Abstract
While the beneficial impact of moderate-vigorous physical activity (MVPA) on blood pressure is well-understood, the relationship between sedentary time (ST) and blood pressure is less clear. We aimed to evaluate the associations between ST and BP in reproductive-age women. This cross-sectional analysis consisted of 431 women enrolled in the Placenta as a Window to Maternal Microvascular Disease Risk study at Magee-Womens Hospital. Blood pressure and self-reported physical activity and ST were collected 8–10 years after delivery at study enrollment. Logistic and linear regression models examined associations between ST and blood pressure and adjusted for MVPA. Women with the highest amount of ST were less likely to be normotensive and more likely to have elevated blood pressure and Stage II hypertension (p = 0.02). Each additional hour of ST was associated with an increased risk of Stage II hypertension (OR 1.12 [1.01–1.24]) and higher systolic blood pressure (0.45 mmHg [0.08–0.82]), diastolic blood pressure (0.29 mmHg [0.02–0.56]), and mean arterial pressure (0.34 mmHg [0.05–0.63]), after adjustment for covariates. This relationship was more apparent in women who participated in less MVPA (bottom 50th percentile) versus more MVPA (top 50th percentile). ST is associated with higher blood pressure, particularly in women who engage in less aerobic activity, and could serve as an important intervention target for reducing blood pressure and hypertension during the reproductive years.
Keywords: Women, Blood pressure, Hypertension, Sedentary behavior, Physical activity, BMI, Cardiovascular disease risk factors, Lifestyle interventions
1. Introduction
Cardiovascular disease (CVD) is the leading cause of death in women and is now understood as a life course disease, with risk accumulating even in young adulthood (Loria et al., 2007). Many reports in the literature describe the association of moderate-vigorous physical activity (MVPA) and sedentary time (ST), defined as energy expenditure < 1.5 metabolic equivalents while in a sitting or reclining position, with CVD and cardiovascular morbidity and mortality in the broader population, and in women specifically (Chomistek et al., 2013, Brocklebank et al., 2015, Biswas et al., 2015, Whitaker et al., 2019, Thorp et al., 2011).
Hypertension is an important risk factor in the development of CVD, and contributes to more CVD events in women compared to men (Figueiró et al., 2019, Cheng et al., 2014). Of the major modifiable CVD risk factors, complete elimination or control of hypertension resulted in the largest impact on CV mortality in women (Patel et al., 2016, Abramson and Melvin, 2014). The reproductive years may be of particular importance, as blood pressure trajectories across the life course rise more steeply in women than men, and this rise begins in women in their 20′s (Ji et al., 2020). The beneficial effects of moderate-vigorous intensity physical activity (MVPA) for blood pressure control are well-studied, and regular MVPA is recommended to prevent the development of hypertension and cardiovascular disease (Poulter et al., 2015, Whelton et al., 2018). Increasingly, sedentary behavior is recognized a potential risk factor for hypertension that is additional to insufficient MVPA (Tremblay et al., 2017). The current literature on the effects of prolonged sedentary time on blood pressure, however, demonstrates variability. Though higher ST has not been consistently associated with hypertension (Whitaker et al., 2019, Healy et al., 2011, Qi et al., 2015), some evidence, including observational (Lee and Wong, 2015) and experimental studies, suggest that higher ST is associated with elevated blood pressure, and breaking up prolonged periods of sedentary time results in blood pressure reductions (Bakker et al., 2018, Barone Gibbs et al., 2017, Dempsey et al., 2016). Moreover, the synergistic effect of MVPA and ST on blood pressure is still not well-understood overall and is even less understood in women specifically. This relationship is important as evidence suggests that meeting the minimum guidelines for PA may not be sufficient for chronic disease prevention if accompanied with excessive ST (Thorp et al., 2011).
The aim of this study was to investigate the association of sedentary time with blood pressure in reproductive age women. Understanding this relationship is important, as there is growing emphasis on nonpharmacologic strategies, such as lifestyle modifications, to meet new, lower blood pressure targets (Wright et al., 2016, Dempsey et al., 2018). Conventional guidelines focus on increasing moderate-vigorous activity, however strategies that focus on minimizing sedentary behaviors also have the potential for lowering incidence and prevalence of hypertension, particularly in women who have lower rates of exercise adherence and higher rates of inactivity (Katzmarzyk, 2010, Hallal et al., 2012).
2. Methods
2.1. Study population
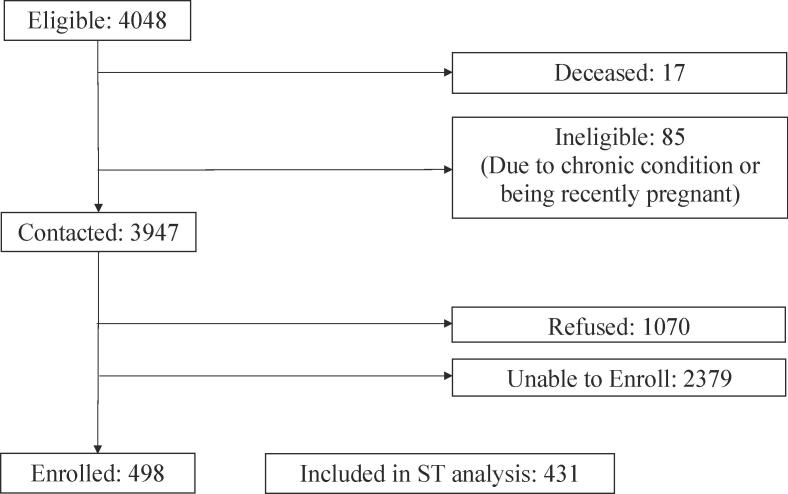
This cross-sectional analysis studied the association of self-reported sedentary behavior with blood pressure and hypertension in women of reproductive age. Eligible women were those with deliveries in 2008–2009 identified from the Magee Obstetric Maternal and Infant (MOMI) database at the University of Pittsburgh, a clinical cohort of women with detailed pregnancy data abstracted from medical records. About 45% of deliveries (n = 4,048) had placental pathology specimen collection at time of delivery for clinical indications, and those with these data were the source population for the study (Catov et al., 2015). Of the 3947 women who were eligible (Alive, non-pregnant and without chronic hypertension prior to the index pregnancy), 1070 declined to participate, 2379 were unable to be contacted, and 498 enrolled (Fig. 1). Enrolled women were, on average, slightly older, more likely to be of African American race/ethnicity and less likely to smoke compared to those who refused or were unable to be contacted. There were no differences in these groups according to pregnancy complications (Table 1). Enrolled women completed a cardiovascular screening visit designed to investigate the relationship between placental malperfusion and later life cardiometabolic and microvascular disease risk (The Placenta as a Window to Maternal Microvascular Disease Study, Window Study) and 431 are included in this analysis with complete sedentary and MVPA data at the time of this analysis. Data collected during this visit included a complete health and reproductive history, blood pressure measurement, anthropometry, and self-reported physical activity. The study was approved by the University of Pittsburgh IRB and women provided written informed consent.
