Abstract
People with disabilities constitute a marginalized population who experience significant health care disparities resulting from structural, socioeconomic, and attitudinal barriers to accessing health care. It has been reported that education on the care of marginalized groups helps to improve awareness, patient–provider rapport, and patient satisfaction. Yet, emergency medicine (EM) residency education on care for people with disabilities may be lacking. The goal of this paper is to review the current state of health care for patients with disabilities, review the current state of undergraduate and graduate medical education on the care of patients with disabilities, and provide suggestions for an improved EM residency curriculum that includes education on the care for patients with disabilities.
In the United States, disability is common, affecting approximately 61 million people or one in four (26%) people. 1 Yet according to a report by the Office of the Surgeon General in 2005, the U.S. health care system is insufficiently prepared to recognize and address the needs of people with disabilities. 2 The causes of this are multifactorial, but one critical factor is a lack of structured, specific, and consistent training on caring for patients with disabilities in medical school and residency. 3
Call to Action
We are an interested group of EM physicians, residents, and medical students with a passion for education on caring for patients with disabilities. Collectively, we have experience and expertise in designing curriculum regarding diversity and inclusion, specifically including disability, as well as personal life experiences with adversity and disabilities. As members of the Accommodations Committee of the Academy for Diversity and Inclusion in Emergency Medicine (ADIEM), a subgroup of the Society for Academic Emergency Medicine (SAEM), we are dedicated to addressing the challenge of insufficient graduate medical education on caring for patients with disabilities in the emergency department (ED) and advocate for EM residency curricular reform to ameliorate the provider knowledge gaps that can perpetuate barriers to equitable care for this group.
Current State of Health Care for Individuals with Disabilities
People with disabilities are a diverse group with a wide variety of impairments or challenges and, thus, a variety of needs. The visibility and degree of these disabilities varies widely, with some being apparent (such as visual impairment) and others being invisible unless they are disclosed (such as learning disability or hearing loss). Regardless of visibility, those with disabilities are likely to be adversely affected. 4 , 5 , 6 , 7 , 8 Many providers are familiar with the Americans with Disabilities Act (ADA) definition of a legal disability as someone with a physical or mental impairment that limits one or more major life activities. This includes people who have a record of such an impairment, even if they do not currently have or identify with the disability, to include all who need to be protected under the law. 9 For instance, a parent or physician of a young child with hearing loss may identify the child as having a disability at a young age to qualify for certain services to aid in development and function; however, as the child matures into adulthood, he or she may no longer identify as having a disability. It is important for all health care providers practicing in the United States to have a general understanding of the ADA and the applications of its provisions to health care noted in Table 1. 9 , 10 Most relevant are Titles II and III of the ADA, which require that medical providers afford individuals with disabilities full and equal access to their health care services and facilities, including making reasonable modifications to policies, practices, and procedures to allow full access. 9 , 10
Table 1.
Relevant Disability Laws
|
Americans with Disabilities Act of 1990 (ADA) |
Federal civil rights law that prohibits discrimination against individuals with disabilities in everyday activities, including medical services. Title I covers employment: requires employers to provide reasonable accommodations to qualified applicants or employees. A “reasonable accommodation” is a change that accommodates employees with disabilities so they can do the job without causing the employer “undue hardship” (too much difficulty or expense). The ADA requires access to medical care services and the facilities where the services are provided (Title II and III) and sets requirements for new construction of and alterations to buildings and facilities, including health care facilities. Title II covers public entities: public hospitals and clinics and medical offices operated by state and local governments: https://www.ada.gov/regs2010/titleII_2010/titleII_2010_regulations.htm Title III covers private hospitals or medical offices as places of public accommodations: https://www.ada.gov/regs2010/titleIII_2010/titleIII_2010_regulations.htm |
| Section 504 https://www2.ed.gov/policy/speced/leg/rehab/rehabilitation-act-of-1973-amended-by-wioa.pdf | Section 504 of the Rehabilitation Act of 1973 (Section 504) is a civil rights law that prohibits discrimination against individuals with disabilities on the basis of their disability in programs or activities that receive federal financial assistance, including health programs and services. |
In contrast to the legal model of disability described by the ADA, an alternative framework of disability that may be less familiar to EM physicians is the World Health Organization (WHO) International Classification of Functioning (ICF). This framework describes disability with regard to functioning within society, covering impairments, activity limitations, and participation restrictions. 11 , 12 The ICF states that disability results from the interaction of the person's body with the social and physical environment in which the person lives 11 , 12 (see Figure 1).
Figure 1.
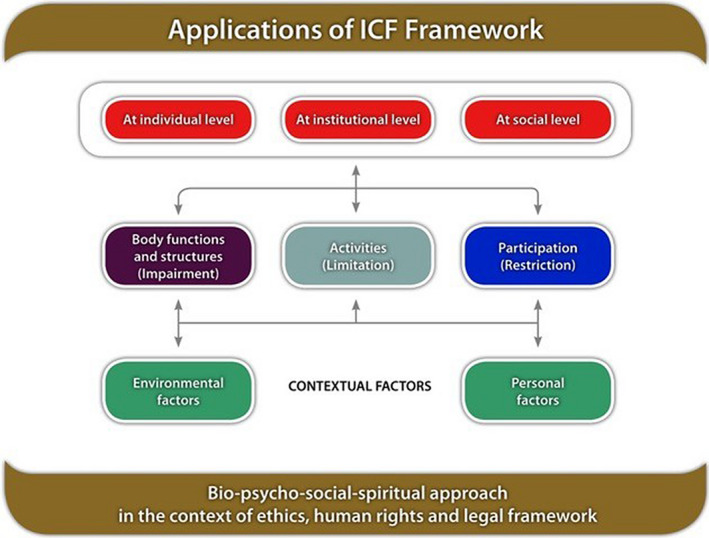
Applications of the ICF framework. Body functions are physiological functions of body systems (including psychological functions). Body structures are anatomic parts of the body such as organs, limbs, and their components. Impairments are problems in body function or structure such as a significant deviation or loss. Activity is the execution of a task or action by an individual. Participation is involvement in a life situation. Activity limitations are difficulties an individual may have in executing activities. Participation restrictions are problems an individual may experience in involvement in life situations. Environmental factors make up the physical, social, and attitudinal environment in which people live and conduct their lives. © Copyright World Health Organization (WHO), 2020. All Rights Reserved. Image accessed on February 26, 2019: http://origin.who.int/hrh/news/2014/hrh_icf_framework/en/. ICF = International Classification of Functioning.
