Abstract
Osteomyelitis is a rare initial presentation of HIV. We report a case of a 25-year-old, apparently well man presenting with a traumatic, pathological fracture of the right radius. He had a 2-week history of low-grade fever, swelling and purulent discharge of the radial aspect of his right forearm. Osteomyelitis, secondary bacteraemia and pneumonia were clues that led physicians to test for HIV. Multiple debridement, sequestrectomy and vacuum-assisted closure were done. Tissue cultures revealed Mycobacterium tuberculosis (TB) and methicillin-sensitive Staphylococcus aureus. He was treated successfully with 6 weeks of culture-guided intravenous oxacillin, staphylococcal decontamination and first-line anti-TB regimen (rifampicin, isoniazid, ethambutol, pyrazinamide). Antiretroviral agents were started thereafter. Successful infection control and preservation of limb functionality was achieved with a multidisciplinary team approach. To our knowledge this is the first reported case of an adult patient with HIV presenting with tuberculous and pyogenic osteomyelitis of the radial bone.
Keywords: musculoskeletal and joint disorders, bone and joint infections, HIV / AIDS, orthopaedic and trauma surgery, TB and other respiratory infections
Background
Worldwide, tuberculosis (TB) remains to be one of the top causes of death.1 In the Philippines, TB is the sixth leading cause of death and remains even more so with the current HIV epidemic.2 Recognising the protean clinical manifestations of atypical extrapulmonary TB (EPTB) is of paramount importance. Osteoarticular tuberculosis accounts for only 1%–3% of all TB cases; moreover, isolated involvement of long bones is a rare presentation.3 We report a case of a pathological fracture caused by tuberculous and pyogenic osteomyelitis of the radial bone in a newly diagnosed young adult Filipino man with HIV.
Case presentation
A 25-year-old, apparently well Filipino man, presented in the emergency room with a 2-week history of post-traumatic swelling on the radial aspect of his right forearm which he sustained after playing volleyball. The swelling progressed to an enlarging pustule with eventual rupture draining gross purulent foul-smelling discharge. Systemic symptoms included productive cough, afternoon low-grade fever and unintentional weight loss of 20%. He was initially prescribed and took sultamicillin 750 mg three times per day, mefenamic acid for pain and applied mupirocin ointment to the lesion, but his symptoms did not improve. Social history revealed that he had four male partners with whom he had unprotected (receptive anal) sexual encounters. He denied illicit drug use.
On physical examination, the vital signs were blood pressure of 100/60 mm Hg, heart rate of 128 beats/min regular, respiratory rate of 24 breaths/min and temperature of 36.7°C. His body mass index was 19 kg/m2. Oxygen saturation was 96% on room air. He had thick whitish plaques on his oral mucosa, suggestive of an oral thrush. No lymphadenopathies were noted. Lung examination revealed crackles on the right middle to lower lung fields. There was a 3×3 cm wound on the dorsoradial aspect of the right forearm with gross yellowish purulent discharge (see figure 1). The surrounding area was swollen, warm, erythematous and tender. Motor strength of the right hand showed 4/5 finger abductor, adductor, flexor and extensor activity. The rest of the physical examination was unremarkable. Baseline funduscopy was unremarkable for signs of septic emboli, cytomegalovirus, or HIV retinopathy.
Figure 1.
Preoperative wound: 3×3 cm, round ulcerated wound with a purulent base at the dorsoradial aspect of forearm. Tendon and fascia are visualised at the base of the lesion.
Investigations
Initial laboratory results revealed normocytic normochromic anaemia with a haemoglobin of 109 g/L, leucocytosis with neutrophilic predominance (white blood cell count 16.9×109/L; 91% neutrophils, 5% lymphocytes, 3% monocytes) and thrombocytopenia (platelet count of 107×109/L). Serum electrolytes were normal. He had elevated creatinine of 388 µmol/L, blood urea nitrogen of 26.5 mmol/L, C reactive protein of >12 mg/L and ferritin of >2000 µg/L, all suggestive of ongoing sepsis (see table 1).
Table 1.
