Abstract
Objective:
To assess potential transmission of antibiotic resistant organisms (AROs) using surrogate markers and bacterial cultures.
Design:
pilot study.
Setting:
1,260-bed tertiary-care academic medical center.
Participants:
25 patients (17 on contact precautions for AROs) and 77 healthcare professionals (HCPs).
Methods:
Fluorescent powder (FP) and MS2 bacteriophage were applied in patient rooms. HCP visits to each room were observed for 2–4 hours; hand hygiene (HH) compliance was recorded. Surfaces in and outside the room and HCP skin/clothing were assessed for fluorescence and swabs were collected for MS2 detection by PCR and selective bacterial cultures.
Results:
Transfer of FP was observed for 20 (80%) rooms and 26 (34%) HCPs. Transfer of MS2 was detected for 10 (40%) rooms and 15 (19%) HCPs. Bacterial cultures were positive for one room and 8 (10%) HCPs. Interactions with patients on contact precautions resulted in fewer FP detections than interactions with patients not on precautions (p<.001); MS2 detections did not differ by patient isolation status. FP detections did not differ by type of HCP, but MS2 was recovered more frequently from physicians vs. nurses (p=0.03). HH compliance was better among HCPs caring for patients on contact precautions vs. HCPs caring for patients not on precautions (p=0.003), among nurses vs. other non-physician HCPs at room entry (p=0.002), and among nurses vs. physicians at room exit (p=0.03). HCPs who performed HH prior to assessment had fewer fluorescence detections (p=0.008).
Conclusions:
Contact precautions were associated with greater HCP HH compliance and reduced detection of FP and MS2.
Introduction
Antibiotic resistant organisms (AROs) present a major infection control threat for patients in hospitals and increase the risk of serious healthcare associated infections. Hospital environmental surfaces can become contaminated with AROs and may contribute to ARO transmission, either directly or via the hands or clothing of healthcare professionals (HCPs).1–5 Contact precautions (gowns and gloves) have been an essential component of infection prevention practices to limit transmission of AROs.6 However, there has been debate about whether contact precautions are effective in reducing ARO transmission.7–9
It is difficult to study the relationship between environmental contamination, HCP cross-contamination, and ARO transmission. Previous studies have demonstrated that contaminated hospital surfaces can contribute to the spread of nosocomial infections.10–12 Other studies have demonstrated ARO transfer from infected patients or contaminated surfaces to the hands and clothing of HCPs.13–17 However, few studies have focused on the relationship between contaminated surfaces in patient rooms and the risk of HCP cross-contamination outside patient rooms.18
Additional studies that examine the associations between environmental surface contamination, HCP cross-contamination, and ARO transmission patterns, and the impact of contact isolation practices on these associations, are needed to better inform policies and procedures for the use of personal protective equipment (PPE) and to reduce ARO transmission and healthcare-associated infections (HAIs). Surrogate markers, such as fluorescent powder (FP) and MS2, a non-pathogenic bacteriophage, are unique tools to study ARO transmission and cross-contamination in hospitals.19,20 FP and MS2 have been used to study HCP self-contamination while donning/doffing PPE,17,21,22 and the effectiveness of hospital cleaning procedures.23–25
The aim of this prospective cohort study was to assess ARO transmission and cross-contamination patterns in real world hospital settings using two surrogate markers (FP and MS2 bacteriophage) and selective bacterial cultures.
Methods
This study was conducted in a general medicine ward, medical intensive care unit (ICU), and emergency department (ED) at a 1,260-bed tertiary care academic hospital in St. Louis, Missouri. Patients age ≥18 years hospitalized between 9/16/2015 and 2/9/2016 and HCPs caring for enrolled patients were eligible for inclusion. The study protocol was reviewed and approved by the Washington University Human Research Protection Office. Written informed consent was obtained from all patients or a legally authorized representative. Participating HCPs provided verbal consent prior to study participation.
Patient Enrollment
Two patients on contact precautions for vancomycin-resistant Enterococcus (VRE) or methicillin-resistant Staphylococcus aureus (MRSA) were enrolled for each patient not on contact precautions. At enrollment, each patient’s room was scanned for fluorescence using a UV light. If fluorescence was detected, the area was wiped clean before surrogate marker application. For patients on contact precautions, flocked swab collection kits (ESwab, Copan Diagnostics, Murietta, CA) were used to collect swabs from each of the surfaces targeted for surrogate marker application and to collect a nasal, axilla, inguinal, and stool or rectal swab from each patient. Baseline patient and environmental samples were interrogated using selective bacterial culture.
Surrogate Marker Application
Four high-touch surfaces in the patient room were selected for surrogate marker application: the front of the patient’s gown, the top of each bedrail, and the bedside table or computer mouse. Fluorescent powder (FP; 0.02g, Glo Germ, Moab, UT) was applied to each surface using a brush applicator. MS2 bacteriophage (MS2; 1:10 dilution of commercially-available stock solution in viral transport medium, 1.0x108 PFU/mL per site,17 ZeptoMetrix, Buffalo, NY) was applied using an atomizer (Teleflex, Morrisville, NC).
