Abstract:
On February 8, 2020, Singapore raised its Disease Outbreak Response System Condition (DORSCON) level to Orange, indicating that coronavirus 2019 (COVID-19) was a severe disease with high human transmissibility. Using lessons learned from the severe acute respiratory syndrome (SARS) outbreak in 2003, the orthopaedic surgery department at Singapore General Hospital, a tertiary-level referral center, was prepared to handle this pandemic through business-continuity planning. The business that we are referring to is the “business” of orthopaedic surgery, encompassing clinical care, education, research, and administration. There is a lack of literature detailing business-continuity plans of surgical departments during pandemics, with new guidelines being developed. A large proportion of orthopaedic work, such as cases of fracture and infection, cannot be postponed. Even elective surgeries cannot be postponed indefinitely as it could result in detriment to the quality of life of patients. The aim of this article is to detail the business-continuity plans at our institution that allowed the delivery of essential musculoskeletal care through personnel segregation measures during the COVID-19 pandemic. Strategies to ensure the provision of timely medical intelligence, the reduction of nonessential ambulatory visits and surgical procedures, ensuring the safety and morale of staff, and continuing education and research efforts were paramount. As the COVID-19 pandemic unfolds, our posture needs to constantly evolve to meet new challenges that may come our way. Our existing business-continuity plan is not perfect and may not be applicable to smaller hospitals. There is conflict between envisioned normalcy, remaining economically viable as an orthopaedic department, and fulfilling training requirements, and educating the next generation of orthopaedic surgeons on the one hand and the need for segregation, workload reduction, virtual education, and social distancing on the other. Orthopaedic surgeons need to strike a balance between business continuity and adopting sustainable precautions against COVID-19. We hope that our experience will aid other orthopaedic surgery departments in adapting to this new norm, protecting their staff and patients, managing staff morale, and allowing the continuation of musculoskeletal care during the COVID-19 pandemic.
On December 31, 2019, an unexplained, severe viral pneumonia affecting young patients was reported in Hubei, People’s Republic of China1. This was the beginning of a new pandemic, coronavirus disease 2019 (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)2. There were an estimated 1,844,863 cases and 117,021 deaths in >150 countries as of April 14, 2020, with the World Health Organization (WHO) declaring a pandemic on March 11, 20203.
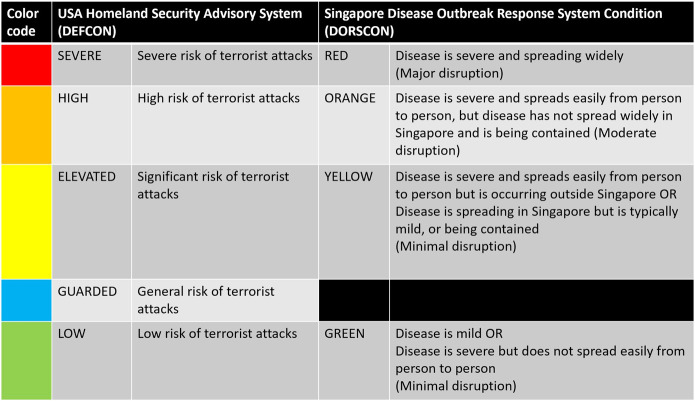
In Singapore, the first COVID-19 patient diagnosis took place on January 23, 2020, which led to the elevation of the Disease Outbreak Response System Condition (DORSCON) level from Green to Yellow. Singapore DORSCON levels for infectious-disease outbreaks are akin to U.S. DEFCON (defense readiness condition) states for terrorism, indicating severity and spread of the disease in Singapore (Fig. 1). Within 2 weeks, community transmission had occurred within Singapore. This was despite enhanced border screening measures geared toward the prevention of further importation of the virus, strong surveillance systems that enabled prompt contact tracing, and quarantining and social distancing by citizens to curb the spread of the virus4.
Fig. 1.
U.S. DEFCON versus Singapore DORSCON levels.
