Abstract
Background
Patient boarding in the emergency department (ED) is a significant issue leading to increased morbidity/mortality, longer lengths of stay, and higher hospital costs. We examined the impact of boarding patients on the ED waiting room. Additionally, we determined whether facility type, patient acuity, time of day, or hospital occupancy impacted waiting rooms in 18 EDs across a large healthcare system.
Methods
This was a retrospective multicenter study that included all ED encounters between January 1, 2018, and September 30, 2019. Encounters with missing Emergency Severity Index (ESI) level were excluded. ESI levels were defined as high (ESI 1,2), middle (ESI 3), and low (ESI 4,5). Spearman correlation coefficients measured the relationship between boarded patients and number of patients in ED waiting room. A multivariable mixed effects model identified drivers of this relationship.
Results
A total of 1,134,178 encounters were included. Spearman correlation coefficient was significant between number of patients in the ED waiting room and patient boarding (0.54). For every additional patient boarded/hour, the number of patients waiting/hour in the waiting room increased by 8% (95% confidence interval [CI] = 1.08–1.09). The number of patients waiting for a room/hour was 2.28 times higher for middle than for high acuity. The number of patients in waiting room slightly decreased as hospital occupancy increased (95% CI = 0.997–0.997).
Conclusion
Number of patients in ED waiting room are directly related to boarding times and hospital occupancy. ED waiting room times should be considered as not just an ED operational issue, but an aspect of hospital throughput.
Keywords: emergency department boarding, emergency department wait times, hospital occupancy, length of stay, crowding, waiting room
1. INTRODUCTION
Emergency department crowding is a critical problem in the delivery of emergency care. In 2007, the Institute of Medicine (now the National Academy of Medicine) reported that between 1993 and 2003, the number of hospitals and hospital beds decreased whereas the number of ED visits increased dramatically. 1 More recently, the National Hospital Ambulatory Medical Care Survey evaluated ED characteristics for 2017 and reported 139 million visits with 10.4% requiring hospital admission. 2 When hospital occupancy is at or near capacity, ED patient boarding occurs. Boarding is defined by the American College of Emergency Physicians as “a patient who remains in the ED after the patient has been admitted or placed into observation status at the facility, but has not been transferred to an inpatient or observation unit.” 3 Boarding leads to increased patient morbidity and mortality for both intensive care and non‐intensive care units, longer lengths of stay, and higher costs for the hospital. 4 , 5 , 6 , 7 , 8 , 9 , 10 Insufficient availability of inpatient beds can also lead to loss of ED revenue estimated at millions of dollars. 5 , 6 In addition to worse patient outcomes, patient satisfaction levels were reported to be lower when patients were boarded in the ED rather than being transferred to inpatient floors. 11 , 12 , 13
ED patient treatment can be divided into 3 stages: waiting room time, treatment time, and boarding time. A previous study examining 4 academic EDs demonstrated that increased wait time in 1 area cascaded into greater wait times in the other 2 areas. In particular, there was a strong correlation between acuity level, time of day, and day of week on waiting room times with one study reporting that middle level acuity patients had the longest wait times. 14 This is an important issue from a patient safety perspective since, unlike boarded patients, ED lobby patients may not have been completely evaluated by a clinician or had the full scope of medical diagnostics and treatment initiated.
Although previous smaller studies have been able to define the relationship between ED lobby wait times and ED boarding, there is little data connecting these variables to hospital throughput and occupancy as a whole. A few studies from Western Australia have examined this issue since the State Health Department implemented the “4 h rule” that targeted hospital systems to meet a goal of total ED time from arrival to departure in 4 hours or less. One prospective study published from a 600‐bed tertiary care hospital in 2017 found that multi‐level intervention with involvement of ED medical staff, Director of Operations, and creation of a “long length of stay committee” with a flow (bed management) unit showed improvement in daily crowding over 20 weeks. This study demonstrated that hospital involvement, not just ED interventions, are essential to improvement in boarding. 15 Another study from Australia set out to improve ED flow by placing inpatient discharge targets. Their results demonstrated that average time for ED patients waiting on an inpatient bed improved. 16 However, neither of these studies examined more than 1 hospital, were performed within US hospitals, or adjusted for hospital occupancy effects on ED lobby wait times.
The Bottom Line
The number of patients in the emergency department waiting room is directly related to boarding times and hospital occupancy. ED waiting room times should be considered as not just an ED operational issue, but an aspect of hospital throughput.
