Abstract
Introduction
We aimed to describe the distribution of excess mortality (EM) during the first weeks of the COVID-19 outbreak in the Stockholm Region, Sweden, according to age, sex and sociodemographic context.
Methods
Weekly all-cause mortality data were obtained from Statistics Sweden for the period 1 January 2015 to 17 May 2020. EM during the first 20 weeks of 2020 was estimated by comparing observed mortality rates with expected mortality rates during the five previous years (N=2 379 792). EM variation by socioeconomic status (tertiles of income, education, Swedish-born, gainful employment) and age distribution (share of 70+-year-old persons) was explored based on Demographic Statistics Area (DeSO) data.
Results
EM was first detected during the week of 23–29 March 2020. During the peak week of the epidemic (6–12 April 2020), an EM of 150% was observed (152% in 80+-year-old women; 183% in 80+-year-old men). During the same week, the highest EM was observed for DeSOs with lowest income (171%), lowest education (162%), lowest share of Swedish-born (178%) and lowest share of gainfully employed residents (174%). EM was further increased in areas with higher versus lower proportion of younger people (magnitude of increase: 1.2–1.7 times depending on socioeconomic measure).
Conclusion
Living in areas characterised by lower socioeconomic status and younger populations was linked to excess mortality during the COVID-19 pandemic in the Stockholm Region. These conditions might have facilitated viral spread. Our findings highlight the well-documented vulnerability linked to increasing age and sociodemographic context for COVID-19–related death.
Keywords: epidemiology, public health, Descriptive study
Key questions.
What is already known?
While the evidence on individual-level influences of age-related and socioeconomic factors on COVID-19 mortality is rapidly growing, reports on the prognostic role of older people’s sociodemographic context are still sparse.
What are the new findings?
We found that in the Stockholm Region of Sweden, COVID-19–related excess mortality was disproportionately born by the older adults and by those living in socioeconomically deprived areas with a higher proportion of young people; these conditions might have facilitated viral spread.
Thus, individual-level influences of age-related and socioeconomic factors represent only one dimension of vulnerability faced by older adults; contextual sociodemographic characteristics are likely involved in the shaping of COVID-19 outcomes as well.
What do the new findings imply?
While different models of stratified shielding have already been suggested, these rarely account for contextual sociodemographic factors, which is likely to lead to poorly targeted public health responses that are not properly calibrated to the people or the areas involved.
Tracking people’s individual characteristics and their sociodemographic context might ease the implementation of future COVID-19–related preventive and containment strategies.
Introduction
In just 3 months since the first death attributed to COVID-19 was reported in Sweden on 11 March 2020, the pandemic has claimed more lives than breast cancer and prostate cancer combined over an entire year in 2017.1 2 Although the high mortality due to COVID-19 is hardly disputed, current estimates of deaths may be underestimated, as figures based on laboratory-confirmed results miss the false-negative cases and those who were not tested at all.3 Further, they do not include the deaths caused by conditions that would have normally been treated, had hospitals not been overwhelmed by a surge of patients needing intensive care. In areas with extensive testing, overestimation is possible too, since deaths in persons who tested positive may be unrelated to COVID-19. Excess mortality, the gap between the deaths from any cause and the historical average for the same place and time of year, offers a more comprehensive way to measure the mortality linked to the COVID-19 outbreak. Assessing excess deaths in Sweden is especially relevant, as restrictions and confinement there have been considerably less widespread compared with the rest of Europe. In brief, there have been no widespread lockdowns to mitigate the spread of COVID-19. Individuals were requested to exercise personal responsibility in order to protect themselves and others. Restaurants and schools for students under the age of 16 have remained open, and gatherings have been restricted to a maximum of 50 people.2
It is known that older adults bear a disproportionate burden of COVID-19 mortality, with 89% of all deaths due to the disease as of 22 June 2020 in Sweden occurring in individuals aged 70 or above.2 Moreover, COVID-19 appears to impact socioeconomically vulnerable populations especially hard. A preliminary analysis of excess mortality between 1 and 10 April 2020 in the Stockholm Region (the area most affected by COVID-19 in Sweden) has revealed that excess deaths were highest in municipalities with lower education, income and share of Swedish-born residents.4 Few attempts have been made to integrate biological (old age) and social (economic deprivation) vulnerabilities to better understand the forces driving COVID-19–related mortality in Sweden. A recent study has found that in older adults, individual measures of socioeconomic deprivation, such as reduced disposable income or lower educational attainment, appeared less predictive of COVID-19 mortality than in the working-age subset of the Swedish population.5