On February 8, 2020, Singapore raised its DORSCON level to Orange, indicating that COVID-19 was a severe disease that can spread easily from person to person (Fig. 1). Prior to this, in 2003, the SARS epidemic led to a high mortality rate of 14% (33 of 238) in Singapore, predominantly among health-care workers. Singapore has since strengthened its response plans for infectious disease outbreaks5. Therefore, within the department of orthopaedic surgery at our institution, the leadership was particularly mindful and placed strong emphasis on staff and patient safety as we developed our pandemic response plans.
Orthopaedic surgery is an essential service at Singapore General Hospital (SGH), a tertiary-level referral center providing high-quality musculoskeletal care. The department has 40 orthopaedic consultants who attend to 126,000 outpatient visits and perform 8,600 surgeries annually. A large proportion of our work, such as the treatment of musculoskeletal trauma and infections, cannot be postponed. Even elective surgeries cannot be postponed indefinitely, as it could result in detriment to the quality of life of patients who need it. If COVID-19 leads to staff attrition, external orthopaedic departments will have to be activated to provide these essential services. There is a lack of literature detailing business-continuity plans of surgical departments during pandemics, with new guidelines being developed for U.S. and U.K. orthopaedic surgical departments6,7. Using lessons learned from SARS, our department was prepared to handle this pandemic through business-continuity planning8. The business that we are referring to is the “business” of orthopaedic surgery, encompassing clinical care, education, research, and administration. The aim of this article is to detail the business-continuity plans at our institution that allowed the delivery of essential musculoskeletal care through personnel-segregation measures during the COVID-19 pandemic.
Business-Continuity Plan
In the 2 weeks prior to DORSCON level Orange status, attending surgeons reviewed and postponed all nonurgent elective surgery and reduced outpatient clinic visits from approximately 500 per day to 250 per day (a 50% reduction). These measures were put in place to free hospital beds in anticipation of the surge in patients with COVID-19. The leadership team provided timely medical intelligence updates to the department and began contingency planning using the principles of business continuity, maintenance of adequate staffing, provision of musculoskeletal subspecialty care, and personnel segregation. The contingency plan was activated on February 8, 2020, when Singapore raised its DORSCON level to Orange.
Provision of Timely Medical Intelligence
The difference between the SARS and COVID-19 outbreaks was the speed of information dissemination, which was more rapid for the latter. The provision of timely, accurate medical intelligence is crucial to preventing panic9. Rapid, timely dissemination of accurate and important information through secured/encrypted instant-messaging platforms allowed the entire department to remain connected at all times. The Ministry of Health further facilitated this by disseminating important COVID-19 information to physicians through emails and secured/encrypted chat groups formed by medical school classes of different years.
For our department, the first step was to ensure that all staff were included in the chat group. The chat group provided a platform for sharing the latest COVID-19 literature and for the dissemination of daily routine instructions by the hospital outbreak-control task force and department-related administrative instructions. The chat group also allowed the sharing of COVID-19-related humor, which sometimes “took the edge off” during these stressful times.
Personnel Management
Staffing
In order to ensure adequate personnel to deal with the COVID-19 pandemic, the hospital cancelled all local and overseas leave of all health-care workers. All local orthopaedic-related meetings, workshops, and conferences were cancelled or postponed indefinitely. Members of the orthopaedic leadership continued their clinical roles to promote solidarity within the department, leading by example. As a large department with 105 medical staff, we transferred personnel to augment frontline emergency department and other musculoskeletal departments while maintaining self-sufficiency. In addition, a mandatory 14-day leave of absence/stay-home notice/quarantine order was given to staff returning from affected areas in February 2020, including mainland China (the whole country) and Daegu city, Cheongdo county, South Korea. These measures prevented cross-institutional spread as well as importation of the virus.
Personal Protection
Ensuring the protection of all staff from COVID-19 was of the utmost importance10. Thermometers were provided for all staff, which ensured a high compliance rate with twice-daily temperature reporting and early detection of infection. Although fever and respiratory symptoms are the most common symptoms of COVID-19, it has been recognized that asymptomatic carrier transmission ocurrs11, and body temperature measurement will not detect all cases. All staff were encouraged to obtain their influenza vaccination. All staff were previously trained in donning personal protective equipment (PPE) and attended N95 mask fittings and powered air-purifying respirator (PAPR) training as indicated (for example, for pregnant staff members, for whom N95 use may be unsuitable). Easily accessible training videos and refresher videos were also made available for staff regarding the proper procedure for donning PPE.