The primary goal of our study was to determine if the number of patients boarded in the ED affects patient number of patients in the ED waiting room over a broad array of hospital facilities in a large integrated health system. Additionally, we sought to determine the relationship of secondary variables that influence number of patients in the ED waiting room, such as ED facility type, patient acuity defined by Emergency Severity Index (ESI) triage acuity levels, time of day (daytime or nighttime), and hospital occupancy.
2. METHODS
2.1. Study design
This was a retrospective multicenter study that included 18 EDs across the healthcare system. This study was approved by the Institutional Review Board of the healthcare system.
2.2. Setting
All EDs in the healthcare system were included in analysis. The EDs were placed into 3 categories: high volume hospital‐based ED, low volume hospital‐based ED, and free‐standing ED. A hospital‐based ED was categorized as high volume if the hospital saw more than 50,000 patients per year. Of the 18 EDs included in the analysis, 4 were classified as high volume hospital‐based ED, 8 were classified as low volume hospital‐based ED, and 6 were classified as free‐standing ED. Demographics for each ED are reported (Table 1). All patients who arrived to one of the EDs within the healthcare system and received an ESI score were included in the analysis.
TABLE 1.
Characteristics of hospital emergency departments within the healthcare system during the study period
| ICU | External Hospital (transfers out of healthcare system) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| ED | Teaching status | Trauma status | ED volume | Admissions/transfers(%) | Discharges (%) | EMS arrivals (%) | % of admissions/transfers | % of ED volume | % of admissions/transfers | % of ED volume |
| Higher‐volume HBED (based on annual >50,000 ED visits) | ||||||||||
| D | EM | Level I | 97,692 | 37.2 | 54.3 | 32.1 | 11.8 | 4.4 | 4.7 | 1.7 |
| I | Non‐EM | Level II | 112,377 | 34.6 | 61.2 | 25.4 | 14.4 | 5.0 | 1.1 | 0.4 |
| L | Non‐EM | Level II | 90,034 | 40.1 | 55.5 | 29.9 | 10.2 | 4.1 | 1.0 | 0.4 |
| P | EM | None | 115,481 | 29.9 | 64.8 | 25.2 | 13.7 | 4.1 | 1.9 | 0.6 |
| Lower‐volume HBED (based on annual <50,000 ED visits) | ||||||||||
| A | NT | None | 59,037 | 19.1 | 77.3 | 18.9 | 10.7 | 2.0 | 7.0 | 1.3 |
| F | NT | None | 73,347 | 26.7 | 71.8 | 11.2 | 8.1 | 2.2 | 2.4 | 0.7 |
| H | NT | None | 74,689 | 17.8 | 79.1 | 19.5 | 12.7 | 2.3 | 5.6 | 1.0 |
| K | NT | None | 68,602 | 28.4 | 69.6 | 11.6 | 5.3 | 1.5 | 9.5 | 2.7 |
| O | NT | None | 65,508 | 17.3 | 78.8 | 14.5 | 11.2 | 1.9 | 8.3 | 1.4 |
| Q | NT | None | 76,068 | 22.0 | 75.0 | 24.7 | 15.4 | 3.4 | 5.8 | 1.3 |
| R | NT | None | 45,623 | 32.7 | 64.9 | 21.2 | 10.6 | 3.5 | 6.3 | 2.1 |
| S | EM (2018) | None | 63,396 | 24.1 | 72.0 | 19.9 | 15.8 | 3.8 | 3.6 | 0.9 |
| FSED | ||||||||||
| B | EM | None | 32,640 | 11.2 | 86.3 | 5.6 | 6.6 | 0.7 | 13.3 | 1.5 |
| C | NT | None | 28,548 | 10.5 | 87.6 | 4.6 | 6.0 | 0.6 | 13.2 | 1.4 |
| E | EM | None | 31,743 | 10.7 | 87.6 | 5.3 | 5.8 | 0.6 | 15.2 | 1.6 |
| G | NT | None | 28,243 | 17.4 | 80.7 | 11.9 | 11.6 | 2.0 | 9.8 | 1.7 |
| N | NT | None | 32,685 | 11.0 | 86.4 | 10.7 | 10.9 | 1.2 | 15.8 | 1.7 |
| T | NT | None | 38,465 | 20.7 | 76.9 | 14.0 | 12.4 | 2.6 | 12.3 | 2.6 |
| Overall | ||||||||||
| 1,134,178 | 25.9% | 70.3% | 19.9 | 11.6 | 3.0 | 4.7 | 1.2 | |||
EM, EM rotation; FSED, free standing ED; Non‐EM, non‐EM Rotation; NT, non‐teaching.
