Abstract
The traditional approach to penetrating injuries to zone II of the neck has included operative neck exploration, extensive enough to allow for proximal and distal vascular control of the potential vascular injury. Few studies have reported cases of entirely endovascular management of penetrating injury to this portion of the neck. In the present case report, we describe the case of a 38-year-old man who had sustained a stab wound to zone II of the neck. The injury to the internal carotid artery was managed endovascularly with placement of a covered stent. The findings from the present case illustrate the potential use of minimally invasive vascular treatment strategies as an alternative to mandated operative intervention.
Keywords: Carotid, Covered stent, Penetrating trauma
The traditional management of penetrating trauma to zone II of the neck (between the cricoid cartilage and angle of the mandible) has included neck exploration, extensive enough to allow for proximal and distal vascular control of a potential vascular injury.1 Few studies have reported on the use of covered stents in traumatic internal carotid artery (ICA) injury with good functional results.2,3 Some centers have studied nonoperative management of venous injury in the neck after penetrating trauma. However, no studies have reported on the endovascular evaluation of the venous system in penetrating neck trauma.4 To the best of our knowledge, the present study is the first to report a total endovascular approach to penetrating trauma to zone II of the neck. This novel approach was developed by the senior author (E.A.). The patient provided written informed consent for the publication of his case.
Case report
A 38-year-old man had presented to the emergency department of our Level I trauma center after sustaining a stab wound with a 2-cm laceration to zone II of the right side of his neck. The Glasgow Coma Scale score at presentation was 12. With no overt signs of hemorrhage, a computed tomography angiogram was obtained, which showed a hematoma surrounding the right ICA with irregularity and tapering of the true lumen at the level of C2 to ∼70% (Fig 1). The findings from delayed phase imaging suggested injury to the right internal jugular vein.
Fig 1.

Computed tomography angiogram of the right internal carotid showing narrowing of the true lumen.
After the wound had been inspected and cleaned in the emergency department, an enlarging hematoma along the right jawline had begun to develop, with brisk bleeding from the laceration site. He was taken emergently to the operating room after he had provided informed consent in his preferred language. Using rapid sequence induction, the patient was intubated. The right common femoral artery was accessed with ultrasound guidance. A 0.035-in. hybrid wire was used, in conjunction with a guiding catheter, to cannulate the right common carotid artery. This was followed by the placement of a 7F sheath in the common carotid artery. An arteriogram confirmed the computed tomography angiographic findings, showing narrowing of the ICA and contrast extravasation (Fig 2). Next, a 7-mm × 10-cm Viabahn covered stent (Gore Medical, Newark, Del) was placed across the injured portion of the ICA. The covered stent repaired both the bleeding segment and the stenotic area (Fig 3). A completion angiogram showed no extravasation and some redundancy of the distal ICA with slight narrowing. Intraoperatively, the patient had received 6000 U of intravenous heparin, which was reversed with 40 mg of protamine at the conclusion of the case.
Fig 2.
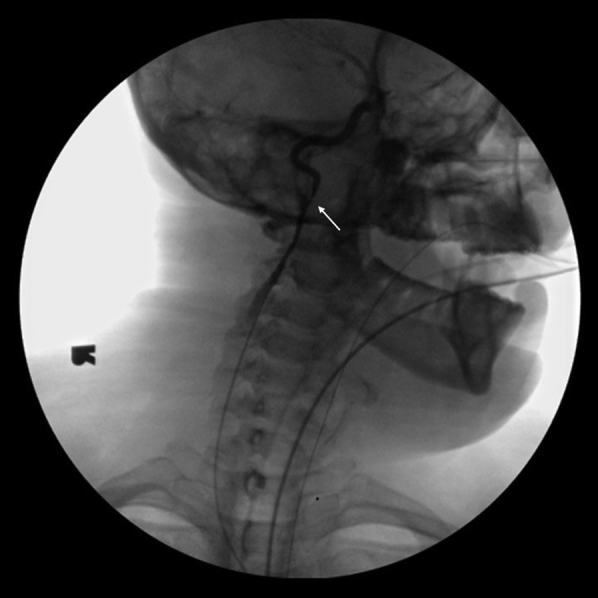
Critical stenosis of right internal carotid artery with extravasation of contrast.
Fig 3.

Right internal carotid artery after stent placement.
Attention was then turned to the venous system. The right femoral vein was accessed under ultrasound guidance. All three segments of the right internal jugular vein (intracranial segment, neck segment, and intrathoracic segment) were imaged, which demonstrated no clots or extravasation. However, extrinsic compression of the right internal jugular vein caused by the neck hematoma was found (Fig 4).
Fig 4.

