Abstract
Background
The homeless patient population is known to have a high occurrence of inappropriate emergency department (ED) utilization. The study hospital initiated a dedicated homeless clinic targeting patients experiencing homelessness with a combination of special features. We aim to determine whether this mode of care can reduce inappropriate ED utilization among homeless patients.
Methods
We conducted a retrospective observational study from July 1, 2017 to Dec 31, 2017. The study enrolled all homeless patients who visited any hospital regular clinic, dedicated homeless clinic, and ED at least once during the study period. ED homeless patients were divided into four groups (A: no clinic visits; B: those who only visited hospital regular clinic; C: those who only visited dedicated homeless clinic; and D: those who visited both hospital regular clinic and dedicated homeless clinic). The New York University algorithm was used to determine appropriate ED utilization. We compared inappropriate ED utilization among patients from these groups. Multivariate logistic regression was used to determine the risks of different clinical visits in association with inappropriate ED utilization.
Results
A total of 16,323 clinic and 8511 ED visits occurred among 5022 unique homeless patients, in which 2450 unique patients were seen in hospital regular clinic, 784 patients in dedicated homeless clinic, 688 patients in both hospital regular clinic and dedicated homeless clinic, and 1110 patients with no clinic visits. Twenty‐nine percent (230/784) of patients from dedicated homeless clinic utilized the ED, among which 21% (175/844) of their ED visits were considered inappropriate. In contrast, 40% of patients from hospital regular clinic utilized the ED, among which 29% were inappropriate (P < 0.001). The adjusted odds ratio (OR) was 0.61 (95% confidence interval [CI] = 0.50–0.74, P < 0.001) on dedicated homeless clinic predicting inappropriate ED visits in multivariate logistic regression.
Conclusion
Implementing a dedicated homeless clinic with these features can reduce ED inappropriate utilization among patients experiencing homelessness.
Keywords: clinics, emergency department, homeless, inappropriate utilization
1. INTRODUCTION
1.1. Background
Homeless patients are considered a unique patient population with a high risk for hospital emergency department utilization, ED returns, hospital admissions, and all‐cause mortalities. 1 , 2 , 3 , 4 , 5 Previous studies have investigated different interventions to improve healthcare quality and decrease inappropriate ED utilization including accommodation, healthcare, and finance supports. 6 , 7 , 8 The most common interventions noted in the literature include providing food and temporary housing, arranging primary care physician (PCP) follow‐up, and providing charity insurance coverage. 2 , 4 , 7 However, the outcomes of these interventions had high degrees of variation.
Some studies reported decreased ED visits, decreased hospital admissions, increased primary clinic follow‐up, and increased adherence to medical treatment plans. 6 , 9 Others questioned the efficacy of these interventions given the fact that healthcare outcomes are multi‐factorial. Studies that reported providing charity insurance coverage to homeless patients did not seem to reduce inappropriate ED utilization, reporting a rate similar to patients covered by Medicaid. 2 , 10 , 11 Hategan et al demonstrated gender differences in which homeless women were more likely to return to the ED even when provided with access to a primary care provider. 12 Rosenheck et al studied the promotion of healthcare integration using outreach ACCESS program (Access to Community Care and Effective Services and Support) among homeless patients and failed to show better clinical outcomes. 13 A study to assist homeless veterans with increasing engagement in their care showed no improvement in the rates of alcohol use, drug use, or hospitalization between patients receiving high and low intensity outreach programs. 14 Overall, these diverse outcomes make any generalization difficult.
Providing clinics dedicated to homeless populations is another common intervention used to reduce unnecessary ED utilization. 15 , 16 , 17 Some clinics dedicated to people experiencing homelessness utilize volunteer medical professionals, have varying types of patient access schedules, and provide free care. 18 , 19 , 20 Others use mobile medical units, located close to homeless shelters, as an alternative to clinic‐based care. 21 , 22 , 23 Studies on such clinics showed better medical compliance, clinical outcomes, and patient satisfaction. 23 , 24 , 25 Better outcomes including decreased ED visits and hospitalizations were also reported among homeless clinic sites with better staffing and fully dedicated physicians. 26 However, some dedicated homeless clinics are staffed with fewer healthcare workers due to limited funding, with an uncertain schedule based on the time availability of the providers; or with healthcare providers of limited experience (eg, medical student, nurse‐run clinics). 27 , 28 , 29
1.2. Importance
Our study healthcare system implemented a program using a bricks‐and‐mortar dedicated homeless clinic, administrated by hospital clinical systems, staffed with family medicine physicians, located close to homeless shelters and camps at Fort Worth, TX, and functions as a medical clinic for this unique population. The dedicated homeless clinic operates in accordance with the hospital regular clinic principles, is provided similar administrative support from the study hospital, and has a stable staff consisting of attending physicians with experience and interest in care of homeless population. The dedicated homeless clinic uses the same electronic health record system. Moreover, the dedicated homeless clinic has a mobile street medicine team that can access the electronic health record system “in the field” while visiting the camps and the shelters, allowing on‐site registration as well as real‐time documentation of patient visits. The dedicated homeless clinic and the street medicine team also use community health workers to coordinate patient care and improve access to the hospital system as well as various safety net programs, and housing agencies in the community. The combinations of these special features separate our dedicated homeless clinic from other clinics reported in the literature.