Our department proactively procured surgical masks, N95 masks, and goggles for all doctors, and doctors donned appropriate PPE in accordance with our hospital guidelines. For example, when reviewing high-risk patients, doctors would don the N95 mask, goggles, gown, and gloves and dispose of them after examining the patient. Surgeons were required to don an N95 mask, a face shield, a gown, and gloves when operating on high-risk patients. Of note, PAPR was not routinely required during orthopaedic procedures, as there was no risk of aerosolization of respiratory secretions. To our knowledge, there is currently no good evidence that the use of power tools, such as high-speed burrs, drills, or saws, results in the aerosolization of SARS-CoV-2 viral particles from patients with COVID-1912. Regardless, we would propose the use of at least an N95 mask, face shield, gown, and gloves or PAPR when operating on high-risk patients, as more research is required to determine the transmissibility of SARS-CoV-2 in an operative theater setting.
Social Distancing and Morale
Social distancing measures were strictly practiced within the department, with frequent reminders to staff to avoid congregating in large groups. As orthopaedic surgeons, we have a gregarious nature and tend to congregate. Being unable to do so adversely affected morale. The orthopaedic leadership was constantly aware of the sentiment and placed strong emphasis on morale management, including fortitude and resilience initiatives. Senior hospital leadership provided daily, transparent updates on the evolving situation and words of encouragement. Senior orthopaedic surgeons provided care and concern for all staff members, showing appreciation and recognition for staff during these times of crisis. There was also a focus on ensuring equality between all individuals with regard to workload, remuneration, and personal aspirations. Special attention was accorded to staff with specific concerns, e.g., pregnancy or living with young children or elderly parents. Although hospital policy mandated the cancellation of leave for all staff, the orthopaedic leadership kept a close eye on global developments, assessing personnel requirements in relation to staff morale, and approved leave in a responsible manner, bearing in mind exigencies of service and recall of doctors when necessary.
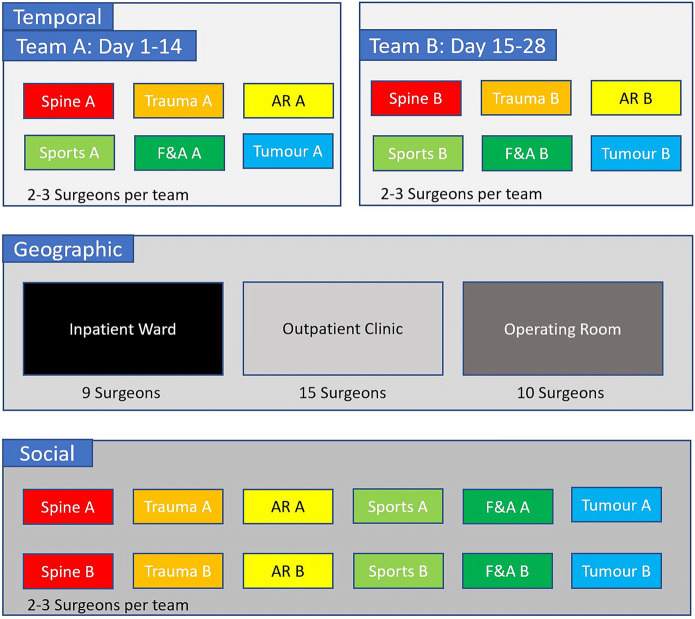
Personnel Management: Geographic and Social Segregation
Three models of personnel segregation were considered: temporal, geographic, and social (Fig. 2). In 2003, our department adopted the temporal segregation model for the SARS outbreak, dividing the department into 2 teams. Each team was on duty for 14 days consecutively, followed by 14 days off work, which allowed staff to be away from work for longer than the SARS incubation period. This model had the advantages of having an active team providing essential services for 14 days, physically separated from the passive team, which served as a back-up team in case of attrition, and allowed a 14-day wash-out period when the active team took its off-days. The disadvantage was that each team had half the personnel but had to perform all aspects of musculoskeletal care with fewer personnel, although this was mitigated by the reduced patient load due to the outbreak.