Fig. 1.
Window Study Enrollment.
Table 1.
Maternal characteristic of those enrolled, ineligible, refused and unable to enroll in Windows Study.
| Enrolled |
Ineligible |
Refused |
Unable to enroll |
||
|---|---|---|---|---|---|
| n = 498 | n = 102 | n = 1069 | n = 2379 | p-value | |
| Age, years (SD) | 28.5 (6.0) | 26.1 (5.6) | 28.4 (5.9) | 27.1 (6.1) | <0.001 |
| Race/Ethnicity, n (%) | |||||
| White | 308 (63.0%) | 65 (64.4%) | 762 (73.0%) | 1532 (65.5%) | <0.001 |
| African Amerian | 177 (36.2%) | 35 (34.7%) | 273 (26.1%) | 778 (33.3%) | |
| Other | 4 (0.8%) | 1 (1.0%) | 9 (0.8%) | 29 (1.2%) | |
| Smoking, n (%) | 84 (18.2%) | 37 (39.4%) | 151 (15.6%) | 522 (23.7%) | <0.001 |
| Gestational diabetes, n (%) | 40 (8.1%) | 4 (4.0%) | 90 (8.5%) | 198 (8.4%) | 0.461 |
| Gestational hypertension, (%) | 39 (7.9%) | 8 (7.9%) | 73 (6.9%) | 162 (6.8%) | 0.845 |
| Preeclampsia, n (%) | 73 (14.7%) | 15 (14.9%) | 145 (13.6%) | 313 (13.2%) | 0.815 |
| Preterm birth < 37 weeks, n (%) | 111 (22.3%) | 21 (20.6%) | 224 (21.0%) | 504 (21.2%) | 0.939 |
3. Sedentary behavior and physical activity
At the Window study visit, women self-reported ST and physical activity. To obtain ST, we used the single item from the Global Physical Activity Questionnaire which asks women to estimate the total amount of time spent sitting and reclining on a typical day (in hours or minutes). Validation and reliability studies demonstrate that this instrument is acceptable for monitoring activity behavior, including sedentary time, and more precise than other self-report measures compared to gold standard objective measures (Bull et al., 2009, Chastin et al., 2018). Women were then asked about their physical activity over the past year using questions adapted from the Paffenberger Physical Activity Questionnaire (Laporte et al., 1983, Ainsworth et al., 1993). They were asked to describe the frequency and duration of up to 14 activities in which they participated. Trained coders then assigned each activity an intensity level [metabolic equivalent (MET)], based on the Physical Activity Compendium (AINSWORTH et al., 2011). The MET value was multiplied by the frequency (times per week or month) and duration (minutes or hours per episode) of each activity to obtain volume for each activity (MET-minutes per week). Total volume of MVPA was calculated by summing MET-minutes per week across all activities greater than 3 METs that were reported.
For stratified analyses by MVPA level, we determined the adequacy of each participant’s exercise regimen based on the guidelines of 150 min of moderate-intensity activity per week, 75 min of vigorous activity per week, or an equivalent combination of moderate and vigorous activity (United States, Department of Health and Human Services, 2008). Moderate activity was defined as physical activity with an intensity greater than or equal to 3 METS and less than 6 METs and vigorous activity was defined as activity greater than or equal to 6 METs. We then calculated the total number of minutes per week spent in the moderate and vigorous intensity level and classified participants as meeting or failing to meet Guidelines. MVPA was also stratified above and below the median for the study population.
4. Blood pressure
Blood pressure was collected during the Window study visit following a standard research protocol. Following five minutes of rest, trained research staff collected three separate readings with one minute between each measurement using a validated automated device (Microlife A6 PC / BP 3GUI-8X). Arm circumference was measured to ensure an appropriately sized cuff was used. The average systolic blood pressure (SBP) and diastolic blood pressure (DBP) were calculated. Mean arterial pressure (MAP) was estimated based on SBP and DBP using the equation MAP = [SBP + (2*DBP)]/3. Additionally, blood pressure was classified as normotensive, elevated blood pressure, Stage 1 or Stage 2 hypertensive based on current American College of Cardiology hypertension guidelines (Normotensive: <120/80 mmHg; Elevated: Systolic 120–129 mmHg and diastolic < 80 mmHg; Stage 1: Systolic 130–139 mmHg or diastolic 80–89 mmHg; Stage 2: Systolic at least 140 mmHg or diastolic at least 90 mmHg or currently on anti-hypertensives) (Whelton et al., 2018).
5. Covariates
Study covariates included maternal age at enrollment in the Window study, race, years of education completed, smoking history, season, medication use for blood pressure and MVPA (Tucker and Gilliland, 2007). We also included a model that adjusted for BMI, based on measured height (using a stadiometer) and weight (Tanita scale TBF-300A) obtained at the Window study visit after women removed shoes, socks, and excessive clothing.
6. Analysis
Descriptive statistics were calculated and compared by tertiles of sedentary minutes per day (low, moderate, high) and median MVPA (bottom 50th percentile vs. top 50th percentile). Means and SDs or medians and interquartile ranges were calculated for maternal characteristics, physical activity, sedentary behavior, and blood pressure. Differences between tertiles of ST and percentiles of MVPA were examined using Chi-square and Analysis of Covariance (ANCOVA). p < 0.05 was considered statistically significant. Only women with complete data were included in the analysis.