Teaching status: refers to whether a site hosts EM resident trainees, non‐EM resident trainees, or no resident trainees.
A traditional ED triage system was used. Once a bed was available, patients were either taken to a fast track or regular patient care area from the ED waiting room. Critically ill patients were immediately brought back to the ED. Patients who arrived via EMS were generally taken straight to an ED room with triage completed at bedside. However, at peak hours, non‐critically ill EMS patients may have been placed in the waiting room.
Patients that were being transferred for admission at another hospital waited in the ED at the original location until a bed was assigned. It was not a system practice for patients to be transferred to the receiving hospital's ED for boarding. Thus, free standing EDs were also subject to boarding.
All sites used the same electronic medical record system (EPIC, Verona, WI) allowing for data acquisition across the system. The electronic medical record allowed for the recording and subsequent retrieval of all discrete time stamps of significant events throughout the patient stay.
2.3. Data collection
All patients who presented to an ED within the system and seen between January 1, 2018 and September 30, 2019 were included in the analysis. The only exclusion criteria was any encounter with missing acuity level on initial chart review.
The ESI is a standardized 5‐level triage algorithm that categorizes ED patients based on acuity (stability of vital signs and potential threat to life) and resource needs. 17 Acuity level on all patients in the system was recorded and was used to categorize Levels 1–5 with the following definitions: ESI Levels 1 and 2 considered high acuity, ESI Level 3 considered “middle acuity,” and ESI Levels 4 and 5 considered “low acuity.” Any encounter for which there was a missing ESI acuity level was excluded from analysis. For the purposes of the study, the ESI acuity levels as listed above were created to examine differences across acuity levels.
Additional data were collected on all encounters based on discrete time stamps from the electronic medical record using standard definitions at the beginning of the hour. ED arrival was defined as the time when the patient presented to the ED and was entered into the electronic medical record. Boarding time was defined from time of disposition as set by provider to time of departure from the ED at all sites, including free standing EDs. 18 Number of boarded patients per hour was recorded throughout the entire study period. ED waiting room was defined as the number of patients per hour waiting to be roomed in the ED and was recorded by hour for the entire study period. Hourly hospital occupancy for the study period was determined by hospital census dashboard and was updated every hour. Hospital census was determined by including only available staffed beds. Closed beds were excluded. Each hospital had their own dashboard consisting of medical/surgical and critical care beds available for that hospital that served adult (≥18 years old) patients. The dashboard was extracted from the same electronic medical record. For the hospital occupancy analysis, free standing EDs were excluded as they do not have inpatient beds available for patients to be admitted. Last, hours of the day for which patients arrived was also abstracted from the data. Daytime was defined as 8:00 am to 7:59 pm and nighttime was defined as 8:00 pm to 7:59 am.
Data were extracted from the medical record, de‐identified and imported into SAS (Cary, NC). Initial statistical analysis used Spearman correlation coefficients to determine if the number of waiting patients in the lobby was correlated with the number of boarding patients; this analysis was also repeated by ED category (high volume hospital‐based ED, low volume hospital‐based ED, and free standing ED). To overcome the violation of the assumptions required for Spearman correlation coefficients, a linear mixed effects model (with a log transformed outcome) was used to identify factors that drove the outcome variable and number of patients waiting per hour. The variables included in the model were: number of boarded patients, ED category, ESI acuity groups, time of day, and percent of occupied hospital beds. Additionally, each ED was treated as a random variable.
3. RESULTS
A total of 1,134,178 encounters were included in this analysis. 16,996 encounters (1.5%) were excluded for missing ESI acuity level triage scoring. We first examined whether there was a positive correlation between number of ED patients in the waiting room and patient boarding. Our analysis showed a system‐level significant Spearman correlation coefficient of 0.54 (Table 2). The high volume hospital‐based EDs had the highest Spearman correlation coefficient of 0.48, demonstrating that the number of patients in the ED waiting room at these sites had a strong positive relationship to number of patients boarding. low volume hospital‐based ED and free standing ED were considered significant as well with Spearman correlation coefficients of 0.34 (P < 0.0001) and 0.26 (P < 0.0001), respectively (Figure 1; Table 2).