The emphasis of the ICF on the experience of the person with a disability in society is rooted in the social model of disability, which states that people are disabled by the way society or the environment is organized, rather than by their individual impairments or differences. This environment includes both the physical environment and the social norms and structures that can either create or limit access for individuals with disabilities. The social model focuses on removing barriers that restrict independence and freedom. 13 In contrast, most health care providers traditionally utilize the medical model of disability, focusing on a person's impairments or differences and trying to “fix'' them, rather than on what the person needs to function in society. The medical model commonly conflates disability with disease and illness, when in fact they are distinct entities. 13 , 14
When using the medical model of disability in practice, a provider often focuses only on what is different about the patient from the general population, a term known as “othering.” Othering is formally defined as identifying and labeling those who are thought to be different from the mainstream population. 14 , 15 By referring to groups as “other” or practicing within this construct, one can unintentionally amplify the difference between groups and perpetuate marginalization. Othering has been associated with increased comorbidities such as hypertension, mental health problems, and shorter life expectancy. 16 , 17 , 18 , 19 The reason for this practice is likely multifactorial but may be fueled by a lack of provider education and training in caring for patients with disabilities or for those who require accommodations, leading to limited provider social and cultural awareness. A shift by health care providers to understanding and incorporating the ICF and the social model of disability is a vital first step to improving access for individuals with disabilities.
There is clear evidence that people with disabilities are a vulnerable and often unrecognized health disparity population. 5 Despite often having greater health care needs than the general population, people with disabilities experience significant barriers to accessing and obtaining health care (see Table 2) and have greater dissatisfaction with the care they do receive when compared to those without disabilities. 8 , 20
Table 2.
Barriers for Individuals With Disabilities When Interacting With Health Care System
| Types of Barriers | Examples |
|---|---|
| Attitudinal barriers |
|
| Communication barriers |
|
| Physical barriers |
|
| Policy barriers |
|
| Programmatic barriers |
|
| Social Barriers |
|
| Transportation barriers |
|
Adapted from CDC Disability Barriers to Inclusion: https://www.cdc.gov/ncbddd/disabilityandhealth/disability-barriers.html
One study demonstrated that patients with disabilities were more likely than those without disabilities to feel that the doctor did not listen to them, did not involve them in the treatment plan, and did not adequately explain treatments. 21 The negative attitudes of health care providers and use of outdated terms is discouraging and remains a significant barrier to effective care for patients with disabilities. 3 , 22 , 23 Additionally, adults with disabilities are substantially more likely to categorize their health as fair or poor (40.3%) when compared to those without disabilities (9.9%) and are more likely to delay seeking health care due to cost. 24 , 25 Physical accessibility also remains a significant challenge, as evidenced by a study in California demonstrating that out of a sample of 2,400 primary care clinics in California, more than half lacked full physical accessibility. 26
Rates of and risk factors for many chronic diseases are higher for patients with disabilities than the general population, including obesity, smoking, hypertension, and cardiovascular disease. 24 , 27 , 28 Despite these increased risks, patients with disabilities are less likely to receive needed preventive care. 27 , 29 , 30 For example, women with physical disabilities are less likely to receive mammograms and Pap smears when compared with able‐bodied peers. 24 , 28
Patients With Disabilities in the ED
Of specific interest to the field of EM, people with disabilities are significantly more likely to be victims of violent crimes than those without disabilities, including increased rates of rape and sexual assault as well as increased rates of intimate partner violence. 31 , 32 Emergency‐preparedness is another issue of disparity, as those with disabilities and their caregivers are less likely to evacuate in case of natural disaster, as evidenced during Hurricane Katrina. 33
Moreover, studies have demonstrated that individuals with disabilities present to the ED at a disproportionately higher rate than individuals without disabilities. A study in 2013 revealed that while 17% of working adults ages 18 to 65 identified as having a disability, this population accounted for 40% of annual ED visits. 34 In 2018, another study in Korea found that individuals with disabilities were twice as likely to visit the ED. 35 Factors that may contribute to increased use of the ED include disability status, complexity of the individual's health profile, and a lack of access to regular medical care (including prescription drug medications). 34 Given the reported rates of increased ED use in patients with a disability, most EM physicians will encounter individuals with disabilities on a regular basis; thus, it is logical to suggest that EM providers could benefit from more comprehensive training and preparation in order to care for this population.
