Abstract
Background
A significant number of patients who present to the emergency department (ED) following a fall or with other injuries require evaluation by a physical therapist. Traditionally, once emergent conditions are excluded in the ED, these patients are admitted to the hospital for evaluation by a physical therapist to determine whether they should be transferred to a sub‐acute rehabilitation facility, discharged, require services at home, or require further inpatient care. Case management is typically used in conjunction with a physical therapist to determine eligibility for recommended services and to aid in placement.
Objective
To evaluate the benefit of using ED‐based physical therapist and case management services in lieu of routine hospital admission.
Methods
Retrospective, observational study of consecutive patients presenting to an urban, tertiary care academic medical center ED between December 1, 2017, and November 30, 2018, who had a physical therapist consult placed in the ED. We additionally evaluated which of these patients were placed into ED observation for physical therapist consultation, how many required case management, and ED disposition: discharged home from the ED or ED observation with or without services, placed in a rehabilitation facility, or admitted to the hospital.
Results
During the 12‐month study period, 1296 patients (2.4% of the total seen in the ED) were assessed by a physical therapist. The mean age was 75.5 ± 15.2 and 832 (64.2%) were female. Case management was involved in 91.8% of these cases. The final patient disposition was as follows: admission 24.3% (95% CI = 22.1–26.7%), home discharge with or without services 47.8% (95% CI = 45.1–50.5%), rehabilitation (rehab) setting 27.9% (95% CI = 25.6%–30.4). The median (interquartile range) time in observation was 13.1 (6.0–20.3), 9.9 (1.8–15.8), and 18.4 (14.1–24.8) hours for patients admitted, discharged home, or sent to rehabilitation (P < 0.001). Among the 979 patients discharged home or sent to rehabilitation, 17 (1.7%) returned to the ED within 72 hours and were ultimately admitted.
Conclusion
Given that the standard of care would otherwise be an admission to the hospital for 1 day or more for all patients requiring physical therapist consultation, an ED‐based physical therapy and case management system serves as a viable method to substantially decrease hospital admissions and potentially reduce resource use, length of hospital stay, and cost both to patients and the health care system.
Keywords: case management, hospital admission reduction, observation units, pathways, physical therapy, rehabilitation placement
1. INTRODUCTION
Given the cost of health care, providing cost‐effective high‐quality care is increasingly necessary, often by streamlining existing services to decrease expenses. In particular, there is scrutiny on the part of insurers to reduce short‐term hospitalizations. 1 Emergency departments are using observation units as efficient modalities for implementing clinical pathways that allow for more rapid evaluation, testing, treatment, and disposition of patients while avoiding inpatient hospital admission. 2 , 3 , 4
A significant number of patients who present to the ED may be unsafe to return home in their current state—whether it be from a fall, deconditioning, or illness—and could benefit from evaluation by a physical therapist. Traditionally, once emergent conditions requiring inpatient hospitalization and treatment were excluded in the ED, these patients were admitted to the hospital primarily for evaluation by a physical therapist. The physical therapist would then determine whether they would benefit from ongoing rehabilitation services at a rehabilitation facility, rehabilitation with home‐based services, or whether they could be safely discharged back to their home. Case management is typically used in conjunction with physical therapy to determine eligibility for recommended services and to aid in placement. We instituted a novel ED‐based physical therapist consult service to avoid hospital admission when possible. Because physical therapist evaluation typically occurs as an inpatient, the use of an ED observation unit as a venue for physical therapist evaluation and subsequent placement into rehabilitation or provision of home rehabilitation services is not welldescribed in the current literature.
In this study, we present the results of an assessment of the initial outcomes of patients evaluated by ED‐based physical therapists. The goal of this study was to demonstrate that this novel clinical pathway is safe, viable, and reduces hospital admission in this cohort of patients.