Extrinsic compression of the right internal jugular vein.
An esophagogastroduodenoscopy and bronchoscopy were performed, which showed no injury to the visualized segments of the esophagus, larynx, and trachea. After the procedure, the patient began anticoagulation therapy with daily aspirin 81 mg and clopidogrel 75 mg. He was observed in the Surgical Intensive Care Unit after surgery. The patient recovered well without neurological deficits or infectious complications and no evidence of missed injury to the aerodigestive tract. Carotid duplex ultrasonography performed postoperatively demonstrated no hemodynamically significant flow disturbance in the right ICA.
He was discharged on hospital day 9 with vascular surgery and trauma surgery follow-up appointments scheduled within 1 week of discharge and prescriptions for aspirin and clopidogrel. The planned surveillance protocol included follow-up examinations every 3 months for the first year, every 6 months for the second year, and annually thereafter. The patient was followed up once in the office ∼1 month after discharge and showed no neurological deficits.
Discussion
In the mid-1950s, Fogelman and Stewart5 reported that in patients with wounds which penetrated the platysma, those who had undergone early operation had a mortality of 6% relative to 35% in those patients who underwent delayed operation. However, 50% of the cervical explorations in these patients had negative findings.5 A series of studies in the 1980s and 1990s upended the early operative exploration standard, especially for patients with moderate symptoms or signs, reporting the apparent safety of a “selective” operative approach.1
Hybrid approaches to traumatic vascular injury have been increasing in prevalence and acceptability, especially at high-volume trauma centers, where the combination of arteriography, esophagoscopy, and bronchoscopy has been shown to be highly accurate. In a study of 193 patients with penetrating neck injury at a Level 1 trauma center, arteriography was 100% accurate, the combination of bronchoscopy and laryngoscopy was 100% accurate, and esophagoscopy was 86% accurate.6 A concern with any minimally invasive approach is the possibility of missed injury. Our patient was observed in the intensive care unit postoperatively. If our patient had developed an enlarging hematoma or concern for airway compromise, an expedient return to the operating room for open exploration would have been warranted.
In the absence of large studies evaluating the effectiveness of endovascular management of the carotid artery, this minimally invasive approach might be ideal for difficult-to-access injuries (eg, distal ICA).7 Previous case reports (three patients total) documented the successful use of covered stents in carotid injury after penetrating trauma to the neck. However, these reports described injuries to the ICA within zone I or III.2,3 In the present patient, who had had an external injury within zone II but in whom the injured ICA segment was distal, neck exploration might not have been sufficient to obtain full exposure. Distal zone II injuries near the base of the skull, like the injury in the present patient, are ideally suited for treatment with endovascular stenting to avoid the morbidity of subluxation of the jaw for distal exposure.8
Management of penetrating injuries to the venous system of the neck has been less well studied than the arterial system. In one series of patients admitted for penetrating neck injuries, <10% had had any venous injury and only 2.9% had had both venous and arterial injuries.4 Approximately one half (51.3%) of the patients required operative management, usually for an associated injury. However, none the patients in the series underwent endovascular treatment.4 In our patient, we were able to image all three segments of the venous system to exclude a penetrating injury without resorting to open operative management. Had significant venous injury been identified, traditional open neck exploration would have been warranted to appropriately address the injury.
Infection is a concern with penetrating trauma, especially with insertion of a foreign body (in the present case, a covered stent) in a vessel in close proximity to the skin. Previous case reports with insertion of stents in penetrating arterial injury have not reported infectious complications.2,9 Our patient did not show any signs of infection during follow-up. Long-term outcomes data for the use of carotid stents in the young population are not available.
Conclusion
The present singular case of a penetrating injury to the distal portion of the carotid artery within zone II of the neck was managed completely endovascularly. To the best of our knowledge, the present report is the first description of a case in which both the arterial system and venous system were fully evaluated using an entirely endovascular approach. The findings have demonstrated an opportunity for total endovascular evaluation and management of traumatic vascular injury in zone II of the neck with close collaboration with trauma surgeons. Additional study of this approach is warranted to confirm our findings.
Footnotes
Author conflict of interest: none.
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Vercruysse G.A., Feliciano D.V. Neck. In: Moore E.E., Feliciano D.V., Mattox K.L., editors. Trauma. 8th ed. McGraw-Hill Education; New York, NY: 2017. [Google Scholar]
- 2.Feugier P., Vulliez A., Bina N., Floccard B., Allaouchiche B. Urgent endovascular covered-stent treatment of internal carotid artery injury caused by a gunshot. Eur J Vasc Endovasc Surg. 2007;34:663–665. doi: 10.1016/j.ejvs.2007.06.011. [DOI] [PubMed] [Google Scholar]
- 3.Kim J.P., Park J.J., Won S.J., Woo S.H. Penetrating carotid artery injuries treated by an urgent endovascular stent technique: report of two cases. Chonnam Med J. 2011;47:134. doi: 10.4068/cmj.2011.47.2.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Madsen A.S., Bruce J.L., Oosthuizen G.V., Bekker W., Laing G.L., Clarke D.L. The selective non-operative management of penetrating cervical venous trauma is safe and effective. World J Surg. 2018;42:3202–3209. doi: 10.1007/s00268-018-4595-9. [DOI] [PubMed] [Google Scholar]
- 5.Fogelman M.J., Stewart R.D. Penetrating wounds of the neck. Am J Surg. 1956;91:581–593. doi: 10.1016/0002-9610(56)90289-6. discussion: 593-6. [DOI] [PubMed] [Google Scholar]
- 6.Noyes L.D., McSwain N.E., Markowitz I.P. Panendoscopy with arteriography vs mandatory exploration of penetrating wounds of the neck. Ann Surg. 1986;204:21–31. doi: 10.1097/00000658-198607000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jacks R., Degiannis E., Jacks R. Endovascular therapy and controversies in the management of vascular trauma. Scand J Surg. 2014;103:149–155. doi: 10.1177/1457496914532248. [DOI] [PubMed] [Google Scholar]
- 8.Feliciano D.V. Management of penetrating injuries to carotid artery. World J Surg. 2001;25:1028–1035. doi: 10.1007/s00268-001-0055-y. [DOI] [PubMed] [Google Scholar]
- 9.Biagioni R.B., Burihan M.C., Nasser F., Biagioni L.C., Ingrund J.C. Endovascular treatment of penetrating arterial trauma with stent grafts. Vasa. 2018;47:125–130. doi: 10.1024/0301-1526/a000672. [DOI] [PubMed] [Google Scholar]


