Abstract
Objectives:
According to the data of Organisation for Economic Cooperation and Development, almost all the countries got increased medical expenditures in these years. Among the diseases, migraine is a condition that affects predominantly young and middle-aged people. It results in great economic losses. So we perform this research to investigate the acupuncture effect of reducing medical expenditure and medical resources use.
Perspective:
Acupuncture is a non-pharmacologic treatment and it became popular in recent years. In Taiwan, about 13% migraine patients visited acupuncture doctor. We hypothesized that the acupuncture had the additional effect than the medical treatment.
Setting:
We analysed the economic cost and medical visits in the real word.
Methods:
We used national cohort data from Taiwan, retrospectively gathered between 2000 and 2010. We selected newly diagnosed migraine patients who were diagnosed by registered neurologists formally licensed by the Taiwan Neurological Society. We divided these patients into two groups: with and without acupuncture treatment. The main outcome was medical expenditures and visits within 1 year after acupuncture.
Results:
In migraine patients who received acupuncture treatment, medical expenditures on emergency care and hospitalization were significantly lower than the group without acupuncture treatment.
Conclusion:
According to our real-world data, acupuncture can reduce the medical expenditure in migraine patients within 1 year after diagnosis. For the health policy maker, it is cost effective to encourage combining acupuncture and western medicine to treat migraine patients. For the doctors in routine clinical practice, who may consider to consult acupuncture doctors to deal with the migraine patients together.
Keywords: acupuncture, economic, health care system, medical expenditure, migraine, real world
1. Introduction
According to the data of Organisation for Economic Cooperation and Development, almost all the countries got increased medical expenditures in these years. Among the diseases, migraine occurs with the highest prevalence between the ages of 25 and 55 years, potentially the most productive period of life.[1] Migraine carries a significant economic burden in several countries.[2–7] In 2016, globally about 1.04 billion (95% CI 1·00–1·09) people had migraine and migraine caused 45.1 million (95% CI 29·0–62·8) years of life lived with disability globally.[8] In Taiwan, the prevalence of migraine is approximately 9.1% (female = 14.4%, male = 4.5%)[9] and also causes numerous economic loss.[10] Some migraine patients visited our clinics and told us that their migraine improved a lot by seeking acupuncture therapy. They had less emergency department visits due to severe headache, and which saved both their time and money. As a result, we retrospectively collected the data from our National Health Insurance Research Database, a real-world clinical data in Taiwan, to analyse the acupuncture effect among migraine patients, by comparing the numbers of emergency visits, hospitalization, and total medical expenditures.
2. Materials and methods
2.1. Study design and data source
The National Health Insurance Research Database (NHIRD) was established by the Taiwanese government and includes historical outpatient, hospitalization, emergency care, and medication information on each insurant. At present, the database covers more than 99% of Taiwanese citizens. To emphasize the protection of privacy, patient identification numbers were encrypted before the database was released by the government.
We conducted this study by searching the Longitudinal Health Insurance Database 2000, which is based on the NHIRD and includes 1 million randomly selected subjects from the original database, about 1/23 of the whole population (with the same age and sex distribution). The Longitudinal Health Insurance Database 2000 also included the diagnostic history of the Chinese herbal medicine department. The historical diagnoses are coded according to the International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9-CM). The Research Ethics Committee of China Medical University and Hospital in Taiwan approved the study (CMUH-104-REC2-115-R3).
2.2. Study subjects
Eligible study subjects were patients with migraine (ICD-9-CM: 346) newly diagnosed by a neurologist and with at least two outpatient or one inpatient visit. The case group was comprised of patients who agreed to undergo acupuncture treatment greater than or equal to 12 times (2 packages) after migraine diagnosis; control group were 4:1 propensity score matched by demographic factors, comorbidities, migraine treatment drugs and frequency of migraine outpatients visits with case group (see Fig. 1).
Figure 1.
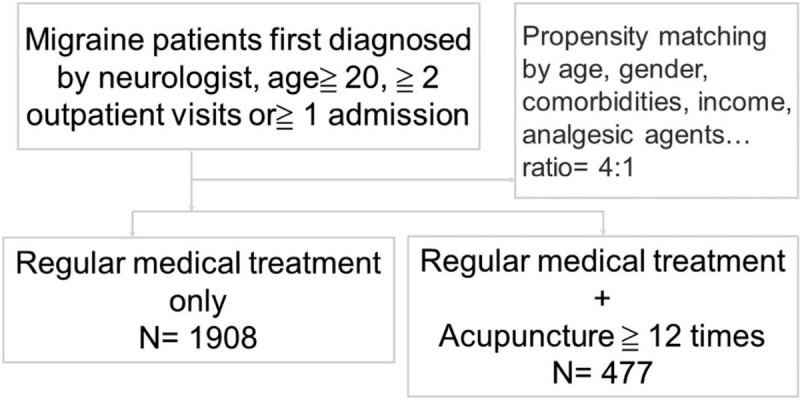
Research algorism in our study.