Fig. 2.
Temporal, geographic, and social segregation models. Subspecialty personnel were divided into Team A and Team B in the temporal and social segregation models. The geographic model includes 3 work zones: inpatient ward, outpatient clinic, and operating room. F&A = foot and ankle, and AR = adult reconstruction.
However, because of the operational requirements mandating that all staff had to be in-hospital to augment the COVID-19 crisis response, the leadership developed a business-continuity plan based on geographic and social segregation. This plan consisted of teams who would function from 3 geographically distinct locales, namely, the outpatient clinic, the operating room (OR), and the inpatient ward. Each team was scaled to perform assigned tasks within their respective sectors. The teams maintained close communication with the other teams, allowing the department to function as a cohesive unit. This model was activated on Monday, February 10, 2020, providing maximum segregation and minimal normalcy.
Ambulatory Care/Outpatient Clinic
The ambulatory care (outpatient clinic) team evaluated patients referred for surgical intervention, postoperative follow-up, and infective, traumatic, and complex musculoskeletal conditions. Our department has approximately 126,000 ambulatory care/outpatient clinic visits per year referred from the SGH emergency department, primary care, and private clinics. In addition, Singapore, being the medical hub of the region, frequently receives patients from Southeast Asia as well as mainland China. The ambulatory care team prevented potential COVID-19 clusters by employing a multipronged strategy:
(1) Reduction of outpatient visits with prioritization of urgent cases over elective cases, achieving a halving of workload.
With the identification of positive cases in Singapore, we worked on the presumption that spread of the infection would occur and started to reduce nonurgent outpatient visits. This decreased patient crowding in the waiting area, reducing exposure to patients and those accompanying them to potentially infected individuals. The reduced outpatient load prevented the system from being overwhelmed and inadvertent lapses in safe practices, while allowing the continued availability of essential musculoskeletal care for patients with urgent orthopaedic conditions.
In collaboration with a core team of clinic executives, anticipated patient attendances scheduled for the successive 2 weeks were emailed to respective surgeons. Surgeons would screen the list and postpone nonurgent appointments. A team of clinic assistants inform these patients, via telephone and letters. Memos, prescription refills, and notes for extending patient medical leave were provided by a doctor rostered for administrative duties, sparing the patient a visit to the clinic. Functional assessments were also performed over the telephone.
(2) Effective screening of patients, PPE requirements, and isolation protocols.
Patients and all accompanying persons presenting to the outpatient clinic were routinely screened for coryzal symptoms, fever, and travel history, as stipulated by national guidelines set by the Ministry of Health. Patients with coryzal symptoms were given a mask. Patients with a notable travel history and coryzal symptoms were immediately directed to a designated isolation room to be assessed by staff in PPE. In view of the possibility of asymptomatic transmission, asymptomatic patients with notable travel history were also assessed by staff in PPE. PPE used at the outpatient clinic to assess suspected COVID-19 cases included N95 masks, goggles, face shields, protective gowns, and gloves. The need for admission or further assessment was discussed with an infectious disease physician whenever required, especially for patients fulfilling the suspected case definition. Patients with suspected COVID-19 who required orthopaedic inpatient care were handed over to the inpatient ward team, with the patients admitted to an isolation ward.
Attention to safety and personal protective precautions is critical, as it has been shown to ease the psychological burden experienced by health-care personnel, who may worry about contracting the disease while on duty10. In addition, these measures prevented the spread of disease in the waiting area and protected other health-care workers within the clinic. In general, high-risk patients with urgent orthopaedic conditions such as wound management needs, fractures, or conditions requiring inpatient admission had to be reviewed. High-risk patients with nonurgent conditions were rescheduled to 2 business weeks later, which is beyond the incubation period of 14 days.
(3) Outpatient clinic team sub-segregation.