Individual-level influences of socioeconomic factors represent only one dimension of vulnerability faced by the older adults. Contextual socioeconomic characteristics have been described as another contributor to social disparities in older adults’ health6 and are likely involved in the shaping of COVID-19 outcomes as well. Furthermore, the consequences of contextual deprivation are probably non-uniform depending on the predisposing conditions that may either accentuate or lessen the effect of individual socioeconomic vulnerabilities. Contextual demography may be one such factor. Preliminary data from New York City have shown that areas with a higher share of the population under the age of 18 had more COVID-19 cases, although it was unclear whether children accelerated the transmission or whether reduced incomes underpinned this association.7 A recently proposed segmentation and shielding strategy places emphasis on those most vulnerable to COVID-19 outcomes and also on their closest contacts and networks, who can transmit the disease to them.8 Therefore, it is important to assess how contextual age distribution and socioeconomic status interact in shaping COVID-19 excess deaths.
Our aim in this study is threefold: (1) to estimate the age-specific and sex-specific excess mortality during the first weeks of the COVID-19 outbreak in the Stockholm Region; (2) to explore to what extent COVID-19 excess mortality varies among socioeconomically diverse areas; (3) to assess if the excess mortality variation linked to socioeconomic characteristics is modified by the age distribution of the population in the area.
Methods
This was a time-trend, ecological study. Weekly all-cause mortality figures and population data for the Stockholm Region (n=2 379 792 residents at the beginning of 2020) were provided by Statistics Sweden (SCB) for the period 1 January 2015 to 31 May 2020. Data from the two last weeks in 2020 (ie, 18–31 May) were discarded due to quality considerations since there is a lag in data reporting by the Swedish Tax Agency to SCB. Official COVID-19–related deaths (deaths with a positive test for COVID-19, regardless of the cause of death) were obtained from the Swedish Public Health Agency.2
Total, age-specific and sex-specific mortality rates were calculated for each week. The size of the resident population, averaged across 13 weeks (3 months), was used as the denominator for each trimester. The expected weekly mortality rates for the first 20 weeks of 2020 were obtained by averaging weekly mortality estimates for the years 2015 to 2019. Observed weekly mortality rates were compared with the expected ones in order to obtain excess mortality estimates: ((observed rate−expected rate)/expected rate)×100.
Mortality rates by socioeconomic (ie, income, level of education, share of Swedish-born, share gainfully employed) and demographic (ie, share of 70+-year-old persons) indicators for Demographic Statistics Areas (DeSO) within the Stockholm Region were also obtained from SCB. DeSOs are adjoining areas with around 1500 inhabitants (range: 700 and 2700) aimed at capturing small within-area and large between-area socioeconomic variability. DeSO subdivisions are based on the boundaries of municipalities, election districts and major urban areas over 1000 inhabitants, and are considered to be stable over time.9 The selection of socioeconomic and demographic indicators was based on pragmatic grounds, given that these are the only ones openly accessible from SCB’s website. These measures represent a comprehensive overview of contextual socioeconomics and are routinely used by statistical bureaus in their reports.
Income was measured as median employment and business (acquisition) income, and level of education as the share of above elementary (12 years) education across DeSOs. A person that is gainfully employed should have worked for at least 1 hour per week in the month of November, including those temporarily absent. If administrative records do not contain information on working hours, SCB consults the Earnings Register that contains information on the salary amount for every person’s employment relationships and the months when the taxable payments were made to infer gainful employment status over the year. Data on DeSO-level sociodemographics corresponded to years 2018–2019. Socioeconomic indicators were categorised into low, medium or high according to tertiles of the DeSO distribution, and further divided according to the share of 70+-year-old persons (below vs above the median) within each tertile.