TABLE 2.
Relationship between patients awaiting an ED room and ED boarding for all hospital types
| Spearman correlation coefficient | n | P | |
|---|---|---|---|
| All EDs | 0.54 | 275,616 | <0.0001 |
| HV HBED | 0.48 | 61,248 | <0.0001 |
| LV HBED | 0.34 | 122,496 | <0.0001 |
| FSED | 0.26 | 91,872 | <0.0001 |
FSED, free‐standing ED; HV HBED, high volume hospital‐based ED; LV HBED, low volume hospital‐based ED.
FIGURE 1.
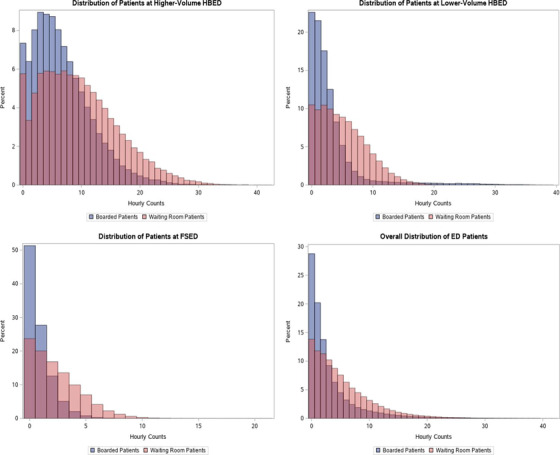
Correlation between waiting room patients and boarding patients for emergency departments
After determining a positive correlation between number of patients in the ED waiting room and ED boarding, a secondary analysis found that for every additional patient boarded per hour, the number of ED patients in the waiting room in an hour would be expected to increase by a factor of 1.08, or an 8% increase (95% CI = 1.08–1.09), assuming that the other variables are held constant in the model (Table 3). With regard to the effect of ESI acuity triage levels on number of patients in the ED lobby, our study found that the number of patients waiting for a ED room per hour was 2.28 times higher for middle level acuity (ESI 3) than for high level acuity (ESI 1 or 2), and the number of patients waiting for a ED room per hour was 1.5 times (50%) higher for low acuity (ESI 4 or 5) compared to high acuity (ESI 1 or 2) (Table 3). Time of day also had an effect on number of patients in the ED waiting room. The number of patients waiting at night decreased by a factor of 0.63 compared to daytime (95% CI = 0.63–0.64). Additionally, high volume hospital‐based EDs had 40% more patients waiting per hour than low volume hospital‐based EDs (Table 3). Last, the secondary analysis demonstrated that as percent of hospital beds occupied increases, the number of patients waiting in the ED waiting room declines slightly. (95% CI = 0.997, 0.997) (Table 3).
TABLE 3.
Mixed effects model of number of ED patients in waiting room
| Effect | Level | Estimate (95% CI) | P |
|---|---|---|---|
| (Intercept) |
1.99 (1.86, 2.13) |
<0.001 | |
| Number of patients boarded |
1.08 (1.08, 1.08) |
<0.001 | |
| ESI acuity groups | Middle (vs high) |
2.28 (2.27, 2.29) |
<0.001 |
| Low (vs high) |
1.50 (1.50, 1.51) |
<0.001 | |
| Time of day | Night time: 8 pm–7:59 am (vs daytime) |
0.63 (0.63, 0.64) |
<0.001 |
| ED category | HV HBED (vs LV HBED) |
1.40 (1.24, 1.58) |
<0.001 |
| Percent occupied beds |
0.997 (0.997, 0.997) |
<0.001 |
CI, confidence interval; HV HBED, high volume hospital‐based ED; LV HBED, low volume hospital‐based ED.
When examining admission rate and lobby waiting time by acuity group, our study found a 26.52% admission rate for middle level acuity (ESI 3). High acuity (ESI 1 and 2) had an admission rate of 63.96% and low acuity (ESI 4 and 5) had an admission rate of 1.44%. Additionally, waiting room time significantly different amongst acuity groups with the middle acuity group having the largest mean waiting room time at 23.2 (SD 69.8) (Table 4).
TABLE 4.