Baseline laboratories on admission
| Result | Reference range | |
| Complete blood count | ||
| Hgb (g/L) | 109 | 135–180 |
| Hct | 36 | 0.40–0.54 |
| Platelet | 107 | 150–450 |
| WBC (x109/L) | 16.9 | 4.50–11.0 |
| Neutrophil | 91% | 50–70 |
| Lymphocyte | 5% | 20–50 |
| Monocyte | 3% | 2–9 |
| Eosinophil | 1% | 0–6 |
| Basophil | 0% | 0–2 |
| Serum chemistry | ||
| Na (mmol/L) | 136 | 137–145 |
| K (mmol/L) | 3.8 | 3.5–5.1 |
| Cl (mmol/L) | 102 | 98–107 |
| Mg (mmol/L) | 0.66 | 0.7–1.0 |
| Calcium (mmol/L) | 2.15 | 2.10–2.55 |
| Crea (µmol/L) | 388 | 58–110 |
| eGFR (mL/min/1.73m2) | 17 | |
| BUN (mmol/L) | 26.5 | 3.7–7.1 |
| BUN/Crea ratio | 16.9 | |
| AST (U/L) | 25 | <35 |
| ALT (IU/L) | 38 | <36 |
| Albumin (g/L) | 27 | 35–50 |
| CRP (mg/L) | >12 | <6 |
ALT, alanine aminotransferase; AST, aspartate aminotransferase; BUN, blood urea nitrogen; CRP, C reactive protein; eGFR, estimated glomerular filtration rate; Hct, haematocrit; Hgb, haemoglobin; WBC, white blood count.
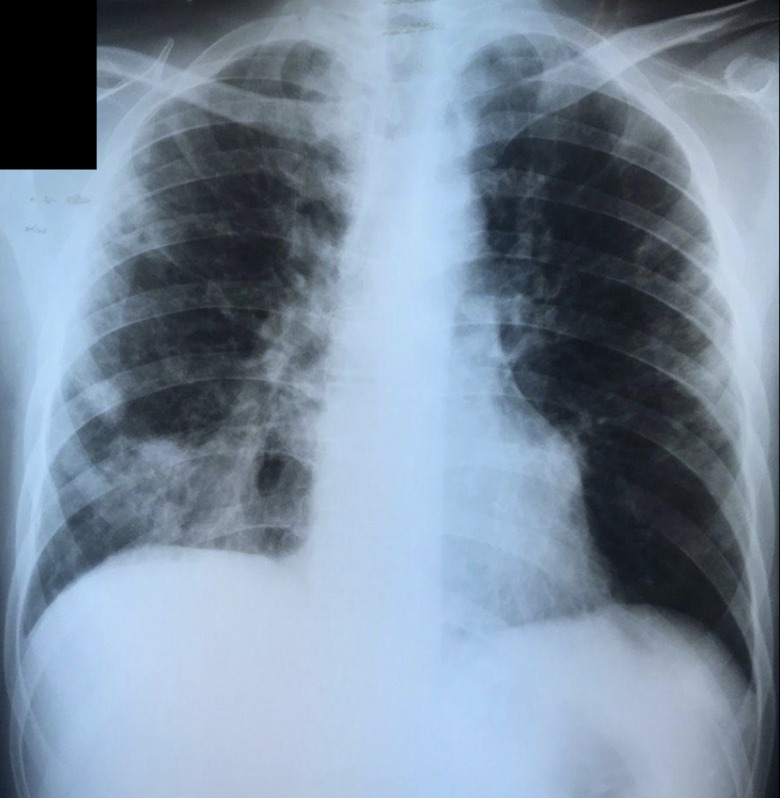
Chest radiograph showed suspicious bilateral apical densities and reticulonodular infiltrates on the right middle and lower lung fields consistent with pneumonia (figure 2). Right forearm radiograph showed lytic changes on the middle diaphysis of the radius, and large sequestrum and involucrum consistent with chronic osteomyelitis (figure 3).
Figure 2.
Chest radiograph shows reticulonodular opacities on the right lower lobe and suspicious bilateral apical opacities.
Figure 3.

Preoperative anteroposterior radiograph of the right forearm shows lytic changes (arrows) over the middle diaphysis of the radius. A large radio-opaque sequestrum (asterisk) surrounded by more radiolucent involucrum was noted on the midshaft of the radius consistent with chronic osteomyelitis.