1.3. Goals of this study
We aimed to determine whether dedicated homeless clinic reduces total and inappropriate ED visits. We also aimed to identify potential differences in homeless patient ED utilization between dedicated homeless clinic and hospital regular clinic.
2. METHODS
2.1. Study design and setting
This is a single‐center retrospective observational study using collected data from the electronic health record system. We reviewed all hospital clinics and ED data from January 1, 2017 to December 31, 2017. The study hospital is a publicly funded urban academic tertiary referral center. The hospital ED sponsors an ACGME accredited emergency medicine residency program and is a local Level 1 trauma center, a chest pain center, and a comprehensive stroke center. The JPS Health network includes over 50 primary care and subspecialty clinics within Tarrant county and one dedicated homeless clinic in Fort Worth, Texas. The system covers an area with an estimated population of 2 million. The JPS Health Network Institutional Review Board approved this study.
Hospital clinics are regular primary care physician clinics staffed by either physicians (including attending, residents, and fellows) or advanced practice providers. The dedicated homeless clinic is staffed by family medicine physicians, advanced practice providers, family medicine fellows, and residents. The dedicated homeless clinic staff is trained in primary care and has special interest in the care of the homeless population. Special features differentiating the dedicated homeless clinic and hospital regular clinics are listed in Table 1. Briefly, the dedicated homeless clinic is close to the shelters for the homeless and has both routine appointments and walk‐in visits. The dedicated homeless clinic has a mobile component with personnel (street medicine team) who visit homeless camps. Mobile visits are registered and documented within the same single hospital electronic health record system. The hospital ED has an annual patient volume of >120,000.
2.2. Selection of subjects
We included all homeless patients presenting to the study hospital clinics and ED during the study period. Homeless patients were defined as those who met the US Department of Housing and Urban Development (HUD) definition of homelessness at the time of entry into our electronic health record system. Patient homeless condition was updated every 6 months or on patients visiting ED or clinics, whichever appeared first. We also excluded homeless patients who became non‐homeless during the study period. Patients were initially identified via our electronic health record system and then further cross‐referenced with the Tarrant County Homeless Management Information System (HMIS) database archived in Fort Worth, TX. A third identification method was through the hospital's “Care Connections Outreach Team.” This group is composed of an advanced practice provider, a social worker, a registered nurse, and community health workers. They round in the hospital to help direct patients to the clinic (dedicated homeless clinic) and are present and meet with the patients in the dedicated homeless clinic. For situations where data did not match between information systems, but in which homelessness status could be verified by the Care Connections Outreach Team, patients were entered into the electronic health record system manually.
The Bottom Line
Patients experiencing homelessness are known to have higher emergency department utilization. This observational study found using a dedicated homeless clinic with multidisciplinary approaches might reduce emergency department inappropriate utilization among homeless patients.
2.3. Measurements
General patient characteristics including age, sex, race/ethnicity, mode of arrival, and insurance type were collected. Mode of arrival was further divided into 5 categories: (1) private transportation (private car or taxi); (2) healthcare‐assisted transportation (emergency ground or air transport, and hospital‐assisted transportation); (3) public transportation (by bus, or other public transportation); (4) ambulatory; and (5) others (police, wheelchair, or unknown). Insurance type was divided into 5 categories: (1) hospital charity insurance (an insurance issued by study hospital to homeless patients to cover patient healthcare costs), such insurance covers the majority of hospital clinical visits, ED visits, procedures, and pharmacy costs; (2) Medicaid; (3) Medicare; (4) others (such as: commercial, work‐compensated insurance, or military insurance); and (5) no insurance.
