Abstract
Objectives
Little academic investigation has been done to describe emergency department (ED) practice structure and quality improvement activities. Our objective was to describe staffing, payment mechanisms, and quality improvement activities among EDs in a nationwide quality improvement network and also stratify results to descriptively compare (1) single‐ versus multi‐site EDs and (2) small‐group versus large‐group EDs.
Methods
Observational study examining EDs that completed activities for the 2018 wave of the Emergency Quality Network (E‐QUAL), a voluntary network of EDs nationwide that self‐report quality improvement activities. EDs were defined as single‐site or multi‐site based on self‐reported billing practices; additionally, EDs were defined as large‐group if they and a majority of other sites with the same group name also identified as multi‐site. All other sites were deemed small‐group.
Results
Data from 377 EDs were included. For staffing, the median number of clinicians was 17 overall (16 single‐site; 19 multi‐site). For payment, 376 of 377 EDs (99.7%) participated in the Merit‐Based Incentive Payment System. Thirty‐five EDs (9.2%) participated in a federal alternative payment model, and 19 (5.0%) participated in a commercial alternative payment model. For quality improvement, single‐ and multi‐site EDs reported similar progress on quality improvement strategies; however, small‐group EDs reported more advanced quality improvement strategies compared to large‐group EDs for 8/10 quality improvement strategies included in a survey (eg, “achieved a formal plan to eliminate waste”).
Conclusion
Among EDs in E‐QUAL, staffing, payment, and quality improvement activities are similar between single‐ and multi‐site EDs. Group‐level analysis suggests that practice structure may influence adoption of quality improvement strategies. Future work is needed to further evaluate practice structure and its influence on quality improvement activities and quality.
Keywords: emergency medicine practice, health policy, health services research, quality improvement, rural, value‐based care
1. INTRODUCTION
1.1. Background
Over the last few decades, healthcare organizations including emergency medicine practices have experienced consolidation. 1 , 2 Administrators may favor consolidation for multiple reasons. First, it may enable quality improvement by increasing operational efficiency. 3 Second, it may reduce clinician‐level burdens of reporting to complex programs such as Medicare's Quality Payment Program. 4 , 5 However, little is known about how structural differences in emergency medicine practices influence quality improvement.
1.2. Importance
Better understanding how practice structure influences quality improvement activities among a nationwide sample of EDs could empower stakeholders to encourage structural designs that favor high‐quality healthcare. However, investigations in this area have been limited for multiple reasons. First, there are no standard measures of emergency department practice structure. Second, the mechanisms by which practice structure might affect the quality of emergency care have not been elucidated. Third, and perhaps most importantly, data sources describing practice structure and quality improvement have not been available on the national level, particularly with respect to rural and community‐based EDs.
1.3. Goals of this investigation
In 2016, as part of Medicare's Transforming Clinical Practice Initiative, the American College of Emergency Physicians (ACEP) launched the Emergency Quality Network (E‐QUAL), which has enabled a unique opportunity to examine emergency medicine practice structure and quality improvement activities among a sample of highly motivated EDs. Moreover, E‐QUAL includes many rural and community‐based EDs, thus enabling an assessment of emergency medicine practices not available in prior data sets. In this study, our objective was to describe staffing, payment, and quality improvement activities among EDs in E‐QUAL and also stratify results to descriptively compare EDs using 2 categories of practice structure: (1) single‐ versus multi‐site EDs and (2) small‐group versus large‐group EDs.
2. METHODS
2.1. Study design and setting
This study is reported in accordance with the STROBE (Strengthening the Reporting of Observational studies in Epidemiology) statement. 6 We conducted an observational study examining ED characteristics and baseline quality improvement data from US hospital‐based EDs participating in the E‐QUAL avoidable imaging or sepsis initiatives in 2018. E‐QUAL is a volunteer learning collaborative in which EDs collect and submit data on quality improvement for benchmarking purposes. 7 Participation in E‐QUAL is self‐selected and likely motivated by a desire to improve quality and also perform well under the Quality Payment Program.
