Abstract
In the field of modern dentistry, ideal three-dimensional positioning of dental implant with optimal prosthetic fit offers successful long-term outcomes. To achieve such accurate implant placement, presurgical evaluation of hard and soft tissue matters the most. Their efforts can be attained using various application programs such as digital imaging, implant planning software, laboratory- or computer-assisted surgical guides, and dynamic navigation approach. To overcome different opinions and choices regarding guided surgery, this article explains an evidence-based literature review to assess its various outcomes and allowing informed choices before using various guided surgical techniques based on its expectation and reality outcomes. This highlights a clinician's choice to guide his successful implant surgery without causing distress in the midway of treatment. An online search was done on PubMed/Medline database to bring in accuracy to the expertise. This review includes reference of publications from 2000 to 2019, which is related to promising outcomes using computer-assisted static or dynamic navigation system for the placement of implant. Out of these, 809 were related to the computer-guided implant placement. Relevant papers were chosen in accordance with the inclusion and exclusion criteria. This review article contemplates to reflect the fact that computer-guided approach is considered to offer more predictable, safer, and faster implant placement with the predetermined final prosthetic outfit. Thus, digital planning and placing of dental implants in the correct position keep escalating to a higher achievement levels than a classical freehand approach. Nevertheless, this guided surgical approach also holds some errors and risks, which must be identified and rectified.
Keywords: Accuracy, computer-assisted surgery, dental implants, dynamic navigation system, flapless approach, guided implant surgery, static guidance system, surgical guide
INTRODUCTION
Implants play a major role in determining the efficiency of the core practices among dental practitioners. Ideal implant placement favors good esthetic and prosthetic outcomes with optimal occlusion and maintaining the health of peri-implant tissues with good oral hygiene and proper implant loading.[1] Improper positioning of implant would lead to unfavorable mechanical load causing peri-implantitis and loss of implant at an early stage. More than mechanical complications, poor implant positioning could lead to biological complications due to the inability of maintaining proper hygiene. Many computer programs are available to help with three-dimensional (3D) implant positioning. Precise preoperative planning for taking future consideration on prosthetic and functional aspects leads to long-term success and survival of implants. Nowadays, the surgical guide performs an important role in transferring the premapped idea to the site of implant placement at their designated positions (angulation and depth).[2]
The surgical template is defined as a “guide to assist proper surgical placement and angulation of dental implants.”[3] The guided implant surgery provides the following: (i) accuracy and precision for placement of implants, (ii) minimally invasive approach to surgery with reduced patient morbidity and avoiding damage to critical anatomic structures, (iii) second-stage implant surgery can be avoided, (iv) use of surgical stents has made immediate loading of implant possible by correct positioning and achieving its primary stability, and (v) less treatment time is needed for the procedure.
HISTORICAL PERSPECTIVE
In the late 1980s, several software programs using computerized tomography to picturize the human head were available. In 1992, a frameless system called the 'Viewing Wand' was the first navigation unit developed surgically by Ontario-based team for neurosurgery.[4] For the purpose of surgical planning and navigation, before and during the operation, this system served as an adjunct to computerized tomography along with magnetic resonance imaging and positron emission tomography. In the following years, surgical navigation became popular in medical field, especially in neurosurgery.[4,5,6] Thus the advantage of using this computer-assisted surgery is the precision it offers.
Later as in medicine, 3D imaging was used in dentistry for presurgical planning and guiding the placement of dental implants during surgery. In 1988, D'haese et al.[7] described the purpose of diagnosing and evaluation of alveolar ridges using dental software to interpret the computerized tomography axial slices into 'three-dimensional cross-sectional images,' which was first introduced by Columbia. Later in 1991, ImageMaster-101 combination software was developed, which provided graphic images of dental implants compared to the cross-sectional images. In the succeeding years, a surgical guide was introduced to gauge the depth and direction of osteotomy site. Recently, newer modalities for guided surgical approach were developed. In 2000, the first dynamic navigation-guided surgery in the field of implant dentistry was introduced.[7]
METHODOLOGY
A complete literature search was done in PubMed/Medline for articles available in English language to review surgical expectations and experience reality of guided implant surgery for implant placement, in lieu with the key terms as “Dental implants, guided implant surgery, computer-assisted surgery, surgical guide, static guidance system, dynamic navigation system, and accuracy in dental surgery.” The relevant papers were chosen according to the inclusion and exclusion criteria. The literature search revealed that most of the studies included were preclinical, clinical, in vitro, and case reports describing the outcomes using computer-assisted static or dynamic navigation systems for implant placement [Chart 1]. All publications focusing freehand approach, manual surgical guide, cadaver, or animal study model of implant placement were excluded.
Chart 1.
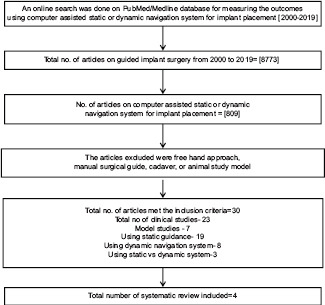
The steps used for study selection
TYPES OF GUIDE-ASSISTED IMPLANT SURGERY
Guided implant surgery protocols are of two types: (1) static- and (2) dynamic-guided approach. The first system uses a surgical template, obtained from computerized tomographic images. However, the implant position cannot be altered intraoperatively. Using specially designed drilling machines, the implant location is usually transferred to the surgical template. The second approach uses virtual implant positioning from the computerized tomographic images and also provides a “real effect for positioning of implant intraoperatively.”[8,9]
TREATMENT PROTOCOL FOR COMPUTER-ASSISTED IMPLANT SURGERY
The treatment protocol for computer assisted implant surgery follows the fundamental steps:
Cone-beam computed tomography (CBCT) scanning
Software program execution
Fabrication of surgical drilling guides
Surgical procedure.
Step 1: Cone-beam computed tomography scanning
3D images are taken preoperatively via cone-beam computed tomography.[10] They offer low-dose and relatively less expensive imaging by giving easy applicability and justification for the presurgical implant placement.[11,12] It analyzes (1) available bone volume for implant placement, (2) mucosal thickness, (3) adjacent teeth structures, (4) maxillary sinus position, and (5) identifying the position of mandibular canal, incisive canal, and mental foramen.
Step 2: Software program execution
Software programs such as EasyGuide, Biohorizons, Nobel Biocare, InVivo5, and Simplant are available for planning and guided implant surgery. The 3D images are transformed into Digital Imaging and Communications in Medicine (DICOM) format. After reformatting the images, proper size of the implants is chosen at the site level of placing implant. This provides a virtual environment mimicking surgical procedure, exhibiting the coronal and apical location of the implant in an imported 3D image model of the jaw bone. This is performed in a transactional view to visualize cortical and trabecular bone. Other planes are also checked for ideal placing implants[7] [Figure 1].
