Abstract
Introduction:
Pacing of the His bundle and conduction system seems an attractive site for pacing. Lead placement in His-pacing might be technically challenging due to surrounding structures and particular anatomic location.
Patient concerns:
A 62-years old male patient was admitted for recurrent syncope. Electrocardiographic monitoring revealed periods of complete atrioventricular block with left branch block morphology and a QRS duration of 160 ms.
Diagnosis:
A diagnosis of intermittent complete atrioventricular block was made with a Class I indication of permanent dual-chamber cardiac pacing.
Interventions:
A lead delivery system with a C315 His catheter and a Select Secure 3830 69 cm pacing lead was placed at the septal area of the atrioventricular junction with good pacing and sensing thresholds. An important narowing of the QRS was observed.
Outcomes:
After the procedure, good pacing and sensing parameters were observed.
Echocardiography revealed disappearance of the previously recorded ventricular dyssynchronism.
Device follow-up at 1 month and 3 months showed stable pacing and sensing parameters.
Conclusion:
Pacing the distal His bundle normalized the QRS complex, therefore “curing” both the atrioventricular and the left bundle branch conduction abnormalities. As such, the technique can be used as an alternative to cardiac electrical resynchronization therapy with acceptable pacing and detection thresholds and better ventricular activation pattern.
Keywords: left bundle branch block, His pacing, electrode, threshold, sensing, AV block
1. Introduction
Cardiac pacing remains the only effective therapy for patients with symptomatic AV block or sinus node disease.[1] To date there is a continuous debate on the optimal ventricular pacing site: apex, RVOT or septum.[2] Biventricular pacing demonstrated improvement in patients with heart failure, reduced ejection fraction and left bundle branch block.[3] However, in the last decades, stimulation of the His bundle emerged as a very attractive site for pacing due to ventricular activation through the intrinsic conduction system. Lead placement in His bundle pacing might be technically challenging due to surrounding structures and particular anatomic location. This is illustrated by our case report: the level of the block was intrahisian, therefore the stimulation of the distal His bundle normalized the QRS complex and synchronized the left ventricular activation.
2. Case report
A 62-years old male patient was admitted to the Cardiology Department of the Brasov County Emergency Clinical Hospital for recurrent syncope. The patient‘s medical history included arterial hypertension, mild valvular regurgitations and nonsignificant coronary artery stenosis. Electrocardiographic monitoring revealed periods of completely intermittent atrioventricular block with left branch block morphology and a QRS duration of 160 ms. Laboratory values showed no reversible causes of AV block. Echocardiography revealed intra and interventricular dyssynchronism, with a preserved ejection fraction.
After thorough cardiological examination, the patient was considered to have Class I indication for permanent dual-chamber cardiac pacing and was proposed for permanent pacing of the His bundle.
A lead delivery system consisting of a C315 His catheter (Medtronic Inc., Minneapolis, MN, USA) and a Select Secure 3830 69 cm pacing lead (Medtronic Inc., Minneapolis, MN) was placed at the septal area of the atrioventricular junction (Figs. 1 and 2). In that region endocardial mapping was performed in a unipolar setting using the lead tip until a distal His bundle signal was obtained. At this level, pacing at variable amplitudes showed nonselective His bundle capture with important narrowing of the paced QRS complex (Fig. 3). The lead was fixed at this level with a final right ventricle pacing threshold of 0.25 V / 1 ms and a non-selective His capture threshold of 1,5 V/L ms with complete correction of the left bundle branch block and a paced QRS duration of 90 ms. Detection was measured at 5.2 mV.
Figure 1.
