Abstract
Background
Point‐of‐care ultrasound (POCUS) is important to the practice of emergency medicine (EM), but requires training to achieve competence. The purpose of this study was to describe the current state of POCUS practice and perceived barriers to the implementation in EM training programs in India.
Methods
A cross‐sectional survey consisting of 28 questions was administered to 378 faculty and residents in postgraduate EM training programs across India.
Results
Data were collected from 159 physicians from 16 institutions; 76% of them were EM residents, with a response rate of 42%. Respondents overwhelmingly reported high interest (91%) in learning POCUS topics. Respondents identified highest levels of comfort with the performance and interpretation of trauma ultrasound (US) and echocardiography. Conversely, there was a scarce interest and low levels of competence in performing obstetric US, which may be a result of the practice of triaging these complaints to obstetricians and gynecologists. Lack of US equipment and dedicated training were the highest rated barriers by a significant margin, which 56% of respondents ranked as “very important.”
Conclusions
While significant interest in POCUS exists among the Indian EM physicians, comfort and competence were limited to trauma and echocardiography applications. Expansion of and comfort with POCUS use in these settings may be sought through improvement of access to US equipment and a dedicated US curriculum.
Point‐of‐care ultrasound (POCUS) has become a widely available and essential tool in the practice of emergency medicine (EM). Its importance in the field is demonstrated by its inclusion in the Model of Clinical Practice of Emergency Medicine as an “integral diagnostic procedure,” 1 and it is now a recognized part of the curriculum in most EM residencies in the United States with dedicated didactics, clinical rotations, and evaluations of competency. 2
Point‐of‐care ultrasound has also been shown to be invaluable to clinicians practicing in austere environments and the developing world. 3 , 4 , 5 , 6 Its relatively low cost, lack of ionizing radiation, and ability to provide immediate diagnostic information make it the ideal imaging modality for these clinical environments. Many of these countries have only recently developed formalized training in EM and, as such, may not have a dedicated curriculum in POCUS.
Emergency medicine is a relatively new specialty in India, achieving specialty status from the Medical Council of India in 2009. Our institution has been active in training emergency physicians across India since 2008, training hundreds of physicians in that time. Training in POCUS is a key component of EM training in North America, but a formal comprehensive curriculum development for the Indian training programs has yet to be determined. Unlike many western institutions, training and practice of ultrasound (US) in Indian facilities has special consideration due to India’s Pre‐Conception and Pre‐Natal Diagnostic Techniques Act. While the Act is meant to regulate fetal US and prevent prenatal sex determination, it has also curtailed the widespread use of POCUS in India. The lack of flexibility in the use of US with current governmental regulations and traditional EM curriculum emerged as part of barriers of implementing POCUS in EM programs in India. 7
The purpose of this study was to survey faculty and residents affiliated with our institution’s postgraduate EM training programs in India to assess the current interest in, competence with, and capacity for POCUS in EM in India. This survey served as a needs assessment for curriculum development in emergency US for Indian emergency physicians.
Methods
Study Design
We conducted a quantitative cross‐sectional survey of faculty and residents in our affiliated EM programs throughout India, using a SurveyMonkey interface. The study was approved by The George Washington University Institutional Review Board, and informed consent was obtained from all study participants.
Study Setting and Population
The Ronald Reagan Institute of Emergency Medicine (RRIEM) at The George Washington University is a nonprofit entity founded in 1991 with a mission to improve emergency care, education, training, and consultative support. One of the key goals of the Reagan Institute is to improve emergency care throughout the world through education, training, and capacity building. In furtherance of this goal, our institution has established partnership training programs across India that have trained over 360 emergency physicians since 2007. 8 The International Masters in Emergency Medicine (MEM) program is a 3‐year certificate program with faculty supervision and teaching, similar to EM residency programs in the United States in structure and scope.
Inclusion criteria for the study were residents and faculty affiliated with the RRIEM MEM training programs in India. The survey was designed to assess the current state of practice in the largest group of EM training programs in India, to provide information regarding the need, interest, and capability for POCUS training in Indian EM training programs.