The outpatient clinic team was subdivided into 6 smaller teams, consisting of attending surgeons, residents, and medical officers. Three active teams capable of providing full-spectrum orthopaedic specialty consults were rostered for clinical duty, while the other 3 teams performed administrative, nonclinical duties as the passive/stand-by team. Doctors were strictly prohibited from socializing or having meals or meetings with individuals from the other teams and practiced strict social distancing measures. Further geographic segregation was performed, with the teams working from separate outpatient clinic locales within the hospital, minimizing contact between physicians on different teams.
(4) Leveraging advanced technology.
Virtual consults, “triage from home,” and direct-to-consumer telemedicine are effective in screening patients, promoting self-quarantine in milder cases of COVID-19, and minimizing risk to patients, the community, and providers13. During this pandemic, our clinics have performed telemedicine consults to reduce outpatient clinic visits. It allows our physicians to obtain information regarding the presenting orthopaedic concern as well as COVID-19-related travel and exposure history. In the future, dedicated telemedicine office spaces or in-car “drive-through” testing could be developed, and future investments in telemedicine are well warranted in this regard.
Operating Room
OR teams had a full complement of orthopaedic subspecialty surgeons who were equipped to handle full-spectrum musculoskeletal care. As there were no elective surgeries during this period, 3 teams, namely 2 acute-care teams and 1 spine team, were established. The 3 teams were assigned to 3 designated ORs, physically separated from each other, providing a total of 15 full-day operative sessions per week. In addition, staff from different teams/ORs wore distinct headgear to minimize interaction within the OR. The OR teams worked closely with anesthesiologists who developed outbreak response measures for the OR complex14.
The acute-care teams were able to manage complex pelvic trauma, foot and ankle trauma, musculoskeletal tumor-related emergencies, periprosthetic trauma, and infection. The spine team managed spine-related emergencies, including spinal trauma, infection, tumor, and cord compression. As the operating team was not allowed to visit the wards, close communication between operating room staff and inpatient ward staff ensured seamless perioperative care for patients requiring urgent surgery during this period.
Inpatient Ward
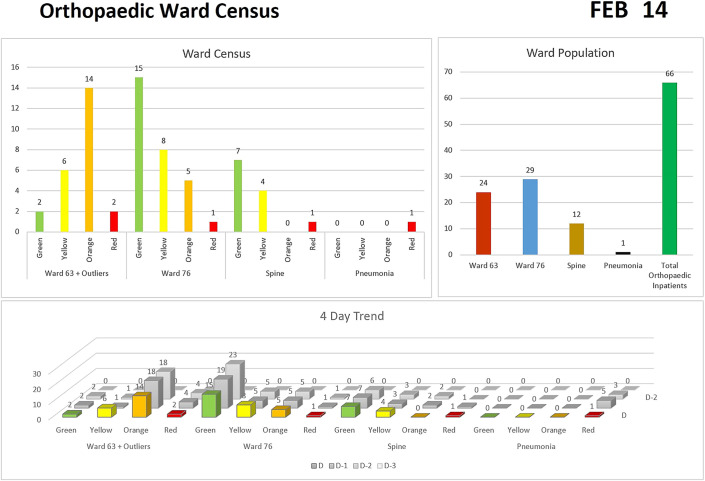
The inpatient ward team was tasked to take over the cases of all existing inpatients who were previously under the care of different surgeons. Prior to the planned implementation on February 10, 2020, primary teams prepared summaries for the new attending surgeons who would be looking after these patients. The inpatient ward team was divided into smaller teams, managing sectors within different wards. Trauma and spine patients were in 1 ward (Ward 76 on Figure 3), while acute-care patients and those with musculoskeletal infection were located in another ward (Ward 63). In addition, the team treating the acute-care patients and those with musculoskeletal infection also took care of orthopaedic patients with fever, respiratory symptoms, and pneumonia and patients in whom COVID-19 was suspected, who were housed in dedicated COVID-19 wards. COVID-19-positive patients were placed in isolation rooms and only reviewed after de-isolation, unless there was a limb-threatening emergency. This arrangement enabled continuity of care, as the same physicians reviewed the same patients daily within their sectors.
Fig. 3.