Multivariable linear and logistic regression models were used to measure the association between sedentary behavior and BP, with BP as a continuous and categorical endpoint, respectively. Sequential models adjusted for demographics (age, race, years of education), smoking, antihypertensive medication use, and log-transformed MVPA. A final model adjusted for BMI, with the understanding that this may be an over adjustment as increased BMI may be a mechanism through which high sedentary behavior contributes to elevated blood pressure. Multivariable linear regression analyses were repeated after stratification by median MVPA to observe whether associations differed in less active women versus more active women, based on prior evidence showing that ST is more deleterious in groups with lower levels of aerobic physical activity (Biswas et al., 2015, Ekelund et al., 2019) and evidence that the association between ST and hypertension in our data may vary by MVPA (Pinteraction = 0.07). Sequential models were adjusted for demographics and BMI as above and MVPA to avoid residual confounding within subgroups. All statistical analyses were performed using SAS 9.4 TS1M3 for Windows.
7. Results
At the time of analysis, 435 women were enrolled in the WINDOW parent study. Physical activity and sedentary time data were available for 431 women. In our diverse cohort, 32.3% of participants identified as African-American and 67.5% as White/other. Forty-six percent of women had an income below $50,000. Women in our cohort had a range of education backgrounds; 19.7% had a high school diploma or less, 34.4% had some college or technical training, and 45% were college graduates.
Physical activity differed by tertile of ST (Table 2). Women who were the least sedentary (lowest tertile) had the greatest amount of MVPA per week, whereas women who were the most sedentary (highest tertile) had the least MVPA per week (360 mins vs. 216 mins, p = 0.001). Related, women in the lowest ST tertile had higher MVPA MET-mins per week than the high ST group (1500 MET-mins vs. 924 MET-mins, p = 0.001). Women in the highest tertile ST had the lowest percentage of women meeting MVPA exercise recommendations, albeit non-significant (p = 0.2812).
Table 2.
Maternal characteristics and sedentary time and physical activity measures of Window participants at Magee-Womens Hospital, by tertiles of ST.a
| Sedentary Time |
||||
|---|---|---|---|---|
| Baseline characteristics | Low ST (n = 127) |
Moderate ST (n = 152) |
High ST (n = 152) |
p-value |
| Maternal age: Mean (SD) | 37.3 (6.2) | 37.3 (5.9) | 38.7 (6.0) | 0.083 |
| Race: n (%) African-American White/other |
41.0 (32.3) 86.0 (67.7) |
52.0 (34.4) 99.0 (65.6) |
46.0 (30.3) 106.0 (69.7) |
0.740 |
| Income: n (%) <$20,000 $20–49,999 $50–99,999 >$100,000 Prefer to not answer |
22.0 (17.3) 38.0 (29.9) 31.0 (24.4) 35.0 (27.6) 1.0 (0.8) |
38.0 (25.0) 41.0 (27.0) 26.0 (17.1) 44.0 (29.0) 3.0 (2.0) |
18.0 (11.8) 39.0 (25.7) 37.0 (24.3) 51.0 (33.6) 7.0 (4.6) |
0.052 |
| Education: n (%) HS Diploma or less Some college/Vo-Tech/Associates degree College graduate Other |
32.0 (25.2) 48.0 (37.8) 46.0 (36.22) 1.0 (0.79) |
34.0 (22.4) 53.0 (34.9) 64.0 (42.1) 1.0 (0.7) |
19.0 (12.5) 47.0 (30.9) 84.0 (55.3) 2.0 (1.3) |
0.031 |
| Insurance: n (%) Medicaid/Medicare Private None |
41.0 (32.3) 83.0 (65.4) 3.0 (2.4) |
58.0 (38.4) 92.0 (60.9) 1.0 (0.7) |
36.0 (23.7) 114.0 (75.0) 2.0 (1.32) |
0.060 |
| Current smoker: n (%) | 27.0 (21.2) | 35.0 (23.0) | 27.0 (17.8) | 0.441 |
| Season: n (%) Fall Winter Spring Summer |
38.0 (29.9) 29.0 (22.8) 32.0 (25.2) 28.0 (22.1) |
39.0 (25.7) 36.0 (23.7) 34.0 (22.4) 43.0 (28.3) |
43.0 (28.3) 41.0 (27.0) 26.0 (17.1) 42.0 (27.6) |
0.613 |
| Body mass index (BMI) Mean (SD) Category: n (%)b Under/Normal weight Overweight Obese |
29.3 (7.6) 44.0 (34.7) 32.0 (25.2) 51.0 (40.2) |
30.0 (8.3) 49.0 (32.2) 42.0 (27.6) 61.0 (40.1) |
31.7 (7.9) 35.0 (23.0) 39.0 (25.7) 78.0 (51.3) |
0.039 0.157 |
| Blood pressure – mmHg: Mean (SD) Systolic Diastolic Mean arterial |
115.0 (12.8) 75.6 (10.1) 88.8 (10.6) |
115.8 (13.9) 75.4 (11.0) 88.8 (11.4) |
118.4 (15.9) 77.3 (11.0) 91.0 (12.0) |
0.120 0.227 0.154 |
| Currently on anti-hypertensive medication: n (%) | 7.0 (5.5) | 14.0 (9.2) | 15.0 (9.9) | 0.379 |
| Total sedentary minutes per day: Median (IQR) | 120.0 (120.0–180.0) | 300.0 (240.0–360.0) | 600.0 (480.0–660.0) | <0.0001 |
| Total sedentary hours per day: Median (IQR) | 2.0 (2.0–3.0) | 5.0 (4.0–6.0) | 10.0 (8.0–11.0) | <0.0001 |
| Women meeting MVPA exercise guidelinesc: n (%) | 96.0 (75.6) | 110.0 (72.4) | 102.0 (67.1) | 0.281 |
| Total minutes of MVPA per week: Median (IQR) | 360.0 (150.0–630.0) | 289.0 (120.0–701.0) | 216.0 (90.0–413.0) | 0.001 |
| MVPA MET-mins per week: Median (IQR) | 1500.0 (552.0–2940.0) | 1270.0 (436.0–3143.0) | 924.0 (338.0–1905.0) | 0.001 |
a Tertiles of ST defined as low=less than 4 hours per day, moderate=4 to less than 7 hours per day, and high=greater than 7 hours per day.
b Overweight=BMI 25.0-29.9, Obese=BMI 30.0 and greater
c Adequate exercise regimen defined as >=150 minutes of moderate activity per week, >=75 minutes of vigorous activity per week, or a combination of moderate and vigorous equal to those guidelines
Women with in the highest tertile of ST were similar to other groups in terms of race, but on average, were more likely to have higher incomes, albeit non-significant, (p = 0.05) and more years of education completed (p = 0.031) compared to the women in other groups (Table 2). Additionally, women in the highest tertile of ST had a higher average BMI than women with low and moderate ST. Women below the median MVPA minutes per week were similar to the group of women above the median in terms of sociodemographic factors. The group of women in the top 50th percentile of MVPA minutes per week had a lower average BMI (30.2 vs 30.6, p = 0.013; see supplemental material, Table 2a).