Study Protocol/Survey Instrument
A 28‐question survey was developed to determine the current state of each site’s equipment, skills, local radiology support (X‐ray, CT, MRI), and US technology and exportability. Respondents were asked to characterize (through a combination of structured multiple‐choice, 5‐point Likert scale and closed‐ended questions) their experience and comfort with various examination types of emergency US, detail the current training available for the use of POCUS, and describe how they employ US in evaluating specific types of chief complaints (dyspnea, shock, trauma, pregnancy, musculoskeletal complaints, chest pain, abdominal pain, etc.). In addition, questions were included regarding barriers to emergency US use, the equipment and transducers available for use, and the ease of image transfer (see Data Supplement S1 [available as supporting information in the online version of this paper, which is available at http://onlinelibrary.wiley.com/doi/10.1002/aet2.10423/full] for full survey).
An e‐mail containing a link to the survey was sent to each participant that was personalized for each user to track responses and e‐mail nonresponders, but data collected were anonymous. Nonresponders were contacted three times over 3 months to maximize survey response.
Data Analysis
Descriptive statistical analyses including frequencies and percentages were used for dichotomous and categorical outcomes. Not all questions were answered by all respondents, and percentages are given for the denominator of respondents for each individual question.
Results
Surveys were sent to 378 physicians. A total of 310 EM residents (82% of those surveyed) and 68 EM faculty (18% of those surveyed) were included. About 159 physicians partially or fully responded to the survey, for a response rate of 42%. A total of 24% of respondents were attending physicians/consultants/specialists in EM and 76% were residents. While 66% had previous hands‐on exposure to POCUS, the number of scans per respondent varied from less than 10 to greater than 1,000. A total of 53% of respondents had received POCUS training at the bedside in the hospital, 26% had taken a continuing medical education course with didactics and hands‐on exposure, and 21% had received no formal training (Table 1). A broad cross‐section of 16 training sites across India was represented (Figure 1).
Table 1.
Characteristics of EM Physicians
| Characteristic | n | % |
|---|---|---|
| Level of training | ||
| First‐year resident | 38 | 35 |
| Second‐year resident | 20 | 19 |
| Third‐year resident | 24 | 22 |
| Attending/specialist/consultant | ||
| 0–5 years | 15 | 14 |
| 6–10 years | 4 | 4 |
| >10 years | 7 | 6 |
| Previous practical exposure to POCUS | ||
| Yes | 71 | 66 |
| No | 37 | 34 |
| Number of independent POCUS examinations performed | ||
| 0–10 | 24 | 26 |
| 11–20 | 6 | 6 |
| 21–40 | 17 | 18 |
| 41–100 | 19 | 20 |
| 101–1,000 | 22 | 24 |
| >1,000 | 5 | 5 |
| Formal instruction in POCUS | ||
| Yes, CME course, didactics, and hands‐on | 28 | 26 |
| Yes, bedside teaching in hospital | 57 | 53 |
| None | 23 | 21 |
Figure 1.
Locations of EM training programs responding to the survey.
Comfort level performing and interpreting POCUS varied across applications (Figure 2). Respondents overwhelmingly reported high interest (91%) in learning more about POCUS. Likelihood of use of POCUS for specific chief complaints is displayed in Figure 3. Perceived barriers to POCUS implementation are reported in Figure 4. Only 63% of respondents reported access to a dedicated ED US machine, and an additional 32% borrowed a machine from radiology or cardiology when needed.
Figure 2.
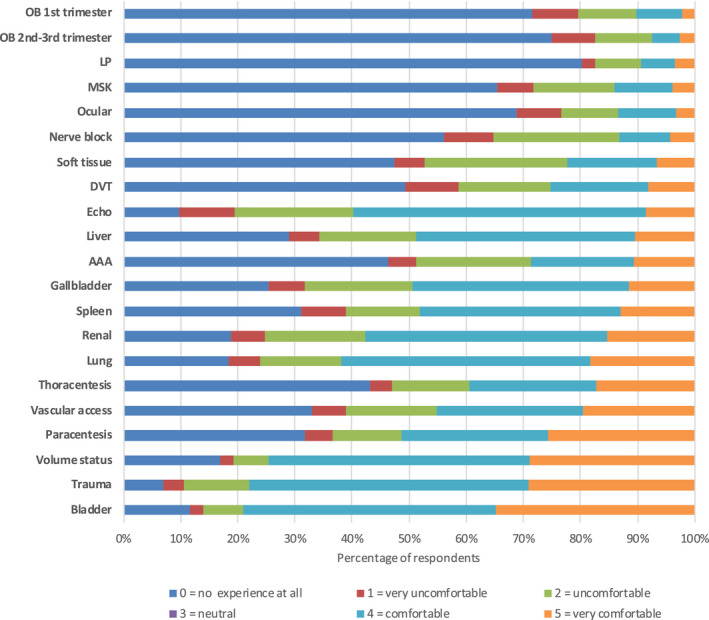
Comfort level performing and interpreting POCUS examinations by examination type. POCUS = point‐of‐care ultrasound.
