Abstract
Objectives
To evaluate age-based differences in prescription opioid misuse (POM) motives and to evaluate substance use and mental and physical health correlates of POM motive categories in older adults.
Design
Data were from the National Survey on Drug Use and Health (NSDUH), a nationally representative US survey.
Setting
The NSDUH is a household survey.
Subjects
A total of 5,826 US residents with past-year POM; 415 were 50 years and older (7.1%).
Methods
Nine POM motives were assessed among those engaged in past-year POM, grouped into three categories: solely physical pain relief, solely non–pain relief, or mixed motives. Prevalence of POM motives were calculated by age group, with logistic models examining age-based differences. Finally, odds of substance use and mental and physical health correlates by motive category were calculated via logistic models in older adults.
Results
POM motivated solely by physical pain relief increased from 35.1% in young adults to 65.4% in older adults; in older adults, 84.7% of POM episodes involved pain relief as a motive. POM for solely non–pain relief or mixed motives was associated with greater odds, vs pain relief only, of past-year benzodiazepine misuse (odds ratio [OR] = 4.43 and 6.15, respectively), any substance use disorder (OR = 5.57 and 5.60, respectively), and suicidal ideation (OR = 4.05 and 3.56, respectively) in older adults.
Conclusions
. POM motives change over the lifespan, with increasing POM for pain relief with aging. Comprehensive nonopioid pain management is needed for those engaged in POM for pain relief, and substance use and mental health treatment are needed for those with non–pain relief motives.
Keywords: Opioid, Prescription Misuse, Motives, Epidemiology
Introduction
In 2016 and 2017, prescription opioid misuse (POM) accounted for >17,000 US overdose deaths [1], resulting in the initiation of significant public health efforts aimed at reducing POM and its consequences. POM is often defined as opioid use without a prescription or use of one’s own prescribed opioid medication in ways not intended by the prescribing clinician [2], which is the definition used in the present study. Consideration of the underlying motives for POM can determine the choice of appropriate interventions. For example, nonopioid pain management approaches may be needed for those motivated to relieve pain, whereas substance use treatment may be warranted for individuals engaged in POM for recreational purposes.
The majority of POM motive research has examined locally derived samples and younger age groups (i.e., adolescents), resulting in a gap in our knowledge of POM motives in adults. One exception is a study by Han et al. [3], in which POM motives were examined across the lifespan using nationally representative data from the 2015 US National Survey on Drug Use and Health (NSDUH). In this study, pain relief was the most common primary motive for POM, and those with recreational substance-related motives (e.g., get high) had the most concerning substance use profiles [3]. To date, we remain unaware of studies focused on older adults, a population particularly vulnerable to POM consequences [4].
Despite evidence of age-related differences in opioid sources for POM, with greater use of physician sources as individuals age [5], motive differences by age group remain unexplored. Risks, such as concurrent substance use and presence of psychopathology, associated with specific POM motives also remain unexplored in older adults. Evidence from across the population suggests that substance use and mental health correlates differ by POM motive [3], and evidence from older adults indicates that older adults who purchase opioid medication from others or use multiple opioid sources have higher odds of concurrent other substance use and poorer mental health [5]. Although older adults have lower POM rates compared with younger adults, POM rates in older adults have significantly increased over the past 15 years [6]. Furthermore, older adults may be particularly vulnerable to opioid-related adverse effects, given drug interactions and comorbidities that may change opioid metabolism and bioavailability [4].
Our primary aim was to evaluate the age-related prevalence of both individual POM motives and motive categories (i.e., pain relief only, non–pain relief only, and mixed motives) using 2015–2016 NSDUH data. As a secondary aim, we evaluated the odds of substance use and mental and physical health correlates by motive category in US adults aged 50 years and older. Together, results from these analyses can provide information about potential treatments to address POM (e.g., comprehensive pain management in those motivated to relieve pain) and identify concurrent behaviors in need of further treatment (e.g., behavioral health and/or substance use treatment in those with recreational motives), reduce POM prevalence, and improve outcomes in those with preexisting POM.
Methods
The NSDUH, an annual US survey of those aged 12 years and older, uses an independent, multistage area probability sampling design that allows for nationally representative estimates. More information on the NSDUH is available elsewhere [7]. For the 2015–2016 NSDUH, 5,826 respondents (representing 11,612,302 US residents) with past-year POM had complete data on motives; these respondents represent 96.6% of the available sample with past-year POM (N = 6,033) and are the sample of focus for this study. Of these, 415 were adults aged 50 years and older (representing 2,614,688 US older adult residents). The 2015–2016 weighted screening response rate was 81.94%, and the weighted interview response rate was 71.20%. The NSDUH was approved by the Research Triangle International IRB [7], and the Texas State University IRB exempted this work from further human subjects oversight.
