Abstract
This study aimed to evaluate the onset characteristics of patients with uremia undergoing maintenance hemodialysis complicated with COVID-19, so as to improve the understanding, diagnosis, and treatment.
26 cases were confirmed cases of COVID-19. Confirmed patients with COVID-19 undergoing maintenance hemodialysis in the blood purification center were recruited. The general data of patients, including age, sex, duration of dialysis, and basic diseases, were analyzed. The clinical features included fever, respiratory symptoms, and gastrointestinal symptoms. The items for laboratory tests included blood routine examination, liver function, C-reactive protein, procalcitonin, creatine kinase, creatine kinase-MB, markers of myocardial injury, B-type natriuretic peptide, D-dimer, and so forth. The imaging examinations referred mainly to computed tomography imaging findings of the lungs.
Twenty-one cases were complicated with chronic basic diseases, such as hypertension or diabetes. In terms of clinical manifestations, 13 cases had fever, which was close to the number of cases without fever (13 cases). The respiratory symptoms included dry cough (19 cases), shortness of breath (9 cases), fatigue (11 cases), and so forth. Further, 15 patients had hypoxemia, indicating more severe patients. Sore throat (2 cases) was not significant, and a few patients reported gastrointestinal symptoms (3 cases). The results of blood routine examination showed decreased absolute lymphocyte count (0.7 ± 0.4 × 10∼9/L), lower hemoglobin level (105.2 ± 20 g/L), and normal absolute neutrophil count 4.2 (3.0, 5.9) × 10∼9/L. Of the inflammatory indexes, procalcitonin was 0.69 (0.24, 2.73) ng/mL; C reactive protein was 17.2 (5.2, 181.6) mg/L, which was higher than normal. Blood biochemistry revealed lower albumin level (38.0 ± 4.0 g/L) and higher troponin 0.11(0.035, 6.658) ng/mL and myoglobin levels (538.5 ± 240.5 ng/mL), suggesting myocardial injury.
The patients with uremia and confirmed COVID-19 undergoing maintenance hemodialysis are more common in males. Although the proportion of fever patients is 50%, the proportion of hypoxemia patients is high (58%). With poor cardiac function. They were prone to respiratory failure complicated with heart failure. According to the onset characteristics of this population, early diagnosis and treatment could help reduce the risk of developing a critical illness and control the spread of the COVID-19 epidemic.
Keywords: COVID-19, hemodialysis, onset characteristics
1. Introduction
Since December 2019, multiple cases of novel coronavirus pneumonia have been reported in Wuhan, Hubei Province. The disease has spread to many provinces in China and some foreign countries, such as Japan, Thailand, the United States, and Europe in a short time with strong infectivity.[1] The International Committee on Taxonomy of Viruses named the novel coronavirus “SARS-CoV-2” based on systematics, taxonomy, and conventions. The National Health Commission of the People's Republic of China temporarily named it as novel coronavirus pneumonia.[2] The Chinese Center for Disease Control and Prevention announced the inclusion of this disease in the national “Category B” infectious disease, and the prevention and control measures for “Category A” infectious diseases were taken.[3] World Health Organization officially named it as COVID-19 on February 11, 2020. As of March 4, 2020, approximately 80,424 confirmed COVID-19 cases were reported across the country. About 520 suspected cases and 2984 deaths have been reported to date; Approximately 49,540 confirmed cases and 2282 deaths were reported in Wuhan, Hubei Province. On March 5, 2020, China released the Diagnosis and Treatment Scheme of New Coronavirus Pneumonia (trial version 7),[4] which proposed that the current diagnostic criteria for COVID-19 included 2 types of cases: suspected and confirmed, with some differences between the 2.
Patients with uremia undergoing maintenance hemodialysis are a special type of population in this epidemic. These patients need to commute between hospitals and home continuously and frequently. At the same time, their body immunity is low because of the diseases. Thus, this patient population is at a high risk of COVID-19. This study analyzed the clinical characteristics of some patients with COVID-19 undergoing maintenance hemodialysis since Tongren Hospital (Wuhan Third Hospital), Wuhan University School of Medicine became designated hospital for dialysis patients. Through a literature review, the study aimed to improve awareness of this disease and enhance understanding, diagnosis, and treatment of patients undergoing hemodialysis in the epidemic.