The New York University ED Algorithm (NYUA) was used to determine inappropriate ED utilization. 30 , 31 NYUA categorized ED patient visits into 4 different conditions: (1) emergent not avoidable, considered as ED appropriate visits; (2) primary care treatable, defined as care that can be safely provided in a primary care setting without the need for emergent treatment; (3) emergent care needed but preventable/avoidable, defined as patients whose disease conditions can be prevented/avoided if preventive care is received in a timely fashion; and (4) non‐emergent. Inappropriate ED utilization was determined if patients were classified as non‐emergent.
2.4. Outcomes
The primary outcome in this study was inappropriate ED utilization among homeless patients. The secondary outcome measurement was ED disposition failure. ED disposition failure was defined as patients that eloped, left against medical advice (AMA), or left without being seen (LWBS).
2.5. Analysis
We divided all enrolled patients into three groups: (1) homeless patients that only visited hospital regular clinics; (2) homeless patients that only visited the dedicated homeless clinic; and (3) homeless patients that visited both hospital regular clinics and the dedicated homeless clinic. We also matched these patients to their ED visits. Homeless patients who visited the ED were further divided into four groups: (1) homeless ED patients without any clinic visits during study period; (2) homeless ED patients who visited only hospital regular clinics; (3) homeless ED patients who visited only the dedicated homeless clinic; and (4) homeless ED patients who visited both hospital regular clinics and dedicated homeless clinic. General patient characteristics including age, gender, race, and ethnicity were compared among patients of the different groups. Inappropriate ED utilizations, and ED disposition failures were also compared among the different groups. Finally, we analyzed whether the two different types of clinics visited by the homeless patients could be considered as an independent risk factor for inappropriate ED utilization and disposition failures.
We analyzed the continuous variables using either Student t tests for two groups or ANOVA for multiple groups. We used Wilcoxon rank‐sum test for median comparisons and Pearson chi square test for categorical data comparisons between groups. To avoid confounding factors, we used multivariate logistic regressions to examine the relationship between homeless patients visiting different clinics and the outcomes of interest. We fit a multivariable logistic regression model evaluating the association between inappropriate ED use and dedicated homeless clinic use. We also fit a model evaluating the association between ED disposition failure and dedicated homeless clinic use. We adjusted the models by patient age, gender, race, and insurance type. Risk predictors of such outcomes were determined with adjusted odds ratios (OR) with 95% confidence intervals (CI). All analyses were performed using STATA 14.2 software (College Station, TX) with P‐value <0.05 considered statistically significant.
3. RESULTS
A total of 16,323 clinic and 8511 ED visits occurred among 5022 unique homeless patients during the study period, in which 2450 unique homeless patients were seen in hospital regular clinics, 784 patients were seen in dedicated homeless clinic, 688 patients visited both hospital regular clinics and dedicated homeless clinic, and another 1100 patients had no clinic visits. The study detail flow diagram is seen in Figure 1. No significant demographic differences were found between patients seen at the clinics versus those seen in the ED (eg, patients seen at homeless clinics versus patients seen in the ED who also visited homeless clinics, see detail in Table 1). Nor were there significant differences in these characteristics between the clinics.
FIGURE 1.
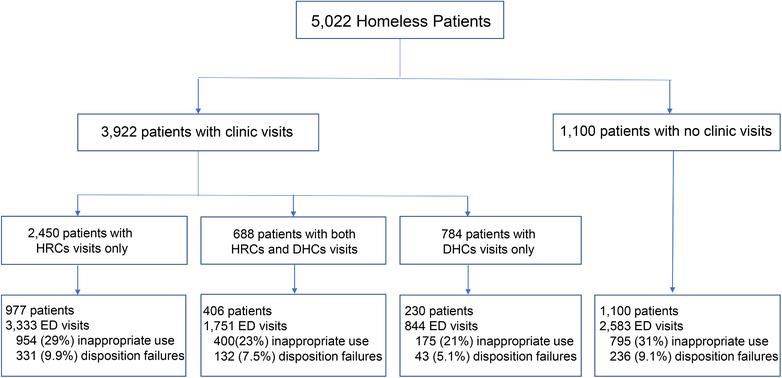
Study flow diagram
TABLE 1.