Survey respondents selected from nine potential POM motives, choosing as many as applied. POM motives included the following: to relieve physical pain, to relax, to experiment, to get high, to sleep, to help with emotions, to alter other drug effects, because I am “hooked,” and for other reasons. We then categorized participants according to POM motive, per past research [8]: pain relief motives only, non–pain relief motives only, or mixed motives (i.e., both pain and non–pain relief motives).
Sociodemographic variables included sex, race/ethnicity, age group, household income, and population density. Substance use correlates were the following: past-month binge alcohol use, past-year marijuana use, past-year benzodiazepine misuse, past-year nonmarijuana illicit drug use, past-year any Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV) substance use disorder (SUD), and past-year SUD treatment. Mental health correlates were as follows: past-year DSM-IV major depression, past-year mental health treatment, and past-year suicidality. Past-year physical health correlates included past-year emergency department use, past-year hospitalization, and self-reported poor/fair health.
Analyses utilized STATA 15.1 (College Station, TX, USA) and incorporated the complex survey design; adjusted person-level weights (weight/two) created unbiased population-based estimates. Weighting procedures were used to create unbiased estimates of the behaviors measured in the NSDUH that are representative of the civilian, noninstitutionalized US population in the year of the survey, using US Census data to structure weighting (please see reference [9] for more information on the development of NSDUH person-level weights). Adjusted person-level weights were mandated by the aggregation of two years of data; therefore, division of the weight value by two was needed to provide accurate annualized estimates of the US population [10].
The Taylor series approximation, with adjusted degrees of freedom, created robust variance estimates. This approximation is a mathematical transformation to make nonlinear survey data linearized, and it is a common and valid technique for household surveys, like the NSDUH [11]. Weighted cross-tabulations estimated the prevalence and 95% confidence intervals of individual POM motives and motive categories by age group. Design-based (i.e., incorporating the complex survey features of the NSDUH) logistic models evaluated pairwise differences in motive prevalence by age group, whereas multinomial regressions evaluated age-based differences in motive category. Models were Bonferroni-corrected for multiple comparisons (0.05/10 comparisons for an a priori P value of 0.005).
Similar analyses evaluated differences in individual motives and motive categories by sex and race/ethnicity and were restricted to older adults (50 years and older). Next, differences in prevalence of any SUD symptoms from POM were estimated for the individual (nonexclusive) motives in older adults. Finally, design-based multivariable logistic regression analyses in older adults evaluated differences in the substance use and mental and physical health correlates by POM motive category. All logistic models controlled for sex, race/ethnicity, income, and population density (except for models examining sex- or race/ethnicity-based differences, where the list of control variables excluded sex or race/ethnicity, respectively).
Results
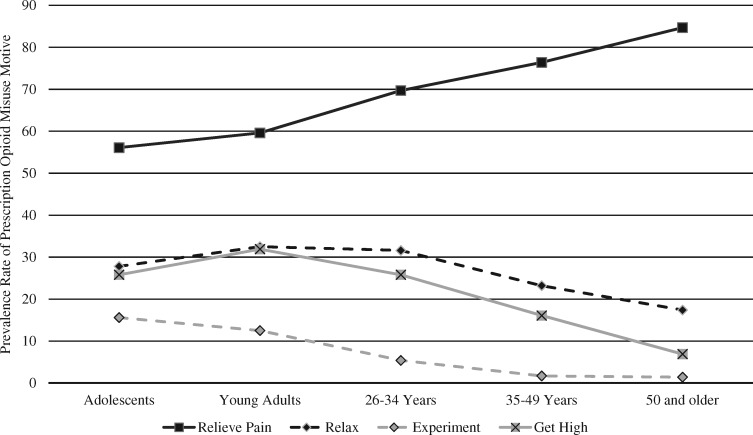
Per Table 1, the prevalence of pain relief as a motive increased over the lifespan, from 56.1% in adolescents aged 12–17 years to 84.7% in adults aged 50 years and older, with significant differences between each age group (except between adolescents and young adults [aged 18–25 years]). Conversely, the prevalence of the POM motive to experiment or help with emotions decreased across the lifespan. Finally, the POM motives to relax and to get high peaked in young adults (32.5% and 31.9%, respectively) and decreased in older adults, who were lowest in prevalence (17.4% and 16.4%, respectively). The prevalence rates of these four POM motives (i.e., pain relief, to relax, to experiment, and to get high) are also captured graphically in Figure 1.