Figure 3.
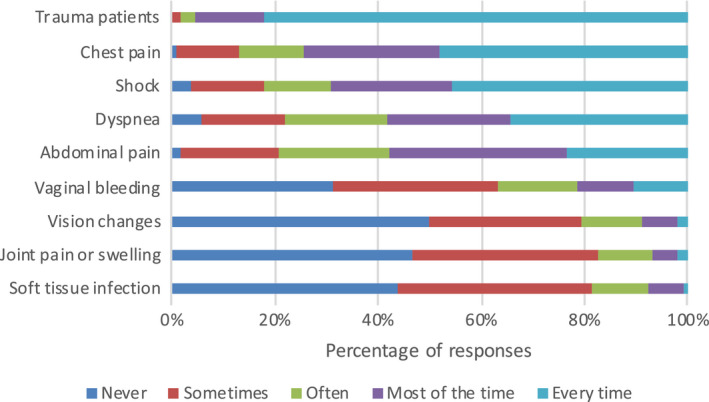
Use of POCUS for specific chief complaints. “When patients present with these chief complaints, how likely are you to use POCUS?” POCUS = point‐of‐care ultrasound.
Figure 4.
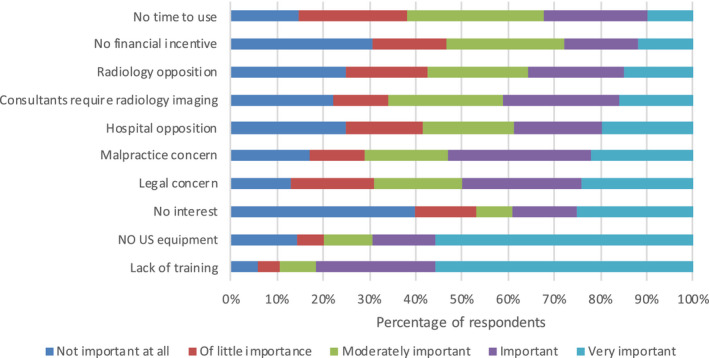
Perceived barriers to POCUS implementation. POCUS = point‐of‐care ultrasound.
A total of 64% of respondents reported dedicated time in their residency training program to learn US, but only 42% had a POCUS curriculum. A total of 98% of respondents reported that it is “important” or “very important” to have a structured curriculum with dedicated time for POCUS in their training program.
Discussion
The original purpose of this study was to collect information that could be used to improve POCUS training in India, but it also provides interesting information regarding the current state of provider comfort and usage patterns of US in Indian emergency departments. This paper adds to a growing and important body of literature exploring the use of US in the international community. A previous study of 41 Indian EM residents addressing US training in Indian EM programs found that eFAST was the examination most commonly performed, but noted a wide range of adoption of other indications and pointed to a need for a guideline/standardization of POCUS in the EM curriculum. 9
Our respondents represented a wide range of levels of training, with 24% having completed their residency and the remaining 76% relatively evenly divided among each of the 3 years of training. Interestingly, while the experience level of providers is quite evenly distributed (with representation gradually tapering off in the more senior respondents), the reported number of scans performed is nearly bimodal, with 26% having performed 0 to 10 and 28% having performed >100 scans. It is unclear whether this represents a temporal effect relating to the timing of US’s introduction into emergency departments and training programs in India, with junior providers making more frequent use, or if this indicates a more heterogenous distribution with “superusers” across all levels of experience based on personal practice patterns and interest.
The breakdown of that experience by imaging modality yields insight into how POCUS is currently being used. Relatively few respondents reported experience with obstetric US across all trimesters, a fairly common application in emergency departments in the United States and European countries and one of the American College of Emergency Physicians core applications. 10 This is likely in part due to India’s Pre‐Conception and Pre‐Natal Diagnostic Techniques Act of 1994 that regulates fetal US and prohibits prenatal sex determination. Prenatal sex determination is a crime punishable by imprisonment in India secondary to a high rate of female infanticide in the country. Parallel practice by obstetric services as the primary providers for these presentations may have some impact as well. Trauma US had the highest reported comfort level in performing and interpreting US, with 62% of respondents “comfortable” or “very comfortable” with this modality. Echocardiography was the next highest with 45% of respondents reporting being “comfortable” or “very comfortable,” although fewer participants reported being “very comfortable” with echocardiography compared with trauma, likely due to the increased technical skill required in echocardiography. Interestingly, determination of volume status was the fourth most common application and had the second highest rates of comfort (62% reporting being “comfortable” or “very comfortable”), indicating that this is well integrated into their practice pattern, and supported by the fact that 50% of respondents indicated they use US in evaluating patients in shock “every time.” Instituting a formalized QA process with feedback and education for sonographers may help close the confidence gap.