Current State of Education on Care for People with Disabilities
Undergraduate Medical Education
Many medical students report little to no awareness of the ADA of 1990 as well as minimal experience with people with disabilities. 36 There is a lack of formal and standardized education on caring for patients with disabilities in most U.S. medical schools. Much of the learning in this domain comes from clinical experiences involving interacting with patients with disabilities. 37 Of the schools surveyed in the AAMC curriculum inventory in 2015 to 2016, only 23 of 134 schools explicitly addressed disability in their curriculum. 38
There are a few medical schools that have incorporated caring for patients with disabilities into their curricula. Some institutions do so through a variety of formats including traditional lectures, didactic teaching, objective structured clinical examinations, and use of standardized patients with disabilities (or acting disabilities); however, there are very few that incorporate a longitudinal and integrated disability‐based education. 39 , 40 , 41 One example of an institution that utilizes a longitudinal curriculum to integrate disability education throughout the 4 years of medical school is Jacobs School of Medicine and Biomedical Sciences at the State University of New York at Buffalo. Their disability education is a part of the core curriculum via lectures, small‐group sessions with families and patients with disabilities, standardized patient interactions with patients with disabilities, and didactic and clinical training during family medicine and internal medicine clerkships. Students also have the opportunity to participate in elective experiences, such as a family medicine research internship related to health care for individuals with disabilities and an elective on primary care for patients with disabilities. 37 , 41 Tufts Medical School and the University of South Carolina have also incorporated the use of standardized patients with disabilities (or acting disabilities) into their undergraduate medical curriculum. 41 The University of Rochester School of Medicine and Dentistry incorporates a Deaf health day, largely led by the local Deaf community, where medical students spend the day in simulations of what it is like to navigate the health care field as a Deaf American Sign Language (ASL) user. 42 Although these are distinct institutions with a wide variety of educational strategies regarding patients with disabilities, shared commonalities of these programs exist including improving communication, developing specific competencies, learning how to partner with the patient, and learning how to dissociate patients' disabilities from their capacity to be good sources of information. 36 Despite the relative lack of standardized, widespread curricula in medical schools across the United States, education on caring for patients with disabilities seems to be an effective way to improve students' knowledge, skills, and self‐reported attitudes about caring for such patients. 37 , 43 , 44
Graduate Medical Education
The Accreditation Council of Graduate Medical Education (ACGME) requires that residents demonstrate competence in respect and responsiveness to diverse patient populations, including but not limited to diversity in sex, age, culture, race, religion, disabilities, national origin, socioeconomic status, and sexual orientation as part of their core requirements. 45 However, there are no specific curriculum guidelines from the ACGME or the Residency Requirement Committee on how to achieve this competency. Additionally, there is no publicly available literature or research on existing educational programs for EM residents on caring for individuals with disabilities.
Much like the lack of standardized disability education in undergraduate medical education, there is also a lack of standardized curriculum and core competencies in graduate medical education. A study in one physical medicine and rehabilitation residency program demonstrated that even a small amount of disability training and awareness led to long‐term attitude changes in residents providing care for disabled patients. 46 In a Canadian obstetrics and gynecology residency program, a cross‐sectional study revealed that there was a need and interest in the area of caring for individuals with disabilities. 47 In a small study of psychiatry residents, there was improved self‐reported confidence and capacity to care for patients with intellectual disabilities. 48 There is little research and literature available on formal EM resident education on caring for people with disabilities and is an obvious area for improved exploration and curricular innovation. Given that EM providers are first‐line health care providers, a lack of attention to disability education and training in EM residency programs can perpetuate the marginalization of patients with disabilities.
Recommendations for EM Residency Curriculum
Design Curricula Utilizing a Model of Cultural Humility
To move to a social model of disability and avoid the trap of othering, EM programs should think about the best way to teach residents about disability. One commonly used approach is to teach cultural competency; however, the challenge with using only this method is that it erroneously assumes one can “know” another culture—that culture is something concrete, static, and applicable to all members of the group. There is increasing literature that suggests that cultural competency training alone is inadequate and may have negative results on health care providers as it can mistakenly be seen as a list of “do's and don't's” for a given group and inadvertently perpetuates stereotypes among the trainees. 49 , 50 , 51 While cultural competency teaching methods have some value, limitations to these teaching methods include false competence and ecologic fallacy (flawed reasoning that occurs when an inference is made about an individual based on aggregate data for a group). 52 , 53 , 54 There may be some positive impact on health care professional knowledge and patient satisfaction with cultural competency training, but a systematic review found poor evidence that this training positively impacts patient treatment adherence and there are no studies demonstrating improved health outcomes, which is arguably more important. 55 The same review also noted significant methodologic differences in all of the studies that were incorporated and no data on the most successful way to teach cultural competency. 55 It is clear that cultural competency alone, regardless of educational model, is imperfect and ultimately inadequate to reduce the health disparities experienced by those with disabilities.
An improved approach is to recognize culture as inextricably tied to power differences and societal inequalities. Culture represents more than the beliefs, practices, and values of particular groups; it is also located within a constantly shifting “network of meanings enmeshed within historical, social, economic and political processes.” 56 As cultural knowledge transfer for all types of accommodations is daunting and a longitudinal experience, medical students should start by learning cultural humility during their undergraduate medical education and continue this throughout EM residency training. 49
Cultural humility is a process tied to lifelong learning. Honing such humility is a skill that requires respect, cognizance, sincere effort, partnership with the community, and communication. 57 The Latin derivation of communication means “to find common with.” With such commonality arises insight and understanding as well as inspires confidence and comfort between patient and provider 57 (see Figure 2).
Figure 2.