2. Methods and participants
The study protocol was approved by the Ethics Committees of the Wuhan Third Hospital, Tongren Hospital of Wuhan University, Wuhan (No. KY2020-023), and all participants provided written informed consent. We screened 350 patients with maintenance hemodialysis since Wuhan Third Hospital became designated hospital and divided them into nucleic acid positive group and negative group according to the results of fluorescence Reverse Transcription-Polymerase Chain Reaction detection of pharynx swabs. There are 26 cases in the nucleic acid positive group.
2.1. Inclusion criteria
The patients undergoing hemodialysis in the hospital, who met the diagnostic criteria for COVID-19, were included. The diagnostic criteria referred to the Diagnosis and Treatment Scheme of New Coronavirus Pneumonia (trial version 7) developed by the National Health Commission[4]:
Diagnostic criteria for suspected cases: A comprehensive analysis was conducted by combining the following epidemiological history and clinical features:
2.1.1. Epidemiological history
-
(1)
History of traveling to or living in Wuhan and its surrounding areas, or from other communities with case reports, within 14 days before the onset of illness.
-
(2)
History of contact with patients with COVID-19 (positive result of the nucleic acid test) within 14 days before the onset of illness.
-
(3)
History of exposure to patients with a fever or respiratory symptoms from Wuhan and its surrounding areas, or from communities with case reports, within 14 days before the onset of illness.
-
(4)
Cluster of cases (2 or more cases with a fever and/or respiratory symptoms in a small area, such as home, office, school classroom, and so forth within 2 weeks).
2.1.2. Clinical features
-
(1)
Fever and/or respiratory symptoms.
-
(2)
Imaging characteristics of COVID-19.
-
(3)
The total white blood cell count (WBC) was normal or decreased in the early stage of onset, and the lymphocyte count was normal or decreased.
Suspected cases had any 1 of the epidemiological history and any 2 of the clinical features. If no definite epidemiological history was found, 3 of the clinical features needed to be met.
Diagnostic criteria for confirmed cases: Suspected cases had one of the following etiological or serological findings:
-
(1)
The result of real-time fluorescent Reverse Transcription-Polymerase Chain Reaction test of COVID 19 nucleic acid was positive;
-
(2)
viral gene sequencing was highly homologous to known COVID 19; and
-
(3)
serum COVID 19-specific IgM and IgG antibodies were positive; serum COVID 19-specific IgM antibody changed from negative to positive or increased 4 times or more in the recovery phase than in the acute phase.
2.2. Outcome measures
2.2.1. General data
They included age, sex, duration of dialysis, and accompanying basic diseases, such as hypertension, diabetes, coronary heart disease, and heart failure (HF).
2.2.2. Clinical features
They included the presence or absence of fever (body temperature above 37.3°C), cough, panting, dyspnea, resting-finger oxygen saturation, and presence or absence of nausea, vomiting, diarrhea, and other gastrointestinal symptoms.
2.2.3. Laboratory tests
They included WBC count, neutrophil percentage (N%), lymphocyte percentage (L%) and absolute count (L), hemoglobin, and platelet count in the blood routine examination. The inflammatory markers included C-reactive protein and procalcitonin. The markers for myocardial injury included myoglobin and troponin; atrial natriuretic peptide (BNP); biochemical indicators including liver function, prealbumin, and so forth; and D-dimers and other indicators reflecting changes in patients’ conditions.
2.2.4. Imaging examinations
The computed tomography findings of patients’ lungs were mainly observed. According to the imaging pathological features, the ground-glass opacity, consolidation, stripe, nodular areas, and latticed shadows of images were observed, and the specific imaging features were analyzed.