General characteristics of study patients
| Patients seen at different locations (hospital regular clinics, dedicated homeless clinics, and ED) | ||||||
|---|---|---|---|---|---|---|
| Hospital regular clinics (n = 2450) | ED and hospital regular clinics (n = 977) | Dedicated homeless clinic (n = 784) | ED and dedicated homeless clinic (n = 230) | Hospital regular clinics and dedicated homeless clinic (n = 688) | ED, hospital regular clinics, and dedicated homeless clinic (n = 406) | |
| Age (year) | ||||||
| Median (IQR) | 48 (36, 56) | 48 (36,55) | 51 (41, 56) | 49 (38, 56) | 52 (44, 49 | 51(42,56) |
| Mean (SD) | 46 (13) | 46 (13) | 48 (11) | 47 (11) | (10)57) | 49 (11) |
| Gender, n (%) | ||||||
| Male | 1518 (62) | 616 (63) | 484 (62) | 128 (56) | 426 (62) | 245 (60) |
| Female | 932 (38) | 361 (37) | 300 (38) | 102 (44) | 262 (38) | 161 (40) |
| Race, n (%) | ||||||
| Caucasian | 1164 (48) | 457 (47) | 443 (57) | 134 (58) | 394 (57) | 240 (59) |
| African American | 1099 (45) | 440 (45) | 286 (36) | 79 (34) | 246 (36) | 139 (34) |
| Others | 187 (7) | 80 (8) | 55 (7) | 17 (7) | 48 (7) | 27 (7) |
| Ethnicity, n (%) | ||||||
| Hispanic | 215 (9) | 94 (10) | 58 (7) | 18 (8) | 60 (9) | 36 (9) |
| Non‐Hispanic | 2222 (91) | 881 (90) | 723 (92) | 212 (92) | 627 (91) | 370 (91) |
| Others | 13 (0.5) | 2 (0) | 3 (0.4) | 0 (0) | 1 (0.2) | 0 (0) |
Twenty‐nine percent (230/784) of patients who were seen at dedicated homeless clinic visited the ED during the study period, 40% (977/2450) of patients seen at hospital regular clinics visited the ED (P < 0.001), and 59% (406/688) of patients seen at both dedicated homeless clinics and hospital regular clinics visited the ED during the study period (P < 0.001). In addition, 21% of ED visits from patients seen at dedicated homeless clinic were considered inappropriate ED utilizations in comparison to 29% inappropriate ED visits from patients seen at hospital regular clinics (Table 2, P < 0.001). Meanwhile, 5.1% of dedicated homeless clinic patients had ED disposition failures in comparison to 9.9% that occurred from hospital regular clinics (Table 2, P < 0.01).
TABLE 2.
Comparisons of ED utilization between patients from hospital regular clinics, dedicated homeless clinics, and both clinics
| No clinics (n = 1100) | hospital regular clinics (n = 977) | Both hospital regular clinics and dedicated homeless clinic (n = 406) | dedicated homeless clinic (n = 230) | |
|---|---|---|---|---|
| Percentage of patients utilized ED from different clinics during study period (n) | 40% (977/2450) | 59% (406/688) | 29% (230/784) | |
| Number of ED visits | 2583 | 3333 | 1751 | 844 |
| Average ED visit (times) | ||||
| Median (IQR) | 1 (1, 2) | 2 (1, 5) | 2 (1, 4) | 2 (1, 3) |
| Mode of arrival % (n) | ||||
| Healthcare assisted | 47 (1223/2583) | 44 (1452/3333) | 51 (895/1751) | 45 (379/844) |
| Private cars | 31 (811/2583) | 33 (1101/3333) | 26 (448/1751) | 24 (200/844) |
| Public transportation | 8 (205/2583) | 8 (258/3333) | 8 (136/1751) | 15 (124/844) |
| Ambulatory | 6 (154/2583) | 6 (214/3333) | 6 (107/1751) | 9 (75/844) |
| Others a | 7 (190/2583) | 9 (308/3333) | 9 (165/1751) | 8 (66/844) |
| Level of acuity n (%) | ||||
| ESI‐1 | 15 (0.6) | 24 (0.7) | 10 (0.6) | 3 (0.4) |
| ESI‐2 | 329 (13) | 559 (17) | 264 (15) | 96 (11) |
| ESI‐3 | 1661 (64) | 2111 (63) | 1089 (62) | 588 (70) |
| ESI‐4 | 500 (19) | 548 (16) | 343 (20) | 141 (17) |
| ESI‐5 | 68 (2.6) | 85 (2.6) | 40 (2.3) | 16 (1.9) |
| Unknown | 10 (0.4) | 6 (0.2) | 5 (0.3) | 0 (0) |
| Inappropriate ED utilizations | ||||
| Non‐emergent conditions | 31% (795/2583) | 29% (954/3333) | 23% (400/1751) | 21% (175/844) |
| ED discharge failures | ||||
| AMA/Eloped/LWBS | 9.1% (236/2583) | 9.9% (331/3333) | 7.5% (132/1751) | 5.1% (43/844) |
Others include police, wheelchair, and unknown mode of arrival.