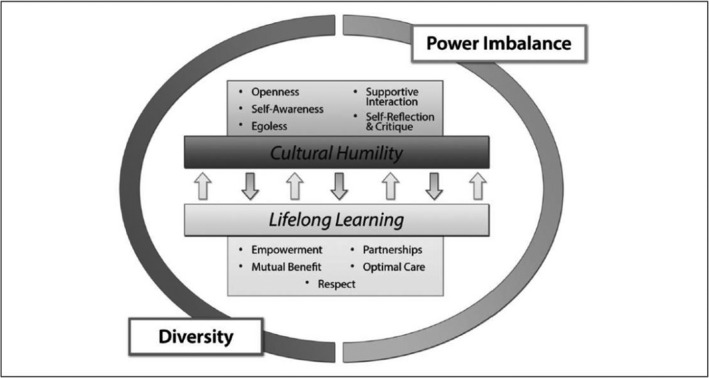
A concept analysis of cultural humility. 57 ICF = International Classification of Functioning. © 2015 by The Authors. Reprinted by Permission of SAGE Publications, Inc.
An example where education on cultural humility may be beneficial is with the Deaf ASL community. This group of people, distinct from those who identify as hearing impaired and communicate orally, often utilizes accommodations in the form of ASL interpreters for access to full communication with the hearing world. They are a cultural and linguistic community that behaves more similarly to other minority groups defined by a unique culture, primary language (ASL), and shared life experiences. 58 However, providers often label the Deaf ASL user as disabled, using only a medicolegal perspective. While people with hearing loss outside of the Deaf community often identify as disabled and do feel distressed by their hearing loss, members of the culturally Deaf community embrace their deafness and “Deafhood” (defined as the process by which they explain their own existence in the world). 59 , 60 Although culturally Deaf people share commonalities with other underrepresented groups (lower socioeconomic status, lower health and medical literacy), they do not identify as being disabled and view their Deafness positively through a cultural lens. 58 , 61 , 62 , 63 , 64 , 65 Through improved undergraduate and EM residency education, we can take steps toward increasing provider awareness of the dynamic definition of disability (not only with regards to the Deaf community) and its relation to power differentials and societal inequalities. This has the potential to mitigate some of the marginalization and othering experienced by the Deaf community and other minority groups. 15
Shifting from the static concept of cultural competency toward cultural humility emphasizes the need to recognize the dynamic nature of culture. We suggest starting with integrating curriculum that introduces cultural concepts regarding disabilities. In learning to care for an individual who needs accommodations, the learner needs to improve self‐awareness, become egoless in the quest for improvement, and be open‐minded enough to incorporate self‐reflection and critique into future interactions. 57 , 66
Integrate Disability Into Existing EM Curriculum and Milestones
Inclusion of education regarding patients with disabilities requires integration into existing EM didactic curriculum, the core competencies, and the evaluation system. Using a multimodal form of education including didactic sessions to introduce basic concepts (example: health disparities, cultural competency vs. humility, othering) and definitions (example, different types of disabilities and their respective accommodations), implicit bias testing, hands‐on simulation scenarios, research opportunities, and community‐based experiences allows for full integration. 67 , 68
We also suggest modification of some of the core ACGME EM milestones to reflect the integration of diversity and inclusion curricula, specifically incorporating milestones that evaluate residents on care of the patient with a disability. Examples of the original ACGME milestones can be seen in Figures 3A through 3C, 69 followed by suggested language modification.
Figure 3.
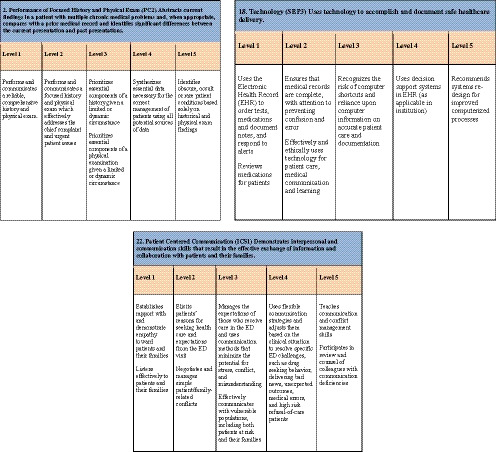
(A) Original EM Milestone 2. (B) EM Milestone 18. (C) Original EM Milestone 22. © 2012 The Accreditation Council for Graduate Medical Education and The American Board of Emergency Medicine. Reprinted with permission. 69
Suggested Modifications for EM Milestone 2 (Performance of Focused History and Physical Exam):
Level 1—Performs and communicates a reliable, comprehensive history and physical examination. Recognizes that a patient may require a modified approach to the history or physical examination in the setting of a disability.
Level 2—Performs and communicates a focused history and physical examination, which effectively addresses the chief complaint and urgent patient issues. Asks the patient (first) and visitors what accommodations are needed during the history and physical exam.
Level 3—Prioritizes essential components of a history and physical given a limited or dynamic circumstance. Establishes patient's baseline level of functioning and recognizes changes from baseline. Seeks appropriate resources necessary to adapt the history and physical for patients who require accommodations.
Level 4—Synthesizes essential data necessary for the correct management of patients using all potential sources of data including acknowledging the patient and/or family as experts by experience and including them in developing a plan.
Level 5—Identifies obscure, occult, or rare patient conditions based solely on historical and physical examination findings in all patients, including those requiring accommodations.
Suggested Modifications for EM Milestone 18 (Technology):
Level 1—Uses the electronic health record (EHR) to order tests, medications, and document notes and respond to alerts. Reviews medications for patients. Recognizes the need for assistive devices in patients with disabilities (communication devices, wheelchairs, hoyers, etc.).
Level 2—Ensures that medical records are complete, with attention to preventing confusion and error. Effectively and ethically uses assistive technology for patient care, medical communication, and learning.