HCP Enrollment and Observations
Following surrogate marker application, trained study coordinators observed each patient room for 2–4 hours from the hallway. During this period, HCP hand hygiene (HH) compliance at room entry and exit, defined as the use of alcohol hand rub or soap and water, were recorded, and the first three surfaces that each HCP touched after exiting the room were flagged for later assessment. Three to four HCPs who entered the room during the observation period were recruited for study participation.
Sample Collection
After the first visit to the patient’s room, participating HCPs had their hands, face/hair, and clothing scanned with a UV light to identify areas of fluorescence. For patients on contact precautions, UV scanning was done after the HCP removed PPE. HCPs were assessed only once, even if they visited the room multiple times. At the end of the observation period, the patient’s room, the first three surfaces that each participating HCP had touched after exiting the room, and four additional locations on the study ward (medication cabinet, door handles, nurse’s station, and elevator buttons) were scanned for fluorescence.
Areas that fluoresced were photographed and trained study coordinators collected surface samples using a viral transport collection kit (Quidel, San Diego, CA). Additional samples were collected from the four locations on the study ward and from each participating HCP’s hands/gloves, face (periorbital/nasal/oral areas), and sleeve/wrist. These samples were tested for the presence of MS2.
If the patient was on contact precautions, flocked swab collection kits were used to collect additional samples from each area where fluorescence was observed and from the four locations on the study ward. One pooled sample was also collected from each participating HCP’s face, hands, and wrists. These swabs were submitted for selective bacterial culture.
After sample collection, the surfaces where the surrogate markers had been applied and any areas where fluorescence was observed were wiped clean to prevent further transmission of FP and MS2. Each patient room was used only once to further minimize the possibility of residual marker from a previous patient.
Bacterial Culture
Swabs collected to identify MS2 contamination had RNA extracted from the transport medium using the QIAamp viral RNA Mini Kit (Qiagen, Germantown, MD). Real-time reverse transcriptase PCR was used to detect MS2 bacteriophage using the Cepheid Smart Cycler (Cepheid, Sunnyvale, CA).
Swabs associated with patients on contact precautions were cultured for VRE, MRSA, and methicillin susceptible Staphylococcus aureus (MSSA). Swabs were plated to CHROMID VRE chromogenic medium (bioMérieux, Marcy-l’Étiole, France) to select for VRE, Spectra MRSA chromogenic agar (Remel, Lenexa, KS) to select for MRSA, and 5% sheep’s blood agar (Hardy Diagnostics, Santa Maria, CA) to recover MSSA. All swabs were also inoculated to 6.5% NaCl broth (Hardy Diagnostics) as an enrichment method to recover VRE, MRSA, and MSSA, if these did not grow on the primary plated media. When growth was observed, four colonies of each type of organism were subcultured and identified using matrix-assisted laser desorption ionization time-of-flight mass spectrometry (MALDI-TOF MS) using the VITEK MS.26–28 After bacterial identification was confirmed, phenotypic antimicrobial susceptibly testing and repetitive sequence-based PCR (repPCR) was performed. Staphylococcal cassette chromosome mec (SCCmec) typing was performed on all S. aureus isolates.29,30
Statistical Analysis
Patterns in the location and type of surrogate marker detections were evaluated qualitatively. Odds ratios with 95% confidence intervals and chi-square/Fisher exact tests were used to characterize associations between predictor and outcome variables. Predictor variables included patient contact isolation status and type of HCP. Outcome variables included FP, MS2, and VRE, MRSA, or MSSA detections in patient rooms, on HCPs, and/or on surfaces touched by HCPs. HCP use of HH at room entry and exit were assessed as both predictor and outcome variables. Two measures of HCP HH compliance were examined: HH at the first room visit by participating HCPs, and HH over all room visits by all HCPs. The first measure was used to determine the association between HH and surrogate marker detections, while the second provided a more complete picture of overall HH practices. All analyses were performed using IBM SPSS Statistics, Version 24.0. (IBM Corp., Armonk, NY).
Results
Twenty-five patients were enrolled: ten in the medicine ward, ten in the ICU, and five in the ED. Seventeen patients (68%) were on contact precautions for VRE (12), MRSA (4), or VRE and MRSA (1). Seventy-seven HCPs participated in the study; half (40, 52%) were nurses (35), nurse practitioners (3), or student nurses (2). Other participating HCPs included physicians (16, 21%), patient care technicians (9, 12%), respiratory therapists (4, 5%), radiology technicians (2, 3%), dieticians (2, 3%), one pharmacist (1%), a pharmacy student, an infection preventionist, and a unit secretary.
Fluorescent Powder Detections
In 20 patient rooms (80%), fluorescence was detected on at least one site outside the areas where FP had been applied, most commonly on the computer keyboard (n=15), counter (n=7), or door handle (n=5). In three cases, fluorescence was also detected in the study ward, at the nurses’ station (n=2) or on the medication cabinet (n=1). Twenty-six HCPs (34%) had fluorescence detected on their body/hands/clothing (n=23) and/or on a surface they touched after exiting the patient’s room (n=10). Examples of FP detections are shown in Figure 1.
Figure 1.