On multivariable logistic regression, dedicated homeless clinic use was independently associated with a decreased odds of inappropriate ED utilization (adjusted odds ratio [AOR] of 0.61, 95% CI = 0.50–0.74). Dedicated homeless clinic use was also independently associated with ED disposition failures (AOR = 0.61, 95% CI = 0.44–0.86, Table 3, P < 0.001).
TABLE 3.
Dedicated homeless clinic reduce inappropriate ED utilization and decrease ED disposition failure (AMA, eloped, and LWBS) using a multivariate logistic regression model
| Inappropriate ED utilization(AOR with 95% CI) | ED disposition failure(AOR with 95% CI) | |
|---|---|---|
| No clinic visits | Reference | Reference |
| Hospital regular clinics | 0.88 (0.79, 0.99) | 1.16 (0.97, 1.39) |
| Dedicated homeless clinics | 0.61 (0.50, 0.74) | 0.61 (0.44, 0.86) |
| Both hospital regular clinics and dedicated homeless clinics | 0.67 (0.58, 0.78) | 0.91 (0.72, 1.15) |
| Age | 1.02 (1.01, 1.02) | 1.00 (1.00, 1.01) |
| Male | Reference | Reference |
| Female | 1.09 (0.98, 1.21) | 0.81 (0.68, 0.96) |
| Caucasian | Reference | Reference |
| African American | 1.63 (1.47, 1.81) | 0.90 (0.77, 1.06) |
| Self‐pay with no insurance | Reference | Reference |
| Charity insurance | 0.96 (0.84, 1.09) | 0.69 (0.56, 0.85) |
| Medicaid insurance | 0.72 (0.63, 0.82) | 0.75 (0.60, 0.92) |
| Medicare insurance | 0.62 (0.53, 0.73) | 0.66 (0.51, 0.85) |
4. LIMITATIONS
Our study has its limitations. First, this is a retrospective, single center study. Given the nature of the study design, information challenges (ie, missing or incorrect data), and patient selection bias cannot be completely avoided. Second, we are not able to consider all confounding factors that could potentially affect homeless patient ED utilization and ED disposition failures, therefore, our findings in this study might be biased. In addition, because we did not measure individual homeless patient chronic disease status, we are unable to compare the frequency of baseline comorbidities among the different groups. Third, these interventions were implemented in a publicly funded hospital. The results cannot be generalized to for‐profit hospital systems. Fourth, this is a single center study, we are unable to analyze homeless patients who visited other local hospitals and EDs, therefore, findings from this study might be limited. Last, because our study period covers only 1 year, we are unable to determine the long‐term effects of these interventions. Taken together, a prospective multi‐center large‐scale study is warranted for external validations.
5. DISCUSSION
An important measure of patient‐centered care is improving healthcare quality while reducing inappropriate ED utilization. 32 This is especially challenging with the homeless patient population. The US government recognizes this challenge and has published the Health Care for the Homeless (HCH) program that emphasizes and supports a multidisciplinary approach to healthcare for the homeless. 20 Interventions include outreach for community collaboration, emphasis on the importance of case management, and the need to actively engage people experiencing homelessness in health care delivery. 20
However, in our healthcare system, these traditional team approaches seem to have less than the desired effect on reducing ED visits and hospitalizations. 2 , 3 In this study, we introduced an alternative intervention by providing a dedicated homeless clinic with several special characteristics. Our findings showed a trend of reduced ED visits and a reduced number of inappropriate ED visits for patients who visited the dedicated homeless clinic. We also found that homeless patients who visited the dedicated homeless clinic tended to have fewer ED disposition failures. Although this is a single center retrospective study, it provides supporting evidence that a dedicated homeless clinic with these features, in addition to the more standard multidisciplinary approach used by others, can produce certain improvements in homeless patients’ healthcare quality. We demonstrate that providing a dedicated homeless clinic with these features attributes improves care and decreases inappropriate ED utilization.
Although providing dedicated homeless clinic decreases inappropriate ED utilization and improves disposition failure among homeless patients, we can see other risk factors affecting their ED utilization and disposition as well. Female homeless patients tended to have less ED disposition failures than male, which has consistent findings with other previous reports. 33 , 34 Patients who had no insurance coverage seem to have higher inappropriate ED utilization and disposition failures, which is also consistent with other reports. 2 , 34 However, no statistically significant differences found in terms of gender in relation to the inappropriate ED utilization. This might partly be because of the limited sample size especially a smaller number of female patients enrolled (<40%, see Table 1) in this study. Certainly, a large‐scaled study will need to be done for validation.