Level 3—Recognizes the risk of computer shortcuts and reliance upon computer information on accurate patient care and documentation. Recognizes limitations of assistive devices (i.e., limited access to Wi‐Fi, battery power, physical/spatial constrictions).
Level 4—Uses decision support systems in EHR (as applicable in institution). Participates in departmental efforts to navigate the limitations of assistive devices.
Level 5—Recommends systems redesign for improved access to appropriate technology to facilitate care for all patients, especially those requiring accommodations.
(Patient Centered Communication):
Level 1—Establishes rapport with and demonstrate empathy toward patients and their families. Listens effectively to patients and their families or caregivers. Recognizes that a patient requires language accommodations.
Level 2—Elicits patients' reasons for seeking health care and expectations from the ED visit in the resident's primary language or through the use of appropriate language accommodations. Negotiates and manages simple patient‐/family‐related conflicts.
Level 3—Manages the expectations of those who receive care in the ED and uses communication methods that minimize the potential for stress, conflict, and misunderstanding. Effectively communicates with vulnerable populations, including both patients at risk and their families. Recognizes when there has been communication breakdown even with appropriate use of language accommodations.
Level 4—Uses flexible communication strategies and adjusts them based on the clinical situation to resolve specific ED challenges, such as drug‐seeking behavior, delivering bad news, unexpected outcomes, medical errors, and high‐risk refusal‐of‐care patients. Adapts communication strategies for patients requiring accommodations to resolve communication breakdown (interpreter services, visual communication, language assistive devices, etc.)
Level 5—Teaches communication and conflict management skills. Participates in review and counsel of colleagues with communication deficiencies. Recognizes systems‐based challenges to establishing appropriate communication with patients and their families (lack of interpreters, private space, etc.) and participates in departmental effort for improvement.
Engage the Disability Community in Residency Education
In undergraduate medical education, it has been demonstrated that incorporating individuals from the community with disabilities into training on caring for patients with disabilities had a positive effect on the self‐reported comfort levels of young learners in caring for these patients. 37 , 68 Additionally, the incorporation of narratives from the “expert by experience” has the potential to positively influence one's perspective of those with disabilities. 70 Outside of the field of medicine, research has shown that learning from a person with a disability is more beneficial not only to others with disabilities, but also to those without disabilities. 71 This is particularly true because people with disabilities as educators are equipped with unique knowledge, which comes from having a different perspective on navigating the world. 71 Such a perspective is not only beneficial to learners with disabilities as they have someone to relate to, but is also beneficial to learners without disabilities as they may deem the information to be more reputable coming from someone having experienced life with a disability. Furthermore, seeing people with disabilities as educators also challenges the stigma that typically surrounds disability, which can provide a new perspective for those without disabilities. 71 In a study on students' perceptions of having a tutor with a disability, namely, quadriplegia mixed‐type cerebral palsy, students found that having a tutor with a disability was beneficial for them as learners. Not only was the tutor competent in the material on which she was tutoring but also the tutor also caused them to reflect on and reevaluate their perspective on the abilities possessed by those living with a disability. 72 As a result of her own experiences, the tutor was able to take on a mentoring role in addition to a tutoring role. Overall, the students felt enlightened and empowered by their interactions with the tutor with a disability. 72 Inclusion of people with disabilities both as educators during medical education and training and within the health care profession has a multitude of potential benefits for patients and for healthcare professionals with and without disabilities alike. 72 , 73 , 74 , 75
Identify Resources and Champions
When trying to develop a disability curriculum (such as presenters for didactic presentations, resources for simulations sessions, or ideas for community engagement), identifying local champions can be beneficial. If you are affiliated with a school of medicine, there should be resources available to help students and learners who need accommodations, often through a disability service office or office of diversity and inclusion. Consider reaching out to these offices and asking them to participate in a hands‐on session or to give a brief presentation to your interns at the start of their residency. This will have the dual benefit of exposing the learner to information on different types of disabilities and simultaneously making them aware of available resources should the need ever arise. Other sources include national organizations such as ADIEM (part of SAEM), which has a speaker's list with associated areas of expertise, or approaching other national organizations for regional or national experts (see Table 3). Finally, utilizing the experience and network of connections within your faculty group will allow access to local experts who may be able to provide education on this topic and relate it specifically to the community in which they serve.
Table 3.
National Organizations and Teaching Resources.
AAMC = Association of American Medical College; ADIEM = Academy for Diversity and Inclusion in Emergency Medicine; CDC = Centers for Disease Control and Prevention.
Advocate for the Inclusion of Individuals With Disabilities in Emergency Medicine
A recent paper notes that medical students with disabilities may be discouraged from pursuing specific specialties, such as EM, due to erroneous assumptions or beliefs regarding the student's abilities and/or possible accommodations. 76 In 2002, a study found the rate of disability within residents in EM was 1.3%, as reported by program directors, although this number likely represents slight underreporting due to the barriers and challenges to reporting a disability. 77 As previously noted, inclusion of people (community member or provider) with disabilities as educators and into the medical profession has multiple benefits. 37 , 67 , 69 , 70 , 71 , 72 , 73 , 74 , 78 Residency programs can promote inclusion of residents with disabilities by seeking to develop transparent processes, solidifying their understanding of the ADA, identifying a knowledgeable disability expert, and understanding the benefits of inclusion to patients and residents. 79 Residencies can advertise their willingness to incorporate those with disabilities or who require accommodations on residency brochures, websites, and social media, thereby demonstrating a safe and inclusive environment. 76 Prejudice and bias may also be lessened by interacting with a provider who has experienced some of the same challenges of navigating the health care system as a physician‐patient who is part of a marginalized group, leading to decreased misinformation and negative attitudes about this group of people. 73
We recommend that EM residency programs share their experiences integrating curriculum, engaging the community, accommodating residents with disabilities, and promoting inclusion of those with disabilities into EM to foster knowledge transfer and establish best practices within EM.