2. METHODS
We examined patients presenting to our ED between December 1, 2017 and November 30, 2018, who had a physical therapist consult placed in the ED, in an urban, tertiary care academic medical center ED with an annual volume of ∼55,000 patients. We established an ED‐based physical therapist consult service in 2012. This, coupled with pre‐existing ED case management, enables rapid evaluation and disposition of patients who otherwise would have required inpatient observation or admission for their management.
At the conclusion of a patient's ED evaluation, once acute medical conditions have been addressed or excluded and the patient is deemed medically cleared for discharge, a bedside ambulation trial is performed. If the patient is unable to satisfactorily complete this, a physical therapist and case management consult is placed. Consults were placed at the discretion of the emergency physician team that often consisted of a primary resident, senior resident, and attending physician. Patients with an anticipated prolonged ED length of stay were placed in observation status and were clinically re‐evaluated by an attending physician every 24 hours. If a medical issue evolved during the patient's ED stay and if they were deemed no longer safe for discharge, or if on re‐evaluation the patient was felt to no longer require a physical therapy evaluation, they were removed from observation and their disposition was adjusted accordingly.
The physical therapist makes recommendations regarding patient suitability for rehabilitation placement or home rehabilitation services. Case management facilitates these recommendations by submitting clinical information to patients’ insurance providers to facilitate placement and identifies which patients will require inpatient admission for insurance to reimburse rehabilitation placement. Case management also works with patients and their family members to determine eligibility for services and arrange for the best options for families based on insurance coverage and their financial resources.
Patients were excluded if the physical therapist consult was not completed. Reasons for incomplete consults included changes in disposition such as identification of a medical problem warranting admission, clinical re‐evaluation determining that a consult was no longer needed, the patient refusing to work with the physical therapist, and leaving against medical advice or eloping (Figure 1).
FIGURE 1.
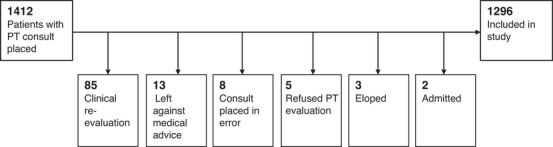
Exclusion criteria
We extracted de‐identified patient data from the electronic medical record, including patient demographics, Emergency Severity Index, chief complaint, consults placed, length of stay in the ED and inpatient settings, time spent in ED observation, and ED disposition. ED dispositions included discharges to home with home physical therapy or visiting nurse association (VNA) services, discharges to home without services, transfers to rehabilitation facilities, or admissions to the hospital. Patient disposition was coded using the preliminary recommendations left by physical therapist and case management as recorded in the electronic medical record. In cases where a physical therapist recommended a course of action that a patient did not comply with, we retained the original recommendation. Chief complaints were selected by the triage nurse from a list of pre‐selected categories. For the purposes of this study, these were sub‐categorized into the following groupings: Fall, Musculoskeletal, Back pain, Neurologic, Cardiopulmonary, Gastrointestinal, Generalized Weakness, and Other (Supporting Information Table S1).
To assess the safety of our intervention, we additionally identified patients that re‐presented to the ED within 72 hours and examined their disposition during their re‐presentation to ascertain whether these patients had been properly assessed and dispositioned during their initial presentation.
A physical therapist was available as a consult service in the ED from 8 am–5 pm 7 days a week. Depending on daily staffing availability, a dedicated physical therapist was assigned to the ED or the ED assignment was split between multiple floor physical therapists. ED consults were prioritized over inpatient evaluations, because ED physical therapist evaluations constitute possible barriers to discharge. Consults were placed electronically via the ED electronic medical record with a time stamp as well as a posted forum for physical therapist to communicate their recommendations to the team in real time (Figure 2). Case management services were available 7 am–10 pm Monday through Friday and 7 am–7 pm on weekends and holidays. When consults for physical therapist and case management were placed off‐hours, this was noted on a shared electronic medical record space so that when these services returned, they were immediately able to see those patients waiting in the ED for their recommendations and professional services.