Figure 1.
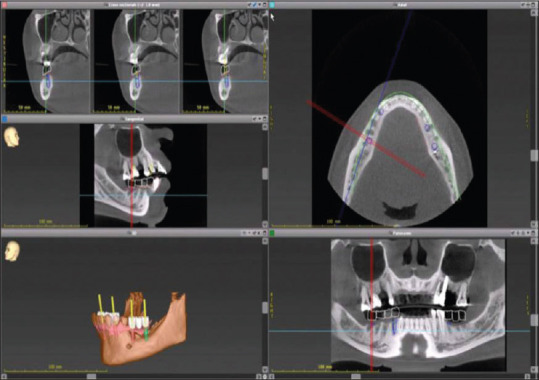
Preoperative scanning by cone beam computed tomography in order to provide cross sectional view
Step 3: Fabrication of surgical drilling guides
Upper and lower impressions are taken and bite is registered. Later, the impressions need to be articulated as the poured models on an articulator. The surgical guides are prepared manually or using computer-assisted methods after planning preoperatively.[7,13] It provides precise implant placement and speedy treatment time.
The steps needed to fabricate the surgical guide are as follows.
Guide supporting surfaces
The surgical guide designs are prepared on the type of supporting surfaces. They are (1) tooth-supported, (2) mucosa-supported, (3) bone-supported, and (4) special-supported surgical guides. In the first type, the remaining teeth are used for supporting the surgical guide. The second type uses mucosa as used in complete edentulous patients. The third type uses bone support after raising mucoperiosteal flap and has a higher chance of inaccuracy. The fourth type called special-supported guides uses mini implants or pins for supporting the surgical guide placement during implant surgery [Figure 2]. After planning the supporting tissues, the surgical guide can be fabricated through computer-assisted guidance.[7]
Figure 2.
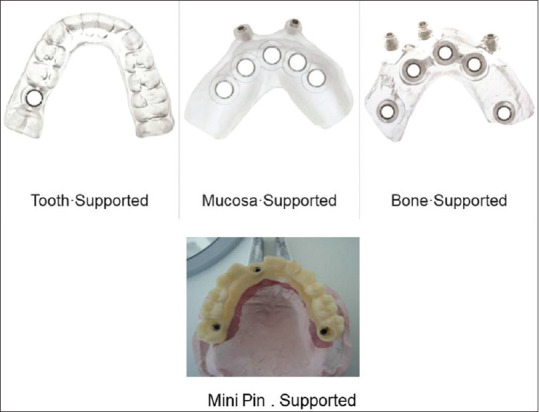
Types of guide supporting surfaces
Reverse treatment planning
Ideal prosthetic treatment plan has to be assessed initially in this digital planning. It is done using one-scan or double-scan procedures. The first procedure includes prosthesis in the patient's mouth using radiopaque resin. The second procedure as explained by the researcher at the University of Leuven is a double-step scanning.[7] Primary scanning includes the patient wearing the denture and secondary scanning allows only prosthesis imaging. Therefore, it explains digital imaging, both on the bone and prosthetic models. After the scanning process, according to individual system protocol, DICOM images are imported from software programs such as Simplant, Nobel guide, and EasyGuide. Then, the fusion of scan prosthesis and the surgical site with an optimal implant position are made by using fiducial markers such as gutta-percha, barium sulfate, and silicone index.[14] After planning, fabricating the surgical guides for enhanced surgical interpretation is to be analyzed. There are different companies such as keystone (EasyGuide), Compu Guide (Biohorizons), Anatomage, and SurgiGuide (Materialise) to fabricate surgical guides for universal implant system, except Nobel Biocare, for its own implant system.
Method of guide fabrication
It can be fabricated using model-based or rapid prototyping technique. Surgical templates using model-based guides are fabricated manually or using computerized technology by milling or laser printing. Preoperative planning for proper implant positioning and surgical guide sleeve placement is assessed. This model-based guide system provides soft and hard tissue assessment and predictable prosthetic outfit. The prepared sleeve bed is placed over the surgical site using the drilling arm. The main disadvantages of this surgical guide are the option of many manual steps needed to design.[7]
The other technique is stereolithographic or rapid prototyping technology. This provides digital-based data by intraoral scanning for guide preparation. The guides are fabricated by various implant providers using photopolymerization techniques.[15] This approach provides precision and the least manual steps.[16] In a dynamic navigation system, the surgical guides are used for placing implants, by viewing directly on the computerized screen.[11,17]
Design of surgical guide
The design of the surgical guides contains either metallic sleeves or without metallic sleeves [Figure 3]. The metal sleeves in the surgical guide require wider mesiodistal space and cause overheating of the bone during drilling due to inadequate saline irrigation into the surgical site. Lesser mesiodistal space can be achieved using customized sleeve design (without metallic sleeves either open or closed sleeves). In an open sleeve, a slot is located on the buccal or lingual side. This reduces the interarch space which minimizes bone heat by allowing the saline irrigation to fall on the drill directly. Advance in the digital effort will make the sleeve-designed surgical guide easier and less expensive using nonmetallic guiding tubes.[18,19] Still lack of evidence exists to compare the accuracy of newer and conventional templates.
Figure 3.
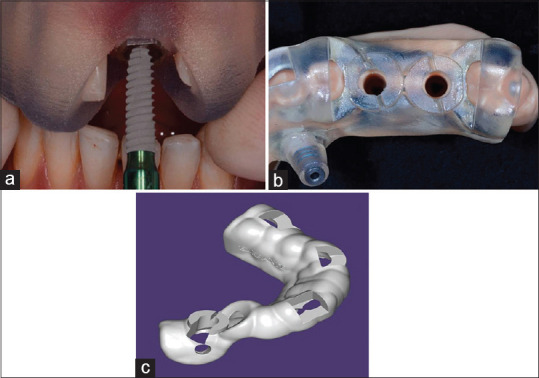
Design of sleeves in the surgical guide. (a) Metallic sleeve; (b) non-metallic sleeve; (c) customized open sleeve
Step 4: Surgical procedure
For static computer-assisted approach
Before procedure, the surgical guide is fitted in the mouth. It must be precisely adapted and stabilized to the soft tissues or teeth using an index [Figure 4]. A flap or flapless approach is followed. However, the second approach has many advantages with a lesser amount of bone loss, preserving the papilla, and improves esthetic effects after surgery.[20] The surgical procedure using this guide follows either fully or partially guided systems for implant placement. The first system is used commonly that includes osteotomy preparation with implant placement using surgical guides or templates. In the second system, only osteotomy preparation has been done using surgical templates and implants placed in a freehand manner. The findings of the 5th International Team for Implantology Consensus Conference concluded “that fully guided protocols performed more accurately compared with partially guided systems.”[7] Some systems require serial surgical guides to handle consecutive drill sequences or single surgical guide with different adjustable drills inserted during surgery.[21,22]
Figure 4.