Women in the highest tertile of ST were less likely to be normotensive and were more likely to have elevated blood pressure and Stage II hypertension (Fig. 2), despite no difference in mean SBP, DBP, and MAP between tertiles of ST. Use of anti-hypertensive medications did not differ significantly between groups (Table 2). Interestingly, there were no differences in hypertension diagnoses between the women above and below the median MVPA minutes per week (see supplemental material, Fig. 2a).
Fig. 2.
Chi-square analysis, p-value testing hypothesis that there is difference in distribution of blood pressure categories between tertiles of ST. aNormotensive: Less than 120/80 mmHg; Elevated: Systolic 120–129 mmHg and diastolic <80 mmHg; Stage 1: Systolic 130–139 mmHg or diastolic 80–89 mmHg; Stage 2: Systolic at least 140 mmHg or diastolic at least 90 mmHg or currently on anti-hypertensives.
Each additional hour of ST per day was associated with increased risk of Stage II hypertension when adjusted for demographic factors, smoking history, anti-hypertensive medications and log-transformed MVPA (OR 1.12 [95% CI 1.01–1.24]; Table 3). This was attenuated when accounting for BMI (OR 1.09 [95% CI 0.99–1.21]). There was no increased risk of elevated BP or Stage I hypertension with higher ST, after accounting for covariates.
Table 3.
Multinomial logistic regression analysis of hypertension diagnosis by amount of ST; excluding women on anti-hypertensive medications (n = 395).
|
Elevated (n = 221) |
Stage I HTN (n = 71) |
Stage II HTN (n = 59) |
||||
|---|---|---|---|---|---|---|
| ST (hrs/day) | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value |
|
Model 1 Model 2 Model 3 |
1.08 (0.99–1.18) 1.09 (0.99–1.19) 1.05 (0.96–1.16) |
0.081 0.074 0.311 |
1.06 (0.99–1.14) 1.06 (0.99–1.14) 1.04 (0.96–1.12) |
0.083 0.101 0.323 |
1.11 (1.00–1.22) 1.12 (1.01–1.24) 1.09 (0.99–1.21) |
0.042 0.032 0.095 |
Odds ratio (OR) represents increased risk of hypertension for each additional hour of ST per day; reference group=elevated blood pressure.
Model 1: adjusts for age, race, education level, current smoking, and anti-hypertensive medication.
Model 2: Model 1 + log-transformed MVPA.
Model 3: Model 2 + BMI.
Multivariable linear regression showed that each additional hour of ST was associated with a higher SBP (Β = 0.45 mmHg [0.08–0.82]), DBP (Β = 0.29 mmHg [0.02–0.56]), and MAP (Β = 0.34 mmHg [0.05–0.63]) when adjusted for covariates (Table 4). These associations were attenuated after adjustment for BMI.
Table 4.
Multivariable linear regression analysis of blood pressure by amount of ST; excluding women on anti-hypertensive medications (n = 395).
|
SBP |
DBP |
MAP |
||||
|---|---|---|---|---|---|---|
| ST (hrs/day) | β (95% CI) | p-value | β (95% CI) | p-value | β (95% CI) | p-value |
|
Model 1 Model 2 Model 3 |
0.42 (0.05–0.79) 0.45 (0.08–0.82) 0.26 (−0.11 to 0.63) |
0.023 0.018 0.166 |
0.42 (0.05–0.79) 0.29 (0.02–0.56) 0.18 (−0.09 to 0.50) |
0.023 0.037 0.200 |
0.33 (0.04–0.62) 0.34 (0.05–0.63) 0.20 (−0.9 to 0.50) |
0.023 0.020 0.162 |
Beta (β) represents increase in blood pressure (mmHg) for each additional hour of ST per day.
Model 1: adjusts for age, race, education level, current smoking, and anti-hypertensive medication.
Model 2: Model 1 + log-transformed MVPA.
Model 3: Model 2 + BMI.
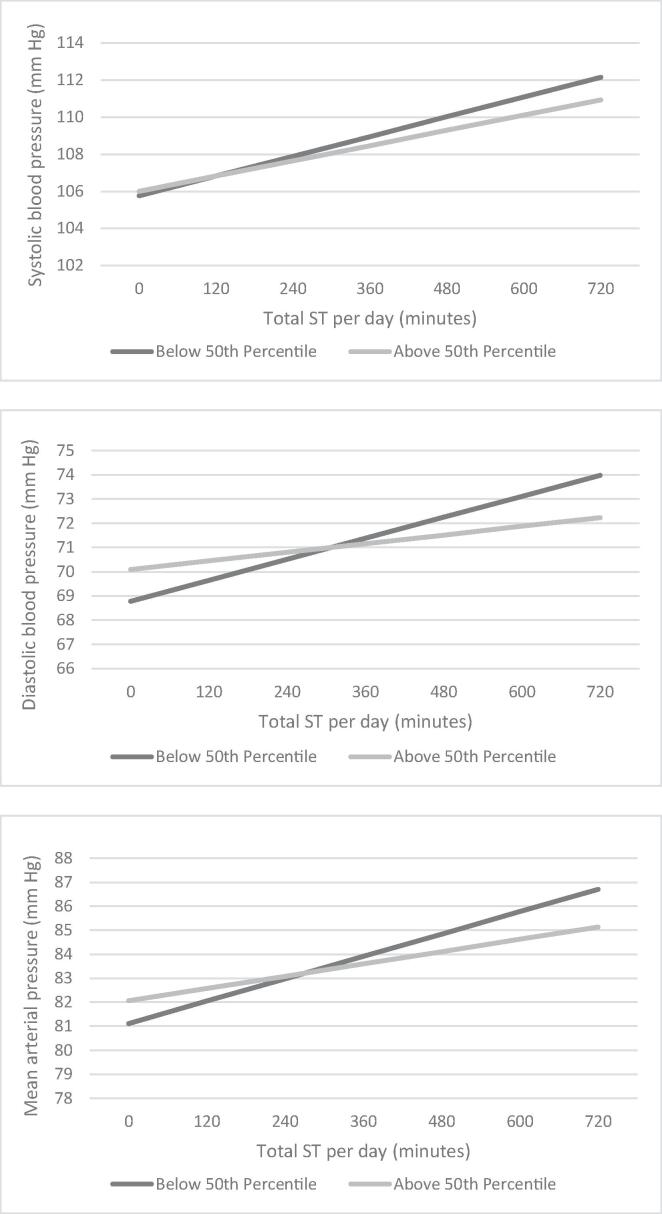
The linear associations between ST and blood pressure were more pronounced and retained statistical significance in women who were below the 50th percentile of total MVPA minutes per week (Table 5, Fig. 3). Each additional hour of ST was associated with a statistically significant higher SBP (Β = 0.53 mmHg [0.06–1.00], p = 0.03), DBP (Β = 0.43 mmHg [0.10–0.76], p = 0.01), and MAP (Β = 0.47 mmHg [0.10–0.84], p = 0.10), in women who were below the median MVPA minutes per week. These associations were again attenuated once adjusted for BMI.