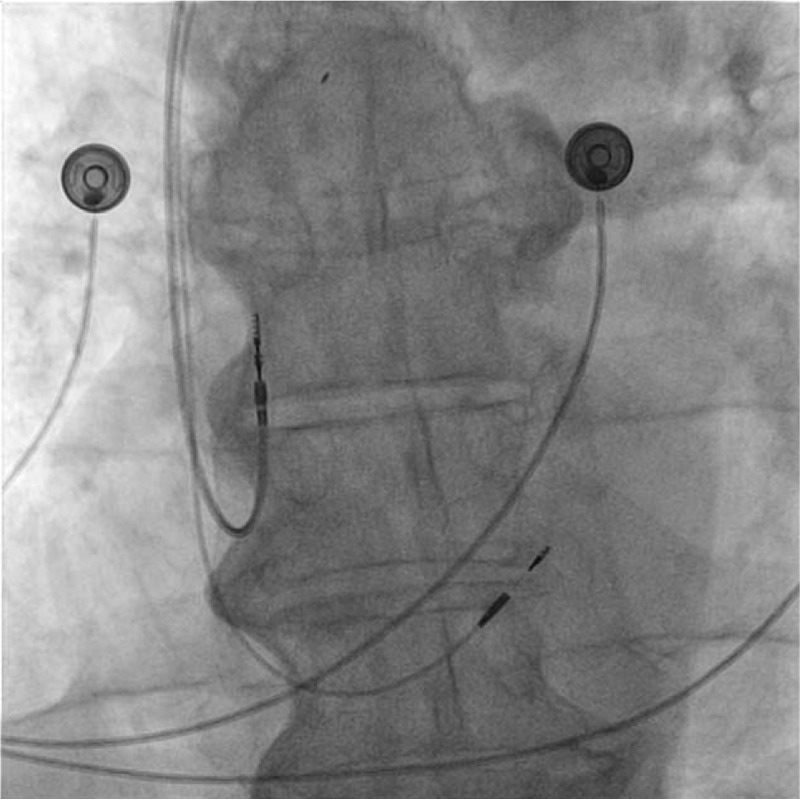
Fluoroscopic antero-posterior view of the atrial and ventricular leads implanted inside the right heart chambers: both leads are active fixation leads. The superior lead is fixated at the level of right atrial appendage and the inferior lead at the level of His bundle.
Figure 2.
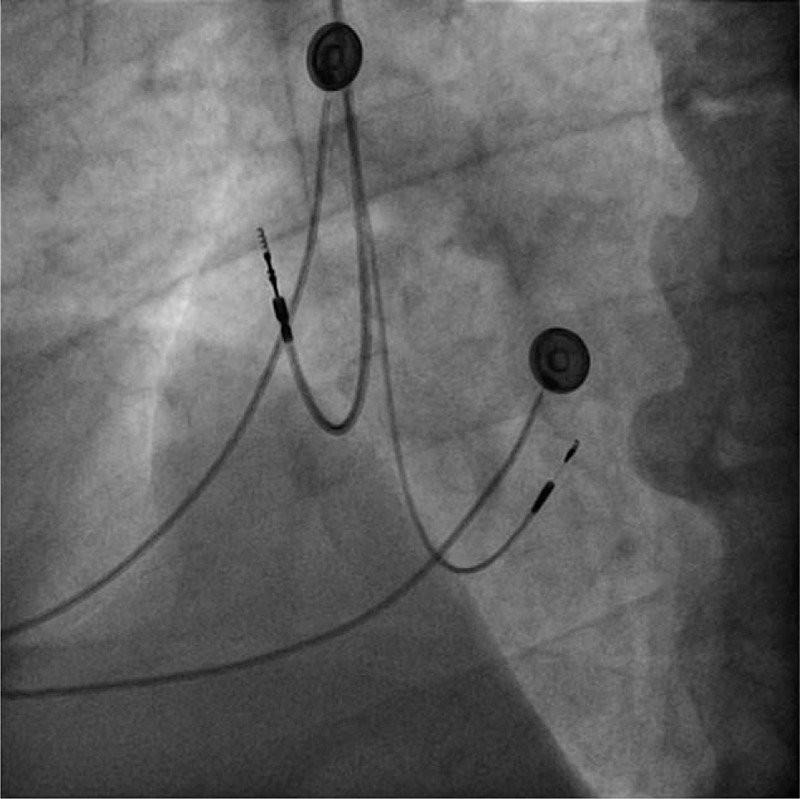
Fluoroscopic left anterior oblique view of the atrial and ventricular leads implanted inside the right heart chambers: both leads are active fixation leads. The superior lead is the atrial lead and is oriented towards the lateral wall of the right atrium, in contrast with the inferior lead which is the His-bundle pacing lead oriented towards the interventricular septum.
Figure 3.