Waiting room time and admission rates amongst different acuity groups
| Acuity group | Mean in minutes (SD) | Median in minutes [IQR] | P (vs high) a | P (vs middle) a | Admission rate (%) |
|---|---|---|---|---|---|
| Low (ESI 4 and 5) | 17.6 (33.6) | 9 [4, 19] | <0.0001 | <0.0001 | 1.44 |
| Middle (ESI 3) | 23.2 (69.8) | 8 [2, 18] | <0.0001 | 26.52 | |
| High (ESI 1 and 2) | 14.0 (82.8) | 3 [0, 10] | 63.96 |
All P values are pairwise comparison (Kruskal–Wallis).
4. LIMITATIONS
The potential limitations for this study include those inherent to all retrospective studies and include sampling bias, measurement bias, and classification bias. Some patient encounters did not include an ESI acuity level and those were excluded from our study sample, although this number was small (1.5%). This study was conducted in a single large healthcare system in a particular geographic region of the country which may limit generalizability. However, because all encounters within the study period were included, the sheer number of encounters and narrow confidence intervals strengthens our notion that the number of patients ED waiting room can be directly correlated to ED boarding. We also were able to include different types of EDs, thereby accounting not only for large academic and tertiary care centers but also lower volume community EDs and free standing EDs. Although ED beds may expand and contract during different hours of the day or as a function of ED staffing, this was unable to be accounted for in our analysis. This study was based in a US healthcare system and may not be generalizable to hospital systems outside the United States.
As free standing EDs in our system lack inpatient or observation facilities, these patients were generally transferred to either a high volume hospital‐based ED or low volume hospital‐based ED within the system in the event of a patient admission. Rarely, an outside‐the‐system patient transfer occurred (<5%) (Table 1). However, given the low frequency of this event, it was unlikely to skew the results.
The hospital occupancy data were also limited as it was extracted from a dashboard of adult medical/surgical and critical care bed availability, which may have over‐reported true bed availability as well as available staffing for that hospital bed. Although the hospital does report number of closed beds as of midnight, this number may have been adjusted and not reflected in real‐time on the dashboard. Additionally, OBGYN, pediatrics, and behavioral health beds were not counted.
Last, it is possible ED staffing may have limited ED bed availability. EDs across the country vary their staffing depending on time of day and day of the week. Challenges such as nursing call‐offs that may impact ED bed availability are difficult to control for in large retrospective studies but could be a potential area for future study. However, we are unable to obtain that data and thus is a confounder.
5. DISCUSSION
Our study demonstrates that the number of ED patients in the waiting room awaiting an ED bed is directly correlated to ED boarding. The strength of this correlation indicates that ED waiting room times, much like ED boarding, should be considered a system‐wide hospital concern and not a localized ED issue and that moving patients from boarding status into hospital rooms could help decrease ED lobby wait times. The value of our analysis was strengthened by the fact that this phenomenon was replicated across multiple sites with varying volumes within our large healthcare system. Likewise, across our multiple site healthcare system, our study accounted for the effects of hospital occupancy on ED patient throughput and found that as more patients move into inpatient beds and occupy the hospital, the number of patients in the ED lobby decreases, thereby strengthening the premise that the number of patients in the ED waiting room are a reflection of hospital throughput.
To our knowledge, this is the first study to examine ED boarding over a large number of hospitals encompassing greater than 1 million patient encounters in the United States. Our analysis was strengthened by the inclusion of different types of EDs, including high volume hospital‐based EDs, low volume hospital‐based EDs and free standing EDs. Our analysis found that the high volume hospital‐based EDs within the system had the strongest predictor of having an association between ED boarding and increased number of patients in the ED waiting room. This would be expected as these hospitals in our system are usually at full occupancy and serve as referral centers for accepting patients from hospitals outside the health system as well as from low volume hospital‐based ED and free standing ED within the system. Additionally, although all HBEDs had inpatient beds, the low volume hospital‐based EDs did transfer patients to HV hospitals as there are a certain subset of patients who require inpatient specialty services that may not be available at a smaller community hospital offered by a low volume hospital. With the lower volumes at these sites, there may have been less boarding and therefore the low volume hospital‐based EDs may have had shorter wait times compared to the high volume hospital‐based EDs, explaining the smaller spearman correlation coefficient. However, in our healthcare system, to offload boarding times at high volume hospital‐based EDs, patients with limited subspecialty needs (including intensive care unit patients) may have been transferred to low volume hospitals that had capacity and the ability to care for the patient. We therefore categorized admissions and transfers together.