Proper placement of stereolithographic guide using index in static-guided approach
For dynamic navigation approach
The dynamic navigation approach requires precise and continuous coordination of the patient, the image data, and the surgical instrumentation. The navigation system consists of stereovision with natural light cameras rather than infrared light-emitting diode. It uses either passive or active arrays of optical technologies.[17] The arrays use reflected light emitted from a light source, tracking to the stereo cameras for imaging the surgical procedure. The fiducial markers are used as an index for a surgical guide and implant placement. The surgical site is recorded using cameras, with arrays positioned extraorally. This allows stereo camera to control the real time movements of the drill and implant placement through patient 3D imaging.[23,24]
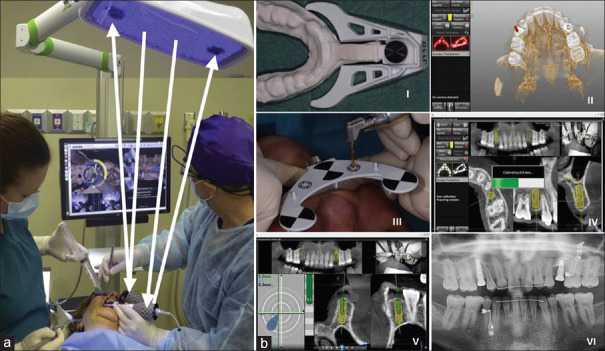
The main components of a dynamic navigation system include patient jaw attachment, handpiece attachment, and a system consisting of a camera, overhead-positioned emitting light, computer, and sensor.[23] During surgery, the surgical guide is attached. An open flap or flapless approach may follow depending on the thickness of keratinized tissue.[19] The conventional drilling sequence is used for osteotomy preparation.[23] Once the drilling bur accords with the planned implant position, the procedure is carried out and implant placed. The whole surgery involves direct vision on the computer screen, thereby controlling the direction and depth of implant placement.[25] This provides real motion tracking effect of the surgery [Figure 5]. The navigation systems commonly used are DenX Image Guided Implantology, X-Guide Dynamic 3D Navigation, Navident, and Inliant.[8]
Figure 5.
Dynamic navigation system. (a) Components: Patient jaw attachment, handpiece attachment and a system consisting of a camera, overhead blue emitting lights, computer and sensor; (b) ) Surgical procedure: I- Thermoplastic stent attaches with the remaining teeth in the arch using the radiographic marker; II-Digital planning; III and IV-Preoperative planning; V- Osteotomy drilling by viewing on the screen; VI- Postoperative image after implant placement
EXPECTED ADVANTAGEOUS OUTCOMES
The conventional implant placement approach uses either freehand surgery or laboratory-made surgical guide. Compared to static or navigation methods, freehand approach results in significant errors when placing implants.[23] More accuracy is evident at the apical and coronal position of implant when using computer-assisted static system by following its proper depth of placement. It results in a lesser deviation in crestal and apical position (<2 mm) and angulation inaccuracy (<5°).[26,27,28] On the other hand, the dynamic navigation approach has more advantages with its accuracy and speediness with the capability to adjust the location during surgery.[23,29,30,31] Compared with freehand approaches, it is a noninvasive approach causing lesser trauma and morbidity and helps to uphold better posture to the working surgeon.[23]
CONSIDERING THE REALITY
It is the choice of the clinician to decide which guided system to be used for implant placement. Still, many debates are argued based on these guided implant surgery protocols, but to know the reality, some facts to consider are as follows.
Using the static computer-assisted approach
The use of static computer-assisted system, using flapless approach in single/partially/fully edentulous cases, is very advantageous, which helps in replicating the precise implant position in the dental arch with successful immediate loading.[32,33] There are some challenges when placing these surgical guides in the restricted mouth opening or in the posterior regions due to its varying sizes of the drills.[23]
Accuracy
The accuracy of using the computer-assisted guides varies from clinician to clinician. It provides precision in 3D implant placements.[34] The pioneers in the conference concluded 'that highest inaccuracy using bone-supported surgical guides and highest accuracy using mini implants acting as a reference to support computerized tomography scan'. Comparing their precision placement in the maxilla and mandible, both exhibit an equal level of accuracy and errors. However, few studies reported significant differences between maxillary and mandibular accuracy.[9] For example, Pettersson et al.[28] found higher error of deviation in the mandible compared to the maxilla. However, Ozan et al.[35] stated that mandible has better accuracy with significant results than the maxilla. Based on different materials for manufacturing surgical guide, better accuracy is evident using computer assisted manufacture (CAM) guide than the lab made guides.[9] There is still a lack of evidence to support manufacturing material for the guide.
Errors
Chance of implant deviations may occur as an error, during planning or surgical procedures. Cassetta et al.[36] noted minimal deviation at the coronal and apical part of implant and slight change in angulation of implant. Arisan et al.[37] in their study observed the mean deviation of 0.6–1.5 mm and 0.6–1.27 mm at the apex and the shoulder level of implants, placed using tooth- or mucosa-supported guides. In the meta-analysis, Tahmaseb et al.[15] found significant differences comparing freehand surgical placement of implants with mucosa- or bone-supported surgical guides in complete edentulous patient. The freehand method showed error of 2.7 mm and 2.9 mm linear deviance in coronal and apical position and 9.9° of angular deviance. Whereas, using surgical guides, the deviance of 1.4 mm and 1.6 mm noted at the coronal and apical portion of implants and range of 3.0°–8.86° angular deviance noted. However, Di Giacomo et al.[38] suggested that the improper support and stability of the surgical guide during implant placement might lead to errors. Thus, proper planning and positioning needed for making flawless procedures using surgical guides.
Flapless approach
A flapless approach is commonly used in guided implant procedures. It helps in situations having an adequate keratinized tissue thickness or implant site adjacent to the anatomic structures, i.e., mandibular nerve, maxillary sinus, and mental foramen.[15,19] According to Hahn,[39] the success rate for this approach is similar to the conventional procedures. In 2007, Nickenig and Eitner[40] had validated the reliability of static assisted computer guidance with the use of a flapless approach, provided the precise and speedy treatment. A major drawback of this approach is the lack of access and gauging the surgical bone area. Even perforation through the crest and on the crest can occur accidentally leading to implant failure.[41]
Immediate loading and guided surgical approach
Immediate loading with interim prosthesis can be followed after guided implant placement.[42] Meloni et al.[43] observed immediate loading using computer-assisted guidance and instant restoration with computer-aided design-CAM technology offers predictable option for managing fully edentulous cases.