More importantly, according to the study findings, we believe that the combination of features used in our dedicated homeless clinic is the key to reducing inappropriate ED utilization and ED disposition failures. Previous studies demonstrated that there are many barriers to improving the care for the homeless. First, homeless patients often lack transportation. This is a major contributor, more so than housing, to the inappropriate use of EDs due to easy access via emergency medical services to EDs rather than to the less costly medical homes in the community, thereby disrupting continuity of care for these patients. 35 , 36 Second, many homeless clinics rely on volunteer medical providers as staff. The volunteer staff is not often able to provide stable long‐term provider–patient relationships, a prerequisite to a therapeutic medical relationship. 22 , 27 , 37 It has been demonstrated that dedicated family medicine physicians are well suited to manage the needs of homeless patients, providing continuity of care for patients and leadership for multidisciplinary teams. 38 Third, homeless patients often have chronic diseases, suffer from lack of self‐awareness and understanding of their medical condition (particularly regarding prevention, amelioration, and progression) and have a high degree of medical non‐compliance with a poor record of follow‐up in clinics due to a number of issues. 39 , 40 , 41 In our study, the dedicated homeless clinic was designed to overcome previously defined barriers by: (1) locating the dedicated homeless clinic within walking distance of the shelters, thus avoiding transportation issues; (2) recruiting family medicine physicians who are dedicated to providing care to the homeless patient population and who use the dedicated homeless clinic to its full capacity rather than referring care to the ED (we suspect the stability of the staff at the dedicated homeless clinic and the strength of the staff‐patient relationships also contributed to the increased use of the dedicated homeless clinic by clients in preference to the ED); and (3) providing mobile outreach staffed by dedicated, consistent healthcare providers (the street medicine team) to extend care beyond clinic walls into the shelters and the camps, bringing with them access to the integrated electronic health record, along with necessary medical equipment and supplies, thereby providing care similar to traditional hospital regular clinics to inaccessible locations.
On the other hand, none of these interventions are novel and most likely will not produce the same optimal outcomes if performed individually. We demonstrate that better outcomes occurred with the combination of these interventions. Although difficult to definitively prove, we believe the following aspects should be considered: (1) the combination of these specific interventions leads to positive synergistic effects; (2) the clinic's focus on good patient‐staff rapport lays the foundation for stable, trusting relationships which in turn foster better clinical outcomes; and (3) the provision of healthcare beyond the clinic walls integrated with the rest of the health network leads to improved continuity of care, better transitions of care from field to clinic or ED, and improved overall integration. Providing evidence of these links is beyond the scope of this project. Future studies are warranted to investigate these associations.
6. CONCLUSIONS
Implementing a dedicated homeless clinic might reduce ED utilization among homeless patients more than regular hospital clinics. In this study, inappropriate ED visits and ED disposition failures were reduced for these patients who utilized the dedicated homeless clinics. Our findings indicate the possible effectiveness of implementing this combination of interventions in improving healthcare among the homeless population. A large prospective multicenter intervention study is warranted for further validation before applying this concept more broadly across the nation.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
AUTHOR CONTRIBUTIONS
CTH, KAH, and HW conceived the research and designed the study. AM, FL, JH, SS, and RC performed data collection. CTH, KAH, and HW performed analysis. CTH, KAH, FL, JH, JPD, NRZ, and HW drafted the manuscript. CTH, KAH, AM, FL, JH, JPD, NRZ, and HW contributed to data interpretation, critical review, and revisions of the manuscript for important intellectual content. All authors approved the final version of the submitted manuscript and agree to be accountable for all aspects of the work.
Biography
Hao Wang, MD, PhD, is Research Director in the Department of Emergency Medicine, John Peter Smith Health Network, Ft. Worth, TX.

Holmes CT, Holmes KA, MacDonald A, et al. Dedicated homeless clinics reduce inappropriate emergency department utilization. JACEP Open. 2020;1:829–836. 10.1002/emp2.12054
Funding and support: By JACEP Open policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist.