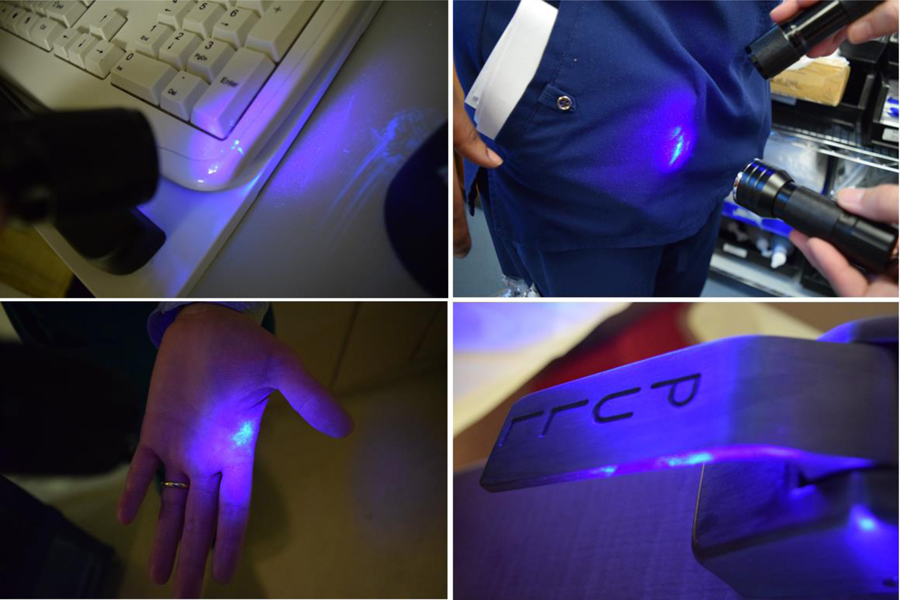
Examples of fluorescent powder detections observed in this study
HCPs caring for patients on contact precautions had significantly fewer FP detections, on themselves and/or on the surfaces they touched, than HCPs caring for patients not on precautions (19% vs. 70%, p<0.001; Table 1). There was no significant difference in rates of FP detection among different types of HCPs (Table 2).
Table 1.
Fluorescent powder and MS2 detections on participating healthcare professionals (HCPs) and surfaces touched by participating HCPs after exiting the patient’s room, by patient isolation status.
| Type of detection | All HCPs N=77 (%) |
HCPs caring for Patient on Contact Precautions N=54 (%) |
HCPs caring for Patient not on Precautions N=23 (%) |
OR (95% CI) | pa |
|---|---|---|---|---|---|
| Fluorescent Powderb | 26 (34) | 10 (19) | 16 (70) | 0.10 (0.03 – 0.31) | <0.001 |
| HCPc | 23 (30) | 9 (17) | 14 (61) | 0.13 (0.04 – 0.39) | <0.001 |
| Touched surfaced | 10 (13) | 3 (6) | 7 (30) | 0.13 (0.03 – 0.58) | 0.006 |
| MS2e | 15 (19) | 8 (15) | 7 (30) | 0.40 (0.12 – 1.27) | 0.13 |
| HCPc | 10 (13) | 4 (7) | 6 (26) | 0.23 (0.06 – 0.90) | 0.06 |
| Touched surfaced | 6 (8) | 4 (7) | 2 (9) | 0.84 (0.14 – 4.94) | 1.00 |
Abbreviations: HCP, healthcare professionals
Fisher’s exact test was used for comparisons due to small cell sizes.
Defined as the visualization of fluorescence when the HCP/surface was scanned with a handheld UV light.
Includes HCP hands, sleeves/wrist, gloves, face, and clothing.
Environmental surfaces touched by HCPs after leaving the patient room.
Defined as the detection of MS2 on a swab collected from the HCP/surface via real-time reverse transcriptase PCR.
Table 2.
Fluorescent powder and MS2 detections on participating healthcare professionals (HCP) and/or surfaces touched by participating HCP by type.
| Type of detection | Surrogate marker detected | Surrogate marker not detected | OR (95% CI) | p |
|---|---|---|---|---|
| Fluorescent Powder | N=26 (%) | N=51 (%) | ||
| Nursea (n=40) | 13 (50) | 26 (51) | Reference | |
| Physician (n=16) | 3 (12) | 13 (26) | 0.48 (0.12 – 1.98) | 0.31 |
| Otherb (n=21) | 10 (39) | 12 (24) | 1.89 (0.64 – 5.57) | 0.25 |
| MS2 | N=15 (%) | N=62 (%) | ||
| Nursea (n=40) | 4 (27) | 35 (57) | Reference | |
| Physician (n=16) | 6 (40) | 10 (16) | 5.40 (1.27 – 22.93) | 0.02 |
| Otherb (n=21) | 5 (33) | 17 (27) | 2.57 (0.67 – 11.88) | 0.16 |
Abbreviations: HCP, healthcare professional
Includes nurse practitioners and student nurses.
Includes patient care technicians, respiratory therapists, radiology techs, dieticians, pharmacist, pharmacy student, infection prevention technician, and unit secretary.
