due to the high fatality rate of EVD and the stigma associated with it as compared to COVID-19 which puts health care workers at higher risk for mental health disorders (Cénat et al., 2020; Rossi et al., 2020; Shi et al., 2020).
We also found a gradual increase in Open Access publications in mental health research during infectious outbreaks from 32% during H1N1 up to 81% during the COVID-19 pandemic. Although a similar trend was observed for publications in medicine and mental health in general, the proportion of Open Access publications in mental health aspects of COVID-19 was double that observed for mental health in general (Piwowar et al., 2018). Besides seeking higher citations associated with Open Access articles (Piwowar et al., 2018), researchers likely aimed at making their research results as widely accessible as possible during outbreaks in general and COVID-19 pandemic in particular (Eysenbach, 2006).
Most of the mental health research during COVID-19 originated from the United States, China, and the United Kingdom. Publications on mental health and EVD, specifically, came predominately from the United States or were led by American authors even when co-authored by researchers from West African countries. This may explain why international collaboration is much more evident in EVD research as compared to COVID-19 and H1N1. This is also in-line with our findings that only a small minority (12%) of research about mental health in any of the three outbreaks included authors from low and low-middle-income countries. Indeed, it has been previously reported that only 6% of the mental health literature is published from regions of the world that account for over 90% of the global population (Helal et al., 2011; Patel and Kim, 2007; Zeinoun et al., 2020). Acceptance bias, low submission rate, and low quality of submitted research are likely reasons for these geographical disparities (Patel and Sumathipala, 2001).
The proportion of publications on mental health-related to the outbreaks that reported receiving funding was lower than the proportion of publications on general mental health that reported receiving funding. This difference may be because, amid an outbreak, investigators do not have time to seek funding and seem to prioritize getting much-needed evidence out to the scientific community over waiting for projects to get funded. In addition, in many parts of the world, mental health is still not a research priority for major funding agencies (Maalouf et al., 2019). Interestingly, however, despite receiving less funding, the proportion of publications on mental health aspects of the outbreaks published in the top 10% journals was remarkably higher than that of medicine and mental health overall.
5. Clinical implications
Despite the time lag between the first studies on all three outbreaks in general and the first studies on mental health aspects of the outbreaks in particular, research output in the latter area follows an upward trend similar to that of other research areas. Indeed, previous bibliometric analyses found increased output in microbiological, epidemiological, and clinical research of coronaviruses that peaked one to two years following SARS and MERS outbreaks (Haghani et al., 2020; Nowakowska et al., 2020; Tao et al., 2020). The gradual increase in mental health research over time is important for all pandemics, particularly COVID-19, given the dire need for generating evidence to guide best practices.
The impact of the COVID-19 pandemic extends beyond infected individuals and healthcare workers. While quarantine is a common denominator for all infectious outbreaks (Tognotti, 2013), widespread lockdown and social distancing were essential public health tools used in the COVID 19 pandemic (News, 2020). On the one hand, strict lockdown measures increased worries about physical health, anger, impulsivity, suicidal ideations as well as symptoms of anxiety, depression, insomnia, and PTSD among mentally ill patients. On the other hand, access to direct emergency and outpatient psychiatric care was reduced (Hao et al., 2020). Consequently, mental health practitioners and policymakers called for research on regulations and implementations of alternative clinical interventions, such as telepsychiatry (Kannarkat et al., 2020; Shore et al., 2020).
6. Research implications
This is the first bibliometric analysis of mental health research comparing research aspects of the three infectious disease outbreaks that took place over the last decade or so, namely H1N1, Ebola, and COVID-19. The analysis shows rapid exponential growth in the number of mental health research during outbreaks. Our study also highlights the paucity of funding, collaboration, and contribution of LIC to mental health research during all outbreaks in general but more importantly during the current COVID-19 pandemic. Albeit the increased awareness of the short- and long-term psychological impacts of infectious outbreaks that lead to better representation of mental health research in the top 10% journals, efforts need to be aggregated to fill the prevailing gaps in mental health research. Anticipating a mental health pandemic, experts have called for action for mental health research (Hoffmann, 2020). That research should prioritize key questions, produce high-quality studies, and involve international multidisciplinary collaboration (Holmes et al., 2020). The results of this study could help experts set a roadmap for future COVID-19 related mental health research and contribute to the international response to the current pandemic.
CRediT authorship contribution statement
Fadi T. Maalouf: Conceptualization, Design, Methodology, Formal analysis, Writing - review & editing. Bernadette Mdawar: Conceptualization, Design, Methodology, Formal analysis, Writing - review & editing. Lokman I. Meho: Conceptualization, Design, Methodology, Formal analysis, Writing - review & editing. Elie A. Akl: Conceptualization, Design, Methodology, Formal analysis, Writing - review & editing.