Implant survival
Schneider et al.[44] in their systematic review suggested that inclusive of studies with 1–5 year follow up reported 91% to 100% survival rates of implant is attained through computer assisted template based approach. Similar implant survival rates are reported by Vasak et al.[45] in their 1-year prospective study and Rocci et al.[46] in their 3-year retrospective study. From their review, the success of survival rate is observed after prosthetic loading with the bone loss of about 1.5 mm using static-guided system.
Using dynamic-assisted approach
Dynamic approach has become easier in complex cases such as challenging bone topography and critical anatomic situation. Wittwer et al.[47] using this approach pointed accuracy, safer, and immediate implant placement in smooth and wide bone areas. However, Vercruyssen et al.[48] pointed out that the sleeves in the guide for the dynamic approach have rigidity and control the drilling in irregular bone areas. This approach even seeks treatment faster and better in patients with physical and psychological problems.
Accuracy
The navigation system exhibits a greater accuracy at the coronal and apical portion of the implants. It shows precision between planned and finally placed implant during the procedure.[49]
Errors
Using a dynamic approach, few studies have indicated a negligible error with a linear deviation of 0.4 mm and 4° angular deviances in the final implant.[29,30,31,50] Thus, dynamic approach is considered to be highly accurate having a mean error of 0.35 mm.[31,51]
Implant success
In a systematic review, Jung et al.[8] described that the success rate was the same when compared with conventional implant surgery. Still, very few studies are existing using this approach. Further longitudinal studies are needed in using the dynamic navigation system.
Comparing static- versus dynamic-assisted approach
The static-assisted implant placement is commonly used in fully edentulous patient, whereas navigation approach is used in cases of limited mouth opening or inaccessible posterior region of the jaw. The main advantage on using the dynamic approach is that it allows the real effect of osteotomy sequential drilling and implant placement, using shorter surgical instruments without viewing the mouth of the patient rather viewing on the screen. The surgical guide requires an adequate gap between the implants, mucosa, and adjacent teeth to provide accuracy.[23,52] Computer-assisted guidance allowed an error of <2 mm linear deviation and angular deviance <5°, when compared with a laboratory-made acrylic guide.[53] On comparing static and dynamic guided approach, studies done by Kaewsiri et al.[54] and Mischkowski et al.[55] explained dynamic navigation, provided higher accuracy than the static guide system.
In reality, dynamic navigation approach exerts work in an easy manner like scanning the surgical site, planning it preoperatively, and finally placing implant within a shorter time and on single visit, by directly monitoring the screen. However, it is very costly to invest when comparing computer-assisted static system for perfect implant placement. Finally, navigation system at present found to have various difficulties to practice in a daily scenario.[7] Block et al.[23] noticed for navigation surgery, a team approaches are needed to learn the work together and for easy use.
Literature search reveals promising outcomes for computer-assisted, static- or dynamic navigation-guided implant placements by considering the included studies [Table 1]. Many queries related to the outcomes for guided surgical protocol are solved in our literature using the systematic review [Table 2]. No meta-analysis is still present. Thus, computer-guided approach is considered to offer more predictable, safer, and faster implant placement with the predetermined final prosthetic outfit.
Table 1.
Literature search for assessing the outcomes by computer-guided static system or dynamic navigation system for implant placement
| Author(s) | Study design | Type of guided surgery | System | Dentition | Guide supporting tissues | Type of jaw | Open flap/flapless surgery | Outcomes |
|---|---|---|---|---|---|---|---|---|
| Brief et al. 2005[50] | In vitro phantom model | Dynamic | RoboDent system, DenX Image Guided Implantology | Partially edentulous | NA | Mandibles | NA | High accuracy |
| Di Giacomo et al. 2005[21] | Clinical trial | Static | Simplant | Partially edentulous | Bone/tooth | Both | Open flap | Mild angular and linear deviations |
| Kramer et al. 2005[30] | Invitro cast model | Dynamic | DenX Image Guided Implantology | Partially edentulous | NA | Maxilla | NA | High accuracy |
| van Steenberghe et al. 2005[18] | Prospective | Static | Nobel Biocare | Fully edentulous | Mucosa | Maxillae | Flapless | Faster implant placement Stable |
| Chiu et al. 2006[29] | Invitro Model | Dynamic | CAN system | Na | NA | Mandible | NA | Mild angular and linear deviations Mandibular canal perforation occurs rarely |
| Mischkowski et al. 2006[55] | In vivo | Static versus dynamic | Med3D, coDiagnostix/gonyX, SimPlant, RoboDent and VectorVision2 | Both | NR | NR | NR | High accuracy Slight complication rate evident in dynamic system |
| Nickenig and Eitner 2007[40] | In vivo | Static | coDiagnostiX | Partially edentulous | Tooth | Mandible | Flapless | No complications |
| Wittwer et al. 2007[47] | Pilot study | Dynamic | VISIT navigation system | Fully edentulous | Mucosa | Mandible | Flapless | Precise, predictable, safe procedure |
| Elian et al. 2008[49] | Case series | Dynamic | DenX Image Guided Implantology | Partially edentulous | Mucosa | Both | Flapless | Mild angular and linear deviations |
| Komiyama et al. 2008[32] | Prospective | Static | Nobel Guide | Fully edentulous | Mucosa | Both | Flapless | Successful immediate loading Stable Minimal complication |
| Tahmaseb et al. 2009[22] | Case report | Static | Exe–plan | Fully edentulous | Mini-implants | Both | Flapless | High accuracy |
| Arisan et al. 2010[37] | In vivo | Static | Three software: Stent CAD, Media Lab, Simplant | Both | Both | All supporting tissues | open flap | Bone supported guides had the highest deviations. no surgical complications |
| Meloni et al. 2010[43] | Prospective | Static | Nobel Biocare | Fully edentulous | mucosa | maxilla | Flapless | Successful immediate provisional done Improves the survival rate |
| Ozan et al. (2011)[35] | Clinical study | Static | Stent Cad | Fully edentulous | Mucosa/pin | Both | Flapless/open flap | Higher angular deviation in lower bone density |
| Cassetta et al. (2012)[36] | In vivo | Static | Simplant | Both | Mixed | Both | Open flap | mild angular and linear deviations |
| Di Giacomo et al. (2012)[38] | In vivo | Static | Implant Viewer | Fully edentulous | Mucosa + pin | Both | Open flap | Mild linear deviations. Complications may present |