Table 5.
Multivariable linear regression analysis of blood pressure by amount of ST; stratified by median total MVPA minutes per week (n = 395).a
|
SBP |
DBP |
MAP |
||||
|---|---|---|---|---|---|---|
| ST (hrs/day) | β (95% CI) | p-value | β (95% CI) | p-value | β (95% CI) | p-value |
| Below 50th Percentile – MVPA (n = 197) | ||||||
|
Model 1 Model 3 |
0.53 (0.06–1.00) 0.33 (−0.14 to 0.80) |
0.030 0.170 |
0.43 (0.10–0.76) 0.34 (0.01–0.67) |
0.010 0.050 |
0.47 (0.10–0.84) 0.47 (0.10–0.84) |
0.010 0.070 |
| Above 50th Percentile – MVPA (n = 198) | ||||||
|
Model 1 Model 3 |
0.41 (−0.20 to 1.0) 0.25 (−0.34 to 0.84) |
0.310 0.400 |
0.18 (−0.27 to 0.63) 0.04 (−0.41 to 0.37) |
0.440 0.850 |
0.26 (−0.21 to 0.73) 0.11 (−3.6 to 0.58) |
0.290 0.640 |
Beta (β) represents increase in blood pressure (mmHg) for each additional hour of ST per day.
a Median MVPA minutes per week was 262.9 minutes.
b Model 1 adjusts for age, race, education level, current smoking, and anti-hypertensive medication.
c Model 3 adjusts for Model 1 + log-transformed MVPA and BMI.
Fig. 3.
Plot of ST and blood pressure; stratified by median of total MVPA minutes per week. aAdjusts for age, race, education level, current smoking, anti-hypertensive medication, and log-transformed MVPA, bMedian MVPA minutes per week was 262.9 minutes.
8. Discussion
The primary findings of this cross-sectional study were that higher self-reported ST was modestly associated with higher blood pressure in women of reproductive age once adjusted for MVPA, and this relationship was more prominent in women with less MVPA. Additionally, we showed that higher ST was cross-sectionally associated with an higher risk of stage II hypertension. These associations persisted even with adjustment for covariates, including MVPA, but were attenuated with adjustment for BMI, suggesting that higher adiposity may play a role in these associations.
The current literature on the relationship between ST and blood pressure is primarily from observational and acute experimental studies, and evidence to date has been heterogeneous and inconsistent (Dempsey et al., 2018). Additionally, there are almost no sex-specific reports. From a physiologic standpoint, many potential underlying mechanisms by which sedentary behavior modulates blood pressure exist. Evidence shows that insulin resistance (Dempsey et al., 2016) and circulating vasoconstrictive mediators (Dempsey et al., 2016, Law et al., 2009) increase during periods of prolonged sitting. It is possible that over time, these perturbations may promote oxidative stress and low-grade inflammation that subsequently contributes to the development of hypertension and vascular damage (Dempsey et al., 2018).
Despite these plausible mechanisms, previous cross-sectional studies from Healy et al. and Qi et al. have shown that ST was not associated with systolic and diastolic blood pressure (Qi et al., 2015, Healy et al., 2015). Similarly, Whitaker et al. did not see significant longitudinal changes in blood pressure after replacement of ST with light-intensity physical activity or MVPA. However, an accumulating body of evidence points to the importance of breaking up prolonged periods of sitting for BP control. In randomized trials from Larsen et al, Dempsey et al., and our group, blood pressure reductions by interrupting periods of prolonged sitting with standing, light or moderate-vigorous intensity PA were observed (Barone Gibbs et al., 2017, Dempsey et al., 2016, Zeigler et al., 2016, Larsen et al., 2014). Interestingly, some studies have shown that such reductions in blood pressure with activity breaks during prolonged sedentary bouts have been more pronounced in at-risk populations including those with obesity, type II diabetes mellitus, and overt hypertension (Dempsey et al., 2016, Dempsey et al., 2018, Larsen et al., 2014).
One explanation for the variation in evidence is the difference in measurement methodologies across studies. The current literature consists of a mix of self-report and objective activity data, which makes comparison challenging (Healy et al., 2011). Additionally, studies have heterogenous demographics, particularly by age, which contributes to small effect sizes (Dempsey et al., 2018). This study had a relatively homogenous group by age and gender, with minimal use of anti-hypertensive therapy, which may have allowed us to observe associations between sedentary time and blood pressure. Another possibility is that the effect of ST on blood pressure may be more pronounced in participants with minimal MVPA. Our study supports this explanation, as the association between ST and blood pressure was independent of MVPA and we demonstrated that ST was more strongly related to blood pressure among women with lower MVPA. Our findings support the need for future studies to clarify the associations we detected using gold-standard objective measurement of ST.