Stata V.16 (StataCorp) was used for all the analyses. No ethical approval or consent was needed for the present study given the use of aggregate-level data. SCB is responsible for coordinating the system for the official statistics in Sweden and follows UN’s basic principles for official statistics and the Guidelines for European Statistics.
Patient and public involvement
There was no direct public involvement either in the setting of the research questions or developing the study design.
Results
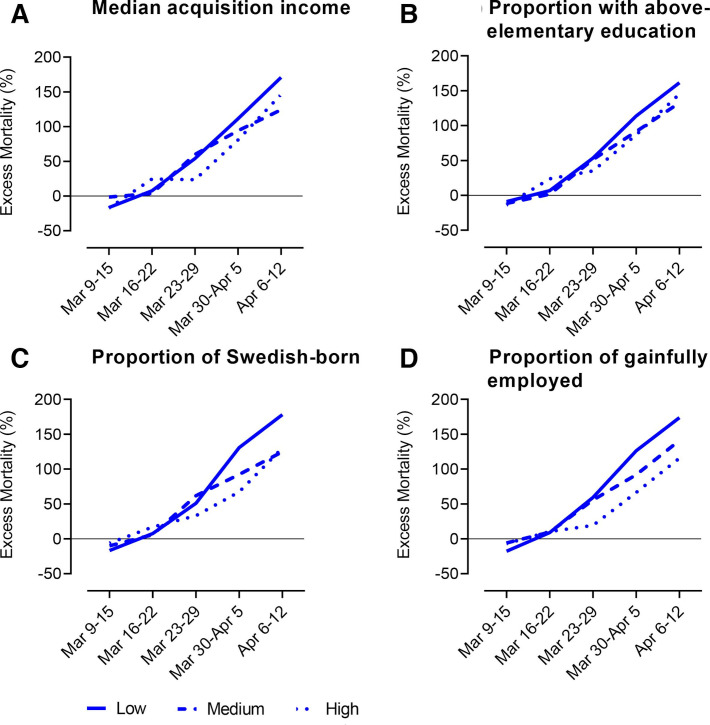
Between 11 March 2020—the date of the first death attributed to COVID-19—and 17 May 2020, 5119 deaths were reported in the Stockholm Region, compared with an average of 3009 during the same period in 2015–2019, that is, an estimated excess of 2110 deaths. Within the same period, 1942 deaths were officially attributed to COVID-19 by the Swedish Public Health Agency. Starting in the week of 9–15 March 2020, an ascending trend in excess mortality was observed, which peaked during the week of 6–12 April 2020 (figure 1).
Figure 1.
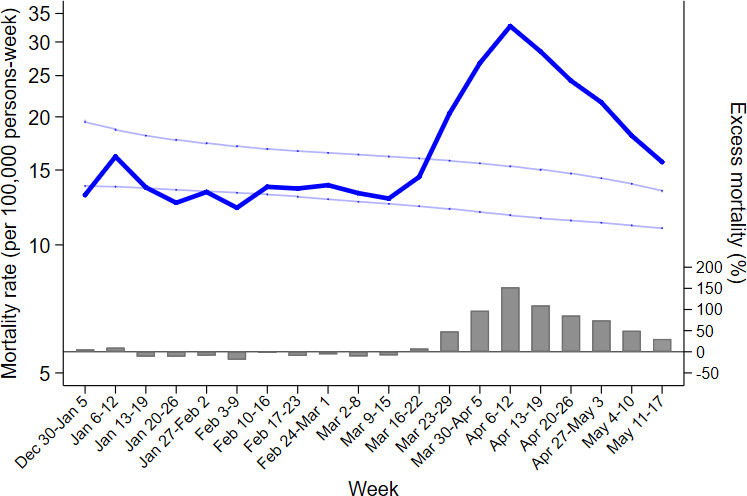
All-cause mortality rates and excess mortality in the Stockholm Region (N=2 379 792), Sweden, during the first 20 weeks of 2020. The dark blue line indicates the mortality rates per 100 000 persons-week reported on the logarithmic scale. The light blue lines indicate 95% CIs for the average mortality rates corresponding to the five previous years. Bars depict the excess mortality during the first 20 weeks of 2020 in comparison with the average from five previous years.