This 4:1 ratio was according to their propensity score through nearest neighbor matching, initially to the eighth digit and then as required to the first digit. Therefore, matches were first made within a caliper width of 0.0000001, and then the caliper width was increased for unmatched cases to 0.1. We reconsidered the matching criteria and performed a rematch (greedy algorithm). For each patient with acupuncture treatment, the corresponding comparisons were selected based on the nearest propensity score.
We did this propensity score matching to reduce the confounding factors. The comorbidities of hypertension, diabetes mellitus, etc., are highly related to the medical expenditure[11] and medical visits.[12,13] According to the previous research,[14,15] the migraine severity and acute medication use are associated with higher all-cause health care costs for patients with migraine. So we matched the two groups of patients by migraine acute treatment drugs and frequency of outpatients visits to control these confounding factors.
About the sample size calculation, we used the R software, package: epiDisplay (Epidemiological calculator, author: Virasakdi Chongsuvivatwong), under the condition of Alpha = 0.05, power = 0.9, n2/ n1 = 4 (by propensity score). The minimal required sample size was 112 patients in “acupuncture” group, and 445 patients in “medical treatment only” group. Our actual patient number is 477 and 1908 respectively, four times larger than the minimal requirement number.
2.3. Types of acupuncture used in this study
Eligible acupuncture types included manual acupuncture of the Traditional Chinese Medicine type (B41, B42, B45, B46, B80-B84, B90-B94, P27041, P31103, P32103, and P33031) and electro acupuncture (B43, B44, B86–89, and P33032).
2.4. Primary outcome and covariates
In this study, we aimed to investigate migraine-related medical expenditures and the number of visits for emergency care and hospitalization for migraine. The covariates included a history of diabetes mellitus (ICD-9-CM: 250), hyperlipidemia (ICD-9-CM: 272), mental disorders (ICD-9-CM: 290-319), epilepsy (ICD-9-CM: 345), hypertension (ICD-9-CM: 401–405), ischemic heart disease (ICD-9-CM: 410–414), congestive heart failure (ICD-9-CM: 428.0), osteoporosis (ICD-9-CM: 733.0, 733.1), stroke (ICD-9-CM: 430–438), asthma (ICD-9-CM: 493), and non-infectious kidney disease (ICD-9-CM: 580–589), as comorbidities. The interventional drugs discussed in this study came from the Taiwan migraine treatment guidelines,[16] which are followed by most neurologists. These drugs were Sumatriptan [ATC (Anatomical Therapeutic Chemical) code: N02CC01], Rizatriptan (ATC code: N02CC04), Ergotamine (ATC code: N02CA52), Caffeine (ATC code: R05X, N02BE54, R01BA51, R05DA, N02BE51, N02BE71, R06AA52, R05FA02, N06BC, R06AK, N02CA52, G03BA, R06AK, M03BB53, R06AE55, M03BC51, M03BB03), Acetaminophen (ATC code: N02BE01, M03BB52, N02BE01, M03BC51, M03BA02, M03BB53, N02AX52, M03BA52), Ibuprofen (ATC code: N02CC01), Naproxen (ATC code: M01AE02), Diclofenac (ATC code: M01AB05), Celecoxib (ATC code: M01AH01), and Etoricoxib (ATC code: M01AH05). Age, gender, geographic region, income, and urbanization were the demographics-adjusted factors in this study.
2.5. Statistical analyses
To test for significant differences in demographic factors, comorbidities, and medications between migraine patients with or without acupuncture, a chi-square test was used; the mean age, frequency of visits, and medical expenditures on emergency care and hospitalization in the acupuncture and non-acupuncture groups were compared by an unpaired t-test. The statistical analysis was conducted with a type I error rate of α = 0.05 using the statistical software package SAS, version 9.4 (SAS Institute, Inc, Cary, NC).