FIGURE 2.
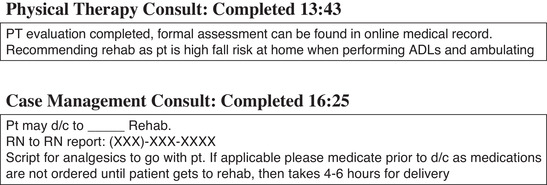
Example of physical therapist and case management recommendations from the electronic medical record. ADL, activities of daily life
The Bottom Line
Physical therapy in the emergency department is a unique concept that may result in improved and expedited patient care, reduction in hospital admissions, and costs to patients and the health care system. In this study of 1296 ED patients receiving physical therapy consultation, 979 (76%) were able to be discharged home or sent to rehabilitation. Only 17 (1.7%) returned to the ED within 72 hours.
Data were summarized overall and by disposition category. Statistical comparisons across disposition category were performed with a χ2 test for categorical variables. ED length of stay was not normally distributed, so a Kruskal‐Wallis test was performed to compare ED length of stay across disposition categories.
3. RESULTS
In total, 1412 patient encounters were identified where a physical therapist consult was placed in the ED over the study period. Of these, 108 physical therapist consults were not completed, and 8 consults were placed in error, leaving 1296 patients (2.4% of the total seen in the ED during the study period) to be included in the study (Figure 1). A total of 359 patients were discharged to rehabilitation (27.7%), 389 were discharged home with additional services (30.0%), 231 were discharged home without services (17.8%), and 317 (24.5%) were admitted. The most common chief complaints were Fall (40.0%) and Musculoskeletal (19.4%), followed by Neurologic (12.2%), Back Pain (11.7%), Other (5.3%), Weakness (3.9%), Cardiopulmonary (3.7%), and Gastrointestinal (3.7%). 64.2% of patients were female, the average age was 74, 91.8% had a case management consult placed, and 81.0% spent time in ED observation status (Table 1).
TABLE 1.
Descriptive summary of visits with a physical therapy consult placed in the emergency department, December 1, 2017–November 30, 2018
| Visit characteristic | Number (n = 1296) | Percent |
|---|---|---|
| Emergency Severity Index level | ||
| 1 | 40 | 3.1 |
| 2 | 433 | 33.4 |
| 3 | 785 | 60.6 |
| 4 | 38 | 2.9 |
| Sex | ||
| Female | 832 | 64.2 |
| Male | 464 | 35.8 |
| Case management consult | 1190 | 91.8 |
| Time spent in ED observation | 1050 | 81.0 |
| Disposition | ||
| Admitted | 317 | 24.5 |
| Home without services | 231 | 17.8 |
| Home with services | 389 | 30.0 |
| Rehabilitation | 359 | 27.7 |
| Chief complaint | ||
| Fall | 519 | 40.0 |
| Musculoskeletal | 252 | 19.4 |
| Neurologic | 158 | 12.2 |
| Back pain | 151 | 11.7 |
| Other | 69 | 5.3 |
| Weakness | 51 | 3.9 |
| Cardiopulmonary | 48 | 3.7 |
| Gastrointestinal | 48 | 3.7 |
| Age (mean, SD) | 74 | 15.2 |
The ED length of stay varied significantly by disposition group (Figure 3, P < 0.0001). Among patients admitted to the hospital the median ED length of stay was 24.3 hours. For those discharged home without services the median ED length of stay was 16.8 hours, for those discharged home with services the median ED length of stay was 19.1 hours, and for those discharged to a rehabilitation facility the median ED length of stay was 28.6 hours. Case management consultation varied significantly by disposition category (P < 0.0001). Case management was consulted for 100% of patients transferred to rehab, 97.7% of patients discharged home with services, 87.1% of patients that were admitted, and in 75.8% of patients discharged home without services (Figure 3).
FIGURE 3.