2.3. Statistical analysis
IBM SPSS Statistics 23.0 software was used. The measurement data conforming to normal distribution were presented as mean ± standard deviation. Measurement data with non-normal distribution were presented as median (25th and 75th percentiles). The count data were expressed as a percentage.
3. Results
3.1. General data
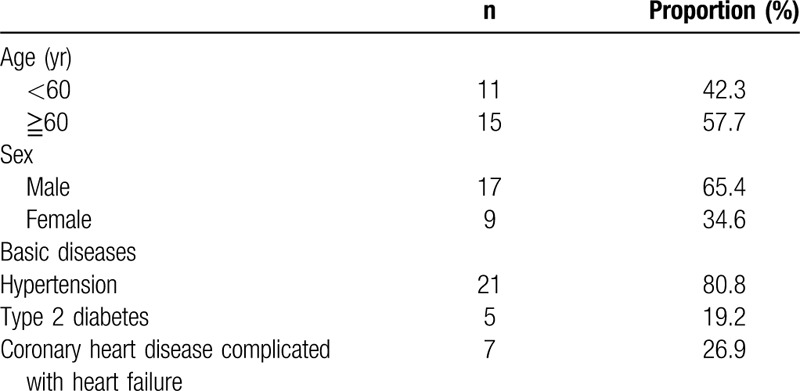
From January 25, 2020, monitoring of body temperature and computed tomography (CT) scan of the lungs were performed for each patient. For patients with abnormal pulmonary imaging, blood laboratory tests, and COVID 19 nucleic acid test were immediately performed. As of March 1, 2020, 26 patients were screened to meet the diagnostic criteria for COVID 19. A total of 26 patients (17 male and 9 female) undergoing hemodialysis were complicated with COVID 19; male patients were predominant. Further, 15 patients were aged more than 60 years and 11 were aged less than 60 years. The average duration of dialysis was 4.6 ± 3.5 years. At the same time, most patients were complicated with basic diseases, such as hypertension and diabetes, and some had developed chronic HF. The specific general data are shown in Table 1.
Table 1.
General data.
3.2. Clinical features
The clinical features are shown in Table 2. The patient was considered to have a fever if the body temperature exceeded 37.3°C. The table shows that among patients with uremia and COVID 19, the number of patients with a fever was similar to that of patients without a fever. Many patients still had no elevated temperature at the onset.
Table 2.
Clinical features of patients with uremia and NCP.
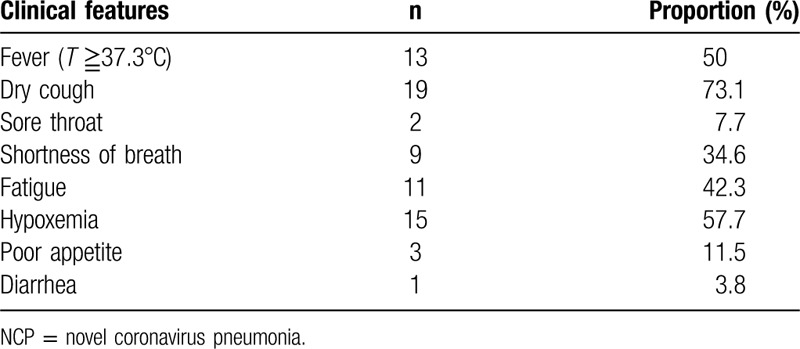
The main respiratory symptom of COVID 19 was dry cough; a few patients also had symptoms, such as nasal congestion, runny nose, and sore throat. Severe cases experienced shortness of breath, dyspnea, and hypoxemia, which were mainly manifested as follows: Respiratory rate ≥30 breaths/min; in resting state, finger oxygen saturation <93%; and arterial partial pressure of oxygen/fraction of inspiration O2 ≤300 mm Hg (1 mm Hg = 0.133 kPa).[4] In this study, the respiratory symptoms of patients with uremia and COVID 19 were cough, shortness of breath, and fatigue; sore throat was not obvious. Only a few patients had gastrointestinal symptoms, but careful attention was still needed when they had gastrointestinal symptoms. The assessment was made in time to determine whether patients were complicated with COVID 19.