Our findings revealed that the associations between sedentary time and blood pressure were attenuated once accounting for BMI. Based on the cross-sectional nature of our study, and some studies suggesting sedentary behavior is bidirectionally associated with BMI, we are unable to disentangle whether BMI is a confounding variable or is a mediator on the pathway to elevated blood pressure in women with increased ST (Pedisic et al., 2014, Barone Gibbs et al., 2020). It is possible that the association we observed between ST and blood pressure is simply due to confounding by obesity. However, obesity is a major risk factor for the development of hypertension (Hall, 2000, Hall et al., 2002, Frohlich, 2002), and comparably more research suggests sedentary behavior is longitudinally associated with increased BMI than the opposite direction of this effect (Katzmarzyk et al., 2019, Barone Gibbs et al., 2017). Thus, BMI is likely both a mediator and confounder of the association between ST and BP and, further, the significant association we observed without BMI adjustment may be appropriate and meaningful. Future studies with longitudinal and experimental designed will be needed to more definitely quantify the direct effect of ST on BP.
Another important finding in our study was the differences in ST and MVPA based on educational attainment and income. In our cohort, women who were the most sedentary were also found to have the least amount of MVPA per week. These women were more likely to be of a higher income bracket and have completed more years of education. These findings may suggest that occupation plays an important role in health behaviors and that women of higher socioeconomic status may have occupations that promote a more sedentary lifestyle.
The clinical significance of these results is that blood pressure elevations may be a mechanism by which sedentary behavior leads to increased cardiovascular morbidity and mortality in women. Our results showed increased risk of Stage II hypertension with higher ST, suggesting it is possible that sedentary behaviors may hasten the progression of hypertension in women who are susceptible to blood pressure elevations. This was further supported by our findings that women who were below the median MVPA showed a more significant association between ST and blood pressure. Thus, reducing ST may serve as a strategy for decreasing blood pressure, particularly in women who engage in less aerobic activity. While the effect size in our study was modest, the replacement of 7.8 h of ST, the difference between women in the high and low ST groups, with more metabolically demanding activity, could be associated with a 3.5 mmHg decrease in blood pressure. Additionally, it is possible that the association between ST and blood pressure demonstrates a threshold effect in which ST becomes riskier at the most excessive levels. These possibilities need to be tested in ST interventions, as it is also possible that interruptions in long bouts of ST may also be beneficial for blood pressure.
From a public health standpoint, these findings further support the growing need for sedentary behavior guidelines in the United States (Katzmarzyk et al., 2019). Additional studies, including randomized control trials that experimentally decrease ST, are needed to further inform sedentary behavior recommendations.
The limitations of our study include self-reported ST and physical activity rather than objective measurement with an inclinometer (sedentary behavior) (Chastin et al., 2018) or accelerometer (physical activity) (Lee and Shiroma, 2014). While objective measures are superior to self-report measures, one validation shows that of all self-report methods, a single item measure to assess the proportion of the day spending sitting, as was used in our study, showed the best precision compared to objective measures (Chastin et al., 2018). Another limitation is that our study is cross-sectional in nature, so we were unable to establish any temporal relationships. The cross-sectional nature and small to moderate sample size also limits the representativity of our sample. Notably, the women in our study engaged in more MVPA than the general population which limits the generalizability of our findings (Song et al., 2020). Moreover, the small to moderate sample size reduces the power of our findings, particularly those of the subgroup analysis. Strengths of our study include the robust sampling of a diverse group of women for whom we have sedentary and physical activity data. Additionally, women of reproductive age are an understudied but clinically important group in the literature on consequences of sedentary behavior.
9. Conclusion
More time spent in self-reported sedentary behavior was associated with higher blood pressure and higher risk of stage II hypertension, even after adjustment for MVPA, in women of reproductive age. This relationship was only apparent in women with less participation in MVPA. BMI plays an important role in this relationship as either a modifier or confounder which will need to be further elucidated. Nevertheless, these findings suggest that minimizing ST may be a novel intervention target to reduce the development of hypertension in susceptible women.
Funding
American Heart Association Strategically Focused Center Go Red for Women Research Network at Magee-Womens Research Institute (16SFRN28930000, Catov).
CRediT authorship contribution statement
Stephanie M. Spehar: Conceptualization, Methodology, Formal analysis, Data curation, Writing - original draft, Writing - review & editing, Visualization. Bethany Barone Gibbs: Conceptualization, Methodology, Validation, Writing - review & editing. Matthew Muldoon: Conceptualization, Validation, Supervision. Janet M. Catov: Conceptualization, Methodology, Formal analysis, Investigation, Resources, Writing - review & editing, Project administration, Funding acquisition.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2020.101219.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Abramson B.L., Melvin R.G. Cardiovascular risk in women: focus on hypertension. Can. J. Cardiol. 2014;30(5):553–559. doi: 10.1016/j.cjca.2014.02.014. [DOI] [PubMed] [Google Scholar]