3. Results
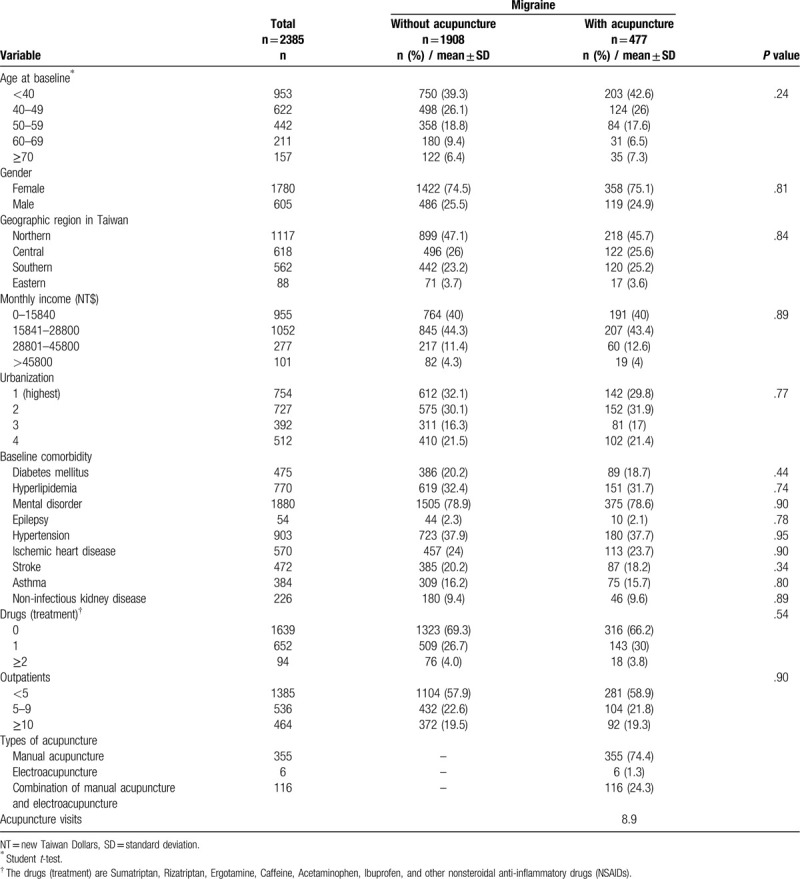
We enrolled a total of 2385 migraine patients (Table 1), including 477 with acupuncture treatment (case) and 1908 without acupuncture treatment (control). Approximately 75% were female, and the mean ages were 44.36 and 44.91 years in the case and control groups, respectively. After propensity score matching, there was no significant difference in demographic factors, comorbidities, frequency of migraine outpatient visits, or medication usage. Considering the type of acupuncture used among patients with acupuncture treatment, 74.4% only accepted manual acupuncture, 1.3% only accepted electro acupuncture, and 24.3% underwent a combination of manual acupuncture and electro acupuncture.
Table 1.
Demographic characteristics and comorbidities in patients newly diagnosed with migraine with or without acupuncture in Taiwan from 2000 to 2010.
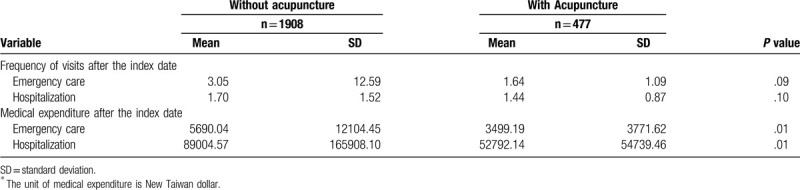
Medical expenditures on emergency care (P = .01) and hospitalization (P = .01) were significantly lower in patients who underwent acupuncture treatment (see Table 2).
Table 2.
Medical visits and ∗expenditures in 1 year with and without acupuncture.
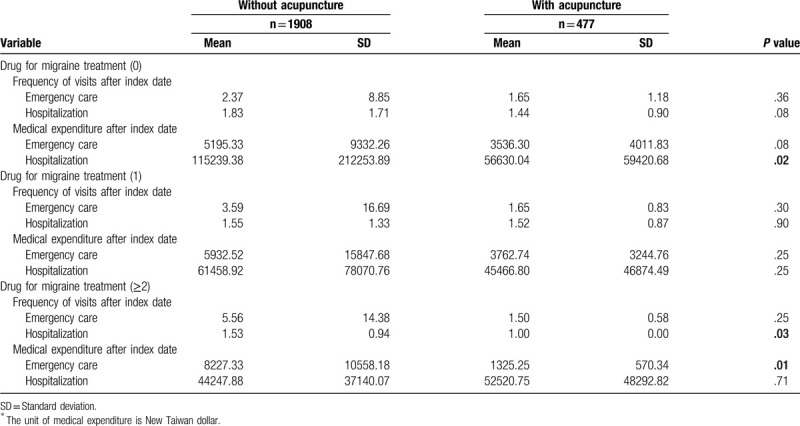
When stratified by medication usage (Table 3), migraine patients with more than one type of drug treatment combined with acupuncture had significant lower frequency of hospitalization (P = .03) and emergency care expenditure (P = .01) within one year. Which result may indicate that the severe migraine patients get more benefit from the combined acupuncture treatment.