Table 1.
Prescription opioid misuse motive prevalence by age group (N = 5,826)
| Motives* | Adolescents (12–17 y; A) | Young Adults (18–25 y; B) | 26–34 y (C) | 35–49 y (D) | ≥50 y (E) | Pairwise Comparisons‡ |
|---|---|---|---|---|---|---|
| Sample size | (N = 977) | (N = 2,156) | (N = 1,229) | (N = 1,049) | (N = 415) | |
| % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | |||
| To relieve pain | 56.1 (51.9–60.3) | 59.6 (56.6–62.5) | 69.7 (66.6–72.7) | 76.4 (73.5–79.0) | 84.7 (79.1–89.0) | A, B < C < D < E |
| To relax | 27.8 (24.1–31.7) | 32.5 (29.7–35.4) | 31.6 (28.5–34.9) | 23.2 (20.4–26.3) | 17.4 (12.7–23.3) | D, E < A, B, C |
| To experiment | 15.6 (12.8–18.8) | 12.5 (10.7–14.4) | 5.4 (3.7–7.6) | 1.7 (0.9–3.0) | 1.4 (0.7–3.1) | D, E < C < B < A |
| To get high | 25.8 (22.5–29.4) | 31.9 (29.7–34.2) | 25.8 (22.5–29.4) | 16.1 (13.2–19.5) | 6.9 (4.7–10.2) | E < D < C < B;E, D < A |
| To sleep | 14.4 (12.0–17.2) | 17.4 (15.1–20.0) | 14.9 (12.1–18.1) | 12.6 (10.3–15.2) | 16.4 (12.5–21.2) | D < B |
| To help with emotions | 14.1 (11.3–17.4) | 14.1 (12.3–16.0) | 10.8 (9.1–12.7) | 8.7 (6.8–11.0) | 6.3 (4.1–9.7) | D, E < A, B;E < C;C < B |
| To alter other drug effects | 2.0 (1.2–3.3) | 3.7 (3.1–4.5) | 3.0 (1.9–4.5) | 1.5 (0.8–2.8) | 1.2 (0.5–2.9) | D, E < B |
| Because I am “hooked” | 0.9 (0.4–1.9) | 3.2 (2.3–4.4) | 5.6 (4.3–7.3) | 3.4 (2.3–5.0) | 1.5 (0.7–3.4) | A < B, C, D;B, D, E < C |
| Other reason | 5.2 (3.8–7.1) | 2.6 (1.8–3.7) | 2.2 (1.5–3.2) | 3.0 (2.0–4.4) | 1.3 (0.5–3.4) | B, C, D, E < A |
| Motive category† | ||||||
| Pain relief only | 38.4 (34.4–42.6) | 35.1 (32.2–38.2) | 43.6 (39.9–47.5) | 55.0 (51.3–58.7) | 65.4 (58.6–71.6) | Base outcome |
| Non–pain relief only | 43.9 (39.7–48.2) | 40.4 (37.5–43.4) | 30.3 (27.3–33.4) | 23.7 (21.0–26.6) | 15.3 (11.0–20.9) | E < D < C < A, B |
| Mixed motives | 17.7 (14.8–21.1) | 24.5 (21.9–27.3) | 26.1 (22.8–29.6) | 21.4 (18.3–24.8) | 19.3 (15.2–24.2) | D, E < B, C;E < A;A < B |
Source: 2015–16 NSDUH surveys.
CI = confidence interval; NSDUH = National Survey on Drug Use and Health; POM = prescription opioid misuse.
Individual opioid motives are not mutually exclusive (i.e., “select as many as apply”) and are from the last POM episode in those with past-year POM.
Motive category variables are mutually exclusive and are based on the individual opioid motives selected by respondents.
Pairwise comparisons are based on logistic or multinomial logistic models that control for sex, race/ethnicity, household income, and population density of residence; significant listed differences are Bonferroni-corrected for 10 comparisons (P ≤ 0.005).
Figure 1.
Prevalence rates of opioid misuse motives by age group (N = 5,826). Source: 2015–2016 National Survey on Drug Use and Health surveys.