Initial microbiological work-up showed sputum gram stain of >25 polymorphonuclear cells per low power field (LPF), <25 squamous cells/LPF and gram-negative bacilli 1–5 per oil-immersion field. Two consecutive sputum acid-fast bacilli smears were negative. Blood culture revealed gram-positive cocci in pairs after 27-hour incubation on two sites but showed no growth on the 5th day of incubation. Induced sputum Pneumocystis jirovecii stain was negative. Intraoperative tissue culture taken from the middle diaphysis of the radius was positive for Staphylococcus aureus. This was sensitive to clindamycin (<0.25 µg/mL), erythromycin (0.5 µg/mL), oxacillin (<0.25 µg/mL), but resistant to penicillin and trimethoprim sulfamethoxazole. Tissue acid fast bacilli was negative but TB PCR was positive. Unfortunately, additional wound culture and TB PCR from the distal radius were not collected during the initial debridement.
We widened our investigation for signs of immunodeficiency due to the presence of infection in multiple organs as well as the presence of infection with an opportunistic organism in a relatively young man with no known comorbidities. Initial screening for HIV with ELISA was positive with a CD4 count of 12 cells/mm3. Hepatitis panel was anti-HBs and anti-HBc IgG reactive consistent with past hepatitis B infection. Rapid plasma reagin was non-reactive, herpes simplex virus (HSV) I IgG was positive (Demedetic 104 u/mL) and HSV II IgG Biokit was negative. Screening for diabetes mellitus with fasting blood sugar and 75 g oral glucose tolerance test was normal.
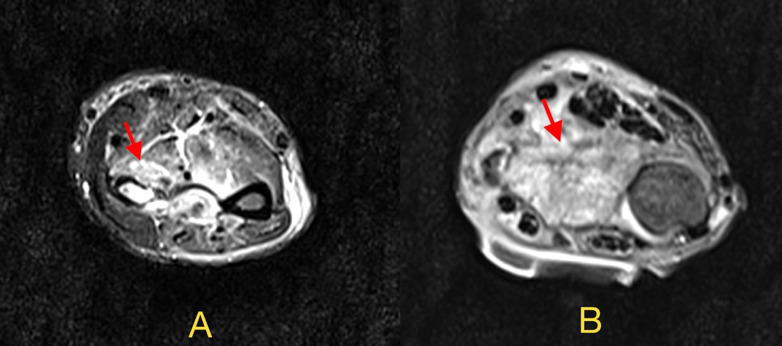
An MRI of the right forearm and hand was ordered for further surgical planning and management. This revealed right radial osteomyelitis, acute on chronic, with distal humeral epicondyle, and olecranon process involvement. A small complex fluid collection measuring 1.5×0.8 cm was seen compatible with proximal preradial abscess formation. There was also extensive myositis of the flexor and extensor muscles and accompanying synovial sheath synovitis of the distal radioulnar joint. The radial and ulnar neurovascular bundle and nerves were intact (figures 4A, B and 5A, B).
Figure 4.
(A) Coronal T1 MRI of the right forearm shows abnormal marrow signals (arrows) with restricted diffusion on the right radius extending from its proximal head to the distal radial epiphysial aspects associated with cortical erosive and lytic changes. This is in contrast to the normal ulnar bone on the right side of the image. (B) T2 MRI shows hyperintense lesions (yellow arrows) and abnormal marrow signals on the olecranon process and the humeral epicondyle.
Figure 5.
(A) T2 turbo inversion recovery magnitude MRI transverse view of the distal right forearm which shows 1.5×0.8 cm complex fluid collection (red arrow) on the ventral aspect of the radius. Abnormal signals are seen in the overlying subcutaneous fat. (B) T1 MRI transverse view of the right distal forearm shows loss of the cortical outline of the right radius. The abscess surrounding the radius is also seen (red arrow).
Bone densitometry showed signs of osteopenia. Bone mineral density Z-score are as follows: lumbar (−1.5), total body (−0.3), total hip (−1.3 to −1.5) and femur (−1.1 to −0.9). His vitamin D assay was insufficient at 13.57 ng/mL (normal value: 30–100 ng/mL).