2.2. Selection of participants
EDs were included in the sample if they completed all E‐QUAL activities related to the avoidable imaging or sepsis initiative in 2018. EDs were excluded if they did not report on taxpayer identification number billing practices. See Supporting Information Figure S1 for a flowchart depicting how inclusion and exclusion criteria affected selection of participating sites.
2.3. Data collection
Data were collected locally by individual ED sites and submitted to E‐QUAL by a designated ED administrator who completed a survey on a standardized web‐based submission portal. The data included in this study was collected in January through and March of 2018 as part of a pre‐initiative assessment of quality improvement practices.
2.4. Measurements
Practice structure and consolidation have previously been measured by health services researchers and federal policymakers by using taxpayer identification number billing practices, but to our knowledge, these definitions have not been adapted for use in emergency medicine. Thus, for this study, we created new definitions of practice structure based on taxpayer identification number billing practices at 2 different levels: first, EDs were defined as single‐site if all clinicians at 1 and only 1 site billed under a single taxpayer identification number or multi‐site if clinicians at multiple sites billed under the same taxpayer identification number. Sites were excluded if they reported that physicians billed under individual taxpayer identification numbers (11 sites) or if they billed as part of a multi‐specialty group (6 sites). Second, we defined sites as large‐group if (1) the site reported billing as multi‐site and (2) the majority of sites with the same group name also reported billing under a multi‐site taxpayer identification number. All other sites were defined as being small‐group. Note that single‐site EDs are counted as small‐group sites. See Supporting Information Figure S2 for a figure further elucidating these definitions with examples.
Participating EDs submitted data describing annual ED volume, number of clinicians, number of beds, and ZIP code. Each ED was classified as rural or urban based on the Rural‐Urban Commuting Area Code for the practice location's ZIP code. Each ED was also asked whether they were participating in Medicare's Quality Payment Program and whether it was via the Merit‐Based Incentive Payment Program or an advanced alternative payment model. Each site was also asked about participation in alternative payment models through commercial insurance carriers. Finally, EDs were asked to provide information about specific current and future quality improvement practices as part of the E‐QUAL Quality Readiness Assessment. This assessment was a non‐validated adaptation of the CMS Practice Assessment Tool (PAT) specified for use with emergency clinicians. 8 The assessment included 3 domains: readiness assessment (including staffing and payment mechanisms), practice transformation (readiness for new quality improvement initiatives), and quality improvement (progress on specific improvement practices related to sepsis and avoidable imaging). See the Supporting Information material for samples of questionnaires.
The Bottom Line
The impact of emergency department practice structure on quality improvement activities has rarely been studied. In this investigation of existing data from the emergency quality network (E‐QUAL), small group EDs reported more advanced quality improvement activities than large group EDs.
2.5. Analysis
We report descriptive statistics overall at the ED site level. We also report results by measures of practice structure, including for single‐ versus multi‐site EDs and for small‐group versus large‐group EDs. Analysis was performed with R version 3.6.0 (The R Foundation for Statistical Computing, Vienna, Austria).
The data submitted by ED administrators of these hospitals did not include patient‐identifiable information and was deemed not human subjects research.
3. RESULTS
3.1. Characteristics of the study sample
A total of 377 sites participated in E‐QUAL and submitted data related to their taxpayer identification number status necessary for inclusion in the study sample. Ninety‐two EDs (24%) were located in rural areas. See Figure 1 for a map displaying the locations of all EDs in the sample. A total of 348 sites participated in the E‐QUAL Sepsis Initiative, 295 sites participated in the E‐QUAL Avoidable Imaging Initiative, and 266 sites participated in both.
FIGURE 1.
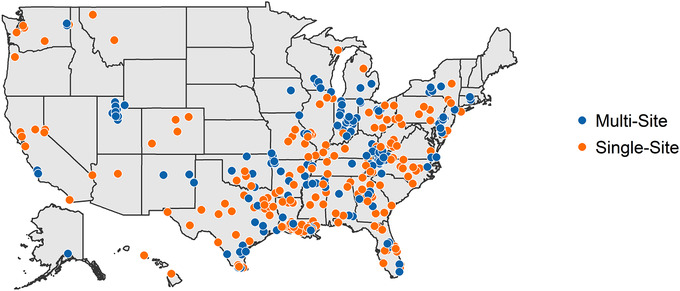
Map demonstrating the location of emergency departments in the sample by single‐ and multi‐site designation
3.2. Main results
The median number of clinicians in single‐site versus multi‐site EDs was 16 and 19, respectively. The median annual site visit volume was 23,432 for single‐site versus 21,533 for multi‐site EDs, and the number of treatment spaces was 22.5 and 22, respectively. See Table 1 for more descriptive statistics characterizing the sites in the sample and their staffing.