Conclusion
People with disabilities are often marginalized and overlooked, yet they are a group we often care for in emergency medicine. To provide equitable care for these patients, emergency medicine providers must be equipped with the appropriate knowledge and training. Consequently, new curricula and teaching modalities need to be developed and integrated into emergency medicine residency education training programs. The impact of cultural humility and its positive implications on care for specific groups of marginalized patients has been well documented for the past several years, yet there remains no standardized method of teaching cultural humility in emergency medicine residency training. As a group of professionals committed to the education of physicians caring for those with disabilities, we urge residencies and residency leadership to recognize those with disabilities as a marginalized population and to incorporate the aforementioned recommendations into emergency medicine residency education.
AEM Education and Training 2020;4:450–462
Presented at the Society for Academic Emergency Medicine Annual Meeting, May 2019, Las Vegas, NV.
The authors have no relevant financial information or potential conflicts to disclose.
References
- 1. Okoro CA, Hollis ND, Cyrus AC, Griffin‐Blake S. Prevalence of disabilities and health care access by disability status and type among adults—United States, 2016. Morb Mortal Wkly Rep 2018;67:882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Office of the Surgeon General (US); Office on Disability (US) . The Surgeon General's Call to Action to Improve the Health and Wellness of Persons with Disabilities. Rockville, MD: Office of the Surgeon General (US); 2005. [PubMed] [Google Scholar]
- 3. Agaronnik N, Campbell EG, Ressalam J, Iezzoni LI. Exploring issues relating to disability cultural competence among practicing physicians. Disability Health J 2019;12:403–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Davis NA. Invisible disability. Ethics 2005; 116:153–213. [DOI] [PubMed] [Google Scholar]
- 5. Krahn GL, Walker DK, Correa‐De‐Araujo R. Persons with disabilities as an unrecognized health disparity population. Am J Public Health 2015;105:S198–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lagu T, Hannon NS, Rothberg MB, et al. Access to subspecialty care for patients with mobility impairment: a survey. Ann Intern Med 2013;158:441–6. [DOI] [PubMed] [Google Scholar]
- 7. Mahmoudi E, Meade MA. Disparities in access to health care among adults with physical disabilities: analysis of a representative national sample for a ten‐year period. Disability Health J 2015;8:182–90. [DOI] [PubMed] [Google Scholar]
- 8. Gulley SP, Altman BM. Disability in two health care systems: access, quality, satisfaction, and physician contacts among working‐age Canadians and Americans with disabilities. Disability Health J 2008;1:196–208. [DOI] [PubMed] [Google Scholar]
- 9. Americans with Disabilities Act Title III Regulations. Washington, DC: Department of Justice, 2010. [Google Scholar]
- 10. Jette AM, Field MJ. The Future of Disability in America. Washington, DC: The National Academies Press, 2007. [PubMed] [Google Scholar]
- 11. Classification of Functioning, Disability, and Health: Children & Youth Version: ICF‐CY. Geneva: World Health Organization, 2007. [Google Scholar]
- 12. International Classification of Functioning, Disability and Health (ICF). Geneva: World Health Organization, 2001. [Google Scholar]
- 13. Goering S. Rethinking disability: the social model of disability and chronic disease. Curr Rev Musculoskelet Med 2015;8:134–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Roberts ML, Schiavenato M. Othering in the nursing context: a concept analysis. Nursing Open 2017;4:174–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Johnson JL, Bottorff JL, Browne AJ, Grewal S, Hilton BA, Clarke H. Othering and being othered in the context of health care services. Health Commun 2004;16:255–71. [DOI] [PubMed] [Google Scholar]
- 16. Krieger N. Embodying inequality: a review of concepts, measures, and methods for studying health consequences of discrimination. Int J Health Serv 1999;29:295–352. [DOI] [PubMed] [Google Scholar]
- 17. Krieger N, Sidney S. Racial discrimination and blood pressure: the CARDIA study of young black and white adults. Am J Public Health 1996;86:1370–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Littleford LN, Wright MO. Health consequences of positive and negative interracial interactions at a predominantly Caucasian public university. J Gender Cult Health 1998;3:129–45. [Google Scholar]
- 19. Noh S, Beiser M, Kaspar V, Hou F, Rummens J. Perceived racial discrimination, depression, and coping: a study of Southeast Asian refugees in Canada. J Health Soc Behav 1999;40:193–207. [PubMed] [Google Scholar]
- 20. Common Barriers to Participation Experienced by People with Disabilities . Centers for Disease Control and Prevention. 2019. Available at: https://www.cdc.gov/ncbddd/disabilityandhealth/disability-barriers.html. Accessed Mar 20, 2020.