Differential diagnosis
Findings of a pathological fracture with purulent discharge on the arm of a patient with newly diagnosed HIV, point to subacute to chronic pyogenic osteomyelitis and malignancy as differential diagnoses. Opportunistic infections are kept in mind in this patient population. Both of these conditions can lead to constitutional symptoms and focal symptoms at the site of tumour growth or infection. Aggressive B cell lymphomas associated with HIV can lead to bone infiltration and pathological fractures accompanied with cytopenias. Kaposi sarcoma (KS) has rarely been reported to involve musculoskeletal tissue. Only patients with long-standing locally aggressive cutaneous KS have been implicated to cause osteolytic lesions and pathological fractures. Histopathology of excised tissue and fungal cultures is essential in distinguishing between these other conditions.
Treatment
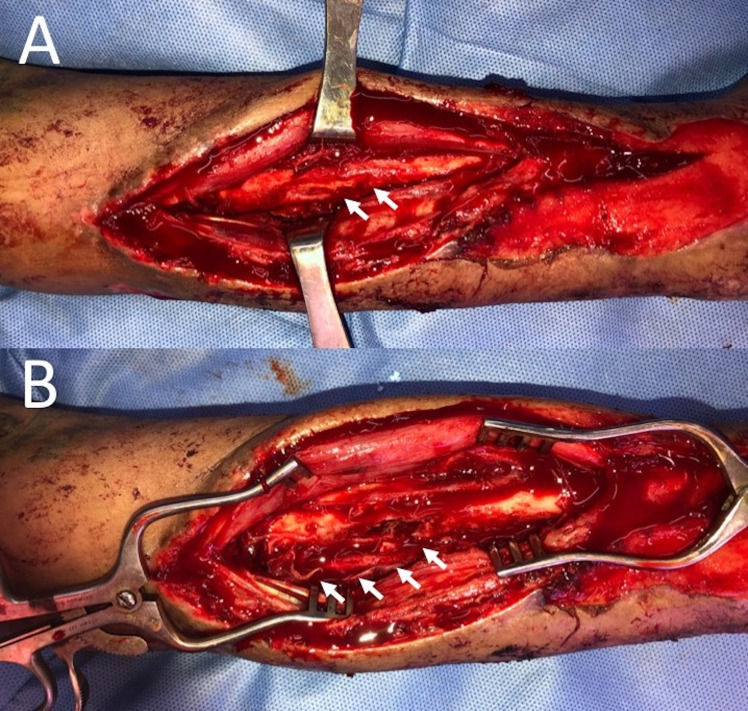
Intravenous piperacillin–tazobactam, azithromycin and vancomycin were started on admission for empirical treatment of community-acquired pneumonia, osteomyelitis and oral candidiasis. He underwent initial surgical debridement with postoperative vacuum-assisted closure. Repeat debridement, curettage, sequestrectomy and right forearm splinting was done a week later. All necrotic bone and soft tissue were removed until good bleeding bone and healthy surrounding soft tissues were visualised. Sinuses were also excised. Intraoperatively, a 1.5×1.5 cm defect was noted on the posterior cortex of the radius that was filled with caseous material, involucrum and a 1×1 cm bony sequestrum (see figure 6). The distal radius still had intact periosteum. Intraoperative biopsy was consistent with necrotic bone sequestrum. Given the relatively small size of the wound and the superficial nature, we deemed healing using foam dressings as sufficient coverage, and did not see the need to do skin grafting which may result in complications such as donor site morbidity. A long arm splint was maintained postoperatively to avoid pronation and supination until healing occurred for about 3 months. No external fixation or bone substitute was done because only less than 30% of the cortex was removed. Locally delivered antibiotics were not used because no dead space was appreciated after removing the necrotic tissue.
Figure 6.
(A) Intraoperatively, the middle third of the radial shaft was visualised via dorsal approach revealing a hard layer of involucrum (arrow) around a 2.0×1.5 cm segment of sequestrum (not seen). There were no pockets of abscess. (B) A 3.0×1.5 cm defect on the dorsomedial aspect of the radius and less than 50% of the circumference of the radial shaft were left after debridement, curettage and sequestrectomy. The sequestrum was removed, but the bleeding involucrum that exhibited the paprika sign was preserved.