Table 3.
Medical visits and ∗expenditure of migraine, stratified by analgesic drugs.
4. Discussion
Acupuncture is a complementary and alternative medicine therapy in use for migraine. In the 2016 Cochrane Library,[17] the authors concluded that adding acupuncture to symptomatic treatment of migraine attacks reduces the frequency of headaches. Thus, acupuncture can be considered a treatment option for patients willing to undergo this treatment. Eleven years ago, a randomized, controlled trial held in Germany found that acupuncture is cost effective in patients with headache.[18] Two years ago, the group in Czech Republic published their randomized controlled trial, specified to investigate the cost effectiveness about acupuncture in “migraine” patients.[19] Not only European countries demonstrated the efficacy of acupuncture, the team from Beijing did the randomized controlled trial and found that true acupuncture plus placebo is better than the group of sham acupuncture plus flunarizine.[20] The Taiwanese team focused on the chronic migraine and found the acupuncture group got better improvement than the Topiramate group.[21] And the adverse events were significantly lower in the acupuncture group (6%) than the Topiramate group (66%). Our real world data analysis is consistent to the finding of above several randomized control trials that acupuncture is cost effective in treating migraine patients.
The strength of this study was that it was the real world data reflecting the clinical practice and the real medical expenditure in Taiwan. Our study included a large number of patients to lessen the effects of minor confounding factors. The Taiwan Health Insurance Program has covered approximately 99% of the population since 1995, and a growing body of articles has confirmed the validity of the dataset.[22] Instead of the prospective study, our retrospective analysis of the real world data supports the value of acupuncture treatment from the other side. The acupuncture add-on therapy can reduce the medical expenditure of migraine patients, and reduce the hospitalization in severe migraine patients.
The first limitation of our study is the retrospective design. There are some common threats to internal validity in retrospective studies.[23] For example, the two groups weren’t randomly assigned. There was some existing selection bias. And there are another events, other than the intervention, influence the outcome. As we had mentioned in the section of “material and methods”, the comorbidities and disease severity are highly related to the medical expenditure and medical visits.[11–15] The previous study using the same national cohort (NHIRD in Taiwan) also told us that age, income, and urbanization would significantly influence the medical expenditure.[24,25] So we controlled these factors by the propensity matching (Table 1), trying our best to reduce their confounding effects. But there are still some other factors that we cannot control, for example, some social and behavior factors (influence the patients to choose acupuncture treatment).[26]
About the propensity score, in intervention trials, only randomization guarantees equal distributions of all known and unknown patient characteristics between an intervention group and a control group and enables causal statements on treatment effects.[27] The propensity score is a widely used tool for non-randomized trials to analyze with multiple regression models. And the previous research had confirmed the power of this tool.[28–31]
The second limitation was the diagnosis of migraine. We could not select patients by the International Classification of Headache Disorders 3rd edition criteria[32] because of lack of detail headache history. And we enrolled both chronic migraine (≥15 headache days/month) and episodic migraine (<15 headache days/month). The previous studies told us that chronic migraine had greater medical expenditure than the episodic migraine.[33,34] We attempted to increase the precision of diagnosis by selecting migraine patients who were first diagnosed with migraine by a certificated neurologist. Most of our certificated neurologists adhere to the Chinese form of International Classification of Disease, Ninth Revision, Clinical Modification criteria translated by Taiwan Headache Society.
The third limitation was the different severity of migraine patients.[35] We matched the two groups by the number of analgesic drugs (acetaminophen, triptans, nonsteroidal anti-inflammatory drugs, and others) and the number of outpatient department visits (generally more severe patients visited the clinic more often). We did not match the patients for migraine preventive medication (propranolol, flunarizine, etc.) use because of the low prescription rates and poor drug adherence.[36–38]
The forth limitation was the overlapping of neck myofascial pain and migraine.[39] Clinically, several migraine patients complained not only headache but also neck pain or tenderness. We speculated, on the basis of previous research, that the relief of neck pain improved the patients’ symptoms of migraine and prevented further migraine attacks.[40–52]
The fifth limitation is that we did not know the acupoints chosen by the doctors. According to traditional Chinese medicine theories, migraine is considered a disorder of the Shaoyang meridians (including Foot Shaoyang and Hand Shaoyang meridians, Figs. 2 and 3).[53–56] One randomized controlled trial in China also showed that the best treatment effect was achieved by choosing acupoints on the Shaoyang meridian, in comparison with other meridians or sham acupuncture.[57]
Figure 2.