MS2 Detections
MS2 was detected inside nine patient rooms (36%), most commonly on the computer (n=4), and outside one room, on a medication cabinet. Fifteen HCPs (19%) had MS2 detections, either on their body or clothing (n=10), and/or on surfaces touched after exiting a patient room (n=6), most commonly the door handle (n=3). One HCP had MS2 identified on two sites on the body/clothing and one HCP had MS2 identified on two touched surfaces.
In general, MS2 was recovered less frequently on HCPs and/or surfaces touched by HCPs caring for patients on contact precautions versus HCPs caring for patients not on precautions, but these differences did not achieve statistical significance (Table 1). MS2 was more often detected on physicians than nurses (40% vs. 27%, p=0.02; Table 2).
Bacterial Culture Results
Twelve of the patients on contact precautions (71%) had baseline swabs that were positive for the ARO for which the patient was placed on contact precautions. Two patients, one on precautions for MRSA and one for VRE, had swabs positive for both MRSA and VRE. One patient on precautions for VRE had baseline swabs positive for MSSA.
Seven patients on contact precautions (41%) had one or more room surfaces with a positive baseline bacterial culture (Table 3). For six, the organism identified was the organism that triggered contact precautions; two patients had surfaces that were also positive for MSSA. The remaining patient, who was on precautions for VRE but had a baseline swab positive for MSSA, had baseline room surface swabs that were also positive for MSSA.
Table 3.
Microbiologic culture results for the patients on contact precautions and the healthcare professionals (HCP) who cared for these patients
| Samples | All Positive |
VRE | MRSA | MSSA |
|---|---|---|---|---|
| Samples from patients (n=17) | ||||
| Baseline patient swabsa | 13b | 9c | 5d | 1e |
| Baseline room surface swabs | 7f | 3g | 3h | 3i |
| Surface swabs from areas where fluorescence was observed inside patient rooms | 1 | 1j | 0 | 0 |
| Surface swabs from areas where fluorescence was observed outside patient rooms | 1 | 0 | 0 | 1k |
| Samples from HCPs (n=54) | ||||
| Pooled swab from face, hands, and wrist | 8 | 0 | 0 | 8l |
| Swabs collected from surfaces touched by participating HCP after leaving patient rooms | 2 | 1m | 0 | 1n |
Abbreviations: VRE, vancomycin-resistant Enterococcus; MRSA, methicillin-resistant Staphylococcus aureus; MSSA, methicillin-susceptible Staphylococcus aureus; NA, not applicable; HCP, healthcare professional.
Note: MSSA is not an indication for contact precautions.
Included nasal, axilla, inguinal skin, and stool or rectal swabs.
For 12 patients, the identified organism matched the reason for contact precautions; two patients had swabs that were positive for both VRE and MRSA. One patient had swabs that were positive for only MSSA.
Repetitive sequence-based PCR (repPCR) results were variable: samples from one patient were type B, samples from 4 patients were type C, samples from 2 patients were types B and C, samples from 1 patient were types A, B and C, and samples from 1 patient were types A, D, E, and F.
Samples from 4 patients were repetitive sequence-based PCR (repPCR) type B and staphylococcal cassette chromosome mec (SCCmec) type IV. Samples from one patient were repPCR types E and G, SCCmec type III.
Samples were repPCR types C and B, SCCmec type III.
For 6 patients, the identified organism matched the reason for contact precautions; one patient had baseline room surface swabs that were positive for both MRSA and MSSA and one patient had swabs that were positive for both VRE and MSSA. One patient had baseline room surface swabs that were positive for only MSSA.
Baseline room surface samples from two patient rooms were all repPCR type C, samples from the third room were repPCR types D and F.
Samples from 2 rooms were repPCR type B, SCCmec type IV. Samples from one room were repPCR types E and G, SCCmec type III.
Samples from the first room were repPCR type B, SCCmec type III. Samples from the second room were repPCR type E, SCCmec type I. Samples from the third room repPCR types B and D, SCCmec type III.
Samples were repPCR types D and E.
These samples were repPCR type A, SCCmec type I.
One HCP had samples that were repPCR type A, SCCmec type III; one had samples that were repPCR type B, SCCmec type III; one had samples that were repPCR type E, SCCmec type I; 3 had samples that were repPCR type F, SCCmec type III; one had samples that were repPCR types A, C, and D, SCCmec type III; and one had samples that were repPCR types E and D, SCCmec type III.
Samples were repPCR type C.
Two surfaces touched by the same HCP had samples that were positive for MSSA types H and A, SCCmec type III.
Among the swabs collected from surfaces where fluorescence was observed, only two had a positive bacterial culture (Table 3). One, from the foot of a bed, was positive for VRE. The other, from an elevator button, was positive for MSSA. Both were associated with the same patient, who had a baseline swab positive for VRE.
Of the 54 HCPs who cared for a patient on contact precautions, 8 (15%) had a positive pooled swab; all of which were positive for MSSA (Table 3). These HCP had cared for four different patients, none of whom had a baseline swab positive for MSSA, but one of whom had a baseline room surface positive for MSSA.
Only two (4%) HCPs who cared for a patient on contact precautions had a touched surface with a positive bacterial culture (Table 3). The first, a blood glucose monitor, was positive for VRE, although the HCP was positive for MSSA and MRSA was identified in the patient’s room. The second, a door handle, was positive for MSSA and was touched by a HCP who was also positive for MSSA, although VRE was identified in the patient’s room.