- Ainsworth B.E., Leon A.S., Richardson M.T., Jacobs D.R., Paffenbarger R.S., Jr Accuracy of the college alumnus physical activity questionnaire. J. Clin. Epidemiol. 1993;46(12):1403–1411. doi: 10.1016/0895-4356(93)90140-v. [DOI] [PubMed] [Google Scholar]
- Ainsworth B.E., Haskell W.L., Herrmann S.D. Compendium of Physical Activities: a second update of codes and MET values. Med. Sci. Sports Exerc. 2011;43:1575–1581. doi: 10.1249/MSS.0b013e31821ece12. [DOI] [PubMed] [Google Scholar]
- Bakker, E.A., Sui, X., Brellenthin, A.G., Lee, D.C., 2018. Physical activity and fitness for the prevention of hypertension. Curr. Opin. Cardiol., 33 394–401. [DOI] [PubMed]
- Barone Gibbs B., Pettee Gabriel K., Carnethon M.R., Gary-Webb T., Jakicic J.M., Rana J.S., Reis J.P., Siddique J., Sternfeld B., Lewis C.E. Sedentary time, physical activity, and adiposity: cross-sectional and longitudinal associations in CARDIA. Am. J. Prev. Med. 2017;53(6):764–771. doi: 10.1016/j.amepre.2017.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barone Gibbs B., Kowalsky R.J., Perdomo S.J., Taormina J.M., Balzer J.R., Jakicic J.M. Effect of alternating standing and sitting on blood pressure and pulse wave velocity during a simulated workday in adults with overweight/obesity. J. Hypertens. 2017;35(12):2411–2418. doi: 10.1097/HJH.0000000000001463. [DOI] [PubMed] [Google Scholar]
- Barone Gibbs B., Aaby D., Siddique J., Reis J.P., Sternfeld B., Whitaker K., Pettee Gabriel K. Bidirectional 10-year associations of accelerometer-measured sedentary behavior and activity categories with weight among middle-aged adults. Int. J. Obes. 2020;44(3):559–567. doi: 10.1038/s41366-019-0443-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biswas A., Oh P.I., Faulkner G.E., Bajaj R.R., Silver M.A., Mitchell M.S., Alter D.A. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis. Ann. Intern. Med. 2015;162(2):123. doi: 10.7326/M14-1651. [DOI] [PubMed] [Google Scholar]
- Brocklebank L.A., Falconer C.L., Page A.S., Perry R., Cooper A.R. Accelerometer-measured sedentary time and cardiometabolic biomarkers: a systematic review. Prev. Med. 2015;76:92–102. doi: 10.1016/j.ypmed.2015.04.013. [DOI] [PubMed] [Google Scholar]
- Bull F.C., Maslin T.S., Armstrong T. Global physical activity questionnaire (GPAQ): nine country reliability and validity study. J. Phys. Act Health. 2009;6:790–804. doi: 10.1123/jpah.6.6.790. [DOI] [PubMed] [Google Scholar]
- Catov J.M., Peng Y., Scifres C.M., Parks W.T. Placental pathology measures: Can they be rapidly and reliably integrated into large-scale perinatal studies? Placenta. 2015;36(6):687–692. doi: 10.1016/j.placenta.2015.03.001. [DOI] [PubMed] [Google Scholar]
- Chastin S.F.M., Dontje M.L., Skelton D.A., Čukić I., Shaw R.J., Gill J.M.R., Greig C.A., Gale C.R., Deary I.J., Der G., Dall P.M. Systematic comparative validation of self-report measures of sedentary time against an objective measure of postural sitting (activPAL) Int. J. Behav. Nutr. Phys. Act. 2018;15(1) doi: 10.1186/s12966-018-0652-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng S., Claggett B., Correia A.W., Shah A.M., Gupta D.K., Skali H., Ni H., Rosamond W.D., Heiss G., Folsom A.R., Coresh J., Solomon S.D. Temporal trends in the population attributable risk for cardiovascular disease: the atherosclerosis risk in communities study. Circulation. 2014;130(10):820–828. doi: 10.1161/CIRCULATIONAHA.113.008506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chomistek A.K., Manson J.E., Stefanick M.L., Lu B., Sands-Lincoln M., Going S.B., Garcia L., Allison M.A., Sims S.T., LaMonte M.J., Johnson K.C., Eaton C.B. Relationship of sedentary behavior and physical activity to incident cardiovascular disease. J. Am. Coll. Cardiol. 2013;61(23):2346–2354. doi: 10.1016/j.jacc.2013.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dempsey P.C., Sacre J.W., Larsen R.N., Straznicky N.E., Sethi P., Cohen N.D., Cerin E., Lambert G.W., Owen N., Kingwell B.A., Dunstan D.W. Interrupting prolonged sitting with brief bouts of light walking or simple resistance activities reduces resting blood pressure and plasma noradrenaline in type 2 diabetes. J. Hypertens. 2016;34(12):2376–2382. doi: 10.1097/HJH.0000000000001101. [DOI] [PubMed] [Google Scholar]
- Dempsey P.C., Owen N., Yates T.E., Kingwell B.A., Dunstan D.W. Sitting less and moving more: improved glycaemic control for type 2 diabetes prevention and management. Curr. Diab. Rep. 2016;16(11) doi: 10.1007/s11892-016-0797-4. [DOI] [PubMed] [Google Scholar]
- Dempsey P.C., Larsen R.N., Dunstan D.W., Owen N., Kingwell B.A. Sitting less and moving more: implications for hypertension. Hypertension. 2018;72(5):1037–1046. doi: 10.1161/HYPERTENSIONAHA.118.11190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ekelund U., Brown W.J., Steene-Johannessen J., Fagerland M.W., Owen N., Powell K.E., Bauman A.E., Lee I.-M. Do the associations of sedentary behaviour with cardiovascular disease mortality and cancer mortality differ by physical activity level? a systematic review and harmonised meta-analysis of data from 850 060 participants. Br. J. Sports Med. 2019;53(14):886–894. doi: 10.1136/bjsports-2017-098963. [DOI] [PubMed] [Google Scholar]
- Figueiro, T.H., Arins, G.C.B., Santos, C., et al. Association of objectively measured sedentary behavior and physical activity with cardiometabolic risk markers in older adults. PLoS One 2019; 14:e0210861. [DOI] [PMC free article] [PubMed]
- Frohlich E.D. Clinical management of the obese hypertensive patient: Cardiol. Rev. 2002;10(3):127–138. doi: 10.1097/00045415-200205000-00001. [DOI] [PubMed] [Google Scholar]
- Hall J.E. Pathophysiology of obesity hypertension. Curr. Sci. Inc. 2000;2(2):139–147. doi: 10.1007/s11906-000-0073-4. [DOI] [PubMed] [Google Scholar]
- Hall J.E., Crook E.D., Jones D.W., Wofford M.R., Dubbert P.M. Mechanisms of obesity-associated cardiovascular and renal disease. Am. J. Med. Sci. 2002;324(3):127–137. doi: 10.1097/00000441-200209000-00003. [DOI] [PubMed] [Google Scholar]
- Hallal P.C., Andersen L.B., Bull F.C., Guthold R., Haskell W., Ekelund U. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet. 2012;380(9838):247–257. doi: 10.1016/S0140-6736(12)60646-1. [DOI] [PubMed] [Google Scholar]