Some of the less traditional applications of US had very low levels of confidence and experience. A total of 65% of participants reported no experience with ocular US and musculoskeletal US. Likewise, confidence with procedural guidance was low and skewed toward traditional procedures (vascular access, paracentesis, thoracentesis), while 73% had no experience with using US for lumbar puncture and 52% had no experience with US‐guided nerve blocks. These can be targets of future training opportunities and workshops with live models.
In identifying perceived barriers to POCUS use, lack of equipment and education were the highest rated by a significant margin with 56% of respondents ranking them as “very important.” These results are similar to the findings of other surveys of US use in Vietnam and Kenya. 11 , 12 A survey performed in India of participants in a 4‐day US course in 2010 reported that 97% had “potential access” to an US machine in the near future, but this selection of participants at an emergency US course may not be representative of emergency physicians across India. 13 Lack of access to US equipment in India is problematic since in addition to the usual issues with acquiring hospital equipment (cost, institutional approval, etc.), the sale and import of US machines are tightly regulated by the Indian government, and once obtained they must be registered so that they can be tracked. This additional regulatory burden is pointed to by almost 70% of respondents rating legal concerns as moderately important to very important. As the pressures that led to this regulation have not disappeared, the rapidly increasing availability of handheld US and increasing demands for the use of US in emergency and critical care services will need to be balanced with the need to prevent misuse of this technology. Additional use of educational technology and in‐country training from affiliated hospitals will boost the training.
In addition, barriers related to hospital administration, other department interference, and malpractice concerns were rated as moderately important, important, or very important by over 50% of respondents. It remains to be seen whether these administrative issues will become even more significant when education and equipment shortages have been addressed. Given the high level of respondent interest in learning POCUS, the identified variations of training, comfort level, and experience across POCUS applications suggest the need for and likely success of increased training focused at closing competency gaps.
Limitations
We surveyed the residents and faculty affiliated with RRIEM MEM training programs in India regarding the use of POCUS in their practice environment to help design a curriculum to bridge gaps in competence. The overall response rate was 42%, and a smaller number of participants responded to each question, with variability in response rate across training program sites. This may result in a sampling bias, with respondents having a different perspective than other EM physicians.
In addition, there are other postgraduate training program options in EM in India, including MD programs, Diplomate of National Board (DNB) programs, other international training partnerships, and other local options. In 2018, there were 194 positions in the MD and DNB programs, although 52 positions went unfilled. 14 The total number of training positions in other EM programs is less clear. The RRIEM MEM programs represent a substantial portion of EM trainees in India, and the survey reached twice as many EM physicians affiliated with training programs as are in the MD and DNB programs. However, as this study surveyed only physicians related to our institution’s partnership programs, it may not represent the environment at other training programs. Although this may limit generalizability, there still was significant representation across training sites and geographic regions of India.
The Pre‐Conception and Pre‐Natal Diagnostic Techniques Act impacts the use of US to a significant, although variable, degree across the country. Regions with higher percentages of male births tend to have stricter enforcement of the Act, and access to US equipment is therefore more difficult. In addition, even those sites with more ready access to POCUS machines tend to defer imaging of pregnant women to radiology or obstetrics and gynecology services. This is reflected in this survey by respondents’ decreased level of interest in, and comfort with, obstetric US. While this is not necessarily a limitation of the survey directly, the cultural and legal implications of obstetric US will require special consideration during curriculum development. Finally, the majority of the respondents were residents, which may reflect the relative lack of core faculty in India compared to North American institutions, but may also impact the results of the survey because of the relatively novice perspective of the respondents.
Conclusions
This cross‐sectional survey of residents and faculty in Masters in Emergency Medicine programs across India illustrates current exposure, training, comfort, experience, and interest in point‐of‐care ultrasound across relevant applications to emergency medicine. Barriers to increasing use of point‐of‐care ultrasound include access to equipment and training and opposition from administration and other specialties. Future point‐of‐care ultrasound training should be tailored to the unique and diverse practice environments across India, with consideration for the health care system as a whole, its patterns of disease, and cultural concerns. Clinicians and educators will need to work with policy makers to modify regulations to improve access to ultrasound in emergency and critical care settings, while maintaining a foundation of safe, competent, and ethical use of point‐of‐care ultrasound.