Among samples that were positive for VRE, 6 strain types were identified by repPCR. The most common, type C, was associated with 8 patients, three of whom were also positive for type B. Two patients had VRE type C identified in both patient and room surface samples. Another patient had multiple VRE types (A, D, E, F) identified in patient and room surface samples.
Among samples that were positive for S. aureus, 9 strain types were identified by repPCR (3 among MRSA samples and 8 among MSSA samples). Four strain types were identified by SCCmec typing. Four of the five patients who were positive for MRSA and two of the three patients with room surfaces positive for MRSA had the same strain typing (repPCR B, SCCmec IV). Among eight HCPs who were positive for MSSA, seven had the same SCCmec type (III). Three of these samples were repPCR type F, the others had diverse repPCR typing.
HCP Hand Hygiene Observations
Both measures of HCP HH compliance yielded similar estimates. HH compliance was lower at room entry than at room exit. Only 18% of HCPs performed HH at room entry (14/77 first visits by participating HCPs and 54/298 total HCP visits), while 52% performed HH at room exit (40/77 first visits and 54/290 total visits).
HCP HH compliance at room entry did not differ by patient isolation status (Table 4). However, compliance at room exit was better among HCPs caring for patients on contact precautions versus HCPs caring for patients not on precautions (61% vs. 30% first room visits, p=0.02 and 58% vs. 37% all room visits; p<0.01). No differences in HH compliance at first room visit were observed for nurses versus physicians or other HCPs (Table 5). However, when considering all room visits, nurses were more likely than other non-physician HCPs to perform HH at room entry (25% vs. 8%, p<0.01) and more likely than physicians to perform HH at room exit (59% vs. 43%; p=0.03).
Table 4.
Healthcare professional observations where hand hygiene was performed, at first room entry/exit and all room entries/exits, by patient isolation status.
| Observation | Patients on contact precautions | Patients not on contact precautions | OR (95% CI) | pa |
|---|---|---|---|---|
| First room visit by participating HCP | N=54 (%) | N=23 (%) | ||
| Room entry | 8 (15) | 6 (26) | 2.03 (0.61 – 6.71) | 0.33 |
| Room exit | 33 (61) | 7 (30) | 0.28 (0.10 – 0.79) | 0.02 |
| All HCP room visits | N=221 (%) | N=77 (%) | ||
| Room entry | 38 (17) | 16 (21) | 1.26 (0.66 – 2.43) | 0.50 |
| Room exitb | 124 (58) | 28 (37) | 0.44 (0.26 – 0.75) | 0.003 |
Fisher’s exact test was used for comparisons due to small cell sizes.
Eight room exit observations were missing because room exit could not be observed.
Table 5.
Healthcare professional hand hygiene observations, at first room entry/exit and all room entries/exits, by type of healthcare professional.
| Observation | Hand hygiene performed N (%) |
OR (95% CI) | p |
|---|---|---|---|
| First room visit by participating HCP | |||
| Room entry (n=77) | |||
| Nursea n=40 | 7 (18) | Reference | |
| Physician n=16 | 5 (31) | 0.47 (0.12 – 1.77) | 0.26 |
| Otherb n=21 | 2 (10) | 2.02 (0.38 – 10.70) | 0.41 |
| Room exit (n=77) | |||
| Nursea n=40 | 19 (48) | Reference | |
| Physician n=16 | 9 (56) | 0.70 (0.22 – 2.26) | 0.56 |
| Otherb n = 21 | 12 (57) | 0.68 (0.23 – 1.97) | 0.48 |
| All HCP room visits | |||
| Room entry (n=298) | |||
| Nursea n=150 | 38 (25) | Reference | |
| Physician n=71 | 10 (14) | 2.07 (0.97 – 4.44) | 0.06 |
| Otherb n=77 | 6 (8) | 4.02 (1.62 – 9.98) | 0.003 |
| Room exitc (n=290) | |||
| Nursea n=147 | 87 (59) | Reference | |
| Physician n=68 | 29 (43) | 1.95 (1.09 – 3.49) | 0.03 |
| Otherb n=75 | 36 (48) | 1.57 (0.90 – 2.75) | 0.11 |
Includes student nurses and nurse practitioners.
Includes patient care technicians, respiratory therapists, radiology techs, dieticians, pharmacist, pharmacy student, infection prevention technician, and unit secretary.
Eight room exit observations were missing because room exit could not be observed.
The association between HCP HH and surrogate marker detections is shown in Table 6. Although few associations were observed between either HH measure and surrogate marker detections, HCPs who performed HH immediately after the first room exit and before being swabbed were less likely than HCPs who did not perform HH at room exit to have fluorescence detected (20% vs. 49%; p=0.008).
Table 6.