During the week of 6–12 April 2020, overall mortality exceeded the average rates observed in the preceding 5 years by 150% (126% for women, 176% for men). Excess mortality varied across age groups and sex. During the same week, mortality rates were in excess of the 5-year averages by 69% (49% for women and 82% for men) in individuals 0–64 years old, by 129% (68% for women and 175% for men) in individuals 65–79 years old, and by 165% (152% for women and 183% for men) in individuals 80 years old or older (table 1).
Table 1.
All-cause mortality rates (per 100 000 persons-week) and excess mortality in the Stockholm Region (N=2 379 792), Sweden, by age group and sex during the COVID-19 outbreak (ie, 9 March 2020 to 12 April 2020)
| Week | <65 years | 65–79 years | 80+ | ||||||
| Observed rate | Expected rate | Excess (%) | Observed rate | Expected rate | Excess (%) | Observed rate | Expected rate | Excess (%) |
|
| Women | |||||||||
| Mar 9–15 | 2.3 | 2.0 | 14.9 | 18.1 | 26.4 | −31.5 | 172.9 | 179.3 | −3.6 |
| Mar 16–22 | 1.5 | 1.5 | 1.5 | 25.9 | 27.4 | −5.5 | 158.6 | 181.6 | −12.7 |
| Mar 23–29 | 2.0 | 1.7 | 17.0 | 30.4 | 29.7 | 2.4 | 258.6 | 184.3 | 40.3 |
| Mar 30–Apr 5 | 1.8 | 1.7 | 0.2 | 53.6 | 25.6 | 109.9 | 326.8 | 192.8 | 69.5 |
| Apr 6–12 | 2.5 | 1.7 | 48.8 | 47.8 | 28.6 | 67.5 | 425.1 | 168.8 | 151.9 |
| Men | |||||||||
| Mar 9–15 | 2.6 | 2.7 | −3.0 | 33.4 | 35.9 | −7.0 | 164.0 | 212.6 | −22.9 |
| Mar 16–22 | 2.6 | 2.7 | −5.9 | 42.7 | 38.2 | 11.8 | 248.4 | 186.3 | 33.3 |
| Mar 23–29 | 2.8 | 3.0 | −6.5 | 61.9 | 37.7 | 64.0 | 340.0 | 185.3 | 83.5 |
| Mar 30–Apr 5 | 5.0 | 2.8 | 77.7 | 82.5 | 38.0 | 117.4 | 395.4 | 193.5 | 104.4 |
| Apr 6–12 | 5.0 | 2.8 | 81.6 | 103.8 | 37.8 | 174.7 | 518.4 | 183.4 | 182.7 |
Excess mortality calculated comparing mortality rates during weeks 11–15 of 2020 with the average mortality rates recorded for the corresponding weeks during the five previous years.
During the outbreak, the highest excess mortality was recorded among DeSOs in the lowest tertiles for income, educational level, share of Swedish-born and share of gainfully employed (excess of 171%, 162%, 178% and 174%, respectively, for the peak week of 6–12 April 2020; figure 2). The evolution of excess mortality according to DeSO-level socioeconomic characteristics from the start of the COVID-19 outbreak until the end of the observation period (17 May 2020) is shown in online supplemental figure 2.
Figure 2.
Average excess mortality across the 1287 DeSOs of the Stockholm Region (N=2 379 792), Sweden, by levels of socioeconomic indicators during the COVID-19 outbreak (ie, 9 March 2020 to 12 April 2020). Demographic Statistics Areas (DeSO) produced by Statistics Sweden gather groups of around 1500 inhabitants (range: 700 and 2700) and are built within the municipal boundaries across Sweden. Excess mortality calculated comparing mortality rates during weeks 11–15 of 2020 with the average mortality rates recorded for the corresponding weeks during the five previous years. Socioeconomic indicators were categorised into low, medium or high according to tertiles of the DeSO distribution.