The POM motives to alter other drug effects, because I am “hooked,” and other reasons were uncommon (<6% each) across age groups. For motive categories, older adults (65.4%), adults aged 35–49 years (55.0%), and adults aged 26–34 years (43.6%) most commonly engaged in POM for pain relief only, whereas non–pain relief motives were most commonly in adolescents (43.9%) and young adults (40.4%). Mixed motives were least common (17.7% to 26.1%), peaking in adults aged 26–34 years.
No sex differences in nonexclusive individual motives or in motive category were found in older adults (data not shown). Only one older adult race/ethnicity-based difference was found: Caucasians were more likely to engage in POM to get high than were Hispanic/Latino respondents (9.1% vs 0.6%; also not shown). Analyses also examined the prevalence rate of any SUD symptoms from POM in those engaged in POM for a specific motive (i.e., to get high) vs those without that motive (i.e., for reasons other than to get high). These analyses found that older adults who engaged in POM to get high had a higher prevalence of any SUD symptoms from POM (58.1% vs 37.2% in those not engaged to get high). Similarly, older adults who engaged in POM because they were “hooked” (100% vs 37.9% in older adults engaged in POM for reasons other than because they were “hooked”) or for other reasons (91.4% vs 37.0% in older adult not engaged in POM for other reasons; data not shown in tables or figures) had a higher prevalence of any SUD symptoms from POM.
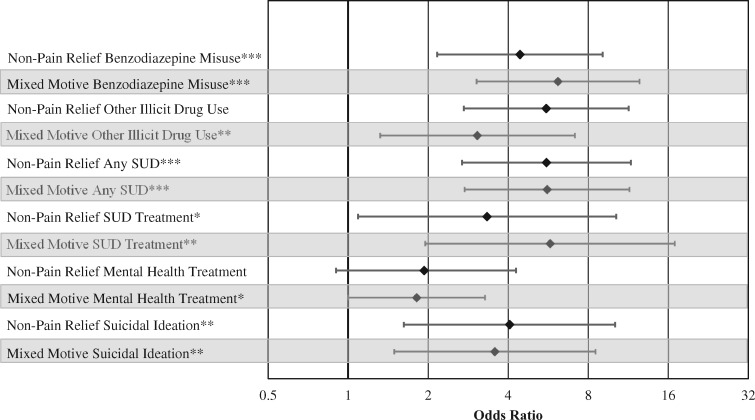
Finally, six significant elevations in past-year substance use and mental health correlate prevalence rates were found in older adults who reported non–pain relief only or mixed motives for use (vs the reference group of those with pain relief only motives) (Figure 2). Four correlates were related to substance use: benzodiazepine misuse (non–pain relief: odds ratio [OR] = 4.43, 95% confidence interval [CI] = 2.16–9.07; mixed motive OR = 6.15, 95% CI = 3.04–12.46), past-year nonmarijuana illicit drug use (non–pain relief: OR = 5.56, 95% CI = 2.72–11.35; mixed motives: OR = 3.06, 95% CI = 1.32–7.12), past-year any SUD (non–pain relief: OR = 5.57, 95% CI = 2.68–11.57; mixed motives: OR = 5.60, 95% CI = 2.74–11.42), and past-year any SUD treatment (non–pain relief: OR = 3.33, 95% CI = 1.09–10.20; mixed motive: OR = 5.75, 95% CI = 1.95–16.91).
Figure 2.
Substance use and psychopathology correlates by opioid misuse motive category in older adults (N = 415). Source: 2015–2016 National Survey on Drug Use and Health surveys. Comparisons are between the pain relief only group (reference; N = 267) and either the non–pain relief only group (unshaded; N = 63) or the mixed motive group (shaded; N = 85); the point captures the odds ratio, with 95% confidence intervals included as error bars. * = p < 0.05, ** = p < 0.01, *** p < 0.001. SUD = substance use disorder.
The two mental health–related correlates with higher prevalence rates in those with non–pain relief and/or mixed motives were past-year mental health treatment (mixed motive: OR = 1.81, 95% CI = 1.00–3.27) and past-year suicidal ideation (non–pain relief: OR = 4.05, 95% CI = 1.62–10.10; mixed motive: OR = 3.56, 95% CI = 1.49–8.51). POM for non–pain relief only did not demonstrate differences from pain relief only in terms of past-year mental health treatment odds (non–pain relief: OR = 1.93, 95% CI = 0.90–4.16). No differences in odds were found for the three physical health correlates: past-year major depression, past-month binge alcohol use, or past-year marijuana use by motive category (Supplementary Data).