Declaration of competing interest
The authors declare no conflict of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jpsychires.2020.10.018.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Alradhawi M., Shubber N., Sheppard J., Ali Y. Effects of the COVID-19 pandemic on mental well-being amongst individuals in society- A letter to the editor on "The socio-economic implications of the coronavirus and COVID-19 pandemic: a review. Int. J. Surg. 2020;78:147–148. doi: 10.1016/j.ijsu.2020.04.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonilla-Aldana D.K., Quintero-Rada K., Montoya-Posada J.P., Ramírez-Ocampo S., Paniz-Mondolfi A., Rabaan A.A., Sah R., Rodríguez-Morales A.J. SARS-CoV, MERS-CoV and now the 2019-novel CoV: have we investigated enough about coronaviruses? - a bibliometric analysis. Trav. Med. Infect. Dis. 2020;33 doi: 10.1016/j.tmaid.2020.101566. 101566-101566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bults M., Beaujean D.J.M.A., de Zwart O., Kok G., van Empelen P., van Steenbergen J.E., Richardus J.H., Voeten H.A.C.M. Perceived risk, anxiety, and behavioural responses of the general public during the early phase of the Influenza A (H1N1) pandemic in The Netherlands: results of three consecutive online surveys. BMC Publ. Health. 2011;11(1):2. doi: 10.1186/1471-2458-11-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC . 2009. 2009 H1N1 Early Outbreak and Disease Characteristics.https://www.cdc.gov/h1n1flu/surveillanceqa.htm [Google Scholar]
- CDC . 2010. 2009 H1N1: Overview of a Pandemic Impact of 2009 H1N1.https://www.cdc.gov/h1n1flu/yearinreview/yir5.htm [Google Scholar]
- CDC . 2019. 2009 H1N1 Pandemic (H1N1 Pdm09 Virus)https://www.cdc.gov/flu/pandemic-resources/2009-h1n1-pandemic.html [Google Scholar]
- CDC . 2019. 2014-2016 Ebola Outbreak in West Africa.https://www.cdc.gov/vhf/ebola/history/2014-2016-outbreak/index.html [Google Scholar]
- CDC . 2020. Coronavirus Disease 2019 (COVID19) Stress and Coping.https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/managing-stress-anxiety.html [Google Scholar]
- Cénat J.M., Felix N., Blais-Rochette C., Rousseau C., Bukaka J., Derivois D., Noorishad P.-G., Birangui J.-P. Prevalence of mental health problems in populations affected by the Ebola virus disease: a systematic review and meta-analysis. Psychiatr. Res. 2020;289:113033. doi: 10.1016/j.psychres.2020.113033. [DOI] [PubMed] [Google Scholar]
- De Felice F., Polimeni A. Coronavirus disease (COVID-19): a machine learning bibliometric analysis. Vivo. 2020;34(3 Suppl. l):1613–1617. doi: 10.21873/invivo.11951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutheil F., Mondillon L., Navel V. PTSD as the second tsunami of the SARS-Cov2 pandemic. Psychol. Med. 2020:1–6. doi: 10.1017/S0033291720001336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg J. 2020. R0: How Scientists Quantify the Intensity of an Outbreak like Coronavirus and its Pandemic Potential.https://sph.umich.edu/pursuit/2020posts/how-scientists-quantify-outbreaks.html [Google Scholar]
- Eysenbach G. Citation advantage of open access articles. PLoS Biol. 2006;4(5):e157. doi: 10.1371/journal.pbio.0040157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haghani M., Bliemer M.C.J., Goerlandt F., Li J. The scientific literature on Coronaviruses, COVID-19 and its associated safety-related research dimensions: a scientometric analysis and scoping review. Saf. Sci. 2020;129:104806. doi: 10.1016/j.ssci.2020.104806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hao F., Tan W., Jiang L., Zhang L., Zhao X., Zou Y., Hu Y., Luo X., Jiang X., McIntyre R.S., Tran B., Sun J., Zhang Z., Ho R., Ho C., Tam W. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav. Immun. 2020;87:100–106. doi: 10.1016/j.bbi.2020.04.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helal M.N., Ahmed U., Vostanis P. The representation of low- and middle-income countries in the psychiatric research literature. Int. Psychiatr. 2011;8(4):92–94. [PMC free article] [PubMed] [Google Scholar]