TABLE 1.
Descriptive characteristics of emergency departments in the sample overall and by single‐ and multi‐site designation
| Characteristic | Overall, n = 377 median (IQR) | Single‐site, n = 190 median (IQR) | Multi‐site, n = 187 median (IQR) |
|---|---|---|---|
| Annual ED volume | 22,967 (13,285, 35,854) | 23,432 (13,079, 38,843) | 21,533 (13,693, 33,133) |
| Pediatric ED volume | 3,606 (1,942, 5,609) | 4,010 (2,332, 5,959) | 3,325 (1,748, 5,126) |
| No. of ED beds | 16 (10, 26) | 15.5 (10, 26) | 16 (10, 26) |
| No. of ED spaces | 22 (14, 37) | 22.5 (14, 39) | 22 (14, 34) |
| No. of physicians | 10 (8, 17) | 10 (7, 16) | 12 (8, 20) |
| No. of nurse practitioners and/or physician assistants | 7 (4, 11) | 6 (4, 10) | 7 (4, 14) |
| Inpatient admission rate | 12.5% (8.8%, 19.2%) | 12.5% (9.0%, 19.0%) | 12.62% (8.5%, 19.2%) |
| Rural location no. of sites (%) | 92 (24.4%) | 55 (28.9%) | 37 (19.8%) |
Abbreviations: IQR, interquartile range
In terms of payment, a total of 376 EDs reported participation in the Merit‐Based Incentive Payment System (MIPS) in 2018, and 1 reported participation in an advanced alternative payment model. For MIPS participants, the most common quality reporting mechanism was to use a non‐ACEP third‐party vendor (79.5% of single‐site and 61.5% of multi‐site EDs). The second most popular reporting mechanism was ACEP's Clinical Emergency Data Registry (6.3% of single‐site and 4.3% of multi‐site EDs), followed by direct reporting (3.7% of single‐site and 0.5% of multi‐site EDs) and web interface (1 single‐site ED). Thirty‐five EDs (9.2%) reported participation in any federal alternative payment model and 19 (5.0%) reported participation in a commercial alternative payment model.
In terms of quality improvement, all sites in the sample reported collecting data for quality reporting to the federal government. For sites in the sepsis collaborative, 100% of single‐site and 98.3% of multi‐site EDs had initiated pop‐up alerts in the electronic health record to warn clinicians about possible cases. For sites in the avoidable imaging collaborative, 86.4% of single‐site and 76.9% of multi‐site EDs delivered clinician‐specific feedback reports on at least 1 imaging test. Overall, single‐ and multi‐site EDs reported similar rates of having “achieved” various quality improvement strategies (Figures 2A and 2B). We also compared quality improvement practices between small‐group and large‐group EDs, and the results suggest a trend toward more advanced quality improvement practices for small‐group EDs: as displayed in Figures 2C and 2D, small‐group EDs, when compared to large‐group EDs, more commonly reported having “achieved” quality improvement strategies for 8 of 10 survey questions. However, large‐group EDs more commonly reported achieving goals related to eliminating waste and reducing unnecessary testing.
FIGURE 2.