| Platzer et al. (2013)[34] | Pilot study | Static | Simplant | Partial edentulous | Tooth | Both | Flapless | Successful immediate provisional placed High accuracy |
| Beretta et al. (2014)[27] | In vivo | Static- Flapless Surgery | 3D diagnosis | Both | Mixed | Both | Flapless | Mild angular and linear deviations |
| Pettersson et al. (2014)[28] | In vitro models | Static | Nobel Biocare | NR | NA | Maxilla | NA | mild deviation regarding implant position, angle, depth and apex |
| Vasak et al. (2014)[45] | Prospective | Static | Nobel Guide | Both | Mucosa/tooth or both | Both | Flapless | Higher success rate |
| Vercruyssen et al. (2014)[48] | Randomized controlled trial | Static | Simplant | Fully edentulous | Mucosa or bone supported | Both | Flapless/open flap | Higher success rate |
| Zhao et al. (2014)[26] | Prospective | Static | Simplant | Partially edentulous | Mucosa/ tooth | Both | NR | Mild angular and linear deviations in mucosa supported guides |
| Geng et al. (2015)[16] | Prospective | Static | Simplant | Both | Mucosa/tooth | Both | Flapless | High accuracy in tooth supported guide |
| Somogyi-Ganss et al. (2015)[53] | In vitro models | Static versus dynamic | Simplant, Nobel Biocare Navident | Nr | NA | Both | NA | Both showed better outcomes except mild angular and linear deviations |
| Emery et al. (2016)[51] | In vitro model | Dynamic | X-Guide Dynamic 3D Navigation | Both | NR | Both | NA | High accuracy |
| Naziri et al. (2016)[33] | Clinical trial | Static | CoDiagnostiX | Partially edentulous | Pin+tooth | Both | Open flap | High accuracy |
| Block et al. (2017)[52] | In vivo | Dynamic | X-Guide Dynamic 3D Navigation | Partially edentulous | NR | Both | Flapless | High accuracy |
| Kaewsiri et al. (2019)[54] | Randomized controlled trial | Static versus dynamic | coDiagnostiX Iris–100 | Single tooth space | Tooth | Both | Flapless/open flap | High accuracy using dynamic navigation |
| Pellegrino et al. (2019)[56] | In vivo | Dynamic | ImplaNav | Single tooth-premolar | NR | Maxilla | Flapless | High accuracy |
| Tallarico et al. (2019)[19] | Clinical trial | Static | Exocad DentalCAD | Partially edentulous | Tooth | Both | Flapless/open flap | High accuracy |
NR – Not reported; NA – Not applicable; CAN – Computer-assisted navigation
Table 2.
Systematic review for analyzing the outcomes by computer-guided static system or dynamic navigation system for implant placement
| Study | Number of studies | Studies met our inclusion criteria | Type of guided surgery | Outcomes | |||||
|---|---|---|---|---|---|---|---|---|---|
| Accuracy (error mm) | Failure rate (after 12 months survival) (%) | Complication rates (surgical and prosthetic complications) (%) | |||||||
| Entry point | Apex | ||||||||
| Minimum | Maximum | Minimum | Maximum | ||||||
| Schneider et al. (2009)[44] | 18 | 2 | Static | 1.07 | - | 1.63 | - | - | 13.3 |
| Jung et al. (2009)[8] | 32 | 5 | Static and dynamic navigation | 0.74 | 4.5 | 0.85 | 7.1 | 3.36 | 4.6 |
| Tahmaseb et al. (2014)[9] | 38 | 10 | Static | 1.12 | 4.5 | 1.39 | 7.1 | 2.7 | 36.4 |
| Tahmaseb et al. (2018)[15] | 20 | 8 | Static | 1.2 | - | 1.4 | - | - | - |
- – Not mentioned
ANALYZING THE EXPENSES AND DURATION OF LEARNING
Dynamic navigation approach is very expensive and costs about more than 50 lakhs, whereas static-assisted computer design is less expensive and costs twenty thousand, which is easy to fabricate and can avoid the expensive hardware needed for the dynamic approach.[57,58] The learning curve for this dynamic approach is found to be challenging for clinicians initially. Ewers et al.[59] based on their clinical experience revealed that handling of the software for the dynamic approach is quite easy and needs short time to learn. Thus, it depends on the clinician's skill to use it efficiently.
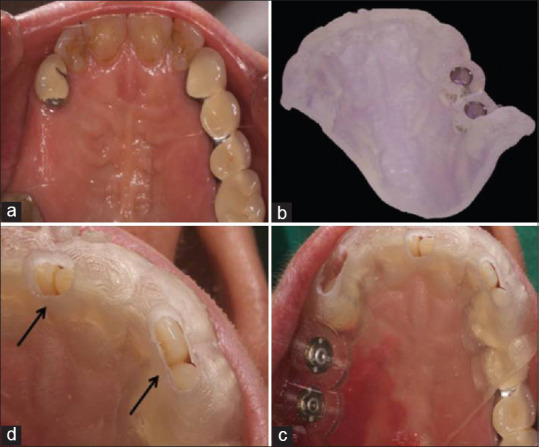
COMPLICATIONS
The complications encountered during guided implant surgery include surgical and prosthetic complications. It also includes early or late complications. The surgical complications may have a broken intraoperative surgical guide, [Figure 6] lead to altered surgical plan or absence of primary stability with early implant loss or prosthetic fracture, or may even cause nerve disturbances by damaging anatomically vital structures.[8,44] The prosthetic complications such as a misfit of the prosthesis and screw loosening could happen. Schneider et al.[44] explained several failures or complications that might encounter during or after guided surgery [Table 3]. Tahmaseb et al.[15] explained using the static computer-guided approach; the surgical and prosthetic complications occurred at the average rate of 13.3%. Fewer complications using a dynamic approach may include impingement of implant on an inferior alveolar nerve or adjacent tooth roots rarely.[60]
Figure 6.

Fracture of surgical guide during the procedure
Table 3.
List of complications/failures may encounter using computer-assisted implant placement
| Early surgical complication/failures[44] |
| Limited access |
| Fracture of template |
| Unpredicted bony dehiscence |
| Infection |
| Difficulties when bone augmentation needed |
| Insertion of wider, narrower or shorter implant than planned |
| Lack of implant stability |
| Soft tissue deficiency |
| Fistula |
| Pain |
| Early prosthetic complication/failures[44] |
| Misfit or loosening of prosthesis |
| Occlusal problem |
| Difficulties in speech |
| Cheek biting |
| Late prosthetic complication/failures[44] |
| Loosening of screw |
| Fracture or misfit of prosthesis |
| Occlusal wear |
| Esthetic unhappiness |
NEW DEVELOPMENTS
Newer technological advancements are made in software and hardware to improve its data acquisition and processing. Newer software may have a synergistic update of intraoral scanning; providing both complete solid 3D representations of soft and hard tissues. In future, guide fabrication through 3D-printing technologies will be providing more accuracy and rapidity. Novel software such as digital wax-up for the future prosthesis helps in improvement or correction if required. Digital impression can be applied for improving the accuracy of implant placement and final prosthetic loading. Nowadays, sand-blasted large grit-acid technology for guide approach paves the way for accuracy and its related treatment.[7,61,62] The augmented procedures for implant placement seem to use dynamic navigation systems without affecting the accuracy. However, further technology seems to improve specific software applications to optimize the results.[56]
CONCLUSION
Guided implant surgery provides precise, effective, and efficient implant placement compared to freehand implant surgery without damaging the critical anatomic dental structures. The major advantage of the dynamic design is the ability to intraoperatively adjust the planned implant positioning.