During the course of treatment, the patient had prolonged lysis of fever postoperatively, hypotensive episodes and sputum production despite being on the 10th day of intravenous vancomycin. Tissue and sputum cultures at this time showed methicillin-sensitive S. aureus (MSSA). The decision to extend vancomycin administration (and start meropenem) was discussed together with an infectious disease specialist to cover for both hospital-acquired pneumonia, sepsis and the radial bone osteomyelitis. However, due to the development of vancomycin-induced neutropenia with a nadir of absolute neutrophil count of 517 cells/µL on day 12 of treatment, the decision was then to shift to culture-guided oxacillin to complete 6-week intravenous antibiotic therapy. There was lysis of fever and improvement of neutropenia when antibiotics were shifted to oxacillin.
Staphylococcal decontamination was done with mupirocin ointment and chlorhexidine bath since his sputum, tissue and blood cultures were all positive for MSSA. First-line anti-TB treatment (rifampicin, isoniazid, ethambutol, pyrazinamide) was given after tissue TB PCR results were positive. Delayed TB PCR results obtained 3 weeks after sending were due to the limited resource setting. Pyridoxine supplementation was added to prevent isoniazid-related peripheral neuropathy. He also developed hospital-acquired pneumonia (Acinetobacter baumanii) that resolved with minocycline treatment.
Antiretroviral therapy (tenofovir/lamivudine/efavirenz) was started 2 weeks after initiation of TB treatment. The patient was sent home with a right forearm splint and was advised to continue his anti-TB medications, vitamin D supplementation and antiretroviral agents.
Outcome and follow-up
After discharge, the patient had regular follow-up at the Philippine General Hospital outpatient primary care internal medicine clinic and HIV clinic. He had good compliance with the anti-TB regimen and antiretroviral regimen at 6 months post-discharge. No adverse drug reactions were noted. There was resolution of fever, cough and forearm pain. The patient had full mobility of his right forearm with good functional capacity. He regularly follows up at the outpatient clinic, however compliance to antiretroviral medications were an issue due to socioeconomic circumstances. The CD4 count on subsequent follow-ups were 20 cells/mm3 (5 months) and 6 cells/mm3 (1 year). Postoperative imaging of the forearm after 6 months showed marked improvement and reduced areas of radiolucency with new bone formation at the midshaft of the radius (figure 7A, B).
Figure 7.
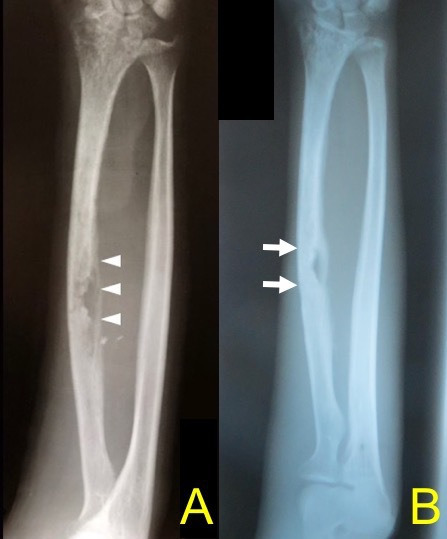
(A) After debridement, curettage and sequestrectomy, this postoperative radiograph shows bone loss (arrowheads) exhibited by radiolucent areas at the midshaft of the radius. (B) 6 months postoperative imaging shows reduced areas of radiolucency with new bone formation at the midshaft of the radius which signifies improvement.
Discussion
Skeletal tuberculosis can affect virtually any bone in the body, although it most commonly involves the spine and the hips.4–6 TB occurrence in long bones accounts for only 1% of all skeletal TB cases.7 Those who develop the disease follow a bimodal pattern (<30 years old and >55 years old) as either primary infection or secondary reactivation from a pulmonary focus that spreads to osteoarticular sites haematogenously.8 9 Lymphatic and contiguous local spread have also been described. The epiphysial and metaphyseal regions are usual common targets in long bones due to the rich vascular supply, with diaphyseal regions less commonly affected.8
The clinical presentation of skeletal TB commonly includes local symptoms (eg, pain, tenderness and limitation of motion if with joint involvement) or in approximately 20%–30% of cases, may include constitutional symptoms (eg, malaise, low-grade fever, night sweats, weight loss) as well. Cold abscesses and sinus tract formation can also occur in TB osteomyelitis.7 8 Radiological findings can range from soft tissue swelling, periosteal reaction, osteopenia/osteoporosis, cystic formation and less commonly, sclerosis and sequestration.8–10 Skeletal TB usually presents with corticomedullary destruction and juxtacortical abscess formation. Sequestra formation is less common.11 Similar case reports of radial bone involvement in tuberculous osteomyelitis were mostly seen in children and infants, perhaps because of the rich vascular supply of the physeal plates during rapid bone growth in developmental stages.11–13
This case was highly atypical because of the site of involvement, the occult nature of its clinical progression, and the dual causality being Mycobacterium tuberculosis and MSSA.