- Healy G.N., Clark B.K., Winkler E.A.H., Gardiner P.A., Brown W.J., Matthews C.E. Measurement of adults' sedentary time in population-based studies. Am. J. Prev. Med. 2011;41(2):216–227. doi: 10.1016/j.amepre.2011.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Healy G.N., Winkler E.A.H., Owen N., Anuradha S., Dunstan D.W. Replacing sitting time with standing or stepping: associations with cardio-metabolic risk biomarkers. Eur. Heart J. 2015;36(39):2643–2649. doi: 10.1093/eurheartj/ehv308. [DOI] [PubMed] [Google Scholar]
- Ji H., Kim A., Ebinger J.E., Niiranen T.J., Claggett B.L., Bairey Merz C.N., Cheng S. Sex Differences in blood pressure trajectories over the life course. JAMA Cardiol. 2020;5(3):19. doi: 10.1001/jamacardio.2019.5306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katzmarzyk P.T. Physical activity, sedentary behavior, and health: paradigm paralysis or paradigm shift? Diabetes. 2010;59(11):2717–2725. doi: 10.2337/db10-0822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katzmarzyk P.T., Powell K.E., Jakicic J.M. Sedentary behavior and health: update from the 2018 physical activity guidelines advisory committee. Med. Sci. Sports Exerc. 2019;51(6):1227–1241. doi: 10.1249/MSS.0000000000001935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laporte R.E., Black-sandler R., Cauley J.A., Link M., Bayles C., Marks B. The assessment of physical activity in older women: analysis of the interrelationship and reliability of activity monitoring, activity surveys, and caloric intake. J. Gerontol. 1983;38(4):394–397. doi: 10.1093/geronj/38.4.394. [DOI] [PubMed] [Google Scholar]
- Larsen R.N., Kingwell B.A., Sethi P., Cerin E., Owen N., Dunstan D.W. Breaking up prolonged sitting reduces resting blood pressure in overweight/obese adults. Nutrit., Metab. Cardiovasc. Dis. 2014;24(9):976–982. doi: 10.1016/j.numecd.2014.04.011. [DOI] [PubMed] [Google Scholar]
- Law M.R.M.J.K., Wald N.J. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338:1665. doi: 10.1136/bmj.b1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee I.-M., Shiroma E.J. Using accelerometers to measure physical activity in large-scale epidemiological studies: issues and challenges. Br. J. Sports Med. 2014;48(3):197–201. doi: 10.1136/bjsports-2013-093154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee P.H., Wong F.K.Y. The association between time spent in sedentary behaviors and blood pressure: a systematic review and meta-analysis. Sports Med. 2015;45(6):867–880. doi: 10.1007/s40279-015-0322-y. [DOI] [PubMed] [Google Scholar]
- Loria C.M., Liu K., Lewis C.E., Hulley S.B., Sidney S., Schreiner P.J., Williams O.D., Bild D.E., Detrano R. Early adult risk factor levels and subsequent coronary artery calcification. J. Am. Coll. Cardiol. 2007;49(20):2013–2020. doi: 10.1016/j.jacc.2007.03.009. [DOI] [PubMed] [Google Scholar]
- Patel S.A., Mehta N.K., Ali M.K. Cardiovascular mortality associated with 5 leading risk factors. Ann. Intern. Med. 2016;164(7):510. doi: 10.7326/L15-0568. [DOI] [PubMed] [Google Scholar]
- Pedisic Z., Grunseit A., Ding D., Chau J.Y., Banks E., Stamatakis E., Jalaludin B.B., Bauman A.E. High sitting time or obesity: which came first? bidirectional association in a longitudinal study of 31,787 Australian adults: prolonged sitting time and obesity. Obesity. 2014;22(10):2126–2130. doi: 10.1002/oby.20817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poulter N.R., Prabhakaran D., Caulfield M. Hypertension. Lancet. 2015;386(9995):801–812. doi: 10.1016/S0140-6736(14)61468-9. [DOI] [PubMed] [Google Scholar]
- Qi Q., Strizich G., Merchant G., Sotres-Alvarez D., Buelna C., Castañeda S.F., Gallo L.C., Cai J., Gellman M.D., Isasi C.R., Moncrieft A.E., Sanchez-Johnsen L., Schneiderman N., Kaplan R.C. Objectively measured sedentary time and cardiometabolic biomarkers in us hispanic/latino adults: the hispanic community health study/study of latinos (HCHS/SOL) Circulation. 2015;132(16):1560–1569. doi: 10.1161/CIRCULATIONAHA.115.016938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song M., Nam S., Buss J., Lee S.-J. Assessing the prevalence of meeting physical activity recommendations among U.S. healthcare workers: data from the 2015 National Health Interview Survey. Arch. Environ. Occup. Health. 2020;75(7):422–430. doi: 10.1080/19338244.2020.1743960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorp A.A., Owen N., Neuhaus M., Dunstan D.W. Sedentary behaviors and subsequent health outcomes in adults. Am. J. Prev. Med. 2011;41(2):207–215. doi: 10.1016/j.amepre.2011.05.004. [DOI] [PubMed] [Google Scholar]
- Tremblay M.S., Aubert S., Barnes J.D., Saunders T.J., Carson V., Latimer-Cheung A.E., Chastin S.F.M., Altenburg T.M., Chinapaw M.J.M. Sedentary Behavior Research Network (SBRN) – terminology consensus project process and outcome. Int. J. Behav. Nutr. Phys. Act. 2017;14(1) doi: 10.1186/s12966-017-0525-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker P., Gilliland J. The effect of season and weather on physical activity: a systematic review. Public Health. 2007;121(12):909–922. doi: 10.1016/j.puhe.2007.04.009. [DOI] [PubMed] [Google Scholar]
- United States. Department of Health and Human Services . U.S. Dept. of Health and Human Services; Washington, DC: 2008. Physical Activity Guidelines for Americans: Be Active, Healthy, and Happy! [Google Scholar]
- Whelton P.K., Carey R.M., Aronow W.S. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2018;71:2199–2269. [Google Scholar]
- Whitaker K.M., Pettee Gabriel K., Buman M.P. Associations of accelerometer-measured sedentary time and physical activity with prospectively assessed cardiometabolic risk factors: the CARDIA study. J. Am. Heart Assoc. 2019;8 doi: 10.1161/JAHA.118.010212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright J.T., Jr., Whelton P.K., Reboussin D.M. A randomized trial of intensive versus standard blood-pressure control. N. Engl. J. Med. 2016;374:2294. doi: 10.1056/NEJMc1602668. [DOI] [PubMed] [Google Scholar]
- Zeigler Z.S., Mullane S.L., Crespo N.C., Buman M.P., Gaesser G.A. Effects of standing and light-intensity activity on ambulatory blood pressure. Med. Sci. Sports Exerc. 2016;48:175–181. doi: 10.1249/MSS.0000000000000754. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.