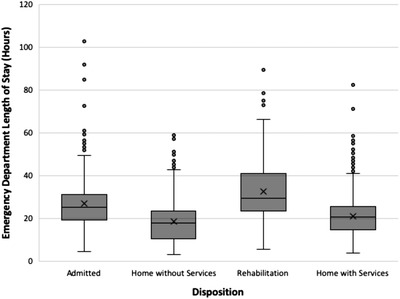
Comparison of patients with a physical therapy consult placed in the ED across disposition categories
Data were further analyzed by chief complaint category subgroups (Table 2). Emergency Severity Index level, sex, case management consult, and final disposition were compared. Approximately 85% of patients with a fall‐related chief complaint or those categorized as “other” spent time in observation status, compared to about 75% of patients with a chief complaint that was cardiopulmonary or back pain. Patients with a chief complaint of gastrointestinal illness or “other” had the highest rate of being admitted (33% and 42%, respectively). Patients with cardiopulmonary concerns, gastrointestinal illness, and neurologic chief complaints had the highest proportion of discharges home with services (42%, 38%, and 36%, respectively). Patients with back pain‐related chief complaints had the highest proportion of discharges to home without services at 27%. Patients with chief complaints categorized as fall and general weakness had the highest proportion of discharge to rehabilitation (35% and 37%, respectively). Case management was consulted most frequently in patients with falls (95%), weakness (94%), and cardiopulmonary (94%) chief complaints. Patients with a fall‐related chief complaint had the highest mean age (79), whereas patients with back pain and musculoskeletal chief complaints had the youngest mean age (70). Patients with neurologic and musculoskeletal chief complaints had the highest number of Emergency Severity Index 1 acuity, constituting 7.0% and 4.4% within each category. Back pain‐related chief complaints had the highest proportion of Emergency Severity Index 4 acuity, at 9.3%. Patients with cardiopulmonary chief complaints were the most likely to be female (72.9%).
TABLE 2.
Descriptive summary of visits with a physical therapy consult placed in the ED, stratified by chief complaint December 1, 2017–November 30, 2018
| Number (%) within each chief complaint | ||||||||
|---|---|---|---|---|---|---|---|---|
| Visit characteristic | Fall (n = 519) | Back pain (n = 151) | Cardiopulmonary (n = 48) | Gastrointestinal (n = 48) | Musculoskeletal (n = 252) | Neurologic (n = 158) | Weakness (n = 51) | Other (n = 69) |
| Emergency Severity Index Level | ||||||||
| 1 | 17 (3.3%) | 0 (0%) | 1 (2.1%) | 0 (0%) | 11 (4.4%) | 11 (7%) | 0 (0%) | 0 (0%) |
| 2 | 208 (40.1%) | 38 (25.2%) | 25 (52.1%) | 10 (20.8%) | 38 (15.1%) | 82 (51.9%) | 17 (33.3%) | 15 (21.7%) |
| 3 | 291 (56.1%) | 99 (65.6%) | 22 (45.8%) | 37 (77.1%) | 190 (75.4%) | 64 (40.5%) | 33 (64.7%) | 49 (71%) |
| 4 | 3 (0.6%) | 14 (9.3%) | 0 (0%) | 1 (2.1%) | 13 (5.2%) | 1 (0.6%) | 1 (2%) | 5 (7.2%) |
| Male sex | 169 (32.6%) | 52 (34.4%) | 13 (27.1%) | 21 (43.8%) | 97 (38.5%) | 60 (38%) | 23 (45.1%) | 29 (42%) |
| Case management consult | 491 (94.6%) | 132 (87.4%) | 45 (93.8%) | 44 (91.7%) | 223 (88.5%) | 144 (91.1%) | 48 (94.1%) | 63 (91.3%) |
| Time spent in ED observation | 440 (84.8%) | 114 (75.5%) | 36 (75%) | 37 (77.1%) | 199 (79%) | 123 (77.8%) | 42 (82.4%) | 59 (85.5%) |
| Disposition | ||||||||
| Admitted | 115 (22%) | 40 (26.5%) | 12 (25%) | 16 (33.3%) | 50 (19.8%) | 41 (25.9%) | 14 (27.5%) | 29 (42%) |
| Home without services | 69 (13.3%) | 41 (27.2%) | 9 (18.8%) | 8 (16.7%) | 58 (23%) | 30 (19%) | 8 (15.7%) | 8 (11.6%) |
| Home with services | 153 (29.5%) | 36 (23.8%) | 20 (41.7%) | 18 (37.5%) | 74 (29.4%) | 57 (36.1%) | 10 (19.6%) | 21 (30.4%) |
| Rehabilitation | 182 (35.1%) | 34 (22.5%) | 7 (14.6%) | 6 (12.5%) | 70 (27.8%) | 30 (19%) | 19 (37.3%) | 11 (15.9%) |
| 72‐h bounce‐back resulting in hospital admission | 19 (8.6%) | 3 (3.9%) | 3 (10.3%) | 3 (11.5%) | 2 (1.5%) | 7 (8.0%) | 4 (22.2%) | 2 (6.9%) |