Brief illustration of Foot Shaoyang meridian (= Gallbladder meridian, GB meridian).
Figure 3.
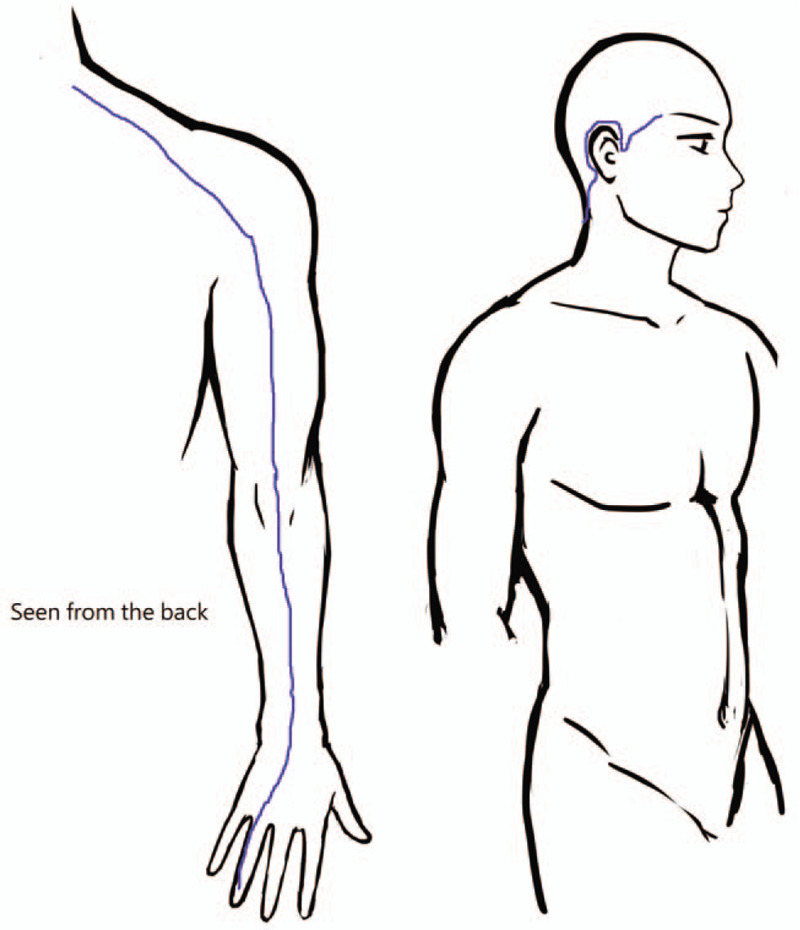
Brief illustration of Hand Shaoyang meridian (=Triple Energizer Meridian, TE meridian).
5. Conclusions
In migraine patients who underwent acupuncture treatment, the medical expenditures on emergency care (P = .01) and hospitalization (P = .01) were significantly lower than patients without acupuncture treatment. For the health policy maker, it is cost effective to encourage combining acupuncture and western medicine to treat migraine patients. For the doctors in routine clinical practice, who may consider to consult acupuncture doctors to deal with the migraine patients together.
Acknowledgments
The authors would like to thank Enago (www.enago.tw) for the English language review, and Yu-Hsin Chen for drawing the Figures 2 and 3 (foot and hand shaoyang meridians).
Author contributions
Conceptualization, Sheng-Ta Tsai; Data curation, Mei-Chen Lin; Formal analysis, Mei-Chen Lin; Project administration, Hung-Yu Huang and Yi-Wen Lin; Resources, Hsien-Yin Liao and Chon-Haw Tsai; Supervision, Hung-Yu Huang and Yi-Wen Lin; Validation, Chun-Hung Tseng; Writing – original draft, Sheng-Ta Tsai; Writing – review & editing, Boon-Khai Teoh and San Shao.
Footnotes
Abbreviations: ATC code = anatomical therapeutic chemical code, ICD-9-CM = International Classification of Disease, Ninth Revision, Clinical Modification, NHIRD = National Health Insurance Research Database.