- Hoffmann C. 2020. Covid-19: Be Ready for the Coming Mental Health Pandemic.https://www.physiciansweekly.com/covid-19-be-ready-for-the-coming-mental-health-pandemic-2/ [Google Scholar]
- Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Cohen Silver R., Everall I., Ford T., John A., Kabir T., King K., Madan I., Michie S., Przybylski A.K., Shafran R., Sweeney A., Worthman C.M., Yardley L., Cowan K., Cope C., Hotopf M., Bullmore E. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatr. 2020;7(6):547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kannarkat J.T., Smith N.N., McLeod-Bryant S.A. Mobilization of telepsychiatry in response to COVID-19-moving toward 21(st) century access to care. Adm. Policy Ment. Health. 2020;47(4):489–491. doi: 10.1007/s10488-020-01044-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau J.T.F., Griffiths S., Choi K.C., Tsui H.Y. Avoidance behaviors and negative psychological responses in the general population in the initial stage of the H1N1 pandemic in Hong Kong. BMC Infect. Dis. 2010;10(139):1–13. doi: 10.1186/1471-2334-10-139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu N., Chee M.L., Niu C., Pek P.P., Siddiqui F.J., Ansah J.P., Matchar D.B., Lam S.S.W., Abdullah H.R., Chan A., Malhotra R., Graves N., Koh M.S., Yoon S., Ho A.F.W., Ting D.S.W., Low J.G.H., Ong M.E.H. Coronavirus disease 2019 (COVID-19): an evidence map of medical literature. BMC Med. Res. Methodol. 2020;20(1):177. doi: 10.1186/s12874-020-01059-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maalouf F.T., Alamiri B., Atweh S., Becker A.E., Cheour M., Darwish H., Ghandour L.A., Ghuloum S., Hamze M., Karam E., Khoury B., Khoury S.J., Mokdad A., Meho L.I., Okasha T., Reed G.M., Sbaity E., Zeinoun P., Akl E.A. Mental health research in the Arab region: challenges and call for action. Lancet Psychiatr. 2019;6(11):961–966. doi: 10.1016/S2215-0366(19)30124-5. [DOI] [PubMed] [Google Scholar]
- News B. 2020. Coronavirus: the World in Lockdown in Maps and Charts. [Google Scholar]
- Neilson S., Woodward A., Mosher D. Sep 29, 2020. A Comprehensive Timeline of the Coronavirus Pandemic at 9 Months, from China's First Case to the Present.https://www.businessinsider.com/coronavirus-pandemic-timeline-history-major-events-2020-3 [Google Scholar]
- Nicola M., Alsafi Z., Sohrabi C., Kerwan A., Al-Jabir A., Iosifidis C., Agha M., Agha R. The socio-economic implications of the coronavirus and COVID-19 pandemic: a review. Int. J. Surg. 2020 doi: 10.1016/j.ijsu.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nowakowska J., Sobocińska J., Lewicki M., Lemańska Ż., Rzymski P. When science goes viral: the research response during three months of the COVID-19 outbreak. Biomed. Pharmacother. 2020;129:110451. doi: 10.1016/j.biopha.2020.110451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Leary A., Jalloh M.F., Neria Y. Fear and culture: contextualising mental health impact of the 2014-2016 Ebola epidemic in West Africa. BMJ Glob. Health. 2018;3(3) doi: 10.1136/bmjgh-2018-000924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel V., Kim Y.R. Contribution of low- and middle-income countries to research published in leading general psychiatry journals, 2002-2004. Br. J. Psychiatry. 2007;190:77–78. doi: 10.1192/bjp.bp.106.025692. [DOI] [PubMed] [Google Scholar]
- Patel V., Sumathipala A. International representation in psychiatric literature: survey of six leading journals. Br. J. Psychiatry. 2001;178:406–409. doi: 10.1192/bjp.178.5.406. [DOI] [PubMed] [Google Scholar]
- Piwowar H., Priem J., Larivière V., Alperin J.P., Matthias L., Norlander B., Farley A., West J., Haustein S. The state of OA: a large-scale analysis of the prevalence and impact of Open Access articles. PeerJ. 2018;6:e4375. doi: 10.7717/peerj.4375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reardon S. Ebola's mental-health wounds linger in Africa. Nature. 2015;519:13–14. doi: 10.1038/519013a. [DOI] [PubMed] [Google Scholar]
- Reger M.A., Stanley I.H., Joiner T.E. Suicide mortality and coronavirus disease 2019—a perfect storm? JAMA Psychiatr. 2020 doi: 10.1001/jamapsychiatry.2020.1060. [DOI] [PubMed] [Google Scholar]