As expected, ESI levels 1 and 2 (high acuity) had the shortest ED wait times. Surprisingly, moderate acuity (ESI level 3) had the longest wait times. This likely reflects wide‐spread adoption of ED split flow or fast track areas and processes to expedite care for low acuity (ESI levels 4–5) patients. This warrants further examination, because ESI level 3 patients often require hospitalization (with ED admission rates in our system of 26.52% for ESI level 3 compared to 25.9% for all patients in the system). It was important for us to study ESI levels, because we were interested in how hospital occupancy and number of patients in the ED lobby affected our high acuity patient population.
As an additional secondary outcome, we accounted for hospital occupancy in relation to number of patients in the ED waiting room. To our knowledge, this is the first large scale study in the United States to attempt to account for hospital occupancy and its effects on ED boarding and ED waiting room times. We excluded free‐standing EDs from this data analysis as free standing ED facilities lacked inpatient services and did not preferentially admit to one facility over another (usual practice was to look for the closest hospital with an available bed). This may have reduced their overall boarding times. Likewise, as stated above, low volume hospital‐based EDs transferred patients as needed to the high volume hospital‐based ED facilities when acuity dictated. The relationship to hospital occupancy was less pronounced at low volume hospital‐based EDs as we examined the relationship between the number of patients in the ED lobby and hospital occupancy only at each site and not between sites.
The overall relationship between hospital occupancy and number of patients in the ED waiting room found that as hospital occupancy increased, there was a very slight decrease in the number of patients in the ED waiting room. Hospital occupancy is a multi‐factorial as there are many variables that affect occupancy. In our healthcare system, bed control is affected by patients coming in from hospitals outside the healthcare system, post‐surgical patients requiring beds, transfers from other hospitals within our system, bed closures, and nursing/staffing issues. We attempted to examine this relationship and found that as more patients are placed into hospital beds within the hospital, there is a slight decrease in the number of patients in the ED waiting room. As we expect, this is not a 1:1 relationship due to the other factors listed above, meaning that for every patient that gets placed in a hospital bed, we do not see the waiting room decrease by one. Rather, the patients getting placed in beds can be from many other areas within the system (out‐of‐hospital transfers, post‐surgical, in‐hospital transfers, etc). We do see a slight decrease demonstrating that moving patients into hospital beds does trickle down to affect the number of patients in the ED waiting room. Additionally, EMS traffic could be a variable that may have affected ED waiting room times as sites with increased EMS volume may prevented patients from being roomed faster from the waiting room.
Although we have described a correlative relationship between ED boarding and number of patients in the ED waiting room, we were unable to discern the functional causality of the relationship, where boarding results in a backed up department thus increasing wait times for initial evaluation or, inversely, whereby many people in the waiting room results in more admissions, leaving the remaining people in the waiting room to accumulate. Finally, it is possible that a relationship with both, or neither, causal elements may be in effect. For example, busy days are busy days and yield patients both waiting for beds at admission and waiting in the waiting room. However, regardless of the direction of the causal relationship, the result is that to decrease the number of patients in the ED waiting room, hospital occupancy should be taken into account.
With health system leadership focused on patient experience while decreasing ED patients who left without being seen or left before triage complete, attention has been focused on ED leadership to strategize plans to reduce these numbers. The findings of our study suggest that these ED metrics are not solely the purview of ED leadership, rather it is a multi‐factorial problem that is related to ED throughput which is, in turn, related to hospital throughput. Given our findings, health system leaders should consider number of patients in the ED waiting room a hospital‐wide issue and a reflection of overall hospital crowding.
6. CONCLUSION
Number of patients in the ED waiting room across a large multi‐hospital healthcare system were directly correlated to ED boarding. Additionally, this number also correlated with hospital occupancy data. Our results indicate that number of patients in the ED waiting room should be considered as an aspect of hospital throughput and not simply an ED operational issue. Further studies should assess interventions from an administrative hospital level to increase patient flow to help alleviate patient boarding and ED waiting room times.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
AUTHOR CONTRIBUTIONS
All authors contributed to the manuscript. CS takes responsibility of the final manuscript.
Biography
Courtney Smalley, MD, is an emergency physician at Cleveland Clinic, Cleveland, OH.

Smalley CM, Simon EL, Meldon SW, et al. The impact of hospital boarding on the emergency department waiting room. JACEP Open. 2020;1:1052–1059. 10.1002/emp2.12100
Funding and support: By JACEP Open policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist.
Supervising Editor: Chadd K. Kraus, DO, DrPH.