bmjgh-2020-003595supp001.pdf (770.2KB, pdf)
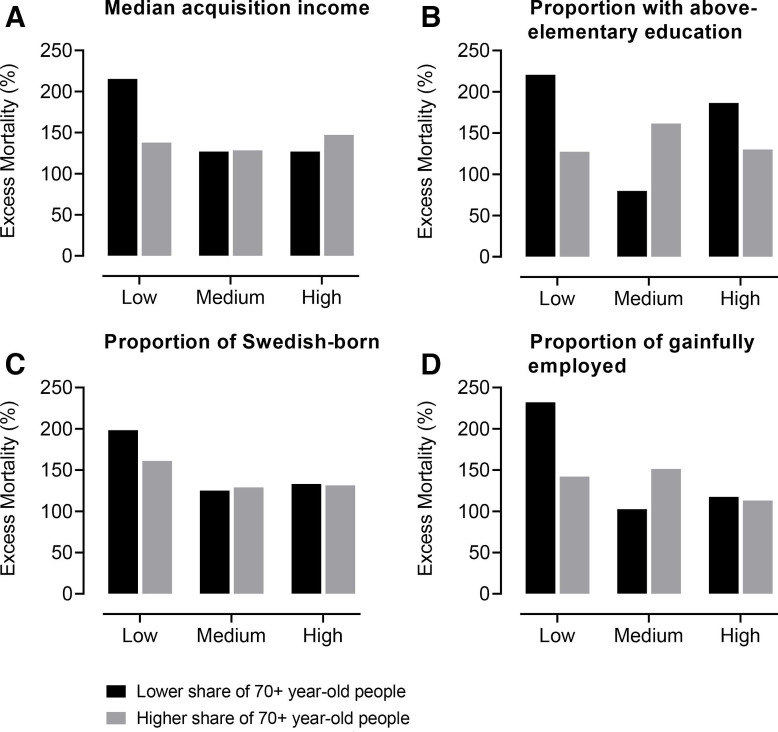
DeSO-level age composition, categorised according to the share of 70+-year-old people, appeared to modify EM differentials according to socioeconomic characteristics: the highest excess mortality rates were observed among more deprived as well as younger DeSOs. The corresponding numbers for the peak mortality week (ie, 6–12 April 2020) were 215% for younger DeSOs with the lowest income, 221% for younger DeSOs with the lowest educational level, 198% for younger DeSOs with the lowest share of Swedish-born and 232% for younger DeSOs with the lowest share of gainfully employed residents (figure 3). Even within the most deprived DeSOs, there was a 1.2-fold to 1.7-fold increase in excess mortality between those with a lower versus higher share of older people during the week of 6–12 April 2020, depending on the socioeconomic indicator considered. Excess mortality rates by socioeconomic and demographic indicators for the entire period until 17 May 2020 are presented in online supplemental table 1.
Figure 3.
Average excess mortality across the 1287 DeSOs of the Stockholm Region (N=2 379 792), Sweden, by levels of socioeconomic indicators and share of 70+-year-old people during the peak of the COVID-19 outbreak (ie, week of 6–12 April 2020). Demographic Statistics Areas (DeSO) produced by Statistics Sweden gather groups of around 1500 inhabitants (range: 700 and 2700) and are built within the municipal boundaries across Sweden. Excess mortality calculated comparing mortality rates during the week of 6–12 April 2020 with the average mortality rates recorded for the corresponding weeks during the five previous years. Socioeconomic indicators were categorised into low, medium or high according to tertiles of the DeSO distribution, and further divided according to the share of 70+-year-old persons (below vs above the median) within each tertile.
Discussion
In the present work, we found that, in the Stockholm Region, the negative impact of the COVID-19 outbreak was disproportionately born by the older adults and by those living in socioeconomically deprived areas with a higher proportion of young people, which underlines the prognostic role of the interplay between old age and a context of social vulnerability.
Deaths with a positive test for COVID-19, regardless of the cause of death, constituted 92% of our estimated number of excess deaths for the period between 9 March 2020 and 17 May 2020. There have been occasional accounts of under-reporting of COVID-19–related deaths that do not occur in hospitals. Our finding seems to support this scenario, rather than a supposed over-reporting of COVID-19–related death.3 We cannot, however, exclude that some of the EM was due to a general strain on the healthcare system.