However, the deviation between virtual implant planning and real implant position occurs due to the surgical learning curve and the accumulated errors that may occur throughout the multiple steps of the digital workflow. The reliability of computer-guided surgery does not justify a blind execution. The learning curve is undeniable and even a clinician with basic surgical skills, including conventional implant dentistry, will be in a better position to address any unforeseen complication.
Despite inconsistent outcomes when compared to traditional surgery, computer-assisted surgery still retains the superiority in terms of proper implant positioning and taking into concern the prosthetic outcomes and survival rate using surgical guides.
Still, a long term study is needed to support the successful criteria using guide based implant placement. Nevertheless, in future, these outcomes can be far beneficial and effective in using newer developed software and hardware identities, leading to successful implant placement and excellent prosthetic outfit in dentistry.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
The authors wish to thank Dr. Sumathi. K. Sripathi, Senior Lecturer, DMI St. Eugene University, IVDL, Lusaka, Zambia, Africa, for her endless guidance to support this work.
REFERENCES
- 1.Buser D, Bornstein MM, Weber HP, Grütter L, Schmid B, Belser UC. Early implant placement with simultaneous guided bone regeneration following single-tooth extraction in the esthetic zone: A cross-sectional, retrospective study in 45 subjects with a 2- to 4-year follow-up. J Periodontol. 2008;79:1773–81. doi: 10.1902/jop.2008.080071. [DOI] [PubMed] [Google Scholar]
- 2.Akça K, Iplikçioǧlu H, Cehreli MC. A surgical guide for accurate mesiodistal paralleling of implants in the posterior edentulous mandible. J Prosthet Dent. 2002;87:233–5. doi: 10.1067/mpr.2002.120900. [DOI] [PubMed] [Google Scholar]
- 3.The glossary of prosthodontic terms. J Prosthet Dent. 2005;94:10–92. doi: 10.1016/j.prosdent.2005.03.013. [DOI] [PubMed] [Google Scholar]
- 4.Dyer PV, Patel N, Pell GM, Cummins B, Sandeman DR. The ISG viewing wand: An application to atlanto-axial cervical surgery using the Le Fort I maxillary osteotomy. Br J Oral Maxillofac Surg. 1995;33:370–4. doi: 10.1016/0266-4356(95)90138-8. [DOI] [PubMed] [Google Scholar]
- 5.Solomon W. The viewing wand--its introduction and uses. Br J Theatre Nurs. 1996;6:11–4. [PubMed] [Google Scholar]
- 6.Schlenzka D, Laine T, Lund T. Computer-assisted spine surgery. Eur Spine J. 2000;1:57–64. doi: 10.1007/PL00010023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.D'haese J, Ackhurst J, Wismeijer D, De Bruyn H, Tahmaseb A. Current state of the art of computer-guided implant surgery. Periodontol. 2000;2017(73):121–33. doi: 10.1111/prd.12175. [DOI] [PubMed] [Google Scholar]
- 8.Jung RE, Schneider D, Ganeles J, Wismeijer D, Zwahlen M, Hämmerle CH, et al. Computer technology applications in surgical implant dentistry: A systematic review. Int J Oral Maxillofac Implants. 2009;24:92–109. [PubMed] [Google Scholar]
- 9.Tahmaseb A, Wismeijer D, Coucke W, Derksen W. Computer technology applications in surgical implant dentistry: A systematic review. Int J Oral Maxillofac Implants. 2014;29:25–42. doi: 10.11607/jomi.2014suppl.g1.2. [DOI] [PubMed] [Google Scholar]
- 10.BouSerhal C, Jacobs R, Quirynen M, van Steenberghe D. Imaging technique selection for the preoperative planning of oral implants: A review of the literature. Clin Implant Dent Relat Res. 2002;4:156–72. doi: 10.1111/j.1708-8208.2002.tb00167.x. [DOI] [PubMed] [Google Scholar]
- 11.Vercruyssen M, Fortin T, Widmann G, Jacobs R, Quirynen M. Different techniques of static/dynamic guided implant surgery: Modalities and indications. Periodontol. 2000;2014(66):214–27. doi: 10.1111/prd.12056. [DOI] [PubMed] [Google Scholar]
- 12.Jacobs R, Quirynen M. Dental cone beam computed tomography: Justification for use in planning oral implant placement. Periodontol. 2000;2014(66):203–13. doi: 10.1111/prd.12051. [DOI] [PubMed] [Google Scholar]
- 13.Johansson B, Friberg B, Nilson H. Digitally planned, immediately loaded dental implants with prefabricated prostheses in the reconstruction of edentulous maxillae: A 1-year prospective, multicenter study. Clin Implant Dent Relat Res. 2009;11:194–200. doi: 10.1111/j.1708-8208.2008.00111.x. [DOI] [PubMed] [Google Scholar]
- 14.Abboud M, Orentlicher G. An open system approach for surgical guide production. J Oral Maxillofac Surg. 2011;69:e519–24. doi: 10.1016/j.joms.2011.07.027. [DOI] [PubMed] [Google Scholar]
- 15.Tahmaseb A, Wu V, Wismeijer D, Coucke W, Evans C. The accuracy of static computer-aided implant surgery: A systematic review and meta-analysis. Clin Oral Implants Res. 2018;29(Suppl 16):416–35. doi: 10.1111/clr.13346. [DOI] [PubMed] [Google Scholar]
- 16.Geng W, Liu C, Su Y, Li J, Zhou Y. Accuracy of different types of computer-aided design/computer-aided manufacturing surgical guides for dental implant placement. Int J Clin Exp Med. 2015;8:8442–9. [PMC free article] [PubMed] [Google Scholar]
- 17.Mezger U, Jendrewski C, Bartels M. Navigation in surgery. Langenbecks Arch Surg. 2013;398:501–14. doi: 10.1007/s00423-013-1059-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.van Steenberghe D, Glauser R, Blombäck U, Andersson M, Schutyser F, Pettersson A, et al. A computed tomographic scan-derived customized surgical template and fixed prosthesis for flapless surgery and immediate loading of implants in fully edentulous maxillae: A prospective multicenter study. Clin Implant Dent Relat Res. 2005;7(Suppl 1):S111–20. doi: 10.1111/j.1708-8208.2005.tb00083.x. [DOI] [PubMed] [Google Scholar]