REFERENCES
- 1. Institute of Medicine . Hospital‐Based Emergency Care: At the Breaking Point. Washington, DC: The National Academies Press; 2007. 10.17226/11621. [DOI] [Google Scholar]
- 2. Rui P, Kang K. National Hospital Ambulatory Medical Care Survey: 2017 Emergency Department Summary Tables. National Center for Health Statistics; Available at: https://www.cdc.gov/nchs/data/nhamcs/web_tables/2017_ed_web_tables-508.pdf. Accessed April 17, 2020. [Google Scholar]
- 3. Definition of boarded patient. Ann Emerg Med. 2019;73(3):e23. [DOI] [PubMed] [Google Scholar]
- 4. Reznek MA, Upatising B, Kennedy SJ, Durham NT, Forster RM, Michael SS. Mortality associated with emergency department boarding exposure: are there differences between patients admitted to ICU and non‐ICU settings? Med Care. 2018;56(5):436‐440. [DOI] [PubMed] [Google Scholar]
- 5. Schreyer KE, Martin R. The economics of an admissions holding unit. West J Emerg Med. 2017;18(4):553‐558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Falvo T, Grove L, Stachura R, et al. The opportunity loss of boarding admitted patients in the emergency department. Acad Emerg Med. 2007;14(4):332‐337. [DOI] [PubMed] [Google Scholar]
- 7. Rabin E, Kocher K, McClelland M, et al. Solutions to emergency department “boarding” and crowding are underused and may need to be legislated. Health Aff. 2012;31(8):1757‐1766. [DOI] [PubMed] [Google Scholar]
- 8. Al‐Qahtani S, Alsultan A, Haddad S, et al. The association of duration of boarding in the emergency room and the outcome of patients admitted to the intensive care unit. BMC Emerg Med. 2017;17(1):34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Andrew Taylor R, Venkatesh A, Parwani V, et al. Applying advanced analytics to guide emergency department operational decisions: a proof‐of‐concept study examining the effects of boarding. Am J Emerg Med. 2018;36(9):1534‐1539. [DOI] [PubMed] [Google Scholar]
- 10. Singer AJ, Thode HC, Viccellio P, Pines JM. The association between length of emergency department boarding and mortality. Acad Emerg Med. 2011;18(12):1324‐1329. [DOI] [PubMed] [Google Scholar]
- 11. Garson C, Hollander JE, Rhodes KV, Shofer FS, Baxt WG, Pines JM. Emergency department patient preferences for boarding locations when hospitals are at full capacity. Ann Emerg Med. 2008;51(1):9‐12, 12.e1‐3. [DOI] [PubMed] [Google Scholar]
- 12. Viccellio P, Zito JA, Sayage V, et al. Patients overwhelmingly prefer inpatient boarding to emergency department boarding. J Emerg Med. 2013;45(6):942‐946. [DOI] [PubMed] [Google Scholar]
- 13. Richards JR, Ozery G, Notash M, Sokolove PE, Derlet RW, Panacek EA. Patients prefer boarding in inpatient hallways: correlation with the National Emergency Department Overcrowding Score. Emerg Med Int. 2011;2011:840459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ding R, McCarthy ML, Desmond JS, Lee JS, Aronsky D, Zeger SL. Characterizing waiting room time, treatment time, and boarding time in the emergency department using quantile regression. Acad Emerg Med. 2010;17(8):813‐823. [DOI] [PubMed] [Google Scholar]
- 15. Richardson DB, Brockman K, Abigail A, Hollis GJ. Effects of a hospital‐wide intervention on emergency department crowding and quality: a prospective study. Emerg Med Australas. 2017;29(4):415‐420. [DOI] [PubMed] [Google Scholar]
- 16. Khanna S, Sier D, Boyle J, Zeitz K. Discharge timeliness and its impact on hospital crowding and emergency department flow performance. Emerg Med Australas. 2016;28(2):164‐170. [DOI] [PubMed] [Google Scholar]
- 17. Agency for Healthcare Research and Quality . Emergency Severity Index: a triage tool for emergency department care, Version 4. 2012. Edition. https://www.ahrq.gov/sites/default/files/wysiwyg/professionals/systems/hospital/esi/esihandbk.pdf
- 18. Welch SJ, Stone‐Griffith S, Asplin B, et al. Emergency department operations dictionary: results of the second performance measures and benchmarking summit. Acad Emerg Med. 2011;18(5):539‐544. [DOI] [PubMed] [Google Scholar]