Our observation that the risk of severe COVID-19 is not uniformly distributed across population groups corresponds to other empirical evidence. Age is the main risk factor for COVID-19–related death, with over two-thirds of deaths in Sweden to date being in people aged 80+ years,2 an age group with EM of 165% according to our findings. The progressive accumulation of multiple chronic conditions begins during adult life and accelerates after the sixth to seventh decade, when more than one in two individuals are affected by two or more chronic diseases (ie, multimorbidity).10 Multimorbidity increases individuals’ risk of developing physical and cognitive impairments and facilitates the onset of infectious diseases, such as pneumonia, due to viral and bacterial agents.11–14 Such lack of resilience to stressful events can lead to biological frailty, a condition that characterises a considerable share of older adults and which has been recently identified as an independent risk factor for intensive care need and in-hospital death among older adults affected by COVID-19.15 16
Protracted social inequalities in non-communicable diseases and socially patterned health determinants are being magnified by the COVID-19 pandemic, which places a disproportionate burden on those who are socioeconomically vulnerable, as shown by our findings.17 These individuals have higher rates of almost all known underlying clinical risk factors that increase the severity and mortality of COVID-19.18 Social determinants of health, governing where people work, live and age, are the likely drivers of the social inequalities in COVID-19’s outcomes. In addition to influencing COVID-19’s chronic comorbidities, life-long socioeconomic adversity may lead to a suppressed immune response due to psychosocial stress increasing the likelihood of infection.19 Reduced incomes may lead to home overcrowding, which increases the risk of contagion too. Environments characterised by increased deprivation may have lower access to healthcare, even in universal healthcare systems, whereas reduced educational level and lower health literacy may impede access to and understanding of public health advice.17 Overall, rather than being socially neutral as claimed in the early days of the pandemic, COVID-19 exacerbates existing social inequalities in health and disease.
Whether Sweden’s less-restrictive approach to containing COVID-19 by promoting ‘social distancing’ instead of compulsory quarantine has been more or less successful is yet to be examined in international comparative studies, but what seems to be evident from our study is that such strategy may have been less effective in deprived areas with a high proportion of younger people. Consistent with the approach taken in other countries as an exit strategy from COVID-19 lockdown, Swedish policy has been directed to reduce intergenerational contact primarily among older people from the beginning.2 However, according to the idea of segmented shielding, almost as important as taking strict precautions to avoid infection among the most vulnerable (ie, the older population) is extending such safety measures to older adults’ regular contacts who tend to be younger: those who live with them, the relatives who visit them and/or the social workers who care for them (ie, the shielders).8 Factors like occupational environments (eg, service sector and other jobs requiring physical contact with others), active social lives, shortage and lack of adapted preventive information, as well as overcrowded and intergenerational cohabitation may have increased the likelihood of the virus exposure among the younger ‘shielders’, with a direct impact on the vulnerable older populations, as shown by excess mortality rates surpassing 200% in socioeconomically deprived areas with a high share of younger residents. Offering quarantine facilities to help people in crowded households to isolate themselves has been one important measure launched by some municipalities in the Stockholm Region,2 but perhaps not enough. The dissemination of translated guidelines about reducing the spread of COVID-19, for example, has incurred an unnecessary delay.20 Setting the limit for public gatherings to 50 people2 might also have been insufficiently restrictive, given the propensity among younger people to meet in smaller groups.
Public health implications
Our findings have important implications for future shielding strategies, under the likely scenario of future resurgences of the COVID-19 infection21 or other pandemics. Furthermore, the need to target interventions (eg, confinement, social distancing, active surveillance) and direct healthcare resources towards the subgroups at increased risk of developing the most severe forms of the disease is widely acknowledged.22 While different models of stratified shielding have already been suggested,23 24 these rarely account for contextual sociodemographic factors, which is likely to lead to poorly targeted public health responses that are not properly calibrated to the people or the areas involved. In this regard, tracking people’s individual characteristics and sociodemographic context might ease the implementation of effective preventive and containment strategies. The lack of exhaustive individual and contextual data coverage has in fact been pointed out as one of the weaknesses of the current response to the COVID-19 pandemic.25 Collecting these data will be one of the most important strategies to successfully cope with future similar scenarios.