How to cite this article: Tsai ST, Tseng CH, Lin MC, Liao HY, Teoh BK, San S, Tsai CH, Huang HY, Lin YW. Acupuncture reduced the medical expenditure in migraine patients: Real-world data of a 10-year national cohort study. Medicine. 2020;99:32(e21345).
Data Availability: All data generated or analyzed during this study are included in this published article. The datasets are not publicly available due to the contract of acquiring data, which the data sharing should be permitted by the Bureau of the National Research Institute (http://english.nhri.org.tw/).
This work was supported by grants from the Ministry of Health and Welfare, Taiwan [MOHW107-TDU-B-212–123004], China Medical University Hospital, Academia Sinica Stroke Biosignature Project [BM10701010021], MOST Clinical Trial Consortium for Stroke [MOST 107–2321-B-039 -004-], China Medical University Hospital (DMR-109-169), Tseng-Lien Lin Foundation, Taichung, Taiwan, and Katsuzo and Kiyo Aoshima Memorial Funds, Japan. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. No additional external funding was received for this study.
The authors have no conflicts of interest to disclose.
The data that support the findings of this study are available from a third party, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are available from the authors upon reasonable request and with permission of the third party.
References
- [1].Lipton RB, Stewart WF, Vonkorff M. The Burden of Migraine - a Review of Cost to Society. Pharmacoeconomics 1994;6:215–21. [DOI] [PubMed] [Google Scholar]
- [2].Iyer RG, Fensterheim LE, Berger JE, et al. Migraine sufferers show significant health care utilization and expenditures. Value Health 2008;11:A143–4. [Google Scholar]
- [3].Mesas AE, Gonzalez AD, Mesas CE, et al. The association of chronic neck pain, low back pain, and migraine with absenteeism due to health problems in Spanish workers. Spine 2014;39:1243–53. [DOI] [PubMed] [Google Scholar]
- [4].Michel P, Dartigues JF, Duru G, et al. Incremental absenteeism due to headaches in migraine: results from the Mig-Access French national cohort. Cephalalgia 1999;19:503–10. [DOI] [PubMed] [Google Scholar]
- [5].Mychaskiw MA, Sankaranarayanan J. An estimate of the direct costs of migraine in the united states using the medical expenditure panel survey. Value Health 2003;6:187–8. [Google Scholar]
- [6].Raval AD, Shah A. National trends in direct health care expenditures among US adults with migraine: 2004 to 2013. J Pain 2017;18:96–107. [DOI] [PubMed] [Google Scholar]
- [7].Shah A, Raval A. National trends in direct health care expenditures among adults with migraine in the United States: 2004-2013. Value Health 2016;19:A28–128. [DOI] [PubMed] [Google Scholar]
- [8].Global, regional, and national burden of migraine and tension-type headache, 1990-2016: a systematic analysis for the Global Burden of Disease Study, 2016. Lancet, Neurol 2018;17:954–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Wang SJ, Fuh JL, Young YH, et al. Prevalence of migraine in Taipei, Taiwan: a population-based survey. Cephalalgia 2000;20:566–72. [DOI] [PubMed] [Google Scholar]
- [10].Fuh JL, Wang SJ, Lu SR. Impact of migraine on the employed labor force in Taiwan. J Chin Med Assoc 2008;71:74–8. [DOI] [PubMed] [Google Scholar]
- [11].Park C, Fang J, Hawkins NA, et al. Comorbidity status and annual total medical expenditures in U.S. hypertensive adults. Am J Prev Med 2017;53(6s2):S172–s181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Hu T, Dattani ND, Cox KA, et al. Effect of comorbidities and medications on frequency of primary care visits among older patients. Can Fam Physician 2017;63:45–50. [PMC free article] [PubMed] [Google Scholar]
- [13].Maeng DD, Hao J, Bulger JB. Patterns of multiple emergency department visits: do primary care physicians matter? Perm J 2017;21:16–063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Bonafede M, Cai Q, Cappell K, et al. Factors associated with direct health care costs among patients with migraine. J Manag Care Spec Pharm 2017;23:1169–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Ford JH, Ye W, Nichols RM, et al. Treatment patterns and predictors of costs among patients with migraine: evidence from the United States medical expenditure panel survey. J Med Econ 2019;22:849–58. [DOI] [PubMed] [Google Scholar]