3.3. Results of laboratory tests
The results of the blood routine examination are shown in Table 3. The mean WBC count showed no significant decrease. The mean lymphocyte count decreased, and no significant decrease in the neutrophil count was found, which were related to the patient's viral infection. The patient's mean hemoglobin level decreased slightly, which was considered to be related to long-term renal anemia in patients with uremia. The mean values of infection indicators increased; it was considered as viral infection and decreased immunity, increasing the risk of bacterial infection.
Table 3.
Statistics of laboratory tests of patients with uremia and NCP.
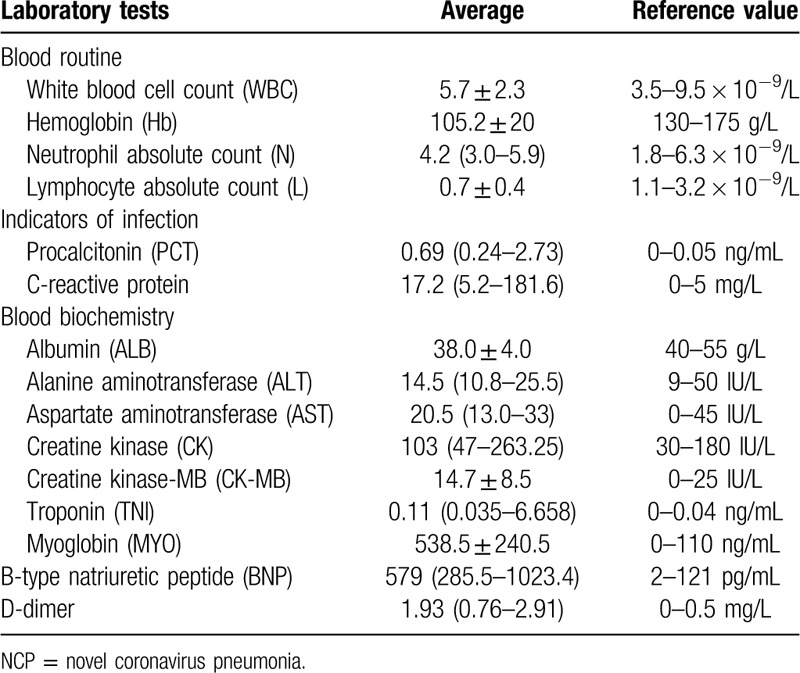
The biochemical and cardiac function indicators of the patients changed as follows. A mild decrease in albumin was observed. The average values of alanine transaminase and aspartate aminotransferase were in the normal range. No significant increase in the levels of myocardial enzymes was found. A mild increase in the levels of markers for myocardial injury was observed, suggesting the presence of myocardial injury. Increased BNP levels suggested a decrease in cardiac function. However, long-term volume overload in patients undergoing dialysis resulted in a long-term elevation in the level of this indicator. Elevated D-dimer levels suggested that patients were at risk of thrombosis.
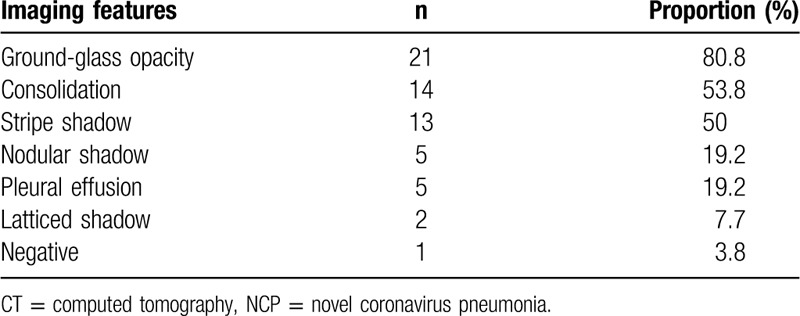
3.4. Results of imaging examinations
The CT imaging findings of patients’ lungs are shown in Table 4. The main lung imaging features were ground-glass opacity, consolidation, and stripe shadows. A few patients showed pleural effusion and latticed shadows. One patient had negative results in the imaging examination.