| Age, mean (SD) | 79 (13) | 70 (17) | 76 (14) | 73 (16) | 70 (16) | 72 (16) | 73 (13) | 73 (13) |
Four patients who were discharged home without additional services re‐presented to the ED within 72 hours and among them, 3 were admitted. Among those discharged home with services, 33 re‐presented and 13 were admitted. Of those discharged to rehabilitation facilities, 6 re‐presented and 1 was admitted (Table 3). In total, 1.3% of patients discharged home without services re‐presented and were admitted, 3.3% of patients discharged home with services re‐presented and were admitted, and 0.3% of patients discharged to rehabilitation re‐presented and were admitted.
TABLE 3.
Descriptive summary of visits in which the patient returned within 72 h
| Original disposition | Number (%) returned within 72 h | Number (%) resulting in admission |
|---|---|---|
| Home without services (n = 231) | 4 (1.7%) | 3 (1.3%) |
| Home with services (n = 389) | 33 (8.5%) | 13 (3.3%) |
| Rehabilitation (n = 359) | 6 (1.7%) | 1 (0.3%) |
Chart review was performed on the 17 patients who re‐presented within 72 hours and were ultimately admitted following discharge home, home with services, or to rehab. Six of the 17 (35%) were recommended for rehabilitation placement on their initial presentation but they refused placement at that time. Chief complaints in this cohort at the time of re‐presentation included fall, chest pain, constipation, and respiratory illness. Seven patients (41%) returned for a seemingly unrelated chief complaint. These included seizures, melena, agitation, depression, change in goals of care, diarrhea, and called back for positive blood cultures. The remaining 4 patients (24%) returned with chief complaints of delirium, fall, dizziness, and syncope. These 4 patients had been discharged home with services and may represent a category where there is room for improvement in their original disposition.
4. LIMITATIONS
There are a number of limitations to this study. The practice patterns in this single center may not be generalizable. Individual charts in their entirety were only reviewed in select cases and it is possible that misclassified data may not have been identified. The ease of access of physical therapist consults in the ED may have resulted in more physical therapist consults than would be obtained if a consult required inpatient admission. Although this study evaluates disposition as is dictated by the physical therapist evaluation, there are a number of instances where an inpatient hospital admission or discharge home are driven by factors external to the physical therapist evaluation which we were unable to account for. Whereas this study was intended to define a clinical pathway to minimize hospital admissions, a significant number of patients were ultimately admitted to the hospital. Further study will be required to ascertain how often this stemmed from physical therapist recommendations, inability to place patients in a timely manner, or as was necessitated by concurrent medical management. This study was performed in a state with comprehensive insurance coverage provided to a significant majority of patients, which may limit generalizability. Last, our follow‐up data that helps demonstrate safety of this pathway is limited to return visits to our institution. It is possible that some patients went to other hospitals following discharge from our ED, but we believe that given the limited adverse outcomes found in the sampling of bounce‐back patients who returned to our hospital, we should expect similar outcome in patients who may have sought subsequent care elsewhere.