Association between hand hygiene performance at room exit and detection of fluorescence and MS2 on healthcare professionals and on environmental surfaces touched by healthcare professionals.
| Observation | Hand hygiene performed | Hand hygiene not performed | OR (95% CI) | p | |
|---|---|---|---|---|---|
| First room exit by participating HCP | N=41 (%) | N=36 (%) | |||
| Fluorescent powder detected | 8 (20) | 18 (49) | 3.79 (1.38 – 10.38) | 0.008 | |
| MS2 detected | 8 (20) | 7 (19) | 0.93 (0.30 – 2.89) | 0.91 | |
| All HCP room exits | N = 29 (%) | N = 48 (%) | |||
| Fluorescent powder detected | 7 (24) | 19 (40) | 2.06 (0.74 – 5.76) | 0.17 | |
| MS2 detected | 7 (24) | 8 (17) | 0.63 (0.20 – 1.97) | 0.42 | |
Abbreviations: HCW, healthcare professional.
Discussion
In this study, transfer of both FP and MS2 was observed both inside and outside patient rooms, on participating HCPs, and on surfaces touched by HCPs after exiting patient rooms. Transfer of FP occurred more frequently than transfer of MS2; positive bacterial cultures were even less frequent.
Although few studies have utilized both FP and MS2 as surrogate markers, some have also reported higher rates of FP compared to MS2 detections.17,31 Others reported similar detection rates,19,32 or more frequent MS2 detections.21 This lack of agreement may indicate that neither marker performs significantly better than the other or may be related to differences in the means of detection (visual versus swabs). However, the two markers are thought to model different types of contamination: FP may model gross bacterial contamination, while MS2 may simulate viral contamination events.21 Therefore, different detection rates may be reasonable. More data are needed to determine which surrogate markers are better models for ARO transmission.
In contrast to surrogate markers, bacterial culture may identify actual ARO transmission events. This study focused on two AROs that routinely trigger contact precautions, MRSA and VRE, as well as MSSA. While MSSA does not routinely trigger contact precautions, it is a clinically relevant pathogen that causes significant morbidity in hospitalized patients.33,34 The greater frequency of surrogate marker detections as compared to ARO detections may suggest that FP and MS2 over-represent the likelihood of ARO transmission. Previous studies using MS2 to model the spread of Clostridioides difficile spores have also reported more frequent MS2 detections versus bacterial detections on HCP skin and clothing.19,35 However, in our study, both surrogate markers were present in all of the patient rooms, while only seven rooms had surfaces that were positive for VRE, MRSA, or MSSA at baseline. Therefore, the lower rate of positive bacterial cultures is not unexpected.
In this study, both surrogate markers were identified less frequently among HCPs caring for patients on contact precautions versus HCPs caring for patients not on contact precautions, although the difference only achieved significance for FP. We also observed that HCPs caring for patients on contact precautions more frequently performed HH at room exit, and that HCPs who performed HH had fewer FP detections. Previous studies have also reported an association between contact precautions and HH compliance,36,37 and between HH and fewer MS2 detections on the hands of HCP.38,39 These findings suggest that both contact precautions and HH play an important role in preventing the spread of AROs and provide additional data to support the role of contact precautions in preventing ARO transmission.
While we found no significant differences in the rate of FP detections among different types of HCPs, MS2 was more frequently detected among physicians compared to nurses. This observation may also be related to HH, as nurses were more likely than physicians to perform HH at room exit. As in prior studies,40 observed HCP HH compliance was low. However, differences in HH compliance by HCP job category suggest that a role exists for interventions promoting HH amongst all HCPs.
A key strength of this study is the use of multiple surrogate markers and bacterial cultures, which helps to generate a more complete model of pathogen transmission. Other strengths include the real-world hospital setting and detailed HCP observations. This study was subject to a few limitations. The small sample size may have limited the statistical power to detect differences in surrogate marker detections. This study also only included patients on contact precautions for VRE and MRSA, and only tested for VRE, MRSA, and MSSA. Therefore, it is unclear how our findings would translate to other AROs, such as C. difficile and multi-drug resistant gram-negative bacteria. Finally, despite detailed HCP observations, it was not always possible to observe HH occurring inside patient rooms when the door was closed. Therefore, we may have under-estimated HCP HH compliance; however, internal, routine HH observations support overall less than ideal HH compliance among hospital staff.
Despite these limitations, this study demonstrated transfer of both FP and MS2 beyond the initial areas of contamination inside patient rooms. This suggests that both surrogate markers may be useful tools to study ARO transmission. Larger studies using surrogate markers to assess ARO transmission and HCP cross-contamination are warranted, especially those focusing on the impact of contact precautions on ARO transmission.
Acknowledgements.
The study team would like to acknowledge the assistance and support of the nursing and staff members at Barnes-Jewish Hospital in this project.
Financial Support. This study was funded by a grant from the Centers for Disease Control and Prevention (3U54CK000162-05S1). The fluorescent powder used in this study was donated by the Glo Germ Company (Moab, UT). Glo Germ did not play a role in the development of the study design or result interpretation. Dr. Kwon is also supported by the Washington University Institute of Clinical and Translational Sciences grant UL1TR000448, sub-award KL2TR000450, from the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health (NIH) and grant 1K23AI137321-01A1 from the National Institute of Allergy and Infectious Diseases.
Footnotes
Preliminary results of the study described in this manuscript were presented at ID Week, 2016, held in New Orleans, LA.
Conflict of Interest. All authors report no potential conflicts of interest relevant to this article.