Table 4.
CT findings of the lungs in patients with uremia and NCP.
4. Discussion
Since December 2019, multiple cases of COVID 19 have been reported in Wuhan, Hubei Province. The geographical distribution of the initially infected population is closely related to the Wuhan Huanan Seafood Wholesale Market. The current population with onset clearly shows that the virus has a characteristic of human-to-human transmission.[5] At present, the source of infection of COVID 19 is mainly infected patients; however, asymptomatic infected persons may also carry the virus. The virus spreads mainly through respiratory droplets and also through direct or indirect contact, such as infection of the mouth, nose, and mucous membranes of eyes via hands. Aerosol transmission may occur in specific closed environments with high concentrations of viruses.[4]
During the entire epidemic, the focus was on patients with uremia undergoing maintenance hemodialysis. Such patients frequently go out and gather in hospitals to become a high-risk population for COVID 19 infection. In response to this situation, the Dialysis Center in the hospital provided education regarding the epidemic to each patient since January. The dialysis room was strictly disinfected daily. Each patient underwent lung CT examinations, and the body temperature, vital signs, and respiratory and gastrointestinal symptoms were closely monitored. Also, blood routine examination and viral nucleic acid test were performed. For suspected and confirmed cases, this center immediately contacted the community for referral, quarantine, observation, or hospitalization.
The incubation period for COVID 19 is 1 to 14 days.[4] Recent reports have identified patients with an incubation period of up to 24 days.[6] COVID 19 is more common in men (41.9%–75.0%), with an average age of 47.0 to 55.5 years; 51% to 55% of patients have basic diseases.[5–9] The symptoms of COVID 19 are variable, with fever being the most common (82.0%–98.6%), followed by cough (59.4%–82.0%), shortness of breath (31.0%), and myalgia or fatigue (11.0%–69.6%); expectoration is rare (28.0%). A small number of patients report a headache (8.0%) and disturbance of consciousness (9.0%). Hemoptysis and sore throat are present in 5.0% of patients. Further, 2.0% to 3.0% of patients are complicated with diarrhea, and 1.0% of patients have nausea and vomiting.[5–9] Patients with COVID 19 and a persistent fever, regardless of a low or high fever, tend to be severe. If patients develop a fever again 1 week after defervescence, it is more likely to be complicated with infection; these patients also may have a poor prognosis.[10] The general data of patients with COVID 19 undergoing hemodialysis in the hospital showed that male patients with onset were predominant, which was consistent with the data of the general population. Patients aged more than 60 years (57.7%) were predominant. The reasons might be as follows. On the one hand, patients undergoing maintenance hemodialysis were mostly middle-aged and elderly people, and therefore the onset age was old. On the other hand, most elderly patients were complicated with hypertension, diabetes, and other basic diseases, and they were easily infected due to low immunity. Among more than 20 patients, patients with hypoxemia still accounted for a large proportion, which might be related to many elderly patients complicated with hypertension, diabetes, and other basic diseases. The immunity of the patients’ body was low. Before the infection, the chronic cardiopulmonary failure occurred due to the long-term volume overload. Hence, the patients were more prone to hypoxemia, thus becoming severely ill. These 2 reasons were also the high-risk factors for infection in patients undergoing hemodialysis. Respiratory symptoms, such as fever, dry cough, and shortness of breath, still accounted for a large proportion, but the proportion of patients without a fever was close to that of those with a fever. Even a small number of patients had gastrointestinal symptoms, such as nausea and vomiting as the initial feature. Some patients were clinically asymptomatic, suggesting that when patients undergoing hemodialysis were complicated with COVID 19, the clinical features might be atypical, and the disease onset was more insidious. Medical workers need to protect and disinfect the hemodialysis room. They also need to monitor the clinical features of patients and the results of lung imaging and laboratory tests more closely and regularly.
