Abstract
Objective
This study was performed to summarize our experience and investigate the safety and efficacy of laparoscopic modified loop cholecystojejunostomy for the treatment of malignant obstructive jaundice.
Methods
Thirteen patients with malignant obstructive jaundice who underwent laparoscopic modified loop cholecystojejunostomy from March 2015 to March 2016 were retrospectively reviewed. The patients’ characteristics, operation time, postoperative intestinal recovery time, length of hospital stay, postoperative bilirubin level, and complications were analyzed.
Results
The patients were followed up as outpatients for 2 years. Nine patients with pancreatic head carcinoma, one patient with periampullary carcinoma, and three patients with distal bile duct carcinoma successfully underwent laparoscopic modified loop cholecystojejunostomy. The mean operation time was 176 ± 45 minutes, and the mean length of hospital stay was 9.5 ± 2.8 days. The serum total bilirubin concentration and gamma-glutamyl transferase concentration significantly decreased on postoperative day 7. The median follow-up time was 7 months. No patients developed bile leakage or required a reoperation.
Conclusions
Laparoscopic modified loop cholecystojejunostomy is not only safe and minimally invasive, but it is also feasible for patients with malignant obstructive jaundice.
Keywords: Obstructive jaundice, laparoscope, cholecystojejunostomy, carcinoma, bilirubin, minimally invasive
Introduction
Malignant obstructive jaundice is characterized by obstruction or compression of the bile duct that causes yellowish pigmentation of the skin, mucosa, and sclera. It is commonly associated with diseases such as pancreatic cancer, cholangiocarcinoma, periampullary carcinoma, or malignant hilar metastasis. Unfortunately, most patients are diagnosed too late to undergo surgical resection. In such cases, choledochojejunostomy or percutaneous transhepatic cholangial drainage is often performed as a palliative treatment.
Laparoscopy is widely used in surgical operations because of its minimal invasiveness and facilitation of rapid patient recovery. In recent years, laparoscopic techniques have greatly progressed in minimally invasive hepatobiliary and pancreatic surgery. Several studies have shown that laparoscopic cholecystectomy, liver resection, splenectomy, and even pancreaticoduodenectomy are safe and feasible with obvious advantages over the open approach.1–4 We modified the traditional surgical technique of laparoscopic choledochojejunostomy into cholecystojejunostomy and herein summarize our experience with this technique for the treatment of malignant obstructive jaundice.
Methods
Patient data
Patients with malignant obstructive jaundice who were treated by laparoscopic modified cholecystojejunostomy in our hospital from March 2015 to March 2016 were retrospectively reviewed. Preoperative computed tomography, magnetic resonance cholangiopancreatography, and liver function examination confirmed the presence of malignant obstructive jaundice with no indication for radical surgical resection in these patients (Table 1).
Table 1.
Characteristics of 13 patients who underwent laparoscopic modified loop cholecystojejunostomy.
| Patient No. | Sex | Age (years) | Diagnosis | OT (minutes) | PIRT (days) | LOS (days) | Complications | Survival state | Follow-up (months) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 70 | CHP | 135 | 4 | 7 | None | Alive | 10 |
| 2 | M | 65 | CHP | 105 | 4 | 7 | None | Alive | 13 |
| 3 | M | 77 | CHP | 185 | 3 | 5 | Gastroparesis | Dead | 1 |
| 4 | F | 63 | CHP | 235 | 4 | 7 | None | Alive | 7 |
| 5 | M | 61 | CHP | 185 | 3 | 7 | None | Alive | 8 |
| 6 | F | 74 | CHP | 140 | 3 | 7 | None | Alive | 3 |
| 7 | F | 72 | DC | 235 | 6 | 12 | None | Alive | 5 |
| 8 | F | 63 | CHP | 210 | 3 | 12 | Pulmonary infection | Alive | 9 |
| 9 | F | 72 | CHP | 120 | 4 | 12 | None | Alive | 4 |
| 10 | M | 84 | DC | 160 | 6 | 12 | None | Alive | 18 |
| 11 | F | 68 | CHP | 190 | 6 | 12 | None | Alive | 6 |
| 12 | F | 65 | VC | 235 | 6 | 12 | None | Alive | 7 |
| 13 | M | 59 | DC | 150 | 7 | 12 | None | Alive | 24 |
M, male; F, female; CHP, carcinoma of head of pancreas; DC, distal cholangiocarcinoma; VC, Vater carcinoma; OT, operation time; PIRT, postoperative intestinal recovery time; LOS, length of hospital stay.