References
- 1.Boyce JM. Environmental contamination makes an important contribution to hospital infection. J Hosp Infect 2007;65 Suppl 2:50–54. [DOI] [PubMed] [Google Scholar]
- 2.Otter JA, Yezli S, Salkeld JA, French GL. Evidence that contaminated surfaces contribute to the transmission of hospital pathogens and an overview of strategies to address contaminated surfaces in hospital settings. Am J Infect Control 2013;41:S6–11. [DOI] [PubMed] [Google Scholar]
- 3.Suleyman G, Alangaden G, Bardossy AC. The Role of Environmental Contamination in the Transmission of Nosocomial Pathogens and Healthcare-Associated Infections. Curr Infect Dis Rep 2018;20:12. [DOI] [PubMed] [Google Scholar]
- 4.Weber DJ, Anderson D, Rutala WA. The role of the surface environment in healthcare-associated infections. Curr Opin Infect Dis 2013;26:338–344. [DOI] [PubMed] [Google Scholar]
- 5.Mitchell A, Spencer M, Edmiston C Role of healthcare apparel and other healthcare textiles in the transmission of pathogens: a review of the literature. J Hosp Infect 2015;90:285–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Muto CA, Jernigan JA, Ostrowsky BE, et al. SHEA guideline for preventing nosocomial transmission of multidrug-resistant strains of Staphylococcus aureus and enterococcus. Infect Control Hosp Epidemiol 2003;24:362–386. [DOI] [PubMed] [Google Scholar]
- 7.Morgan DJ, Murthy R, Munoz-Price LS, et al. Reconsidering contact precautions for endemic methicillin-resistant Staphylococcus aureus and vancomycin-resistant Enterococcus. Infect Control Hosp Epidemiol 2015;36:1163–1172. [DOI] [PubMed] [Google Scholar]
- 8.Morgan DJ, Wenzel RP, Bearman G. Contact Precautions for Endemic MRSA and VRE: Time to Retire Legal Mandates. JAMA 2017;318:329–330. [DOI] [PubMed] [Google Scholar]
- 9.Rubin MA, Samore MH, Harris AD. The Importance of Contact Precautions for Endemic Methicillin-Resistant Staphylococcus aureus and Vancomycin-Resistant Enterococci. JAMA 2018;319:863–864. [DOI] [PubMed] [Google Scholar]
- 10.Chen LF, Knelson LP, Gergen MF, et al. A prospective study of transmission of Multidrug-Resistant Organisms (MDROs) between environmental sites and hospitalized patients-the TransFER study. Infect Control Hosp Epidemiol 2019;40:47–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Drees M, Snydman DR, Schmid CH, et al. Prior environmental contamination increases the risk of acquisition of vancomycin-resistant enterococci. Clin Infect Dis 2008;46:678–685. [DOI] [PubMed] [Google Scholar]
- 12.Huang SS, Datta R, Platt R. Risk of acquiring antibiotic-resistant bacteria from prior room occupants. Arch Intern Med 2006;166:1945–1951. [DOI] [PubMed] [Google Scholar]
- 13.Hayden MK, Blom DW, Lyle EA, Moore CG, Weinstein RA. Risk of hand or glove contamination after contact with patients colonized with vancomycin-resistant enterococcus or the colonized patients’ environment. Infect Control Hosp Epidemiol 2008;29:149–154. [DOI] [PubMed] [Google Scholar]
- 14.Morgan DJ, Rogawski E, Thom KA, et al. Transfer of multidrug-resistant bacteria to healthcare workers’ gloves and gowns after patient contact increases with environmental contamination. Crit Care Med 2012;40:1045–1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Snyder GM, Thom KA, Furuno JP, et al. Detection of methicillin-resistant Staphylococcus aureus and vancomycin-resistant enterococci on the gowns and gloves of healthcare workers. Infect Control Hosp Epidemiol 2008;29:583–589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tenorio AR, Badri SM, Sahgal NB, et al. Effectiveness of gloves in the prevention of hand carriage of vancomycin-resistant enterococcus species by health care workers after patient care. Clin Infect Dis 2001;32:826–829. [DOI] [PubMed] [Google Scholar]
- 17.Kwon JH, Burnham CD, Reske KA, et al. Assessment of Healthcare Worker Protocol Deviations and Self-Contamination During Personal Protective Equipment Donning and Doffing. Infect Control Hosp Epidemiol 2017;38:1077–1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Duckro AN, Blom DW, Lyle EA, Weinstein RA, Hayden MK. Transfer of vancomycin-resistant enterococci via health care worker hands. Arch Intern Med 2005;165:302–307. [DOI] [PubMed] [Google Scholar]
- 19.Alhmidi H, Koganti S, Tomas ME, Cadnum JL, Jencson A, Donskey CJ. A pilot study to assess use of fluorescent lotion in patient care simulations to illustrate pathogen dissemination and train personnel in correct use of personal protective equipment. Antimicrob Resist Infect Control 2016;5:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Koganti S, Alhmidi H, Tomas ME, Cadnum JL, Jencson A, Donskey CJ. Evaluation of Hospital Floors as a Potential Source of Pathogen Dissemination Using a Nonpathogenic Virus as a Surrogate Marker. Infect Control Hosp Epidemiol 2016;37:1374–1377. [DOI] [PubMed] [Google Scholar]