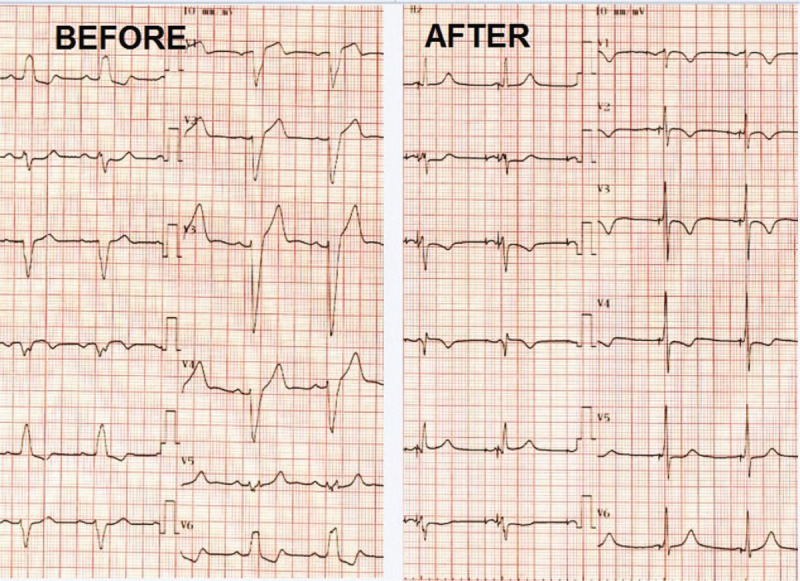
Twelve-lead ECG before and after His-pacing: Before pacing ECG shows a left bundle branch block morphology with a large QRS of 120 ms. After pacing ECG shows atrial and ventricular pacing with a narrow QRS of 90 ms. ECG = electrocardiogram.
The post-procedural echocardiographic reassessment revealed the disappearance of the previously recorded dyssynchrony parameters.
Device follow-up at 1 month and 3 months showed stable pacing and sensing parameters of the His bundle pacing lead: 1.5 V /Lms, respectively 5 mV, the patient being completely asymptomatic.
3. Discussion and Conclusion
In patients with LBBB and mild myocardial impairment (FE > 35%), there is data showing that they have a higher mortality rate than those without conduction disorders and a higher risk of long-term progression to heart failure.[4] These patients were not included in the large trials of cardiac resynchronization therapy and therefore currently there are no device intervention recommendations in these cases.
However, when there is an indication for conventional cardiac pacing, such as sinus node disease or symptomatic atrioventricular block, and the patient associates left bundle branch block, it is intuitive that electrical resynchronization of the heart, both atrioventricular and interventricular, would have long-term benefits.
Cardiac resynchronization therapy (CRT) by biventricular stimulation is currently the gold standard of electrical and mechanical resynchronization. Patients with LBBB and low ejection fraction benefit from CRT with an acute hemodynamic improvement that is translated in reduced morbidity and mortality.[5,6] However, the classical therapy of cardiac resynchronization, which involves endocardial stimulation of the right ventricle and epicardial stimulation of the left ventricle, which might be effective in some patients, is far from being a physiological therapy, and this is observed from the morphology of the paced QRS complex (negative in lead I, positive in V1, most often with a duration longer than 120 ms). In fact, biventricular stimulation induces intraventricular and interventricular dissynchronism if applied to patients that have a narrow QRS which is further translated into worse clinical outcome[7,8] Furthermore, there is electrophysiological evidence that the site of block in LBBB might be at the level of the His bundle or in the proximal portion of the left bundle branch.[9] Therefore, it would be possible to capture the conduction system beyond the level of block, with restoration of the normal conduction of electrical impulses.
In our case report, the level of block was intrahisian and the stimulation of the distal His bundle normalized the QRS complex. Thus, the technique can be used as an alternative to cardiac resynchronization therapy with acceptable pacing and detection thresholds and better results in ventricular activation pattern.[10]
The recently reported His-SYNC pilot trial showed promising results in patients with LBBB and heart failure with His bundle pacing being non-inferior to biventricular pacing in terms of improvement in left ventricular ejection fraction, cardiovascular hospitalization or death.[11] There are some potential drawbacks to this procedure. Due to the limited availability of specialized delivery systems, reaching the His bundle position could be difficult, especially in enlarged cardiac chambers and displaced His bundle. Furthermore the lead tip position at the AV junction could lead to either atrial oversensing or ventricular undersensing. There are also reports of increasing pacing thresholds in time and a possible progression to a more distal conduction disease which would make His bundle pacing redundant, but overall these issues seem to occur rarely.[12] Also, macrodislodgements of the lead have been rarely reported. Taken the above under consideration, patient selection is important in achieving procedural success. Older patients with enlarged cardiac chambers, ischemic heart disease (which usually means diffuse distal conduction disease) and severe comorbidities and with electrophysiological evidence of infrahisian disease are less likely to benefit from this procedure.[13] Nevertheless, if properly achieved, His bundle pacing can normalize the cardiac electrical conduction pattern with less lead burden and lead related complications. This was our case, in which fortunately the patient had an intrahisian block, which was “cured ” by direct pacing of the conduction system just beyond the line of block. Conclusion: Pacing the distal His bundle normalized the QRS complex, therefore “curing” both the atrioventricular and the left bundle branch conduction abnormalities. As such, the technique can be used as an alternative to cardiac electrical resynchronization therapy, with acceptable pacing and detection thresholds and better ventricular activation pattern.