Supporting information
Data Supplement S1. Full survey.
AEM Education and Training 2020;4:387–394
The authors have no relevant financial information or potential conflicts to disclose.
Author contributions: KSB contributed to the study concept and design; KSB, AD, MP, FM, SM, VP, HS, and KD contributed to the acquisition of the data; KSB, AD, MP, and HS contributed to the analysis and interpretation of the data; KSB, AD, MP, FM, SM, VP, HS, and KD contributed to the drafting of the manuscript; KSB, AD, MP, FM, SM, VP, HS, and KD contributed to the critical revision of the manuscript for important intellectual content; and KSB and HS contributed to the statistical expertise.
References
- 1. Counselman FL, Babu K, Edens MA, et al. The 2016 Model of the Clinical Practice of Emergency Medicine. J Emerg Med 2017;52:846–9. [DOI] [PubMed] [Google Scholar]
- 2. Amini R, Adhikari S, Fiorello A. Ultrasound competency assessment in emergency medicine residency programs. Acad Emerg Med 2014;21:799–801. [DOI] [PubMed] [Google Scholar]
- 3. Shah SP, Shah SP, Fiels‐Aime R, et al. Focused cardiopulmonary ultrasound for assessment of dyspnea in a resource‐limited setting. Crit Ultrasound J 2016;8:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Tafoya CA, Tafoya MJ, Osei‐Ampofo M, Oteng RA, Becker TK. Sustainable resuscitation ultrasound education in a low‐resource environment: the Kumasi experience. J Emerg Med 2017; 52:723–30. [DOI] [PubMed] [Google Scholar]
- 5. Boniface KS, Raymond A, Fleming K, et al. The Global Health Service Partnership's point‐of‐care ultrasound initiatives in Malawi, Tanzania and Uganda. Am J Emerg Med 2019;37:777–9. [DOI] [PubMed] [Google Scholar]
- 6. Shokoohi H, Raymond A, Fleming K, et al. Assessment of point‐of‐care ultrasound training for clinical educators in Malawi, Tanzania and Uganda. Ultrasound Med Biol 2019;45:1351–7. [DOI] [PubMed] [Google Scholar]
- 7. Tabaie S. Stopping female feticide in India: the failure and unintended consequence of ultrasound restriction. J Glob Health 2017;7:010304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Douglass K, Pousson A, Gidwani S, Smith J. Postgraduate emergency medicine training in India: an educational partnership with the private sector. J Emerg Med 2015;49:746–54. [DOI] [PubMed] [Google Scholar]
- 9. Thomas VK, Abraham SV, Balakrishnan JM, Krishnan SV, Amalakat A, Palatty BU. Point‐of‐care ultrasound training in Indian emergency medicine programs: a resident’s perspective. Int J Acad Med 2017;3:263–7. [Google Scholar]
- 10. Ultrasound Guidelines: Emergency, Point‐of‐Care and Clinical Ultrasound Guidelines in Medicine. Ann Emerg Med 2017;69:e27–e54. [DOI] [PubMed] [Google Scholar]
- 11. Rice BT, Vu H, Tran LD, Vo QX, Mowafi H. Survey of point of care ultrasound usage in emergency medicine by Vietnamese physicians. Emerg Med Australas 2015;27:580–3. [DOI] [PubMed] [Google Scholar]
- 12. Zaver F, Boniface K, Wachira B, Wanjiku G, Shokoohi H. International scope of emergency ultrasound: barriers in applying ultrasound to guide central line placement by providers in Nairobi, Kenya. Emerg Med Int 2018; 732846:1–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gupta A, Peckler B, Stone MB, et al. Evaluating emergency ultrasound training in India. J Emerg Trauma Shock 2010;3:115–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Douglass K, Gidwani S, Mehta S, et al.White Paper on Emergency Education and Training in India: Where Are We Now and Where Should We Go Next? Available at: https://smhs.gwu.edu/reaganinstitute/sites/reaganinstitute/files/White%20paper-Emergency%20Medicine%20Education%20and%20Training%20in%20India.pdf. Accessed February 11, 2019.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Supplement S1. Full survey.