S. aureus bacteraemia and recurrent infections continue to be a significant cause of morbidity among people living with HIV (PLHIV), particularly those with a recent history of intravenous drug use, neutropenia or lymphatic obstruction.14 High nasal carriage rate has also been reported and may play a role in the development of both local and disseminated infections.15 Although our patient had no intravenous drug use, nasal carriage and the sustained breach on the cutaneous barrier may have predisposed him to MSSA osteomyelitis and subsequent bacteraemia.
The coinfection of tuberculosis and HIV has also led to an increase in the incidence of EPTB. In the USA, it is reported that about 10%–20% of EPTB occur in PLHIV while up to one-third of osteoarticular TB cases in Africa are HIV positive.16
In a case report by Akiki and Bilde, a young, healthy 20-year-old man presented with post-traumatic knee pain which was later found to be M. haemophilum osteomyelitis.17 Investigation for possible causes of immunosuppression led to the diagnosis of HIV infection and AIDS, similar to the approach done for our patient. A 3-year prospective study found non-tuberculous mycobacterium (NTM), particularly M. haemophilum, to be the causative agent in 44% of cases of focal osteomyelitis among 25 patients living with HIV.18 In fact, at the peak of the AIDS epidemic in the 1980s, M. haemophilum was one of the leading differential diagnoses for any osteolytic lesion in patients with AIDS.17 18 Some case reports have also shown Mycobacterium avium complex to be another NTM shown to cause osteomyelitis among PLHIV, although this remains to be rare.19 20
Case reports by Mannepalli et al and Tripathi et al show the emergence of M. tuberculosis as another causative agent of osteomyelitis among PLHIV that should not be forgotten.21 22 A high degree of clinical suspicion is needed to avoid missed opportunities for diagnosis. Our case report aims to highlight that TB osteomyelitis may even be an initial presentation of HIV in some cases.
Immunosuppressed states such as HIV infection increase the risk for developing osteoarticular tuberculosis.6 8 This is due to the lack of the cellular immune response (CD4− and CD8− T cells) responsible for preventing the reactivation of mycobacterial foci.23 Inadequate neutrophil bactericidal capacity, defective chemotaxis and decreased production of immunoglobulins by B lymphocytes may make them prone to infections with common pathogens as well.24 As the immune defences fail, clinical and widespread disease from opportunistic organisms become more apparent.
Diagnosis is often delayed due to the paucibacillary nature of osseous tuberculosis. Acid fast smears and mycobacterial culture, the gold standard for diagnosing TB, are usually low yield. Alternative diagnostic methods include DNA detection using TB PCR and GeneXpert which have higher sensitivity.
With regards to therapy, the dilemma is the same. TB bacilli harboured within sequestrum and necrotic tissue are inaccessible to chemotherapeutic agents due to poor perfusion.13 A combined medical-surgical treatment approach cannot be emphasised enough to ensure eradication of the infection.
The multidisciplinary approach to management of this case encompasses: (1) aggressive treatment of his sepsis and pneumonia on admission; (2) early and multiple debridement to remove all infected and necrotic tissue; (3) isolation of the pathogens for culture-directed antibiotic treatment; (4) tissue reconstruction; and (5) rehabilitative efforts to preserve function and hand mobility.
Due to the extent of involved bone, multiple debridement procedures ran the risk of destabilising the remaining bone. This was a shared decision the surgical team and the patient took to ensure eradication of contaminated tissue while at the same time, preserve forearm function and improve tissue healing. High-resolution imaging with MRI was vital in the preoperative planning in the approach and extent of debridement. Vacuum-assisted closure was initially used to aid in stimulation of granulation tissue, but no significant soft tissue defects were noted in the definitive surgery that necessitated further reconstruction. Curettage and debridement also provided an opportunity to obtain tissue samples for culture-guided antibiotics, and to exclude differential diagnoses such as malignancy or fungal infection.25 Interestingly, this case demonstrates concomitant tuberculosis and bacterial pyogenic osteomyelitis.