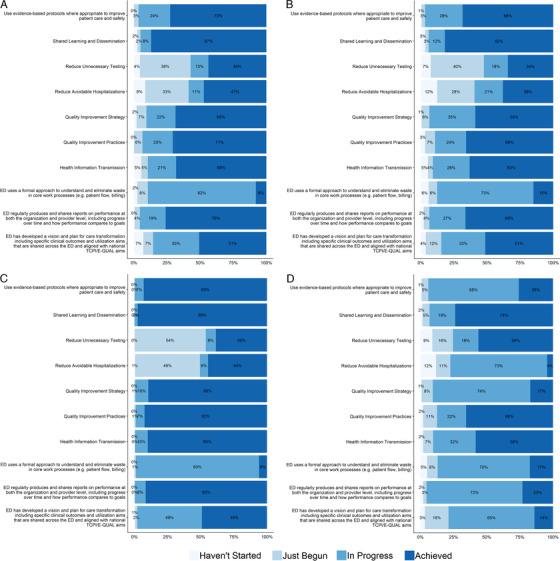
(A and B) Self‐reported degree to which participating E‐QUAL sites had implemented specific quality improvement strategies, stratified by single‐ and multi‐site emergency departments in the sample. (C and D) Self‐reported degree to which participating E‐QUAL sites had implemented specific quality improvement strategies, stratified by small‐ and large‐group emergency departments in the sample
3.3. Limitations
Our study does have several limitations. First, our sample is self‐selected and highly motivated to improve quality, therefore our results may overestimate quality improvement readiness; however, policy incentives such as MIPS have created an incentive for all types of EDs to join E‐QUAL, and other studies using data from E‐QUAL have demonstrated substantial variation in performance on quality measures among participating EDs. 7 , 9 Second, we obtained data by self‐report of ED administrators, and it is possible that the mode of data collection and resulting social desirability bias have affected our results. Third, we were unable to examine the effects of other business factors that may drive consolidation, such as the presence of ED practice management groups or for‐profit status of groups, on our results. Finally, our definitions of single‐site, multi‐site, small‐group, and large‐group may not be ideal for examining quality improvement practices because payment and practice improvement may not occur at the same levels, and because our definitions are novel and have not been validated.
4. DISCUSSION
In this sample of EDs motivated by payment incentives to participate in a national quality improvement network, we did not observe important differences between single‐ and multi‐site EDs in staffing, payment, or quality improvement strategies. Most participating sites reported having achieved numerous nationally recognized practice improvement milestones. In a hypothesis‐generating sub‐analysis comparing small‐group versus large‐group quality improvement practices, we found that small‐group EDs were more likely than large‐group EDs to report implementation of advanced quality improvement strategies.
It is reasonable to believe that E‐QUAL's single‐site and multi‐site EDs have similar site‐level characteristics. Similarly, it is reasonable to believe that quality improvement strategies could be managed well at a single‐site or multi‐site ED either locally or through more aggregated business processes with a similar degree of success. In fact, our site‐level results are reminiscent of a study of 30 EDs in 1985 that found no differences in performance on quality measures for EDs based on staffing patterns (hospital‐based group on contract, nonhospital‐based group on contract, rotating staff, and all other patterns). 10
Our finding that small‐group ED quality improvement practices may be more advanced than those of large‐group EDs is interesting. On one hand, it is possible that EDs with less advanced quality improvement capabilities preferentially join large groups to obtain resources to help them advance. On the other hand, it is also possible that a top‐down approach of promulgating quality improvement strategies reaches EDs more slowly in large groups compared to smaller, less bureaucratic groups. Nevertheless, the presence of these differences, their etiology, and their relationship to outcomes should be validated in future studies before driving any policy changes.
From our assessment of published literature, the most recent comprehensive review of the relationship between practice structure and quality of care found that consolidation within a market reduces independent market participants and does not lead to improved quality of care. 1 While our study is small and limited by its use of cross‐sectional survey data, it reveals that quality improvement activities are progressing well in a highly motivated sample of EDs across the nation. While we feel optimistic that quality improvement capacity is improving in EDs of all types, we recommend further investigation be undertaken to better elucidate how organizations manage ED quality improvement activities and what the impact is on patient health outcomes.
In summary, ED engagement in quality improvement is occurring across the nation, and many commonly referenced improvement strategies have been implemented among a large sample of EDs that includes significant participation in rural areas. At the ED site level, the composition of staffing, payment, and quality improvement strategies are similar overall. Future work should explore multiple definitions of ED group structure and consolidation, and it should also examine the association between practice structure, quality improvement strategies, and more patient‐centric measures such as health outcomes for patients.