Supervising Editor: Marna Rayl Greenberg, DO, MPH
REFERENCES
- 1. Lombardi K, Pines JM, Mazer‐Amirshahi M, Pourmand A. Findings of a national dataset analysis on the visits of homeless patients to US emergency departments during 2005–2015. Public Health. 2019;178:82‐89. [DOI] [PubMed] [Google Scholar]
- 2. Wang H, Nejtek VA, Zieger D, et al. The role of charity care and primary care physician assignment on ED use in homeless patients. Am J Emerg Med. 2015;33:1006‐1011. [DOI] [PubMed] [Google Scholar]
- 3. Knowles H, Huggins C, Robinson RD, et al. Status of emergency department seventy‐two hour return visits among homeless patients. J Clin Med Res. 2019;11:157‐164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Aldridge RW, Story A, Hwang SW, et al. Morbidity and mortality in homeless individuals, prisoners, sex workers, and individuals with substance use disorders in high‐income countries: a systematic review and meta‐analysis. Lancet. 2018;391:241‐250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Morrison DS. Homelessness as an independent risk factor for mortality: results from a retrospective cohort study. Int J Epidemiol. 2009;38:877‐883. [DOI] [PubMed] [Google Scholar]
- 6. Sadowski LS, Kee RA, VanderWeele TJ, Buchanan D. Effect of a housing and case management program on emergency department visits and hospitalizations among chronically ill homeless adults: a randomized trial. JAMA. 2009;301:1771‐1778. [DOI] [PubMed] [Google Scholar]
- 7. Hwang SW, Burns T. Health interventions for people who are homeless. Lancet. 2014;384:1541‐1547. [DOI] [PubMed] [Google Scholar]
- 8. Wolitski RJ, Kidder DP, Pals SL, et al. Randomized trial of the effects of housing assistance on the health and risk behaviors of homeless and unstably housed people living with HIV. AIDS Behav. 2010;14:493‐503. [DOI] [PubMed] [Google Scholar]
- 9. Messeri PA, Abramson DM, Aidala AA, Lee F, Lee G. The impact of ancillary HIV services on engagement in medical care in New York City. AIDS Care. 2002;14(Suppl 1):S15‐S29. [DOI] [PubMed] [Google Scholar]
- 10. Lin WC, Bharel M, Zhang J, O'Connell E, Clark RE. Frequent emergency department visits and hospitalizations among homeless people with Medicaid: implications for Medicaid expansion. Am J Public Health. 2015;105(Suppl 5):S716‐S722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Moulin A, Evans EJ, Xing G, Melnikow J. Substance use, homelessness, mental illness and Medicaid coverage: a set‐up for high emergency department utilization. West J Emerg Med. 2018;19:902‐906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hategan A, Tisi D, Abdurrahman M, Bourgeois JA. Geriatric homelessness: association with emergency department utilization. Can Geriatr J. 2016;19:189‐194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rosenheck RA, Lam J, Morrissey JP, Calloway MO, Stolar M, Randolph F. Service systems integration and outcomes for mentally ill homeless persons in the ACCESS program. Access to community care and effective services and supports. Psychiatr Serv. 2002;53:958‐966. [DOI] [PubMed] [Google Scholar]
- 14. Smelson DA, Chinman M, Hannah G, Byrne T, McCarthy S. An evidence‐based co‐occurring disorder intervention in VA homeless programs: outcomes from a hybrid III trial. BMC Health Serv Res. 2018;18:332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Knopf‐Amelung SM, Jenkins DM. Identifying US veterans who access services from health care for the homeless clinics. Am J Public Health. 2013;103(suppl 2):S216‐S217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Asgary R, Sckell B, Alcabes A, Naderi R, Schoenthaler A, Ogedegbe G. Rates and predictors of uncontrolled hypertension among hypertensive homeless adults using New York city shelter‐based clinics. Ann Fam Med. 2016;14:41‐46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gabrielian S, Chen JC, Minhaj BP, et al. Feasibility and acceptability of a colocated homeless‐tailored primary care clinic and emergency department. J Prim Care Community Health. 2017;8:338‐344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Doughty J, Stagnell S, Shah N, Vasey A, Gillard C. The crisis at Christmas Dental Service: a review of an annual volunteer‐led dental service for homeless and vulnerably housed people in London. Br Dent J. 2018;224:43‐47. [DOI] [PubMed] [Google Scholar]