- 21. Smith DL. Disparities in patient‐physician communication for persons with a disability from the 2006 Medical Expenditure Panel Survey (MEPS). Disability Health J 2009;2:206–15. [DOI] [PubMed] [Google Scholar]
- 22. Iacono T, Bigby C, Unsworth C, Douglas J, Fitzpatrick P. A systematic review of hospital experiences of people with intellectual disability. BMC Health Serv Res 2014;14:505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Shakespeare T, Iezzoni LI, Groce NE. Disability and the training of health professionals. Lancet 2009;374:1815–6. [DOI] [PubMed] [Google Scholar]
- 24. Altman BM, Bernstein A. Disability and health in the United States, 2001‐2005. Hyatsville, MD: National Center of Health Statistics, 2008. [Google Scholar]
- 25. Control CfD, Prevention . Delayed or forgone medical care because of cost concerns among adults aged 18–64 years, by disability and health insurance coverage status National Health Interview Survey, United States, 2009. Morb Mortal Wkly Rep 2010;59(44):1456. [Google Scholar]
- 26. Mudrick NR, Breslin ML, Liang M, Yee S. Physical accessibility in primary health care settings: results from California on‐site reviews. Disabil Health J 2012;5:159–67. [DOI] [PubMed] [Google Scholar]
- 27. Reichard A, Stolzle H, Fox MH. Health disparities among adults with physical disabilities or cognitive limitations compared to individuals with no disabilities in the United States. Disabil Health J 2011;4:59–67. [DOI] [PubMed] [Google Scholar]
- 28. Disability and Health Program, Division of Human Development and Disability, National Center on Birth Defects and Developmental Disabilities, Centers for Disease Control and Prevention . Disability and Health State Chartbook, 2006: Profiles of Health for Adults With Disabilities. Atlanta: Centers for Disease Control and Prevention, 2006. [Google Scholar]
- 29. Diab ME, Johnston MV. Relationships between level of disability and receipt of preventive health services. Arch Phys Med Rehabil 2004;85:749–57. [DOI] [PubMed] [Google Scholar]
- 30. Iezzoni LI, McCarthy EP, Davis RB, Siebens H. Mobility impairments and use of screening and preventive services. Am J Public Health 2000;90:955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Rand MR, Harrell E. Crime Against People With Disabilities, 2007. Washington, DC: US Department of Justice, Office of Justice Programs, Bureau of Justice, 2009. [Google Scholar]
- 32. Centers for Disease Control and Prevention (CDC) . Adverse health conditions and health risk behaviors associated with intimate partner violence‐‐United States, 2005. MMWR Morb Mortal Wkly Rep 2008;57:113‐7. [PubMed] [Google Scholar]
- 33. Brodie M, Weltzien E, Altman D, Blendon RJ, Benson JM. Experiences of Hurricane Katrina evacuees in Houston shelters: implications for future planning. Am J Public Health 2006;96:1402–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Rasch EK, Gulley SP, Chan L. Use of emergency departments among working age adults with disabilities: a problem of access and service needs. Health Serv Res 2013;48:1334–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kim YE, Lee YR, Yoon SJ, Kim Y, Oh IH. Years of life lost due to premature death in people with disabilities in Korea: the Korean national burden of disease study framework. J Korean Med Sci 2019;34:e22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Long‐Bellil LM, Robey KL, Graham CL, et al. Teaching medical students about disability: the use of standardized patients. Acad Med 2011;86:1163–70. [DOI] [PubMed] [Google Scholar]
- 37. Symons AB, McGuigan D, Akl EA. A curriculum to teach medical students to care for people with disabilities: development and initial implementation. BMC Med Educ 2009;9:78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Todd C. Curriculum Inventory in Context. AAMC; Available at: https://wwwaamcorg/download/464750/data/ciic03-5may2016pdf2016. Accessed Nov 1, 2019. [Google Scholar]
- 39. Holder M, Waldman HB, Hood H. Preparing health professionals to provide care to individuals with disabilities. Int J Oral Sci 2009;1:66–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Seidel E, Crowe S. The state of disability awareness in American medical schools. Am J Phys Med Rehabil 2017;96:673–6. [DOI] [PubMed] [Google Scholar]
- 41. Santoro JD, Yedla M, Lazzareschi DV, Whitgob EE. Disability in US medical education: disparities, programmes and future directions. Health Educ J 2017;76:753–9. [Google Scholar]
- 42. Thew D, Smith SR, Chang C, Starr MM. The Deaf Strong Hospital program: a model of diversity and inclusion training for first‐year medical students. Acad Med 2012;87:1496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Shakespeare T, Kleine I. Educating health professionals about disability: a review of interventions. Health Social Care Educ 2013;2:20–37. [Google Scholar]
- 44. Ioerger M, Flanders RM, French‐Lawyer JR, Turk MA. Interventions to teach medical students about disability: a systematic search and review. Am J Phys Med Rehabil 2019;98:577–99. [DOI] [PubMed] [Google Scholar]
- 45. Swing SR. The ACGME outcome project: retrospective and prospective. Med Teach 2007;29:648–54. [DOI] [PubMed] [Google Scholar]
- 46. Moroz A, Gonzalez‐Ramos G, Festinger T, Langer K, Zefferino S, Kalet A. Immediate and follow‐up effects of a brief disability curriculum on disability knowledge and attitudes of PM&R residents: a comparison group trial. Med Teach 2010;32:e360–4. [DOI] [PubMed] [Google Scholar]
- 47. Bekdache GN, Berndl A. Women with physical disability in pregnancy resident education: a national survey as a needs assessment for curriculum improvement in obstetrics and gynaecology in Canada. BMJ Open 2019;9:e024505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Ruedrich S, Dunn J, Schwartz S, Nordgren L. Psychiatric resident education in intellectual disabilities: one program's ten years of experience. Acad Psychiatry 2007;31:430–4. [DOI] [PubMed] [Google Scholar]