Sample daily orthopaedic inpatient ward census used to track inpatient load and the number of suspected and confirmed COVID-19 cases (in red). Green = stable patients awaiting discharge, yellow = preoperative, orange = preoperative cases requiring further optimization before surgery.
New admissions, patients in the high-dependency ward, and intensive care unit patients were reviewed by attending surgeons daily. Advanced practice care nurses provided specialty wound care, allowing for negative pressure dressings to be applied in the ward instead of in the ORs. This allowed many patients to be discharged to home early with these dressings. In addition, the inpatient ward team worked closely with infectious disease and plastic surgery colleagues, allowing robust multidisciplinary care of complex cases, such as those involving severe limb infection or open fracture with soft-tissue loss.
A ward census presented a daily operational picture, providing useful information regarding the number of preoperative cases (yellow) and orthopaedic patients in whom COVID-19 was suspected or confirmed (red) (Fig. 3). Daily coordination meetings were held to allow ward sectors to present complex cases for discussion in a multi-subspecialty conference. The OR team was simultaneously informed regarding the indication for surgery and would prepare for the case. Close communication between OR team surgeons and the inpatient ward team attending surgeons ensured continuity of care for all patients, including weight-bearing status, assessment of thromboprophylaxis need, and the management of drains postoperatively. The lack of inpatient deaths during this period is a testament to the holistic management provided by the ward team.
Night duty was performed by the same team members in each ward to minimize cross-interaction between ward teams. Patients with acute orthopaedic conditions who arrived in the ward on the weekend (Friday to Sunday) requiring urgent surgery were operated on by attending surgeons from the inpatient ward team. As the ward team was the only team performing night duties, morale was most affected in this team. All subsectors allowed time off for staff, keeping skeletal crews after mid-day to prevent burn-out and manage morale.
Management of Close Contact with COVID-19-Positive Patients
On February 14, 2020, 4 days after our department employed its business-continuity contingency plan, an anesthesiologist who was a close contact of 2 doctors within our department was diagnosed as COVID-19-positive. One of them, Dr. A., was symptomatic and was isolated immediately. The other, Dr. B., was asymptomatic and was given a home-quarantine order. Both tested negative for the virus. Close contacts of the 2 doctors were closely monitored as they were considered second-degree contacts who did not require further tests. In addition, all staff had been compliant with the use of a surgical face mask and appropriate PPE while in-hospital.
In another incident, on March 2, 2020, 4 patients admitted to orthopaedic surgery were deemed to be close contacts with a COVID-19-positive patient while awaiting disposition in the emergency department. Of the 4 patients, only 1 had respiratory symptoms and subsequently tested negative. The remaining 3 patients were put on home quarantine upon discharge. All staff who reviewed or operated on the patients were alerted and closely monitored for symptoms.
Fortunately, none of the health-care workers who were in close contact with Dr. A., Dr. B., or the 4 above-mentioned patients contracted the virus. These incidents were managed by our department’s infection-prevention liaison officer (IPLO), who worked closely with the infection prevention and epidemiology (IPE) unit and hospital epidemiology team. The IPLO provided medical advice for staff who were potentially exposed to COVID-19-positive contacts, ensuring quick follow-up actions by these individuals. These incidents suggest that universal precautions and face mask and PPE compliance minimize the risk of COVID-19 spread. In addition, even if colleagues of these close contacts had been infected, the personnel segregation would have allowed business continuity.
Auxiliary Departmental Activities
Many auxiliary departmental activities were affected by the COVID-19 pandemic. New staff, including medical students, medical officers, overseas visitors, and fellows were prohibited from joining the department. Research activities involving patient recall were suspended indefinitely. Departmental meetings, including preoperative audit rounds, mortality and morbidity rounds, journal clubs, subspecialty education rounds, and research meetings, were cancelled. These meetings were subsequently restarted with the aid of a teleconference app, which allowed screen-sharing and live interaction, enabling >100 staff to actively participate on a virtual platform. The leadership team also conducted weekly teleconference meetings allowing us to plan, coordinate, and review processes within each of the teams.