AUTHOR CONTRIBUTIONS
AKV and CTB conceived the study. DS, NT, and PG supervised data collection and quality control. CR and DS facilitated the analysis. CTB, AKV, and KS drafted the manuscript. All authors contributed substantially to its revision. CTB takes final responsibility for the paper as a whole.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
Supporting information
FIGURE S1 Flowchart describing how inclusion and exclusion criteria affected the selection of participating EDs
FIGURE S2 Examples of how EDs with varying self‐reported payment arrangements were categorized in site‐level and group‐level analyses
Biography
Carl T. Berdahl, MD, MS, is an affiliated adjunct policy researcher at the RAND Corporation and an emergency physician and health services researcher at Cedars‐Sinai Medical Center, Los Angeles, CA.
Berdahl CT, Schuur JD, Rothenberg C, et al. Practice structure and quality improvement activities among emergency departments in the Emergency Quality (E‐QUAL) Network. JACEP Open. 2020;1:839–844. 10.1002/emp2.12078
Supervising Editor: John J. Rogers, MD.
Funding and support: The project described was supported by the US Department of Health and Human Services, Centers for Medicare and Medicaid Services (CMS‐1L1CMS331479‐02). The contents provided are solely the responsibility of the authors and do not necessarily represent the official views of US Department of Health and Human Services or any of its agencies. This award supports the American College of Emergency Physicians Support and Alignment Network (SAN) of the CMS Transforming Clinical Practice Initiative (TCPi). AKV reports career development support (KL2TR001862) from the National Center for Advancing Translational Science and Yale Center for Clinical Investigation; support from the Centers for Medicare & Medicaid Services for the development of hospital outcome and efficiency quality measures. AKV and JDS obtained research funding.
REFERENCES
- 1. Gaynor M, Town R. The Impact of Hospital Consolidation. Princeton, NJ: Robert Wood Johnson Foundation; 2012. [Google Scholar]
- 2. Dresnick SJ. The future of the private practice of emergency medicine. Ann Emerg Med. 1997;30(6):754‐756. [DOI] [PubMed] [Google Scholar]
- 3. Tsai TC, Jha AK. Hospital consolidation, competition, and quality: is bigger necessarily better? JAMA. 2014;312(1):29‐30. [DOI] [PubMed] [Google Scholar]
- 4. Fulton BD. Health care market concentration trends in the United States: evidence and policy responses. Health Aff (Millwood). 2017;36(9):1530‐1538. [DOI] [PubMed] [Google Scholar]
- 5. Neprash HT, Chernew ME, McWilliams JM. Little evidence exists to support the expectation that providers would consolidate to enter new payment models. Health Aff (Millwood). 2017;36(2):346‐354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Freytag J, Stroben F, Hautz WE, Schauber SK, Kaemmer JE. Rating the quality of teamwork a comparison of novice and expert ratings using the Team Emergency Assessment Measure (TEAM) in simulated emergencies. Scand J Trauma Resusc Emerg Med. 2019;27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Greenwood‐Ericksen MB, Rothenberg C, Mohr N, et al. Urban and rural emergency department performance on National Quality Metrics for Sepsis Care in the United States. J Rural Health. 2019;35(4):490‐497. [DOI] [PubMed] [Google Scholar]
- 8. TCPI Practice Assessment Tool 2.0 & Practice Assessment Report Template 2.0 (PART): Reporting and Submission User Guide. Centers for Medicare & Medicaid Services. Transforming Clinical Practices Initiative: Data Support and Feedback Reporting Web site. https://innovation.cms.gov/Files/x/tcpi-pat.pdf. Updated 19 Apr 2016 (Version 1). Accessed 13 Jan 2020.
- 9. Venkatesh AK, Slesinger T, Whittle J, et al. Preliminary performance on the new CMS sepsis‐1 national quality measure: early insights from the Emergency Quality Network (E‐QUAL). Ann Emerg Med. 2018;71(1):10‐15.e11. [DOI] [PubMed] [Google Scholar]
- 10. Georgopoulos BS. Organization structure and the performance of hospital emergency services. Ann Emerg Med. 1985;14(7):677‐684. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
FIGURE S1 Flowchart describing how inclusion and exclusion criteria affected the selection of participating EDs
FIGURE S2 Examples of how EDs with varying self‐reported payment arrangements were categorized in site‐level and group‐level analyses