- 21.Casanova L, Alfano-Sobsey E, Rutala WA, Weber DJ, Sobsey M. Virus transfer from personal protective equipment to healthcare employees’ skin and clothing. Emerg Infect Dis 2008;14:1291–1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bell T, Smoot J, Patterson J, Smalligan R, Jordan R. Ebola virus disease: The use of fluorescents as markers of contamination for personal protective equipment. IDCases 2015;2:27–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fattorini M, Ceriale E, Nante N, et al. Use of a fluorescent marker for assessing hospital bathroom cleanliness. Am J Infect Control 2016;44:1066–1068. [DOI] [PubMed] [Google Scholar]
- 24.Boyce JM, Havill NL, Havill HL, Mangione E, Dumigan DG, Moore BA. Comparison of fluorescent marker systems with 2 quantitative methods of assessing terminal cleaning practices. Infect Control Hosp Epidemiol 2011;32:1187–1193. [DOI] [PubMed] [Google Scholar]
- 25.Hung IC, Chang HY, Cheng A, et al. Application of a fluorescent marker with quantitative bioburden methods to assess cleanliness. Infect Control Hosp Epidemiol 2018;39:1296–1300. [DOI] [PubMed] [Google Scholar]
- 26.Manji R, Bythrow M, Branda JA, et al. Multi-center evaluation of the VITEK(R) MS system for mass spectrometric identification of non-Enterobacteriaceae Gram-negative bacilli. Eur J Clin Microbiol Infect Dis 2014;33:337–346. [DOI] [PubMed] [Google Scholar]
- 27.Richter SS, Sercia L, Branda JA, et al. Identification of Enterobacteriaceae by matrix-assisted laser desorption/ionization time-of-flight mass spectrometry using the VITEK MS system. Eur J Clin Microbiol Infect Dis 2013;32:1571–1578. [DOI] [PubMed] [Google Scholar]
- 28.McElvania TeKippe E, Burnham CA. Evaluation of the Bruker Biotyper and VITEK MS MALDI-TOF MS systems for the identification of unusual and/or difficult-to-identify microorganisms isolated from clinical specimens. Eur J Clin Microbiol Infect Dis 2014;33:2163–2171. [DOI] [PubMed] [Google Scholar]
- 29.El Feghaly RE, Stamm JE, Fritz SA, Burnham CA. Presence of the bla(Z) beta-lactamase gene in isolates of Staphylococcus aureus that appear penicillin susceptible by conventional phenotypic methods. Diagn Microbiol Infect Dis 2012;74:388–393. [DOI] [PubMed] [Google Scholar]
- 30.Fritz SA, Hogan PG, Singh LN, et al. Contamination of environmental surfaces with Staphylococcus aureus in households with children infected with methicillin-resistant S aureus. JAMA Pediatr 2014;168:1030–1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Casanova LM, Erukunuakpor K, Kraft CS, et al. Assessing Viral Transfer During Doffing of Ebola-Level Personal Protective Equipment in a Biocontainment Unit. Clin Infect Dis 2018;66:945–949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tomas ME, Kundrapu S, Thota P, et al. Contamination of Health Care Personnel During Removal of Personal Protective Equipment. JAMA internal medicine 2015;175:1904–1910. [DOI] [PubMed] [Google Scholar]
- 33.Thomsen IP, Kadari P, Soper NR, et al. Molecular Epidemiology of Invasive Staphylococcus aureus Infections and Concordance with Colonization Isolates. Journal Pediatr 2019;210:173–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hassoun A, Linden PK, Friedman B. Incidence, prevalence, and management of MRSA bacteremia across patient populations-a review of recent developments in MRSA management and treatment. Crit Care 2017;21:211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Alhmidi H, John A, Mana TC, et al. Evaluation of Viral Surrogate Markers for Study of Pathogen Dissemination During Simulations of Patient Care. Open Forum Infect Dis 2017;4:ofx128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bearman GM, Marra AR, Sessler CN, et al. A controlled trial of universal gloving versus contact precautions for preventing the transmission of multidrug-resistant organisms. Am J Infect Control 2007;35:650–655. [DOI] [PubMed] [Google Scholar]
- 37.Harris AD, Pineles L, Belton B, et al. Universal glove and gown use and acquisition of antibiotic-resistant bacteria in the ICU: a randomized trial. JAMA 2013;310:1571–1580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sassi HP, Sifuentes LY, Koenig DW, et al. Control of the spread of viruses in a long-term care facility using hygiene protocols. Am J Infect Control 2015;43:702–706. [DOI] [PubMed] [Google Scholar]
- 39.Julian TR, Leckie JO, Boehm AB. Virus transfer between fingerpads and fomites. J Applied Microbiol 2010;109:1868–1874. [DOI] [PubMed] [Google Scholar]
- 40.Mastrandrea R, Soto-Aladro A, Brouqui P, Barrat A. Enhancing the evaluation of pathogen transmission risk in a hospital by merging hand-hygiene compliance and contact data: a proof-of-concept study. BMC Res Notes 2015;8:426. [DOI] [PMC free article] [PubMed] [Google Scholar]