5. DISCUSSION
A significant percentage of patients presenting to this ED (2.4%) ultimately received a physical therapist consult in the ED. These were patients deemed medically stable for discharge by an emergency physician but felt to be unsafe for discharge in their current functional state and were thought to require increased services. These patients were predominantly elderly with the most common chief complaints categorized as falls, musculoskeletal, back pain, or neurologic in nature. In total, 748 patients were discharged either to a rehabilitation facility or home with additional services. We identified a total of 979 patients who avoided hospital admission using this clinical pathway. Assuming that the patients included in this study would otherwise be admitted solely for physical therapist and case management evaluation and placement if following traditional protocol, this constitutes a significant proportion of saved inpatient hospital admissions. Moreover, by examining patients re‐presenting to the ED within 72 hours of discharge we found relatively low bounce‐back rates, indicating that these patients are being safely and properly dispositioned from the ED.
Eighty‐one percent of the study population was designated as having spent time in ED observation status. Observation units are a burgeoning setting for high‐quality and cost‐effective care. They are less expensive compared to inpatient hospitalization in treatment of specific conditions. 5 , 6 Observation units are increasingly used, with over one‐third of U.S. EDs housing an observation unit and ∼2% of hospital visits involving admission to an observation unit. 7 , 8 Although few studies reference the provision of physical therapist services in an observation unit setting, the use of physical therapist in an observation unit as a means of rapidly and safely dispositioning patients who require rehabilitation services is not well described in the literature. 9 , 10 The specific intervention of physical therapist evaluation and rehabilitation placement is one that is wellsuited to an observation unit setting: it can be accomplished in a time‐sensitive fashion and uses the framework of case management and physical therapist services that often already exist in or are accessible by the ED.
The benefits of a rapid disposition and avoidance of the harms of prolonged hospital stays are both self‐evident and well‐described with prior studies demonstrating that prolonged wait times to transfer to rehabilitation facilities can result in prolonged rehabilitation stays, increased odds of in‐hospital complications such as development of urinary tract infections, pneumonia, or delirium. 11 , 12 , 13 , 14
A significant proportion of our study population involved older adults who have fallen. Falls are the leading cause of fatal and nonfatal injuries among adults aged ≥65 years. 15 Thirty‐five percent of community‐dwelling individuals over age 65 will fall every year and up to 10% of falls in community‐dwelling older persons result in significant injury. 16 Recurrent falls are associated with increased mortality. 16 Physical therapist evaluation and intervention has been shown to decrease the number of falls and fall‐related ED visits. 16 , 17
Physical therapist evaluation in the ED has been previously described in a variety of contexts. 9 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 physical therapists are often able to provide more specific diagnoses to patients, spend more time on patient education, streamline outpatient follow‐up by performing an initial evaluation, and provide patients with expected symptom trajectory, instructions on activity modification and home exercise techniques. 19 , 22 In particular, ED‐based physical therapists can aid in safety evaluation and disposition or discharge planning. 18 , 19 , 23 , 24 In some instances, evaluation in the ED by physical therapists has been associated with decreased wait times and decreased lengths of stay. 19 , 21 , 22 The addition of physical therapists to the ED has been associated with increased patient satisfaction. 18 , 19 , 22 , 27 physical therapist inclusion in the ED is also associated with high levels of satisfaction among emergency physicians and staff. 19 , 21 , 25 To our knowledge, this study is the first of its kind to describe a robust clinical pathway where physical therapist evaluation in an observation unit can be used to expedite rehabilitation placement and avoid hospital admissions.