Study limitations
We could neither observe mortality for individuals within DeSOs nor could we examine specific DeSOs on their own due to SCB’s rules against backwards identification of individuals. Instead, we aggregated DeSOs into groups defined by contextual socioeconomics and age distributions and examined weekly mortality differences across these SES–age–DeSO slices. This prevented us from obtaining variance estimates within DeSO groups. Given the lack of availability of individual-level data, we cannot ascertain the age of the subjects contributing to the exceptionally high rates of excess mortality seen in the deprived young neighbourhoods of the Stockholm Region. Still, we have reasons to believe that they are most likely 65 years or older, as is the case for the rest of the population. If all people dying in these areas were below 65, the mortality rate for this age group during the peak week of 6–12 April 2020 would not make up for the actual number of deaths observed during that week (expected: 16 deaths; observed: 132–150 deaths depending on the socioeconomic indicator considered). Considering that the 2019–2020 winter in Stockholm was one of the mildest on record, the observed mortality in the period before the COVID-19 outbreak was reduced in comparison with previous years.26 Thus, it is likely that the calculated excess mortality is underestimated. On the other hand, it should be noted that the lower-than-average mortality preceding the outbreak may have increased the ‘pool’ of frail persons and thus inflated excess mortality during the outbreak.
Conclusion
Future COVID-19–related strategies of social distancing, confinement, active surveillance, and eventually vaccination, will necessarily have to consider individuals’ risk of morbidity and mortality if they were to contract the virus. This necessitates to also account for their sociodemographic context. In the Stockholm Region, vulnerable individuals living in deprived areas with a high proportion of young people will require carefully tailored prevention strategies.
Acknowledgments
We thank Tomas Johansson, Ann-Sofie Davidsson and Christina Grandelius from Statistics Sweden for the assistance in the extraction of mortality and census data.
Footnotes
Handling editor: Seye Abimbola
Twitter: @AmaiaCalderon
Contributors: AC-L, DLV, TB and SD developed the study concept and design. AC-L, DLV and DR performed the data analysis. AC-L, DLV and SD drafted the manuscript. AC-L, DLV, DR, TB, LF and SD interpreted the data. All authors provided critical revisions and approved the final version of the manuscript for submission.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available on request. Data for this study were provided by Statistics Sweden (SCB, https://www.scb.se/en/).
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
References
- 1.Swedish National Board of Health and Welfare Statistics on cancer incidence 2017, 2018. Available: https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/statistik/2018-12-51.pdf [Accessed 30 Jun 2020].
- 2.Public Health Agency of Sweden COVID-19 statistics in Sweden. Available: https://www.folkhalsomyndigheten.se/smittskydd-beredskap/utbrott/aktuella-utbrott/covid-19/statistik-och-analyser/bekraftade-fall-i-sverige/ [Accessed 30 Jun 2020].
- 3.Centers for Disease Control and Prevention – National Center for Health Statistics Excess deaths associated with COVID-19, 2020. Available: https://www.cdc.gov/nchs/nvss/vsrr/covid19/excess_deaths.htm [Accessed 30 Jun 2020].
- 4.Calderón-Larrañaga A, Dekhtyar S, Vetrano DL, et al. COVID-19: risk accumulation among biologically and socially vulnerable older populations. Ageing Res Rev 2020;63:101149. 10.1016/j.arr.2020.101149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Drefahl S, Wallace M, Mussino E, et al. Socio-demographic risk factors of COVID-19 deaths in Sweden: a nationwide register study. Stock Res Reports Demogr 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang C-Q, Chung P-K, Zhang R, et al. Socioeconomic inequalities in older adults' health: the roles of neighborhood and individual-level psychosocial and behavioral resources. Front Public Health 2019;7:318. 10.3389/fpubh.2019.00318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.NYU Furman Center COVID-19 cases in New York City, a neighborhood-level analysis, 2020. Available: https://furmancenter.org/thestoop/entry/covid-19-cases-in-new-york-city-a-neighborhood-level-analysis [Accessed 30 Jun 2020].