Discussion
We found that physical pain relief was noted by most individuals engaged in POM, with rates increasing across the lifespan: from 56.1% in adolescents to 84.7% in older adults. Similar patterns were seen in POM engagement solely due to physical pain relief, though the lowest rates were in young adults (35.1%, vs 65.4% in older adults). Across US adults aged 18 years and older, the majority of individuals (63.4%) engaged in POM noted pain relief as the single most important motive, followed by to get high (11.6%) and to relax (10.9%); all other motives accounted for <10% of responses [3,12]. Our results largely support the adult-wide POM motive prevalence rates [3], with pain relief as the most frequently noted motive across all age groups, and to get high and to relax as the second and third most frequently noted motives in all age groups except for older adults. Among adults aged >50, to relax was the second and to sleep was the third most prevalent motive, respectively.
In older adults, those engaged in POM for solely non–pain relief motives had significantly higher rates of past-year benzodiazepine misuse, nonmarijuana illicit drug use, any SUD, and SUD treatment than did those engaged in POM solely for physical pain relief. Those with non–pain relief motives also had higher rates of suicidal ideation, and higher rates of mental health treatment were noted in those with mixed motives. Again, this corresponds to past research in US adolescents and adults that linked prescription opioid misuse for non–pain relief motives to higher rates of other substance use, substance use problems, and suicidal ideation [3,8,13]. Roughly one in 10 US older adults engaged in POM (regardless of motive) noted past-year suicidal ideation; one in four older adults who engaged in both POM and benzodiazepine misuse noted past-year suicidal ideation [14]. Furthermore, Mowbray and Quinn found high rates of past-year illicit substance use in those with POM, from 16.6% in older adults to 36.9% in young adults, compared with a range of 0.3% to 4.6% in those without POM [15].
Our findings suggest limited, if any, differences in substance use and mental health correlates between older adults whose POM is motivated by non–pain relief only motives vs those with mixed motives. Indeed, the only difference between these groups was in terms of past-year mental health treatment, where those with mixed motives had significantly higher odds of mental health treatment than those motivated by pain relief only; however, post hoc analyses indicated no differences in the odds of past-year mental health treatment between those with non–pain relief only and mixed motives. Thus, it appears that the presence of any non–pain relief motive is the key factor in increased odds of concurrent other substance use and mental health problems, a finding consistent with work in adolescents [8].
Our results are limited by self-report and self-selection biases. Causality cannot be inferred due to the cross-sectional nature of the NSDUH, but evidence suggests that self-report substance use data are reliable and valid [16,17]. The NSDUH methodology limits self-report bias via ACASI methods, medication pictures, and trade and generic medication name use [18]. Thus, although self-report bias is likely to have a limited impact on the findings of this study, a minority of those approached who refused participation may have impacted outcomes, though the NSDUH weighting procedures are intended to account for nonresponse. Weighting also creates estimates that are normed to the civilian, noninstitutionalized US population to limit self-selection bias, though these results cannot be generalized to military or institutionalized (e.g., imprisoned) populations. Also, the measure of past-year marijuana use used in this study assessed any marijuana use, whether legitimate medical use (as recognized by a state where such use is legal) or nonmedical and/or illicit use. Marijuana use overall [19] is increasing in older adults, and adults aged 50 years and older have the highest prevalence rates of medical marijuana use [20]. Further research should explore the relationships between opioid use, misuse, POM motives, and medical vs illicit vs mixed motive marijuana use, given that marijuana is commonly used by older adults to treat pain [21]. Finally, despite efforts to include older adults, the NSDUH undersamples individuals from this population who live in controlled-access dwellings [22].
Conclusions
POM motives vary significantly by age group, with increasing age associated with increasing POM solely for physical pain relief and decreasing POM solely for non–pain relief or mixed motives. Older adults with non–pain relief motives may require thorough medical and behavioral health assessment and potential SUD and mental health treatment, given their higher odds of concurrent substance use and psychopathology, as compared with older adults with pain relief motives only. In contrast, most older adults engaged in POM solely for physical pain relief and who have not developed substance-related problems may require comprehensive multimodality pain management interventions to adequately treat their pain and reduce POM risk. Such interventions may include nonpharmacological and nonopioid medication therapies [23,24]. Recent research suggests that buprenorphine and methadone are effective options for pain management in older adults, though both have limitations [25–27], including potential for misuse and diversion [28]. Buprenorphine formulations that include naloxone may reduce misuse liability [29], and both buprenorphine and methadone are firstline treatments for opioid use disorder [30]. Regardless of POM motive, a positive therapeutic relationship is crucial to facilitate disclosure of POM and associated motives.