Studies have shown that coronavirus may suppress cellular immune function in vivo by depleting immune cells. The B-lymphocyte count of patients is significantly reduced, and the CD4 +/CD8 + T-lymphocyte ratio continues to decline, which may be an important indicator of the exacerbation of the conditions. The lymphocyte count decreased in 35% to 69% of patients and was less than 0.8 × 109/L in 97% of patients.[5,8–10] The mean WBC and neutrophil counts did not decrease significantly in patients undergoing maintenance hemodialysis in the hospital, but the mean lymphocyte count decreased significantly. D-dimer elevations occurred in 36% of patients with COVID 19, which was more significant in patients admitted to the intensive care unit.[5,7–9] A decrease in albumin level occurred in 97% of patients with COVID 19, especially in severe cases.[5,7–9] Pathological changes were mentioned in the Diagnosis and Treatment Scheme of New Coronavirus Pneumonia (trial version 7) released by the National Health Commission. Myocardial cell degeneration and necrosis were seen in the heart and blood vessels. Some monocyte, lymphocyte, and/or neutrophil infiltration was noted in the mesenchyme. Vascular endothelial shedding, inflammation of the inner membrane, and thrombosis were observed.[4] This study also found that the levels of markers of myocardial injury (BNP, D-dimer, and so forth) in patients were elevated to varying degrees. These laboratory indicators suggested that patients had experienced virus-induced damage to the myocardium and blood vessels, which helped clinical medical workers in assessing the conditions of patients with systemic complications. In addition, this study found that the indicators of liver function were still in the normal range for patients with COVID 19 undergoing dialysis. The mean serum albumin level was slightly lower, indicating that the liver was not the main damage site compared with the lung, heart, and blood vessels.
Most researchers believe that 100% of patients with COVID 19 have positive CT findings, which are manifested as single ground-glass opacity, multiple external ground-glass opacities, patchy ground-glass opacity of both lungs with segmental pulmonary consolidation, paving stone sign, diffuse ground-glass opacity in the lungs with bronchial inflation sign, or large areas of consolidation in the lungs with lobular interstitial thickening.[7,11] Some studies[12] classified it as 3 stages based on the pathological staging of COVID 19: early, progressive, and severe. A few patients were complicated with small pleural effusion and/or pericardial effusion. The imaging examinations of patients with confirmed COVID 19 in the hemodialysis center revealed the following. For patients with uremia and COVID 19 undergoing maintenance hemodialysis, ground-glass opacity, consolidation, and stripe shadows were still the main imaging features. A few patients were complicated with pleural effusion and latticed changes. Pleural effusion may be related to COVID 19, but it may be more closely associated with the long-term volume overload of patients with uremia; serous membrane fluid may be present in the body for a long time. Hence, while treating patients with uremia and COVID 19 undergoing maintenance hemodialysis, the volume overload patients should be more closely monitored to avoid symptoms, such as congestive HF, which may further worsen the lung disease.
Patients with uremia undergoing maintenance hemodialysis are kept continuously and frequently in the crowded hemodialysis room of the hospital. In the COVID 19 epidemic, the hemodialysis medical workers and patients should be protected to avoid continuous COVID 19 transmission in the hemodialysis room. In addition to good protection and disinfection, attention should be paid to changes in conditions of this population after COVID 19 infection. Also, more experience should be gained in diagnosis and treatment. Clinical medical workers should be provided assistance in making a clinical diagnosis in a faster, more accurate, and timely manner, isolating patients in time, blocking the COVID 19 transmission, guiding the treatment, and evaluating the efficacy. Several risk factors including ischemic heart disease, uncontrolled hypertension, high output HF from shunting through vascular hemodialysis access, and anemia, contribute to development of HF in patients with End-Stage Renal Disease, and the incidence of cardiovascular events, sudden death, and HF mortality is higher than the general generation, which has been reported in other literatures.[13–15] But whether there are still such clinical characteristics between the 2 groups need further verification in the follow-up study. There are some special characteristics in the treatment of dialysis patients with COVID 19 compared to nondialysis patients, such as the application of continuous blood purification, the nephrotoxicity of the drug, whether the drug passes through the dialysis membrane, the limitation of fluid volume and so on. The comparison of treatment options between the 2 groups can be carried out in the follow-up study. Meanwhile, it is necessary to compare the clinical characteristics of dialysis patients with COVID 19 patients and non COVID 19 patients in the future work, so that the characteristics of dialysis patients with COVID 19 can be more clearly understood. Another shortcoming of the study include the small number of included patients, which is related to the small number of confirmed patients in our hospital. Whether the study can represent the characteristics of dialysis patients with COVID 19 need to be further verified, and the sample size can be increased in the later study by cooperating with other designated hospitals. At the same time, the treatment of these patients has some different characteristics compared with the treatment of non-dialysis patients. Mastering these characteristics can contribute to early diagnosis, isolation, and treatment of Covid19 to control the spread of the epidemic.