The Way Ahead
As the COVID-19 pandemic unfolds, our posture needs to constantly evolve to meet new challenges that may come our way. Our existing business-continuity plan is not perfect and may not be applicable to smaller hospitals. It is far from what we consider normalcy. There is conflict between the envisioned return to normal activity, remaining economically viable as an orthopaedic department, fulfilling training requirements, and educating the next generation of orthopaedic surgeons on the one hand and the need for segregation, workload reduction, virtual education, and social distancing on the other.
As orthopaedic surgeons, we need to strike a balance between business continuity and adopting sustainable precautions against COVID-19. We believe that our orthopaedic department, having the experience and resilience of dealing with previous pandemics, will be able to return to a “new” normalcy while protecting our staff and our patients. We hope that our experience will aid other orthopaedic surgery departments in adapting to this new norm, protecting their staff and patients, managing staff morale, and allowing the continuation of musculoskeletal care during the COVID-19 pandemic.
Footnotes
Investigation performed at the Department of Orthopaedic Surgery, Singapore General Hospital, Singapore
Disclosure: The authors indicated that no external funding was received for any aspect of this work. The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJSOA/A167).
References
- 1.Paules CI, Marston HD, Fauci AS. Coronavirus infections-more than just the common cold. JAMA. 2020. January 23. Epub 2020 Jan 23. [DOI] [PubMed] [Google Scholar]
- 2.Adalja AA, Toner E, Inglesby TV. Priorities for the US health community responding to COVID-19. JAMA. 2020. March 3. Epub 2020 Mar 3. [DOI] [PubMed] [Google Scholar]
- 3.Mahase E. Covid-19: WHO declares pandemic because of “alarming levels” of spread, severity, and inaction. BMJ. 2020. March 12;368:m1036. [DOI] [PubMed] [Google Scholar]
- 4.Wong JEL, Leo YS, Tan CC. COVID-19 in Singapore-current experience: critical global issues that require attention and action. JAMA. 2020. February 20. Epub 2020 Feb 20. [DOI] [PubMed] [Google Scholar]
- 5.Wilder-Smith A, Chiew CJ, Lee VJ. Can we contain the COVID-19 outbreak with the same measures as for SARS? Lancet Infect Dis. 2020. March 5:S1473-3099(20)30129-8. Epub 2020 Mar 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.American College of Surgeons. COVID-19: recommendations for management of elective surgical procedures. Accessed 2020 Mar 18. https://www.facs.org/about-acs/covid-19/information-for-surgeons
- 7.British Orthopaedic Association. Information for BOA members on trauma and orthopaedic care in the UK during coronavirus pandemic. Accessed 2020 Mar 18. https://www.boa.ac.uk/resources/statement-for-boa-members-on-trauma-and-orthopaedic-care-in-the-uk-during-coronavirus-pandemic.html
- 8.Fadel M, Salomon J, Descatha A. Coronavirus outbreak: the role of companies in preparedness and responses. Lancet Public Health. 2020. April;5(4):e193. Epub 2020 Feb 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, Rubin GJ. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020. March 14;395(10227):912-20. Epub 2020 Feb 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Adams JG, Walls RM. Supporting the health care workforce during the COVID-19 global epidemic. JAMA. 2020. March 12. Epub 2020 Mar 12. [DOI] [PubMed] [Google Scholar]
- 11.Bai Y, Yao L, Wei T, Tian F, Jin DY, Chen L, Wang M. Presumed asymptomatic carrier transmission of COVID-19. JAMA. 2020. February 21. Epub 2020 Feb 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang W, Xu Y, Gao R, Lu R, Han K, Wu G, Tan W. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA. 2020. March 11. Epub 2020 Mar 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hollander JE, Carr BG. Virtually perfect? Telemedicine for COVID-19. N Engl J Med. 2020. March 11. Epub 2020 Mar 11. [DOI] [PubMed] [Google Scholar]
- 14.Wong J, Goh QY, Tan Z, Lie SA, Tay YC, Ng SY, Soh CR. Preparing for a COVID-19 pandemic: a review of operating room outbreak response measures in a large tertiary hospital in Singapore. Can J Anaesth. 2020. March 11. Epub 2020 Mar 11. [DOI] [PMC free article] [PubMed] [Google Scholar]