Surgical procedure
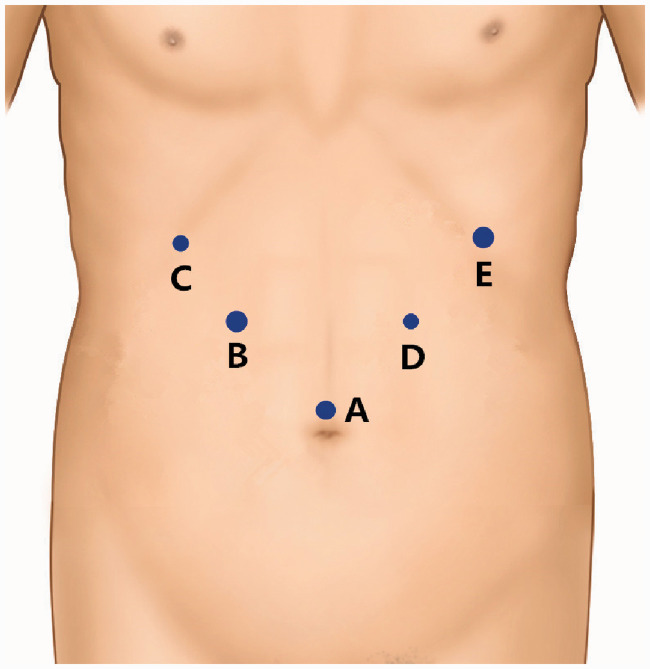
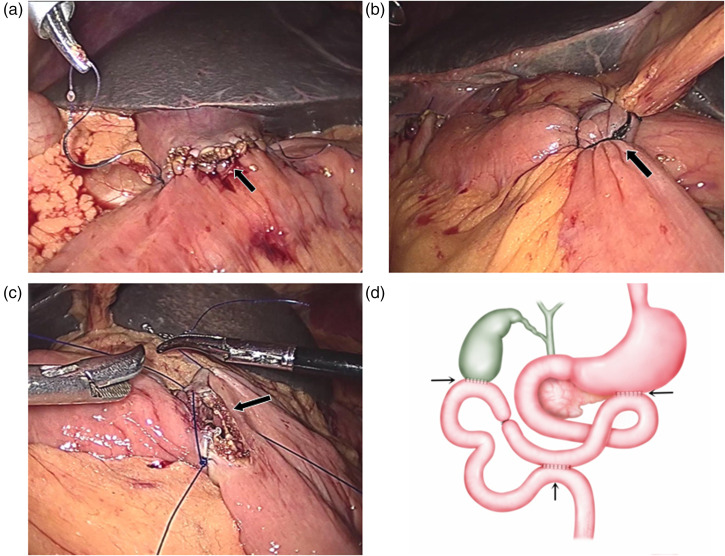
All operations were performed with the patients under general anesthesia and placed in the reverse Trendelenburg position. Pneumoperitoneum was established and maintained at 12 to 14 mmHg. The trocar positions are shown in Figure 1. To create a bypass for the management of biliary tract obstruction, side-to-side antecolonic cholecystojejunostomy was performed 25 cm from the ligament of Treitz using 3/0 absorbable Vicryl sutures (Ethicon, Somerville, NJ, USA). Next, side-to-side Braun enteroenterostomy was performed 55 cm from the cholecystojejunostomy and 15 cm from the ligament of Treitz. The afferent loop of the cholecystojejunostomy was double-tied and closed in the middle using 1/0 silk thread. Gastroenterotomy was performed under the condition of intestinal obstruction or potential intestinal obstruction (Figure 2).
Figure 1.
Port positions for laparoscopic cholecystojejunostomy. A: 10-mm trocar. B, E: 12-mm trocars. C, D: 5-mm trocars.
Figure 2.
Laparoscopic modified loop cholecystojejunostomy. (a) Intraoperative cholecystojejunostomy (black arrow). (b) Double tie and closing of the afferent loop of the cholecystojejunostomy (black arrow). (c) Side-to-side Braun enteroenterostomy (black arrow). (d) Schematic diagram of surgery. →: cholecystojejunostomy, ←: gastroenterotomy, ↑: Braun enteroenterostomy.
Data collection and follow-up
Data regarding the operation time; postoperative intestinal recovery time; length of hospital stay; 1-, 3-, 5-, and 7-day postoperative bilirubin level; and complications were collected. The patients were followed up as outpatients every 2 months. The survival time and occurrence of postoperative jaundice, gastrointestinal obstruction, and bile leakage were monitored for 2 years.
Statistical analysis
Data including the total bilirubin, concentration, gamma-glutamyl transferase concentration, and postoperative day are presented as mean ± standard deviation. SPSS 19.0 (IBM Corp., Armonk, NY, USA) was used for the statistical analysis.
Ethics
This study was approved by the ethics committee of West China Hospital, Sichuan University. The patients provided written informed consent.