In conclusion, different patterns of POM motives in older adults can inform clinicians and better target interventions, with comprehensive pain management approaches used in older adults engaged in POM solely for physical pain relief, and substance use and mental health screening and treatments targeted at those whose POM is due to non–pain relief motives.
Supplementary Material
Contributor Information
Ty S Schepis, Department of Psychology, Texas State University, San Marcos, Texas.
Linda Wastila, Peter Lamy Center on Drug Therapy and Aging, and Department of Pharmaceutical Health Services Research, School of Pharmacy, University of Maryland, Baltimore, Maryland.
Beth Ammerman, Center for the Study of Drugs, Alcohol, Smoking and Health, School of Nursing, University of Michigan, Ann Arbor, Michigan.
Vita V McCabe, Center for the Study of Drugs, Alcohol, Smoking and Health, School of Nursing, University of Michigan, Ann Arbor, Michigan; St. Joseph Mercy Ann Arbor, St. Joseph Mercy Health System, Ypsilanti, Michigan.
Sean Esteban McCabe, Center for the Study of Drugs, Alcohol, Smoking and Health, School of Nursing, University of Michigan, Ann Arbor, Michigan; Institute for Research on Women and Gender, University of Michigan, Ann Arbor, Michigan; Institute for Healthcare Policy and Innovation, University of Michigan, Ann Arbor, Michigan; Center for Human Growth and Development, University of Michigan, Ann Arbor, Michigan, USA; Center for Human Growth and Development, University of Michigan, Ann Arbor, Michigan, USA.
Funding sources: This work was supported by R01 DA043691, R01 DA42146, R01 DA036541, and R01 DA031160 from the National Institute on Drug Abuse (NIDA). The National Survey on Drug Use and Health is funded by the Substance Abuse and Mental Health Services Administration (SAMHSA) and NIDA.
Disclaimer: The content is the authors’ responsibility and does not necessarily represent the views of NIDA or SAMHSA.
Conflicts of interest: The authors note no conflicts of interest.
References
- 1. Scholl L, Seth P, Kariisa M, Wilson N, Baldwin G.. Drug and opioid-involved overdose deaths-United States. MMWR Morb Mortal Wkly Rep 2018;67(5152):2013–7; 1419–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Substance Abuse and Mental Health Services Administration. Key Substance Use and Mental Health Indicators in the United States: Results from the 2017 National Survey on Drug Use and Health (HHS Publication No. SMA 18-5068, NSDUH Series H-53). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; 2018. [Google Scholar]
- 3. Han B, Compton WM, Blanco C, Jones CM.. Correlates of prescription opioid use, misuse, use disorders, and motivations for misuse among US adults. J Clin Psychiatry 2018;79(5):17m11973. [DOI] [PubMed] [Google Scholar]
- 4. Maree RD, Marcum ZA, Saghafi E, Weiner DK, Karp JF.. A systematic review of opioid and benzodiazepine misuse in older adults. Am J Geriatr Psychiatry 2016;24(11):949–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Schepis TS, McCabe SE, Teter CJ.. Sources of opioid medication for misuse in older adults: Results from a nationally representative survey. Pain 2018;159(8):1543–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Schepis TS, McCabe SE.. Trends in older adult nonmedical prescription drug use prevalence: Results from the 2002-2003 and 2012-2013 National Survey on Drug Use and Health. Addict Behav 2016;60:219–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Center for Behavioral Health Statistics and Quality. 2016 National Survey on Drug Use and Health: Methodological Resource Book (Section 8, Data Collection Final Report). Rockville, MD: Substance Abuse and Mental Health Services Administration; 2017.
- 8. McCabe SE, Boyd CJ, Cranford JA, Teter CJ.. Motives for nonmedical use of prescription opioids among high school seniors in the United States: Self-treatment and beyond. Arch Pediatr Adolesc Med 2009;163(8):739–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Center for Behavioral Health Statistics and Quality. 2017 National Survey on Drug Use and Health: Methodological Resource Book (Section 11: Person-Level Sampling Weight Calibration). Rockville, MD: Substance Abuse and Mental Health Services Administration; 2019.