6. CONCLUSIONS
Given that the standard of care in many institutions would be an admission to the hospital for all patients requiring physical therapist and case management consultation, we believe that an ED‐based physical therapy and case management system serves as a viable method to substantially decrease hospital admissions and potentially reduce cost both to patients and the health care system.
AUTHOR CONTRIBUTIONS
KLG and MSB wrote the first draft. All authors reviewed and edited multiple revisions. KLG and MSB take responsibility for the paper as a whole.
Supporting information
Supporting Information
Biographies
Kiersten L. Gurley, MD, is the Assistant QI Director of the Department of Emergency Medicine at Beth Israel Deaconess Medical Center and a clinical instructor at Harvard Medical School.

Maxwell Blodgett is an emergency medicine resident at the Harvard Affiliated Emergency Medicine Residency at Beth Israel Deaconess medical center.

Gurley KL, Blodgett MS, Burke R, Shapiro NI, Edlow JA, Grossman SA. The utility of emergency department physical therapy and case management consultation in reducing hospital admissions. JACEP Open. 2020;1:880–886. 10.1002/emp2.12075
Funding and support: By JACEP Open policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist.
MSB is co‐first author having contributed equally with KLG as first author.
Supervising Editor: Catherine A. Marco, MD.
REFERENCES
- 1. Sheehy A, Caponi B, Gangireddy S, et al. Observation and inpatient status: clinical impact of the 2‐midnight rule. J Hosp Med. 2014;0(4):203‐209. [DOI] [PubMed] [Google Scholar]
- 2. Capp R, Sun B, Boatright D, Gross C. The impact of emergency department observation units on United States emergency department admission rates. J Hosp Med. 2015;10(11): 738‐742. [DOI] [PubMed] [Google Scholar]
- 3. Cheng AHY, Barclay NG, Abu‐Laban RB. Effect of a multi‐diagnosis observation unit on emergency department length of stay and inpatient admission rate at two Canadian hospitals. J Emerg Med. 2016;1(6):739‐747. [DOI] [PubMed] [Google Scholar]
- 4. Brillman J, Mathers‐Dunbar L, Graff L, et al. Management of observation units. Ann Emerg Med. 1995;25(6):823‐830. [DOI] [PubMed] [Google Scholar]
- 5. Roberts RR, Zalenski RJ, Mensah EK, et al. Costs of an emergency department‐based accelerated diagnostic protocol vs. hospitalization in patients with chest pain: a randomized controlled trial. JAMA. 1997;278(20):1670‐1676. [PubMed] [Google Scholar]
- 6. Gomez MA, Anderson JL, Karagounis LA, Muhlestein JB, Mooders FB, Group RS. An emergency department‐based protocol for rapidly ruling out myocardial ischemia reduces hospital time and expense: results of a randomized study (ROMIO). J Am Coll Cardiol. 1991;28(1):25‐33. [DOI] [PubMed] [Google Scholar]
- 7. Wiler JL, Ross MA, Ginde AA. National study of emergency department observation services. Acad Emerg Med. 2011;18(9):959‐965. [DOI] [PubMed] [Google Scholar]
- 8. Venkatesh AK, Geisler BP, Chambers JJ, Baugh CW, Bohan J, Schuur JD. Use of observation care in US emergency departments, 2001 to 2008. PLoS One. 2011;6(9):e24326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Plummer L, Sridhar S, Beninato M, Parlman K. Physical therapist practice in the emergency department observation unit: descriptive study. Phys Ther. 2015;95:249‐256. [DOI] [PubMed] [Google Scholar]
- 10. Southerland LT, Vargas AJ, Nagaraj L, Gure TR, Caterino JM. An emergency department observation unit is a feasible setting for multidisciplinary geriatric assessments in compliance with the geriatric emergency department guidelines. Acad Emerg Med. 2018;25:76‐82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sirois MJ, Lavoie A, Dionne CE. Impact of transfer delays to rehabilitation in patients with severe trauma. Arch Phys Med Rehabil. 2004;85(2):184‐191. [DOI] [PubMed] [Google Scholar]