Based on Philippine guidelines, anti-TB treatment consists of a 2-month intensive phase (with oral rifampicin, isoniazid, ethambutol and pyrazinamide) followed by a 10-month maintenance phase (of oral rifampicin and ethambutol).26 This was accompanied by empirical intravenous vancomycin which was then shifted to a 6-week course of culture-guided intravenous oxacillin therapy. A team approach was essential in coordinating the medical, surgical and rehabilitative management of this patient.
To our knowledge this is the first reported case of an adult patient with HIV presenting with tuberculous and pyogenic osteomyelitis of the radial bone.
Learning points.
The occurrence of osteomyelitis among young, healthy patients should prompt further investigations for causes of immunosuppression such as HIV infection.
More than one pathogen may be implicated in osteomyelitis infections among people living with HIV.
In addition to acid fast bacilli smears and mycobacterial cultures, DNA detection methods such as TB PCR and GeneXpert increase the sensitivity and timely diagnosis of osseous tuberculosis.
MRI is an invaluable tool in perioperative planning since it demonstrates the extent of tissue involvement in osteomyelitis.
Three things must be considered in the operative management of long bone osteomyelitis involving the radius: (1) eradication of infection, (2) microbiological diagnosis for antibiotic guidance, and (3) preservation and/or restoration of hand functionality and mobility.
Acknowledgments
We thank everyone in the team who took care of this patient, especially Dr Sebar Sala, infectious disease specialist, and Dr Nilo T Paner, the consultant orthopaedic surgeon.
Footnotes
Twitter: @nigelsantosmd, @DTomacruzMD
Contributors: NJCS was the primary author and attending physician of this case. IDVT was the secondary author and was also an attending physician of this case. She contributed to the pathophysiology and review of related literature. FLL-A was our case consultant, coauthor, final editor and senior attending physician of this case. PVSJR was the orthopaedic surgeon and coauthored the orthopaedic surgical aspects of this case.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.World Health Organization Global tuberculosis report: Executive summary 2018, 2018. Available: https://www.who.int/tb/publications/global_report/tb18_ExecSum_web_4Oct18.pdf?ua= [Accessed 20 Oct 2019].
- 2.World Health Organization World Health organization: Western Pacific region 2019. tuberculosis, major health problem in the Philippines. Available: http://www.wpro.who.int/philippines/areas/communicable_diseases/tb/story_continuation_tb_area_page/en/ [Accessed 2 Oct 2019].
- 3.Birole U, Ranade A, Mone M. A case report of an unusual case of tuberculous osteomyelitis causing spontaneous pathological fracture of humerus in a middle aged female. J Orthop Case Rep 2017;7:41–5. 10.13107/jocr.2250-0685.680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fuentes Ferrer M, Gutiérrez Torres L, Ayala Ramírez O, et al. Tuberculosis of the spine. A systematic review of case series. Int Orthop 2012;36:221–31. 10.1007/s00264-011-1414-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Trecarichi EM, Di Meco E, Mazzotta V, et al. Tuberculous spondylodiscitis: epidemiology, clinical features, treatment, and outcome. Eur Rev Med Pharmacol Sci 2012;16:58–72. [PubMed] [Google Scholar]
- 6.Peto HM, Pratt RH, Harrington TA, et al. Epidemiology of extrapulmonary tuberculosis in the United States, 1993-2006. Clin Infect Dis 2009;49:1350–7. 10.1086/605559 [DOI] [PubMed] [Google Scholar]
- 7.Hsieh CK, Miltner LJ, Chang CP. Tuberculosis of the shaft of the large long bones of the extremities. J Bone Joint Surg Am 1934;3:545–63. [Google Scholar]