- 49. Kleinman A, Benson P. Anthropology in the clinic: the problem of cultural competency and how to fix it. PLoS Med 2006;3:e294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Betancourt JR. Cultural competence–marginal or mainstream movement? N Engl J Med 2004;351:953–5. [DOI] [PubMed] [Google Scholar]
- 51. Culley L. A critique of multiculturalism in health care: the challenge for nurse education. J Adv Nurs 1996;23:564–70. [DOI] [PubMed] [Google Scholar]
- 52. Te Grotenhuis M, Eisinga R, Subramanian S. Robinson's ecological correlations and the behavior of individuals: methodological corrections. Int J Epidemiol 2011;40:1123–5. [DOI] [PubMed] [Google Scholar]
- 53. Freedman DA. Ecological inference and the ecological fallacy. Int Encycloped Social Behav Sci 1999;6:1–7. [Google Scholar]
- 54. Idrovo AJ. Three criteria for ecological fallacy. Environ Health Perspect 2011;119:a332‐a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Beach MC, Price EG, Gary TL, et al. Cultural competency: a systematic review of health care provider educational interventions. Med Care 2005;43:356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Anderson J, Reimer Kirkham S. Discourses on health: a critical perspective. In: A Cross‐cultural Dialogue on Health Care Ethics Waterloo: Wilfrid Laurier University Press, 1999. p. 47–67. [Google Scholar]
- 57. Foronda C, Baptiste DL, Reinholdt MM, Ousman K. Cultural humility: a concept analysis. J Transcult Nurs 2016;27:210–7. [DOI] [PubMed] [Google Scholar]
- 58. Richardson KJ. Deaf culture: competencies and best practices. Nurse Pract 2014;39:20–8. [DOI] [PubMed] [Google Scholar]
- 59. Hauser PC, O'Hearn A, McKee M, Steider A, Thew D. Deaf epistemology: deafhood and deafness. Am Ann Deaf 2010;154:486–92. [DOI] [PubMed] [Google Scholar]
- 60. Eriksson‐Mangold M, Carlsson S. Psychological and somatic distress in relation to perceived hearing disability, hearing handicap, and hearing measurements. J Psychosom Res 1991;35:729–40. [DOI] [PubMed] [Google Scholar]
- 61. McKee MM, McKee K, Winters P, Sutter E, Pearson T. Higher educational attainment but not higher income is protective for cardiovascular risk in deaf American Sign Language (ASL) users. Disabil Health J 2014;7:49–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Holt JA. Stanford achievement test—8th edition: reading comprehension subgroup results. Am Ann Deaf 1993;138:172–5. [Google Scholar]
- 63. McKee MM, Paasche‐Orlow MK. Health literacy and the disenfranchised: the importance of collaboration between limited English proficiency and health literacy researchers. J Health Commun 2012;17:7–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Martin ML, Heron S, Moreno‐Walton L, Strickland M, editors. Diversity and Inclusion in Quality Patient Care. Basel: Springer, 2019. [Google Scholar]
- 65. Barnett S, Klein JD, Pollard RQ Jr, et al. Community participatory research with deaf sign language users to identify health inequities. Am J Public Health 2011;101:2235–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Tervalon M, Murray‐Garcia J. Cultural humility versus cultural competence: a critical distinction in defining physician training outcomes in multicultural education. J Health Care Poor Underserved 1998;9:117–25. [DOI] [PubMed] [Google Scholar]
- 67. Symons AB, Morley CP, McGuigan D, Akl EA. A curriculum on care for people with disabilities: effects on medical student self‐reported attitudes and comfort level. Disabil Health J 2014;7:88–95. [DOI] [PubMed] [Google Scholar]
- 68. Ankam NS, Bosques G, Sauter C, et al. Competency‐based curriculum development to meet the needs of people with disabilities: a call to action. Acad Med 2019;94:781–8. [DOI] [PubMed] [Google Scholar]
- 69. Beeson JK, Christopher T, Heidt J, et al. The Emergency Medicine Milestones Project. Chicago: The Accreditation Council for Graduate Medical Education and The American Board of Emergency Medicine, 2015. [Google Scholar]
- 70. Pritchard G. Disabled people as culturally relevant teachers. J Social Inclusion 2010;1:43–51. [Google Scholar]
- 71. Sheridan L, Kotevski S. University teaching with a disability: student learnings beyond the curriculum. Int J Incl Educ 2014;18:1162–71. [Google Scholar]
- 72. Corbet B, Madorsky J. Physicians with disabilities. West J Med 1991;154:514. [PMC free article] [PubMed] [Google Scholar]
- 73. DeLisa JA, Thomas P. Physicians with disabilities and the physician workforce: a need to reassess our policies. Am J Phys Med Rehabil 2005;84:5–11. [DOI] [PubMed] [Google Scholar]
- 74. Washington DL, Bowles J, Saha S, et al. Transforming clinical practice to eliminate racial–ethnic disparities in healthcare. J Gen Intern Med 2008;23:685–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Awosogba T, Betancourt JR, Conyers FG, et al. Prioritizing health disparities in medical education to improve care. Ann N Y Acad Sci 2013;1287:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Meeks LM, Jain N. Accessibility, Inclusion, and Action in Medical Education: Lived Experiences of Learners and Physicians with Disabilities. Washington, DC: Association of American Medical Colleges, 2018. [Google Scholar]
- 77. Takakuwa KM, Ernst AA, Weiss SJ. Residents with disabilities: a national survey of directors of emergency medicine residency programs. South Med J 2002;95:436–41. [PubMed] [Google Scholar]
- 78. Cohen JJ, Gabriel BA, Terrell C. The case for diversity in the health care workforce. Health Aff (Millwood) 2002;21:90–102. [DOI] [PubMed] [Google Scholar]
- 79. Meeks LM, Jain NR, Moreland C, Taylor N, Brookman JC, Fitzsimons M. Realizing a diverse and inclusive workforce: equal access for residents with disabilities. J Grad Med Educ 2019;11:498–503. [DOI] [PMC free article] [PubMed] [Google Scholar]