- 19. Batra P, Chertok JS, Fisher CE, Manseau MW, Manuelli VN, Spears J. The Columbia‐Harlem Homeless Medical Partnership: a new model for learning in the service of those in medical need. J Urban Health. 2009;86:781‐790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Zlotnick C, Zerger S, Wolfe PB. Health care for the homeless: what we have learned in the past 30 years and what's next. Am J Public Health. 2013;103(suppl 2):S199‐S205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. O'Carroll A, Irving N, O'Neill J, Flanagan E. A review of a GP registrar‐run mobile health clinic for homeless people. Ir J Med Sci. 2017;186:541‐546. [DOI] [PubMed] [Google Scholar]
- 22. Caires AL. Mobile Health Care for People Who Are Homeless. Creat Nurs. 2017;23:151‐157. [DOI] [PubMed] [Google Scholar]
- 23. Matteoli M, Scaringi C, Carella P, Fruttaldo L, Angeloni U, Laurenza M. A mobile health service to manage diabetic foot in homeless patients. J Am Podiatr Med Assoc. 2015;105:424‐428. [DOI] [PubMed] [Google Scholar]
- 24. Smith SD, Rojas SM, Huang J, Yang K, Vaida F. Longitudinal hypertension outcomes at four student‐run free clinic sites. Fam Med. 2017;49:28‐34. [PMC free article] [PubMed] [Google Scholar]
- 25. Swanson KA, Andersen R, Gelberg L. Patient satisfaction for homeless women. J Womens Health. 2003;12:675‐686. [DOI] [PubMed] [Google Scholar]
- 26. O'Toole TP, Johnson EE, Aiello R, Kane V, Pape L. Tailoring care to vulnerable populations by incorporating social determinants of health: the veterans health administration's “Homeless Patient Aligned Care Team” program. Prev Chronic Dis. 2016;13:E44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Steinbach A, Swartzberg J, Carbone V. The Berkeley Suitcase Clinic: homeless services by undergraduate and medical student teams. Acad Med. 2001;76:524. [DOI] [PubMed] [Google Scholar]
- 28. Reynolds HY. Free medical clinics: helping indigent patients and dealing with emerging health care needs. Acad Med. 2009;84:1434‐1439. [DOI] [PubMed] [Google Scholar]
- 29. Gawron L, Pettey WBP, Redd A, Suo Y, Turok DK, Gundlapalli AV. The “Safety Net” of community care: leveraging GIS to identify geographic access barriers to Texas family planning clinics for homeless women veterans. AMIA Annu Symp Proc. 2017;2017:750‐759. [PMC free article] [PubMed] [Google Scholar]
- 30. Ballard DW, Price M, Fung V, et al. Validation of an algorithm for categorizing the severity of hospital emergency department visits. Med Care. 2010;48:58‐63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Gandhi SO, Sabik L. Emergency department visit classification using the NYU algorithm. Am J Manag Care. 2014;20:315‐320. [PubMed] [Google Scholar]
- 32. Fryer AK, Friedberg MW, Thompson RW, Singer SJ. patient perceptions of integrated care and their relationship to utilization of emergency, inpatient and outpatient services. Healthc. 2017;5:183‐193. [DOI] [PubMed] [Google Scholar]
- 33. Carli A, Moretti F, Giovanazzi G, et al. “Should I stay or Should I go”: patient who leave emergency department of an Italian Third‐Level Teaching Hospital. Acta Biomed. 2018;89:430‐436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Tropea J, Sundararajan V, Gorelik A, Kennedy M, Cameron P, Brand CA. Patients who leave without being seen in emergency departments: an analysis of predictive factors and outcomes. Acad Emerg Med. 2012;19:439‐447. [DOI] [PubMed] [Google Scholar]
- 35. Crawley J, Kane D, Atkinson‐Plato L, Hamilton M, Dobson K, Watson J. Needs of the hidden homeless ‐ no longer hidden: a pilot study. Public Health. 2013;127:674‐680. [DOI] [PubMed] [Google Scholar]
- 36. Durant E, Fahimi J. Factors associated with ambulance use among patients with low‐acuity conditions. Prehosp Emerg Care. 2012;16:329‐337. [DOI] [PubMed] [Google Scholar]
- 37. Baker J, Travers JL, Buschman P, Merrill JA. An efficient nurse practitioner‐led community‐based service model for delivering coordinated care to persons with serious mental illness at risk for homelessness [Formula: see text]. J Am Psychiatr Nurses Assoc. 2018;24:101‐108. [DOI] [PubMed] [Google Scholar]
- 38. Maness DL, Khan M. Care of the homeless: an overview. Am Fam Physician. 2014;89:634‐640. [PubMed] [Google Scholar]
- 39. Moro RN, Sterling TR, Saukkonen J, et al. Factors associated with non‐completion of follow‐up: 33‐month latent tuberculous infection treatment trial. Int J Tuberc Lung Dis. 2017;21:286‐296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Coe AB, Moczygemba LR, Gatewood SB, Osborn RD, Matzke GR, Goode JV. Medication adherence challenges among patients experiencing homelessness in a behavioral health clinic. Res Social Adm Pharm. 2015;11:e110‐e120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Chong MT, Yamaki J, Harwood M, et al. Assessing health conditions and medication use among the homeless community in Long Beach, California. J Res Pharm Pract. 2014;3:56‐61. [DOI] [PMC free article] [PubMed] [Google Scholar]