- 8.Procopie I, Popescu EL, Huplea V, et al. Osteoraticular Tuberculosis-Brief review of clinical morphological and therapeutic profiles. Curr Health Sci J 2017;43:171–90. 10.12865/CHSJ.43.03.01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Watts HG, Lifeso RM. Tuberculosis of bones and joints. J Bone Joint Surg Am 1996;78:288–98. 10.2106/00004623-199602000-00019 [DOI] [PubMed] [Google Scholar]
- 10.De Backer AI, Vanhoenacker FM, Sanghvi DA. Imaging features of extraaxial musculoskeletal tuberculosis. Indian J Radiol Imaging 2009;19:176–86. 10.4103/0971-3026.54873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sarkar AS, Garg AK, Bandyopadhyay A, et al. Tuberculosis of distal radius presenting as cystic lesion in a nine-month-old infant: a rare case report. J Clin Diagn Res 2016;10:RD06–7. 10.7860/JCDR/2016/19916.8564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gomes VMT, Dos Santos TCS, Cañete LAQ, et al. Tuberculosis of the radius in a child. Radiol Bras 2019;52:61–2. 10.1590/0100-3984.2017.0114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rasool MN, Orth FCS. Tuberculosis – the masquerader of bone lesions in children. SA Orthopaedic Journal 2009:21–5. [Google Scholar]
- 14.Jacobson MA, Gellermann H, Chambers H. Staphylococcus aureus bacteremia and recurrent staphylococcal infection in patients with acquired immunodeficiency syndrome and AIDS-related complex. Am J Med 1988;85:172–6. 10.1016/S0002-9343(88)80337-1 [DOI] [PubMed] [Google Scholar]
- 15.Raviglione MC, Mariuz P, Pablos-Mendez A, et al. HighStaphylococcus aureus nasal carriage rate in patients with acquired immunodeficiency syndrome or AIDS-related complex. Am J Infect Control 1990;18:64–9. 10.1016/0196-6553(90)90083-5 [DOI] [PubMed] [Google Scholar]
- 16.Goodman PC. Tuberculosis and AIDS. Radiol Clin North Am 1995;33:707–17. [PubMed] [Google Scholar]
- 17.Akiki A, Bilde Y. Atypical focal osteomyelitis as initial manifestation of AIDS. Case Rep Orthop 2011;2011:1–4. 10.1155/2011/541873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hirsch R, Miller SM, Kazi S, et al. Human immunodeficiency virus-associated atypical mycobacterial skeletal infections. Semin Arthritis Rheum 1996;25:347–56. 10.1016/S0049-0172(96)80020-5 [DOI] [PubMed] [Google Scholar]
- 19.Kadzielski J, Smith M, Baran JL, et al. Nontuberculous mycobacterial osteomyelitis: a case report of Mycobacterium avium intracellulare complex tibial osteomyelitis in the setting of HIV/AIDS. Orthop J Harv Med Sch 2009;11:108–11. [Google Scholar]
- 20.Gray ME, Liu PW, Wispelwey B. Mycobacterium avium complex vertebral osteomyelitis in the absence of HIV infection: a case report and review. BMC Infect Dis 2018;18:235. 10.1186/s12879-018-3143-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mannepalli S, Mitchell-Samon L, Guzman N, et al. Mycobacterium tuberculosis osteomyelitis in a patient with human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS): a case report. Cases J 2010;3:67. 10.1186/1757-1626-3-67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tripathi AK, Gupta N, Khanna M, et al. Tuberculosis presenting as osteolytic soft tissue swellings of skull in HIV positive patient: a case report. Indian J Tuberc 2007;54:193–5. [PubMed] [Google Scholar]
- 23.Kaufmann SHE, Cole ST, Mizrahi V, et al. Mycobacterium tuberculosis and the host response. J Exp Med 2005;201:1693–7. 10.1084/jem.20050842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mayer-Barber KD, Barber DL. Innate and adaptive cellular immune responses to Mycobacterium tuberculosis infection. Cold Spring Harb Perspect Med 2015;5:1–3. 10.1101/cshperspect.a018424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Parsons B, Strauss E. Surgical management of chronic osteomyelitis. Am J Surg 2004;188:57–66. 10.1016/S0002-9610(03)00292-7 [DOI] [PubMed] [Google Scholar]
- 26.Philippine Coalition Against Tuberculosis Clinical practice guidelines for the diagnosis, treatment, prevention and control of tuberculosis in adult Filipinos 2016 update, 2016. Available: http://www.ship.ph/wp-content/uploads/2018/11/CPGs-2016-tuberculosis.pdf [Accessed 16 May 2020].