- 12. Mathew P, Jehan F, Kulvatunyou N, et al. The burden of excess length of stay in trauma patients. Am J Surg. 2018;216(5):881‐885. [DOI] [PubMed] [Google Scholar]
- 13. Rosman M, Rachminov O, Segal O, Segal G. Prolonged patients’ in‐hospital waiting period after discharge eligibility is associated with increased risk of infection, morbidity and mortality: a retrospective cohort analysis. BMC Health Serv Res. 2015;15(1):246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Rojas‐García A. Impact and experiences of delayed discharge: a mixed‐studies systematic review. Health Expect. 2018;21(1):41‐56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Bergen G, Stevens MR, Burns ER. Falls and fall injuries among adults aged 65 years—United States, 2014. Morbid Mortal Wkly Rep. 2016;65(37):993‐998. [DOI] [PubMed] [Google Scholar]
- 16. Davidson J, Bond J, Dawson P, Steen NI, Kenny RA. Patients with recurrent falls attending accident & emergency benefit from multifactorial intervention—a randomised controlled trial. Age Ageing. 2005;34(2):162‐168. [DOI] [PubMed] [Google Scholar]
- 17. Lesser A, Israni J, Kent T, Ko KJ. Association between physical therapy in the emergency department and emergency department revisits for older adult fallers: a nationally representative analysis. J Am Geriatr Soc. 2018;66:2205‐2212. [DOI] [PubMed] [Google Scholar]
- 18. Anaf S, Sheppard LA. Physiotherapy as a clinical service in emergency departments: a narrative review. Physiotherapy. 2007;93:243‐252. [Google Scholar]
- 19. Kim HS, Strickland KJ, Mullen KA, Lebec MT. Physical therapy in the emergency department: a new opportunity for collaborative care. Am J Emerg Med. 2018;36(8):1492‐1496. [DOI] [PubMed] [Google Scholar]
- 20. Lefmann SA, Crane JL. Establishing the diverse value of the emergency department physiotherapist. J Physiother. 2016;62(1):1‐3. [DOI] [PubMed] [Google Scholar]
- 21. Morris C, Hawes S. The value of accident and emergency based physiotherapy services. J Accid Emerg Med. 1996;13(2):111‐113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. McClellan C, Greenwood R, Benger J. Effect of an extended scope physiotherapy service on patient satisfaction and the outcome of soft tissue injuries in an adult emergency department. Emerg Med J. 2006;23:384‐387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Taylor DM, Bennett DM, Cameron PA. a paradigm shift in the nature of care provision in emergency departments. Emerg Med J. 2004; 21(21): 681‐684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kesteloot L, Lebec MT. Physical therapist consultation in the emergency department: a multiple case report describing three Arizona programs. J Acute Care Physical Therapy. 2012;3:224‐231. [Google Scholar]
- 25. Lebec MT, Cernohous S, Tenbarge L, Gest C, Severson K, Howard S. Emergency department physical therapist service: a pilot study examining physician perceptions. Internet J Allied Health Sci Pract. 2010;8: ‐12. [Google Scholar]
- 26. Fleming‐McDonnell D, Czuppon S, Deusinger SS, Deusinger RJ. Physical therapy in the emergency department: development of a novel practice venue. Phys Ther. 2010; 90: 420‐426. [DOI] [PubMed] [Google Scholar]
- 27. Lebec MT, Jogodka CE. The physical therapist as a musculoskeletal specialist in the emergency department. J Orthop Sports Phys Ther. 2009; 39(3):221‐229. [DOI] [PubMed] [Google Scholar]
- 28. Thomas SN. The financial impact of delayed discharge at a level I trauma center. J Trauma Acute Care Surg. 2005;58(1):121‐125. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information