- 19.Tallarico M, Martinolli M, Kim Y, Cocchi F, Meloni SM, Alushi A, et al. Accuracy of computer-assisted template-based implant placement using two different surgical templates designed with or without metallic sleeves: A randomized controlled trial. Dent J (Basel) 2019;7:41–55. doi: 10.3390/dj7020041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Becker W, Goldstein M, Becker BE, Sennerby L. Minimally invasive flapless implant surgery: A prospective multicenter study. Clin Implant Dent Relat Res. 2005;7(Suppl 1):S21–7. doi: 10.1111/j.1708-8208.2005.tb00071.x. [DOI] [PubMed] [Google Scholar]
- 21.Di Giacomo GA, Cury PR, de Araujo NS, Sendyk WR, Sendyk CL. Clinical application of stereolithographic surgical guides for implant placement: Preliminary results. J Periodontol. 2005;76:503–7. doi: 10.1902/jop.2005.76.4.503. [DOI] [PubMed] [Google Scholar]
- 22.Tahmaseb A, De Clerck R, Wismeijer D. Computer-guided implant placement: 3D planning software, fixed intraoral reference points, and CAD/CAM technology. A case report. Int J Oral Maxillofac Implants. 2009;24:541–6. [PubMed] [Google Scholar]
- 23.Block MS, Emery RW. Static or dynamic navigation for implant placement-choosing the method of guidance. J Oral Maxillofac Surg. 2016;74:269–77. doi: 10.1016/j.joms.2015.09.022. [DOI] [PubMed] [Google Scholar]
- 24.Nijmeh AD, Goodger NM, Hawkes D, Edwards PJ, McGurk M. Image-guided navigation in oral and maxillofacial surgery. Br J Oral Maxillofac Surg. 2005;43:294–302. doi: 10.1016/j.bjoms.2004.11.018. [DOI] [PubMed] [Google Scholar]
- 25.Watzinger F, Birkfellner W, Wanschitz F, Millesi W, Schopper C, Sinko K, et al. Positioning of dental implants using computer-aided navigation and an optical tracking system: Case report and presentation of a new method. J Craniomaxillofac Surg. 1999;27:77–81. doi: 10.1016/s1010-5182(99)80017-1. [DOI] [PubMed] [Google Scholar]
- 26.Zhao XZ, Xu WH, Tang ZH, Wu MJ, Zhu J, Chen S. Accuracy of computer-guided implant surgery by a CAD/CAM and laser scanning technique. Chin J Dent Res. 2014;17:31–6. [PubMed] [Google Scholar]
- 27.Beretta M, Poli PP, Maiorana C. Accuracy of computer-aided template-guided oral implant placement: A prospective clinical study. J Periodontal Implant Sci. 2014;44:184–93. doi: 10.5051/jpis.2014.44.4.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pettersson A, Kero T, Söderberg R, Näsström K. Accuracy of virtually planned and CAD/CAM-guided implant surgery on plastic models. J Prosthet Dent. 2014;112:1472–8. doi: 10.1016/j.prosdent.2014.01.029. [DOI] [PubMed] [Google Scholar]
- 29.Chiu WK, Luk WK, Cheung LK. Three-dimensional accuracy of implant placement in a computer-assisted navigation system. Int J Oral Maxillofac Implants. 2006;21:465–70. [PubMed] [Google Scholar]
- 30.Kramer FJ, Baethge C, Swennen G, Rosahl S. Navigated vs. conventional implant insertion for maxillary single tooth replacement. Clin Oral Implants Res. 2005;16:60–8. doi: 10.1111/j.1600-0501.2004.01058.x. [DOI] [PubMed] [Google Scholar]
- 31.Casap N, Wexler A, Persky N, Schneider A, Lustmann J. Navigation surgery for dental implants: Assessment of accuracy of the image guided implantology system. J Oral Maxillofac Surg. 2004;62:116–9. doi: 10.1016/j.joms.2004.06.028. [DOI] [PubMed] [Google Scholar]
- 32.Komiyama A, Klinge B, Hultin M. Treatment outcome of immediately loaded implants installed in edentulous jaws following computer-assisted virtual treatment planning and flapless surgery. Clin Oral Implants Res. 2008;19:677–85. doi: 10.1111/j.1600-0501.2008.01538.x. [DOI] [PubMed] [Google Scholar]
- 33.Naziri E, Schramm A, Wilde F. Accuracy of computer-assisted implant placement with insertion templates. GMS Interdiscip Plast Reconstr Surg DGPW. 2016;5:1–6. doi: 10.3205/iprs000094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Platzer S, Bertha G, Heschl A, Wegscheider WA, Lorenzoni M. Three-dimensional accuracy of guided implant placement: Indirect assessment of clinical outcomes. Clin Implant Dent Relat Res. 2013;15:724–34. doi: 10.1111/j.1708-8208.2011.00406.x. [DOI] [PubMed] [Google Scholar]
- 35.Ozan O, Orhan K, Turkyilmaz I. Correlation between bone density and angular deviation of implants placed using CT-generated surgical guides. J Craniofac Surg. 2011;22:1755–61. doi: 10.1097/SCS.0b013e31822e6305. [DOI] [PubMed] [Google Scholar]
- 36.Cassetta M, Stefanelli LV, Giansanti M, Calasso S. Accuracy of implant placement with a stereolithographic surgical template. Int J Oral Maxillofac Implants. 2012;27:655–63. [PubMed] [Google Scholar]
- 37.Arisan V, Karabuda ZC, Ozdemir T. Accuracy of two stereolithographic guide systems for computer-aided implant placement: A computed tomography-based clinical comparative study. J Periodontol. 2010;81:43–51. doi: 10.1902/jop.2009.090348. [DOI] [PubMed] [Google Scholar]
- 38.Di Giacomo GA, da Silva JV, da Silva AM, Paschoal GH, Cury PR, Szarf G. Accuracy and complications of computer-designed selective laser sintering surgical guides for flapless dental implant placement and immediate definitive prosthesis installation. J Periodontol. 2012;83:410–9. doi: 10.1902/jop.2011.110115. [DOI] [PubMed] [Google Scholar]