Consent: Informed written consent was obtained from the patient for the publication of this case report and any accompanying medical images.
Author contributions
Resources: Catalin Pestrea, Alexandra Gherghina, Florin Ortan.
Supervision: Catalin Pestrea, Cismaru Gabriel, Radu Rosu
Visualization: Catalin Pestrea, Alexandra Gherghina, Florin Ortan, Cismaru Gabriel, Radu Rosu
Writing – original draft: Catalin Pestrea, Cismaru Gabriel
Writing – review & editing: Catalin Pestrea, Cismaru Gabriel, Alexandra Gherghina, Florin Ortan, Radu Rosu.
Footnotes
Abbreviations: AV = atrioventricular, CRT = cardiac resynchronization therapy, LBBB = left bundle branch block, RVOT = right ventricle outflow tract.
How to cite this article: Pestrea C, Gherghina A, Ortan F, Cismaru G, Radu R. His bundle pacing – a curative method: a Case Report. Medicine. 2020;99:32(e21633).
The authors have no conflicts of interest to disclose.
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
References
- [1].Janek S, Thisaranie H, Beaudette D. Safety and efficacy of AAIR pacing in selected pacing with sick sinus syndrome. Medicine 2018;97:e12833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Vijayaraman P, Bordachar P, Ellenbogen KA. The continued search for physiological pacing: where are we now? J Am Coll Cardiol 2017;69:3099–114. [DOI] [PubMed] [Google Scholar]
- [3].Prinzen FW, Vernooy K, Auricchio A. Cardiac resynchronization therapy: state-of-the-art of current applications, guidelines, ongoing trials, and areas of controversy. Circulation 2013;128:2407–18. [DOI] [PubMed] [Google Scholar]
- [4].Witt Chance M, Wu Gang, Yang Dachun, et al. Outcomes with left bundle branch block and mildly to moderately reduced left ventricular function. JACC: Heart Failure 2016;4:897–903. [DOI] [PubMed] [Google Scholar]
- [5].Foster AH, Gold MR, McLaughlin JS. Acute hemodynamic effects of atrio-biventricular pacing in humans. Ann Thorac Surg 1995;59:294–300. [DOI] [PubMed] [Google Scholar]
- [6].Leclercq C, Cazeau S, Le Breton H. Acute hemodynamic effects of biventricular DDD pacing in patients with end-stage heart failure. J Am Coll Cardiol 1998;32:1825–31. [DOI] [PubMed] [Google Scholar]
- [7].Ploux S, Lumens J, Whinnett Z, et al. Noninvasive electrocardiographic mapping to improve patient selection for cardiac resynchronization therapy: beyond QRS duration and left bundle branch block morphology. J AmColl Cardiol 2013;61:2435–43. [DOI] [PubMed] [Google Scholar]
- [8].Ruschitzka F, Abraham WT, Singh JP, et al. Cardiac resynchronization therapy in heart failure with a narrow QRS complex. N Engl J Med 2013;369:1395–405. [DOI] [PubMed] [Google Scholar]
- [9].El-Sherif N, Amay YLF, Schonfield C, et al. Normalization of bundle branch block patterns by distal his bundle pacing. clinical and experimental evidence of longitudinal dissociation in the pathologic his bundle. Circulation 1978;57:473–83. [DOI] [PubMed] [Google Scholar]
- [10].Lustgarten Daniel, Crespo Eric, Arkhpova-Jenkens Irina, et al. His-bundle pacing versus biventricular pacing in cardiac resynchronization therapy patients: a crossover design comparison. Heart Rhythm Journal 2015;12:1548–57. [DOI] [PubMed] [Google Scholar]
- [11].Upadhyay Gaurav A, Vijayaraman Pugazhendhi, Nayak Hemal M, et al. His corrective pacing or biventricular pacing for cardiac resynchronization in heart failure. J Am Coll Cardiol Jul 2019;74:157–9. [DOI] [PubMed] [Google Scholar]
- [12].Keene Daniel, Arnold Ahran D, Jastrzębski Marek, et al. His bundle pacing, learning curve, procedure characteristics, safety and feasibility: insights from a large international observational study. J Cardiovasc Electrophysiol 2019;30:1984–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Upadhyay Gaurav A, Cherian Tharian, Shatz Dalise Y, et al. Intracardiac delineation of septal conduction in left bundle branch block patterns: mechanistic evidence of left intra-hisian block circumvented by his pacing. Circulation 2019;139:1876–88. [DOI] [PubMed] [Google Scholar]