Results
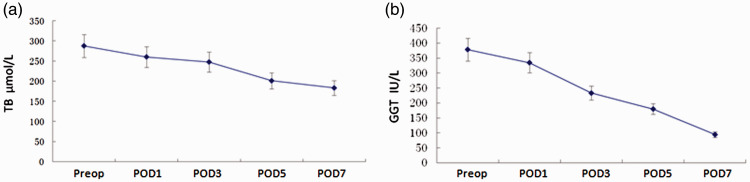
Thirteen patients successfully underwent laparoscopic modified loop cholecystojejunostomy. The patients comprised five men and eight women ranging in age from 59 to 84 years (median age, 68 years). Nine patients had carcinoma of the head of the pancreas, one had periampullary carcinoma, and three had distal cholangiocarcinoma. The mean operation time was 176 ± 45 minutes, postoperative intestinal recovery time was 4.5 ± 1.5 days, and length of hospital stay was 9.5 ± 2.8 days. The serum total bilirubin concentration decreased to a mean of 87 ± 32 µmol/L and the gamma-glutamyl transferase concentration decreased to a mean of 248 ± 54 U/L on postoperative day 7 (Figure 3). One patient developed gastroparesis and one developed a pulmonary infection; both patients recovered after conservative treatment and antibiotics. None of the 13 patients died during the perioperative period. One patient died of tumor progression during follow-up. The median follow-up time was 7 months (range, 1–24 months). No patients developed bile leakage or required a reoperation (Table 1).
Figure 3.
Changes in liver function before and after surgery. (a) Changes in TB within 7 days after surgery. (b) Changes in GGT within 7 days after surgery. TB, total bilirubin; GGT, gamma-glutamyltransferase; POD, postoperative day; Preop, preoperative.
Discussion
Patients with malignant obstructive jaundice have a low surgical resection rate, poor prognosis, and high mortality. Patients who cannot undergo radical resection are usually treated by palliative shunt surgery such as internal or external drainage. Percutaneous transhepatic cholangial drainage and endoscopic nasobiliary drainage are two external drainage techniques that enable the obstructed bile to drain out of the body instead of the intestinal tract. This decreases hyperbilirubinemia and prolongs the survival time, but it is also associated with adverse effects such as indigestion, electrolyte disorders, drainage tube fallout, drainage tube obstruction, and biliary tract infection.5–7 Therefore, external drainage is indicated to prepare for radical resection by reducing jaundice; it is also indicated in patients with multiple organ failure.
Internal drainage techniques include stent implantation and biliojejunostomy, which allow the bile to flow into the intestine and thus improve the quality of life of patients with advanced-stage disease. Stent implantation is performed through endoscopic retrograde cholangiopancreatography (ERCP) or the percutaneous transhepatic approach. ERCP is suitable for lower biliary obstruction such as that caused by pancreatic head cancer, ampullary carcinoma, or cholangiocarcinoma; however, the percutaneous transhepatic approach is available for patients with upper bile duct obstruction that cannot be treated by surgery, especially patients with poor ERCP drainage and unsatisfactory outcomes. These two approaches are prone to stent blockage, stent displacement, postoperative cholangitis, biliary infection, and other complications.5,8,9
Biliojejunostomy is the main surgical shunt technique and is widely used for patients with malignant obstructive jaundice. Traditional Roux-en-Y anastomosis requires surgical resection of the gallbladder and common bile duct with bile duct end-to-side anastomosis followed by side-to-side enteroenterostomy. The main complications are anastomotic stenosis, reflux cholangitis, and biliary leakage. Compared with Roux-en-Y anastomosis, modified loop cholecystojejunostomy is safe, simple, and easy to perform without gallbladder resection or jejunal transection, especially when using a laparoscopic technique. Previous studies have shown that the operation time, postoperative intestinal recovery time, and length of hospital stay were significantly shorter with modified loop cholecystojejunostomy than Roux-en-Y anastomosis.10–15
Ordog et al.16 found that the pacemaker of the jejunum is located in the duodenal bulb. Their research revealed that the integrity of electrical conduction is essential in the small intestine and that discontinuity of the electrical conduction by jejunal transection is likely to cause jejunal motility disorders and thus increase the chance of reflux cholangitis.16 Compared with classic Roux-en-Y anastomosis, loop anastomosis preserves the continuity of the intestinal electrical conduction without interruption of the jejunum and mesenteric vessels, leaving the intestinal motility unaffected. Thus, the postoperative intestinal function recovery time is shortened, the quality of life is improved, and the occurrence rate of reflux cholangitis is low.17 Patients with pancreatic head cancer and papillary cancer usually develop duodenal obstruction due to tumor compression or occupancy, and gastrointestinal anastomosis is therefore routinely performed in these patients. The anastomotic site of cholecystojejunostomy is located at the bottom of the gallbladder, and patients with high bile duct obstruction are not suitable for this procedure. Modified loop cholecystojejunostomy is a palliative treatment for patients with low bile duct obstruction; however, its long-term survival rate and clinical effects require further follow-up.