- [16].Hsu YC, Lin KC, Taiwan Headache Society T. Medical treatment guidelines for acute migraine attacks. Acta Neurol Taiwan 2017;26:78–96. [PubMed] [Google Scholar]
- [17].Linde K, Allais G, Brinkhaus B, et al. Acupuncture for the prevention of episodic migraine. Cochrane Database Syst Rev 2016. CD001218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Jena S, Witt CM, Brinkhaus B, et al. Acupuncture in patients with headache. Cephalalgia 2008;28:969–79. [DOI] [PubMed] [Google Scholar]
- [19].Pokladnikova J, Maresova P, Dolejs J, et al. Economic analysis of acupuncture for migraine prophylaxis. Neuropsychiatr Dis Treat 2018;14:3053–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Wang LP, Zhang XZ, Guo J, et al. Efficacy of acupuncture for migraine prophylaxis: a single-blinded, double-dummy, randomized controlled trial. Pain 2011;152:1864–71. [DOI] [PubMed] [Google Scholar]
- [21].Yang CP, Chang MH, Liu PE, et al. Acupuncture versus topiramate in chronic migraine prophylaxis: a randomized clinical trial. Cephalalgia 2011;31:1510–21. [DOI] [PubMed] [Google Scholar]
- [22].Chen LF, Chang CM, Huang CY. Home-based hospice care reduces end-of-life expenditure in Taiwan: a population-based study. Medicine (Baltimore) 2015;94:e1613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Tofthagen C. Threats to validity in retrospective studies. J Adv Pract Oncol 2012;3:181–3. [PMC free article] [PubMed] [Google Scholar]
- [24].Fang K, Shia BC, Ma S. Health insurance coverage, medical expenditure and coping strategy: evidence from Taiwan. BMC Health Serv Res 2012;12:442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Fang K, Ma C, Jiang Y, et al. Illness, medical expenditure and household consumption: observations from Taiwan. BMC Public Health 2013;13:743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Shih SF, Lew-Ting CY, Chang HY, et al. Insurance covered and non-covered complementary and alternative medicine utilisation among adults in Taiwan. Soc Sci Med 2008;67:1183–9. [DOI] [PubMed] [Google Scholar]
- [27].Kuss O, Blettner M, Borgermann J. Propensity Score: an Alternative Method of Analyzing Treatment Effects. Dtsch Arztebl Int 2016;113:597–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Seeger JD, Williams PL, Walker AM. An application of propensity score matching using claims data. Pharmacoepidemiol Drug Saf 2005;14:465–76. [DOI] [PubMed] [Google Scholar]
- [29].Austin PC, Grootendorst P, Anderson GM. A comparison of the ability of different propensity score models to balance measured variables between treated and untreated subjects: a Monte Carlo study. Stat Med 2007;26:734–53. [DOI] [PubMed] [Google Scholar]
- [30].Seeger JD, Kurth T, Walker AM. Use of propensity score technique to account for exposure-related covariates: an example and lesson. Med Care 2007;45(10 Supl 2):S143–148. [DOI] [PubMed] [Google Scholar]
- [31].Groenwold RHH, Hak E, Hoes AW. Quantitative assessment of unobserved confounding is mandatory in nonrandomized intervention studies. J Clin Epidemiol 2009;62:22–8. [DOI] [PubMed] [Google Scholar]
- [32].Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders. 3rd edition. Cephalalgia 2018;38:1–211. [DOI] [PubMed] [Google Scholar]
- [33].Bloudek LM, Stokes M, Buse DC, et al. Cost of healthcare for patients with migraine in five European countries: results from the International Burden of Migraine Study (IBMS). J Headache Pain 2012;13:361–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Messali A, Sanderson JC, Blumenfeld AM, et al. Direct and indirect costs of chronic and episodic migraine in the United States: a web-based survey. Headache 2016;56:306–22. [DOI] [PubMed] [Google Scholar]
- [35].Silberstein SD, Lee L, Gandhi K, et al. Health care resource utilization and migraine disability along the migraine continuum among patients treated for migraine. Headache 2018;58:1579–92. [DOI] [PubMed] [Google Scholar]
- [36].Hepp Z, Dodick DW, Varon SF, et al. Adherence to oral migraine-preventive medications among patients with chronic migraine. Cephalalgia 2015;35:478–88. [DOI] [PubMed] [Google Scholar]