- Rossi R., Socci V., Talevi D., Mensi S., Niolu C., Pacitti F., Di Marco A., Rossi A., Siracusano A., Di Lorenzo G. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. Front. Psychiatr. 2020;11 doi: 10.3389/fpsyt.2020.00790. 790-790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarukhan A. Ebola: two years and 11,300 deaths later. Glob. Health Lessons Epidemic. 2016 https://www.isglobal.org/en/ebola [Google Scholar]
- Shi L., Lu Z.-A., Que J.-Y., Huang X.-L., Liu L., Ran M.-S., Gong Y.-M., Yuan K., Yan W., Sun Y.-K., Shi J., Bao Y.-P., Lu L. Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 pandemic. JAMA Network Open. 2020;3(7) doi: 10.1001/jamanetworkopen.2020.14053. e2014053-e2014053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shore J.H., Schneck C.D., Mishkind M.C. Telepsychiatry and the coronavirus disease 2019 pandemic—current and future outcomes of the rapid virtualization of psychiatric care. JAMA Psychiatr. 2020 doi: 10.1001/jamapsychiatry.2020.1643. [DOI] [PubMed] [Google Scholar]
- Siddiqui A.H., Jilani N.T., Jamil R.T. 2020. H1N1 Influenza (Swine Flu)https://www.ncbi.nlm.nih.gov/books/NBK513241/?report=classic [Google Scholar]
- Taha S., Matheson K., Cronin T., Anisman H. Intolerance of uncertainty, appraisals, coping, and anxiety: the case of the 2009 H1N1 pandemic. Br. J. Health Psychol. 2014;19(3):592–605. doi: 10.1111/bjhp.12058. [DOI] [PubMed] [Google Scholar]
- Tao Z., Zhou S., Yao R., Wen K., Da W., Meng Y., Yang K., Liu H., Tao L. COVID-19 will stimulate a new coronavirus research breakthrough: a 20-year bibliometric analysis. Ann. Transl. Med. 2020;8(8):528. doi: 10.21037/atm.2020.04.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tognotti E. Lessons from the history of quarantine, from plague to influenza A. Emerg. Infect. Dis. 2013;19(2):254–259. doi: 10.3201/eid1902.120312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho S.C., Ho C.R. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Publ. Health. 2020;17(5) doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . 2020. Coronavirus Disease (COVID-19) Pandemic.https://www.who.int/emergencies/diseases/novel-coronavirus-2019 [Google Scholar]
- WHO . 2020. Mental Health and Psychosocial Considerations during the COVID-19 Outbreak.https://www.who.int/publications-detail/WHO-2019-nCoV-MentalHealth-2020.1 [Google Scholar]
- WHO . 2020. WHO Timeline - COVID-19.https://www.who.int/news-room/detail/08-04-2020-who-timeline---covid-19 [Google Scholar]
- WHO . 2020. Estimating Mortality from COVID-19.https://www.who.int/news-room/commentaries/detail/estimating-mortality-from-covid-19 [Google Scholar]
- Worldmeter . 2020. Coronavirus Incubation Period.https://www.worldometers.info/coronavirus/coronavirus-incubation-period/ [Google Scholar]
- Worldmeter . 2020. Countries where COVID-19 Has Spread.https://www.worldometers.info/coronavirus/countries-where-coronavirus-has-spread/ [Google Scholar]
- Worldmeter . 2020. COVID-19 Coronavirus Pandemic 2020.https://www.worldometers.info/coronavirus/?utm_campaign=homeAdvegas1? [Google Scholar]
- Worldmeter . 2020. COVID-19 Situation Update Worldwide, as of 4 September 2020.https://www.ecdc.europa.eu/en/geographical-distribution-2019-ncov-cases [Google Scholar]
- Yu Y., Shi Q., Zheng P., Gao L., Li H., Tao P., Gu B., Wang D., Chen H. Assessment of the quality of systematic reviews on COVID-19: a comparative study of previous coronavirus outbreaks. J. Med. Virol. 2020;92(7):883–890. doi: 10.1002/jmv.25901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeinoun P., Akl E.A., Maalouf F.T., Meho L.I. The arab region's contribution to global mental health research (2009–2018): a bibliometric analysis. Front. Psychiatr. 2020;11(182):1–11. doi: 10.3389/fpsyt.2020.00182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhai F., Zhai Y., Cong C., Song T., Xiang R., Feng T., Liang Z., Zeng Y., Yang J., Yang J., Liang J. Research progress of coronavirus based on bibliometric analysis. Int. J. Environ. Res. Publ. Health. 2020;17(3766):1–15. doi: 10.3390/ijerph17113766. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.