- 10.Center for Behavioral Health Statistics and Quality. 2016 National Survey on Drug Use and Health: Methodological Resource Book (Section 13: Statistical Inference Report). Rockville, MD: Substance Abuse and Mental Health Services Administration; 2017.
- 11. Yansaneh IS. Estimation of Sampling Errors for Complex Survey Data. New York, NY: United Nations Secretariat, Statistics Division; 2003. [Google Scholar]
- 12. Lipari RN, Williams MR, Van Horn SL. Why Do Adults Misuse Prescription Drugs? The CBHSQ Report. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2017. [PubMed]
- 13. McCabe SE, Cranford JA.. Motivational subtypes of nonmedical use of prescription medications: Results from a national study. J Adolesc Health 2012;51(5):445–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Schepis TS, Simoni-Wastila L, McCabe SE.. Prescription opioid and benzodiazepine misuse is associated with suicidal ideation in older adults. Int J Geriatr Psychiatry 2019;34(1):122–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mowbray O, Quinn A.. Prescription pain reliever misuse prevalence, correlates, and origin of possession throughout the life course. Addict Behav 2015;50:22–7. [DOI] [PubMed] [Google Scholar]
- 16. O’Malley PM, Bachman JG, Johnston LD.. Reliability and consistency in self-reports of drug use. Int J Addict 1983;18:805–24. [DOI] [PubMed] [Google Scholar]
- 17. Johnston LD, O'Malley PM.. Issues of validity and population coverage in student surveys of drug use. NIDA Res Monogr 1985;57:31–54. [PubMed] [Google Scholar]
- 18.Center for Behavioral Health Statistics and Quality. National Survey on Drug Use and Health (NSDUH): Summary of Methodological Studies, 1971-2014. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014. [PubMed]
- 19. Han BH, Palamar JJ.. Marijuana use by middle-aged and older adults in the United States, 2015-2016. Drug Alcohol Depend 2018;191:374–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Choi NG, DiNitto DM, Marti CN.. Nonmedical versus medical marijuana use among three age groups of adults: Associations with mental and physical health status. Am J Addict 2017;26(7):697–706. [DOI] [PubMed] [Google Scholar]
- 21. Lum HD, Arora K, Croker JA, et al. Patterns of marijuana use and health impact: A survey among older Coloradans. Gerontol Geriatr Medi 2019;5:2333721419843707.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Cunningham D, Flicker L, Murphy J, Aldworth J, Myers S, Kennet J. Incidence and impact of controlled access situations on nonresponse. Paper presented at: American Association for Public Opinion Research 70th Annual Conference; May 14–17, 2015; Hollywood, FL.
- 23. Dowell D, Haegerich TM, Chou R.. CDC guideline for prescribing opioids for chronic pain—United States, 2016. JAMA 2016;315(15):1624–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Williams AC, Eccleston C, Morley S.. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database Syst Rev 2012;11:CD007407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Nicholson AB, Watson GR, Derry S, Wiffen PJ.. Methadone for cancer pain. Cochrane Database Syst Rev 2017;2:CD003971.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Pergolizzi JV, Raffa RB, Marcum Z, Colucci S, Ripa SR.. Safety of buprenorphine transdermal system in the management of pain in older adults. Postgrad Med 2017;129(1):92–101. [DOI] [PubMed] [Google Scholar]
- 27. Schmidt-Hansen M, Taubert M, Bromham N, Hilgart JS, Arnold S.. The effectiveness of buprenorphine for treating cancer pain: An abridged Cochrane review. BMJ Support Palliat Care 2016;6(3):292–306. [DOI] [PubMed] [Google Scholar]
- 28. Johnson B, Richert T.. Diversion of methadone and buprenorphine from opioid substitution treatment: Patients who regularly sell or share their medication. J Addict Dis 2015;34(1):1–17. [DOI] [PubMed] [Google Scholar]
- 29. Jones JD, Manubay JM, Mogali S, et al. Abuse liability of intravenous buprenorphine vs. buprenorphine/naloxone: Importance of absolute naloxone amount. Drug Alcohol Depend 2017;179:362–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kampman K, Jarvis M.. American Society of Addiction Medicine (ASAM) national practice guideline for the use of medications in the treatment of addiction involving opioid use. J Addict Med 2015;9(5):358–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.