Author contributions
You Wang is responsible for writing papers; Manli Hu is responsible for data collation and statistical analysis; Gang Ye and Qingqiao Yin are responsible for the results analysis; Pei Pi is responsible for language modification; Dan Luo is responsible for guidance and modificatio.
Footnotes
Abbreviations: BNP = B-type natriuretic peptide, HF = heart failure, WBC = white blood cell count.
How to cite this article: Wang Y, Hu M, Ye G, Zhao Y, Yin Q, Pi P, Luo D. Clinical characteristics of patients with uremia undergoing maintenance hemodialysis complicated with COVID-19. Medicine. 2020;99:32(e21547).
YW and MH contributed equally to this work.
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- [1].Bogoch II, Watts A, Thomas-Bachli A, et al. Potential for global spread of a novel coronavirus from China. J Travel Med 2020;27: [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Lu R, Zhao X, Li J, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet 2020;395:565–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].China NHCotPsRo. Diagnosis and Treatment of Novel Coronavirus-infected Pneumonia (Trial 4th Edition) [EB/OL]. 2020. Available at: http://www.nhc.gov.cn/yzygj/s7653p/202001/4294563ed35b43209b31739bd0785e67/files/7a9309111267475a99d4306962c8bf78.pdf [access February 13th, 2020]. [Google Scholar]
- [4]. China NHCotPsRo. Diagnosis and Treatment Scheme of NCP Infected Pneumonia (Trial Version 7) [J/OL]. Journal of Cardiovascular and Pulmonary Diseases 2020,39; 103-107. [Google Scholar]
- [5].Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Guan WJ, Ni ZY, Hu H, et al. Clinical characteristics of 2019 novel coronavirus infection in China. med Rxiv 2020;382:1708–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Chen L, Liu HG, Liu W, et al. Analysis of clinical features of 29 patients with 2019 novel coronavirus pneumonia. Zhonghua Jie He He Hu Xi Za Zhi 2020;43:E005. [DOI] [PubMed] [Google Scholar]
- [8].Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020;395:507–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020;323:1061–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Yan L, Li YS. Identification and treatment strategies for critically ill patients with COVID-1. J New Med 2020;51:161–7. [Google Scholar]
- [11].Mei HX, Li YS, Chen ZP, et al. Application of CLI in the early diagnosis of sepsis complicated with ARDS. J New Med 2016;47:681–5. [Google Scholar]
- [12].Shi HB, Han XY, Fan YQ, et al. Clinical and imaging features of patients infected with 2019-nCoV pneumonia. J Clin Radiol 2020;39:8–11. [Google Scholar]
- [13].Remppis A, Ritz E. Cardiac problems in the dialysis patient: beyond coronary disease. Semin Dial 2008;21:319–25. [DOI] [PubMed] [Google Scholar]
- [14].Chen TH, Wo HT, Chang PC, et al. A meta-analysis of mortality in end-stage renal disease patients receiving implantable cardioverter defibrillators (ICDs). PLoS One 2014;9:e99418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].US Renal Data System 2012 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. Bethesda, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2012. Available at: http://www.usrds.org/atlas.aspx. Accessed August 1,2013. [Google Scholar]