- 39.Hahn J. Single-stage, immediate loading, and flapless surgery. J Oral Implantol. 2000;26:193–8. doi: 10.1563/1548-1336(2000)026<0193:SILAFS>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 40.Nickenig HJ, Eitner S. Reliability of implant placement after virtual planning of implant positions using cone beam CT data and surgical (guide) templates. J Craniomaxillofac Surg. 2007;35:207–11. doi: 10.1016/j.jcms.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 41.Sunitha RV, Sapthagiri E. Flapless implant surgery: A 2-year follow-up study of 40 implants. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;116:e237–43. doi: 10.1016/j.oooo.2011.12.027. [DOI] [PubMed] [Google Scholar]
- 42.Li W, Chow J, Hui E, Lee PK, Chow R. Retrospective study on immediate functional loading of edentulous maxillas and mandibles with 690 implants, up to 71 months of follow-up. J Oral Maxillofac Surg. 2009;67:2653–62. doi: 10.1016/j.joms.2009.07.015. [DOI] [PubMed] [Google Scholar]
- 43.Meloni SM, De Riu G, Pisano M, Cattina G, Tullio A. Implant treatment software planning and guided flapless surgery with immediate provisional prosthesis delivery in the fully edentulous maxilla. A retrospective analysis of 15 consecutively treated patients. Eur J Oral Implantol. 2010;3:245–51. [PubMed] [Google Scholar]
- 44.Schneider D, Marquardt P, Zwahlen M, Jung RE. A systematic review on the accuracy and the clinical outcome of computer-guided template-based implant dentistry. Clin Oral Implants Res. 2009;20(Suppl 4):73–86. doi: 10.1111/j.1600-0501.2009.01788.x. [DOI] [PubMed] [Google Scholar]
- 45.Vasak C, Kohal RJ, Lettner S, Rohner D, Zechner W. Clinical and radiological evaluation of a template-guided (NobelGuide™) treatment concept. Clin Oral Implants Res. 2014;25:116–23. doi: 10.1111/clr.12038. [DOI] [PubMed] [Google Scholar]
- 46.Rocci A, Martignoni M, Gottlow J. Immediate loading in the maxilla using flapless surgery, implants placed in pre-determined positions, and prefabricated provisional restorations: A retrospective 3-year clinical study. Clin Implant Dent Relat Res. 2003;5:29–36. doi: 10.1111/j.1708-8208.2003.tb00013.x. [DOI] [PubMed] [Google Scholar]
- 47.Wittwer G, Adeyemo WL, Schicho K, Figl M, Enislidis G. Navigated flapless transmucosal implant placement in the mandible: A pilot study in 20 patients. Int J Oral Maxillofac Implants. 2007;22:801–7. [PubMed] [Google Scholar]
- 48.Vercruyssen M, van de Wiele G, Teughels W, Naert I, Jacobs R, Quirynen M. Implant- and patient-centred outcomes of guided surgery, a 1-year follow-up: An RCT comparing guided surgery with conventional implant placement. J Clin Periodontol. 2014;41:1154–60. doi: 10.1111/jcpe.12305. [DOI] [PubMed] [Google Scholar]
- 49.Elian N, Jalbout ZN, Classi AJ, Wexler A, Sarment D, Tarnow DP. Precision of flapless implant placement using real-time surgical navigation: A case series. Int J Oral Maxillofac Implants. 2008;23:1123–7. [PubMed] [Google Scholar]
- 50.Brief J, Edinger D, Hassfeld S, Eggers G. Accuracy of image-guided implantology. Clin Oral Implants Res. 2005;16:495–501. doi: 10.1111/j.1600-0501.2005.01133.x. [DOI] [PubMed] [Google Scholar]
- 51.Emery RW, Merritt SA, Lank K, Gibbs JD. Accuracy of dynamic navigation for dental implant placement-model-based evaluation. J Oral Implantol. 2016;42:399–405. doi: 10.1563/aaid-joi-D-16-00025. [DOI] [PubMed] [Google Scholar]
- 52.Block MS, Emery RW, Lank K, Ryan J. Implant placement accuracy using dynamic navigation. Int J Oral Maxillofac Implants. 2017;32:92–9. doi: 10.11607/jomi.5004. [DOI] [PubMed] [Google Scholar]
- 53.Somogyi-Ganss E, Holmes HI, Jokstad A. Accuracy of a novel prototype dynamic computer-assisted surgery system. Clin Oral Implants Res. 2015;26:882–90. doi: 10.1111/clr.12414. [DOI] [PubMed] [Google Scholar]
- 54.Kaewsiri D, Panmekiate S, Subbalekha K, Mattheos N, Pimkhaokham A. The accuracy of static vs. dynamic computer-assisted implant surgery in single tooth space: A randomized controlled trial. Clin Oral Implants Res. 2019;30:505–14. doi: 10.1111/clr.13435. [DOI] [PubMed] [Google Scholar]
- 55.Mischkowski RA, Zinser MJ, Neugebauer J, Kübler AC, Zöller JE. Comparison of static and dynamic computer-assisted guidance methods in implantology. Int J Comput Dent. 2006;9:23–35. [PubMed] [Google Scholar]
- 56.Pellegrino G, Mangano C, Mangano R, Ferri A, Taraschi V, Marchetti C. Augmented reality for dental implantology: A pilot clinical report of two cases. BMC Oral Health. 2019;19:158. doi: 10.1186/s12903-019-0853-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gulati M, Anand V, Salaria SK, Jain N, Gupta S. Computerized implant-dentistry: Advances toward automation. J Indian Soc Periodontol. 2015;19:5–10. doi: 10.4103/0972-124X.145781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Varun Menon P. Navigation in implant dentistry. EC Dent Sci. 2017;14:167–71. [Google Scholar]
- 59.Ewers R, Schicho K, Truppe M, Seemann R, Reichwein A, Figl M, et al. Computer-aided navigation in dental implantology: 7 years of clinical experience. J Oral Maxillofac Surg. 2004;62:329–34. doi: 10.1016/j.joms.2003.08.017. [DOI] [PubMed] [Google Scholar]
- 60.Block MS, Emery RW, Cullum DR, Sheikh A. Implant Placement Is More Accurate Using Dynamic Navigation. J Oral Maxillofac Surg. 2017;75:1377–86. doi: 10.1016/j.joms.2017.02.026. [DOI] [PubMed] [Google Scholar]
- 61.Marsango V, Bollero R, D'Ovidio N, Miranda M, Bollero P, Barlattani A., Jr Digital work-flow. Oral Implantol (Rome) 2014;7:20–4. [PMC free article] [PubMed] [Google Scholar]
- 62.Mora MA, Chenin DL, Arce RM. Software tools and surgical guides in dental-implant-guided surgery. Dent Clin North Am. 2014;58:597–626. doi: 10.1016/j.cden.2014.04.001. [DOI] [PubMed] [Google Scholar]