- 8.van BBA, Morgan AL, Bessell PR, et al. Segmentation and shielding of the most vulnerable members of the population as elements of an exit strategy from COVID-19 lockdown. medRxiv 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Statistics Sweden (SCB) DeSO – Demografiska statistikområden, 2020. Available: https://www.scb.se/hitta-statistik/regional-statistik-och-kartor/regionala-indelningar/deso---demografiska-statistikomraden/ [Accessed 30 Jun 2020].
- 10.Calderón-Larrañaga A, Vetrano DL, Onder G, et al. Assessing and measuring chronic multimorbidity in the older population: a proposal for its operationalization. J Gerontol A Biol Sci Med Sci 2017;72:1417–23. 10.1093/gerona/glw233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Calderón-Larrañaga A, Vetrano DL, Ferrucci L, et al. Multimorbidity and functional impairment-bidirectional interplay, synergistic effects and common pathways. J Intern Med 2019;285:255–71. 10.1111/joim.12843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vetrano DL, Rizzuto D, Calderón-Larrañaga A, et al. Trajectories of functional decline in older adults with neuropsychiatric and cardiovascular multimorbidity: a Swedish cohort study. PLoS Med 2018;15:e1002503. 10.1371/journal.pmed.1002503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Falcone M, Russo A, Gentiloni Silverj F, et al. Predictors of mortality in nursing-home residents with pneumonia: a multicentre study. Clin Microbiol Infect 2018;24:72–7. 10.1016/j.cmi.2017.05.023 [DOI] [PubMed] [Google Scholar]
- 14.Kundi H, Wadhera RK, Strom JB, et al. Association of frailty with 30-day outcomes for acute myocardial infarction, heart failure, and pneumonia among elderly adults. JAMA Cardiol 2019;4:1084. 10.1001/jamacardio.2019.3511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bellelli G, Rebora P, Valsecchi MG, et al. Frailty index predicts poor outcome in COVID-19 patients. Intensive Care Med 2020;46:1634–6. 10.1007/s00134-020-06087-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hewitt J, Carter B, Vilches-Moraga A, et al. The effect of frailty on survival in patients with COVID-19 (COPE): a multicentre, European, observational cohort study. Lancet Public Health 2020;5:e444–51. 10.1016/S2468-2667(20)30146-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bambra C, Riordan R, Ford J, et al. The COVID-19 pandemic and health inequalities. J Epidemiol Community Health 2020;121 10.1136/jech-2020-214401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baum F. Health divides. Where you live can kill you. Int J Epidemiol 2017;46:1345–6. 10.1093/ije/dyx111 [DOI] [Google Scholar]
- 19.Khalatbari-Soltani S, Cumming RC, Delpierre C, et al. Importance of collecting data on socioeconomic determinants from the early stage of the COVID-19 outbreak onwards. J Epidemiol Community Health 2020;74:jech-2020-214297. 10.1136/jech-2020-214297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.The Local Why are there so many coronavirus cases in Stockholm’s northern suburbs? 2020. Available: https://www.thelocal.se/20200409/why-are-there-so-many-coronavirus-cases-in-stockholms-northern-suburbs [Accessed 30 Jun 2020].
- 21.Kissler SM, Tedijanto C, Goldstein E, et al. Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science 2020;368:860–8. 10.1126/science.abb5793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Douglas M, Katikireddi SV, Taulbut M, et al. Mitigating the wider health effects of COVID-19 pandemic response. BMJ 2020;369:m1557. 10.1136/bmj.m1557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Williams R, Markus A, Yang C, et al. Seek COVER: development and validation of a personalized risk calculator for COVID-19 outcomes in an international network. medRxiv 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McKeigue P, Colhoun H. Evaluation of “stratify and shield” as a policy option for ending the COVID-19 lockdown in the UK. medRxiv. [Google Scholar]
- 25.Hanratty B, Burton JK, Goodman C, et al. COVID-19 and lack of linked datasets for care homes. BMJ 2020;369:m2463. 10.1136/bmj.m2463 [DOI] [PubMed] [Google Scholar]
- 26.Rocklöv J, Forsberg B, Ebi K, et al. Susceptibility to mortality related to temperature and heat and cold wave duration in the population of Stockholm County, Sweden. Glob Health Action 2014;7:22737. 10.3402/gha.v7.22737 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2020-003595supp001.pdf (770.2KB, pdf)