In conclusion, modified loop cholecystojejunostomy is safe and simple to perform and effectively palliates jaundice in patients with malignant low bile duct obstruction.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
The research was funded by the Scientific Research Starting Foundation for Youths of Sichuan University (2015SCU11999-9), the Chinese Foundation for Hepatitis Prevention and Control-TianQing Liver Disease Research Fund Subject (TQGB20170067), and the Science and Technology Support Program of Sichuan Province (2017KZ0019).
References
- 1.Alkhalili E, Berber E. Laparoscopic liver resection for malignancy: a review of the literature. World J Gastroenterol 2014; 20: 13599–13606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goh JC, Tan JK, Lim JW, et al. Laparoscopic cholecystectomy for acute cholecystitis: an analysis of early versus delayed cholecystectomy and predictive factors for conversion. Minerva Chir 2017; 72: 455–463. [DOI] [PubMed] [Google Scholar]
- 3.Borie F. Laparoscopic partial splenectomy: surgical technique. J Visc Surg 2016; 153: 371–376. [DOI] [PubMed] [Google Scholar]
- 4.Matsuda M, Haruta S, Shinohara H, et al. Pancreaticogastrostomy in pure laparoscopic pancreaticoduodenectomy–A novel pancreatic-gastric anastomosis technique. BMC Surg 2015; 15: 80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chandrashekhara SH, Gamanagatti S, Singh A, et al. Current status of percutaneous transhepatic biliary drainage in palliation of malignant obstructive jaundice: a review. Indian J Palliat Care 2016; 22: 378–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bin OY, Zeng KW, Hua HW, et al. Endoscopic nasobiliary drainage and percutaneous transhepatic biliary drainage for the treatment of acute obstructive suppurative cholangitis: a retrospective study of 37 cases. Hepatogastroenterology 2012; 59: 2454–2456. [DOI] [PubMed] [Google Scholar]
- 7.Fujisawa T, Kagawa K, Watanabe S, et al. Endoscopic nasobiliary drainage for obstructive jaundice using either a 5 Fr or 7 Fr catheter: a prospective, randomized trial. BMC Gastroenterol 2014; 14: 161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Popat B, Thakkar D, Deshmukh H, et al. Percutaneous transhepatic biliary drainage in the management of post-surgical biliary leaks. Indian J Surg 2017; 79: 24–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shao JH, Fang HX, Li GW, et al. Percutaneous transhepatic biliary drainage and stenting for malignant obstructive jaundice: a report of two cases. Exp Ther Med 2015; 10: 1503–1506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li Z, Cui N, Chen L. Treatment experience of subsequent complications after Roux-en-Y biliojejunostomy. Eur Surg Res 2009; 43: 34–38. [DOI] [PubMed] [Google Scholar]
- 11.Cook FJ, Khanna I, Giordano J, et al. Long term bone health after Roux-en-Y gastric bypass: a pilot study. Endocr Pract 2017; 3: 1077–1084. [DOI] [PubMed] [Google Scholar]
- 12.Mahawar KK, Sharples AJ. Contribution of malabsorption to weight loss after Roux-en-Y gastric bypass: a systematic review. Obes Surg 2017; 27: 2194–2206. [DOI] [PubMed] [Google Scholar]
- 13.Vella E, Hovorka Z, Yarbrough DE, et al. Bile reflux of the remnant stomach following Roux-en-Y gastric bypass: an etiology of chronic abdominal pain treated with remnant gastrectomy. Surg Obes Relat Dis 2017; 13: 1278–1283. [DOI] [PubMed] [Google Scholar]
- 14.Safioleas MC, Moulakakis KG, Safioleas CM, et al. Stapled cholecystojejunostomy for palliative treatment of the malignant jaundice; an effective and feasible alternative to hand-sewn method. Int J Surg 2010; 8: 423–425. [DOI] [PubMed] [Google Scholar]
- 15.Zheng Q, Chen Y. The effects of cholecystojejunostomy and biliary drainage on biliary motor. J Huazhong Univ Sci Technolog Med Sci 2002; 22: 144–147. [DOI] [PubMed] [Google Scholar]
- 16.Ordog T, Ward SM, Sanders KM. Interstitial cells of Cajal generate electrical slow waves in the murine stomach. J Physiol 1999; 518: 257–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schob O, Schlumpf R, Kunz M, et al. Technique of laparoscopic cholecystojejunostomy with a Roux-en-Y loop. Surg Laparosc Endosc 1993; 3: 386–390. [PubMed] [Google Scholar]