- [37].Lafata JE, Tunceli O, Cerghet M, et al. The use of migraine preventive medications among patients with and without migraine headaches. Cephalalgia 2010;30:97–104. [DOI] [PubMed] [Google Scholar]
- [38].Wenzel RG. Migraine-preventive medications: ensuring their appropriate use. J Am Pharm Assoc (2003) 2008;48:e107–120. [DOI] [PubMed] [Google Scholar]
- [39].Do TP, Heldarskard GF, Kolding LT, et al. Myofascial trigger points in migraine and tension-type headache. J Headache Pain 2018;19:84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Ashina S, Bendtsen L, Lyngberg AC, et al. Prevalence of neck pain in migraine and tension-type headache: a population study. Cephalalgia 2015;35:211–9. [DOI] [PubMed] [Google Scholar]
- [41].Bevilaqua-Grossi D, Goncalves MC, Carvalho GF, et al. Additional effects of a physical therapy protocol on headache frequency, pressure pain threshold, and improvement perception in patients with migraine and associated neck pain: a randomized controlled trial. Arch Phys Med Rehab 2016;97:866–74. [DOI] [PubMed] [Google Scholar]
- [42].Blaschek A, Decke S, Albers L, et al. Self-reported neck pain is associated with migraine but not with tension-type headache in adolescents. Cephalalgia 2014;34:895–903. [DOI] [PubMed] [Google Scholar]
- [43].Calhoun AH, Ford S. Double-blind, placebo-controlled, crossover study of early-intervention with Sumatriptan 85/Naproxen Sodium 500 in (Truly) episodic migraine: what's neck pain got to do with it? Postgrad Med 2014;126:86–90. [DOI] [PubMed] [Google Scholar]
- [44].Carvalho GF, Chaves TC, Goncalves MC, et al. Comparison between neck pain disability and cervical range of motion in patients with episodic and chronic migraine: a cross-sectional study. J Manip Physiol Ther 2014;37:641–6. [DOI] [PubMed] [Google Scholar]
- [45].Donoghue S, Vives-Mestres M, MacGregor A. Correlation of migraine attacks with neck pain and tension. Cephalalgia 2018;38:20–1. [Google Scholar]
- [46].Florencio LL, Chaves TC, Carvalho GF, et al. Neck pain disability is related to the frequency of migraine attacks: a cross-sectional study. Headache 2014;54:1203–10. [DOI] [PubMed] [Google Scholar]
- [47].Hershey AD, McDonald SA, Royall JM, et al. Sinus and neck pain associated with migraines in adolescents. Headache 2011;51:41–141. [Google Scholar]
- [48].Lampl C, Rudolph M, Deligianni CI, et al. Neck pain in episodic migraine: premonitory symptom or part of the attack? J Headache Pain 2015. 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Landgraf MN, von Kries R, Heinen F, et al. Self-reported neck and shoulder pain in adolescents is associated with episodic and chronic migraine. Cephalalgia 2016;36:807–11. [DOI] [PubMed] [Google Scholar]
- [50].MacGregor EA, Donoghue S, Vives-Mestres M. Correlation of migraine attacks with neck pain and tension. J Headache Pain 2018. 19.29500688 [Google Scholar]
- [51].Pradhan S, Choudhury SS. Clinical characterization of neck pain in migraine. Neurology India 2018;66:377–84. [DOI] [PubMed] [Google Scholar]
- [52].Zenkevich A, Filatova E, Latysheva N. Migraine and comorbid neck pain. Cephalalgia 2016;36:55–155. [Google Scholar]
- [53].Li XZ, Liu XG, Song WZ, et al. [Effect of acupuncture at acupoints of the Shaoyang Meridian on cerebral glucose metabolism in the patient of chronic migraine]. Zhongguo zhen jiu = Chinese acupuncture & moxibustion 2008;28:854–9. [PubMed] [Google Scholar]
- [54].Lin XM, Yao X, Di Z. [Acupuncture at “Siguan” combined with Gallbladder Meridian acupoints for migraine: a randomized controlled trial]. Zhongguo zhen jiu = Chinese acupuncture & moxibustion 2014;34:947–50. [PubMed] [Google Scholar]
- [55].Zhang H, Hu Y, Wu J, et al. [Timeliness law on the immediate analgesia on acute migraine treated with electroacupuncture at shaoyang meridian points]. Zhongguo zhen jiu = Chinese acupuncture & moxibustion 2015;35:127–31. [PubMed] [Google Scholar]
- [56].WHO. WHO international standard terminologies on traditional medicine in the western pacific region. Manila: WHO Regional Office for the Western Pacific; 2007. [Google Scholar]
- [57].Deng ZQ, Zheng H, Zhao L, et al. Health economic evaluation of acupuncture along meridians for treating migraine in China: results from a randomized controlled trial. BMC Complem Altern Med 2012;12:75. [DOI] [PMC free article] [PubMed] [Google Scholar]


