Abstract
Introduction: Breast cancer is common among women and reduces their quality of life. The current study aimed to investigate the effectiveness of mindfulness-based stress reduction group counseling in alleviating psychological responses such as anxiety, depression, stress, and regulating laboratory tests including cortisol and C-reactive protein (CRP) in women with breast cancer. Methods: This randomized clinical trial was conducted based on convenience sampling. Participants were divided into 2 groups (control and intervention groups) with block randomization. The intervention group received mindfulness-based stress reduction group counseling during 8 weeks. The participants completed the Beck anxiety inventory, Beck-II depression inventory, and perceived stress scale before and after the intervention and their blood samples were taken to check their cortisol and CRP. Results: After the intervention, the MBSR group had significantly lower anxiety compared with the control group (P < .001). No significant difference was found between the 2 groups in the reduction of perceived stress and depression (P < .05). In addition, no significant difference was found between the 2 groups in CRP and cortisol levels after the intervention (P > .05). Conclusion: The present study showed the effectiveness of mindfulness-based cognitive therapy in improving anxiety rather than the stress, depression, and inflammatory laboratory factors such as cortisol and CRP in women with breast cancer. Therefore, the psychological symptoms of these patients can be improved at different stages of treatment by providing this type of training.
Keywords: stress, anxiety, depression, breast cancer, mindfulness, group therapy, mindfulness-based stress reduction, inflammatory factors
Introduction
Cancer is the second leading cause of mortality in the world after cardiovascular disease.1 Approximately, 1.6 million cancers were diagnosed in the US in 2018, of which 271 000 were breast cancers.2 Breast cancer has the highest mortality rate throughout the world.3 In Iran, breast cancer is on the top of malignancies diagnosed in females,4 with approximately 33.21 cases per 100 000 population.5,6
Patients with breast cancer have numerous physical and psychological problems.7 Various factors such as fear of illness recurrence, body dysmorphic disorder, chemotherapy, surgery, young age, higher degree of illness, and lack of social support can lead to psychological responses in breast cancer patients.8,9 Psychological responses such as stress, depression, and anxiety are all associated with the disease diagnosis and treatment.10 Studies have shown the variable prevalence of depression (from 9% to 66%), stress (14.3%), anxiety (from 17.9% to 33%), and psychological disorders (from 15% to 60%) in women with breast cancer.11-14 Psychological problems not only impair the patients’ immune systems, but also severely affect their quality of life.15,16 They also increase inflammatory responses.17 Inflammatory factors such as cortisol and C-reactive protein (CRP) are associated with breast cancer progression18 and psychological problems.19 Studies have shown that regulated inflammatory factors are important indicators, reduce morbidity, and prolong life expectancy.20
According to the American Cancer Society Guideline, one of the keys to survival in these patients is the evaluation and management of long-term physical and mental health conditions related to breast cancer and its complications.21 Therefore, cognitive-behavioral interventions may be necessary for these patients in addition to drug therapy,22,23 One of these is mindfulness-based stress reduction (MBSR).24,25 Mindfulness focuses on the 3 elements of paying attention in the present moment, capacity to hold the object and non-judgment.26,27 This attitude leads to awareness of negative thoughts and prevents mind rumination.28 Many clinical psychologists believe that MBSR induces neuronal changes in the gray matter and regulates emotions.29,30
Some previous studies showed the effectiveness of mindfulness in improving psychological status,31-33 regulating cortisol level31,33 improving the immune system in breast cancer patients,34 and reducing CRP levels in healthy individuals.33,34 However, some other studies did not confirm the effectiveness of MBSR. Zhang et al showed the effectiveness of mindfulness intervention in the quality of life of breast cancer patients, but not in their sleep quality and pain.35 The results of a review study showed the effectiveness of mindfulness in lowering cortisol, heart rate, blood pressure, and tumor necrosis factor (TNF), but had little effect on CRP.32 Therefore, the impact of mindfulness on inflammatory factors is still unclear. The psychological problems of patients with breast cancer may affect and impair other family members’ quality of life and function.36 A few Iranian studies have assessed the effectiveness of MBSR in psychological problems and inflammatory factors of the patients with breast cancer. Therefore, the current study aimed to determine the effectiveness of mindfulness in psychological problems and inflammatory factors of breast cancer patients.
Method and Materials
Study Design and Setting
This study is a parallel-randomized clinical trial with allocation ratio of 1:1. The research settings were the medical offices of oncologists and medical centers affiliated to the Medical Science Universities of Kerman, southeast Iran. The intervention was performed in Bahonar Hospital. The study lasted from August 2017 to November 2019.
Sample Size and Sampling
The sample size was 22 individuals for each group according to a previous study (anxiety score: x1 = 47.53; S1 = 4.18 and x2 = 43.06; S2 = 4.39),33 the confidence coefficient of 95% and the test power of 90%.
Inclusion criteria were diagnosed disease between 3 months and 5 years, no use of psychological treatment before and during the intervention, no drug addiction, no acute psychiatric disorders (psychosis, severe mood disorder, etc.), no mental disorders,37 no use of anxiolytic and antidepressant medications, undergoing at least 1 chemotherapy period or surgery, ages between 18 and 70 years,37 breast cancer without metastasis,38 and no use of corticosteroids, psychoactive and hormonal drugs. Exclusion criteria were being absent in more than 3 sessions of MBSR, physical disability due to illnesses and treatments, use of corticosteroids, psychoactive and hormonal drugs,38 suffering from a major crisis during or about 3 months before intervention such as death of loved ones, comorbidity with autoimmune diseases, previous involvement in mindfulness groups,37 or endocrine diseases such as Cushing’s disease.39
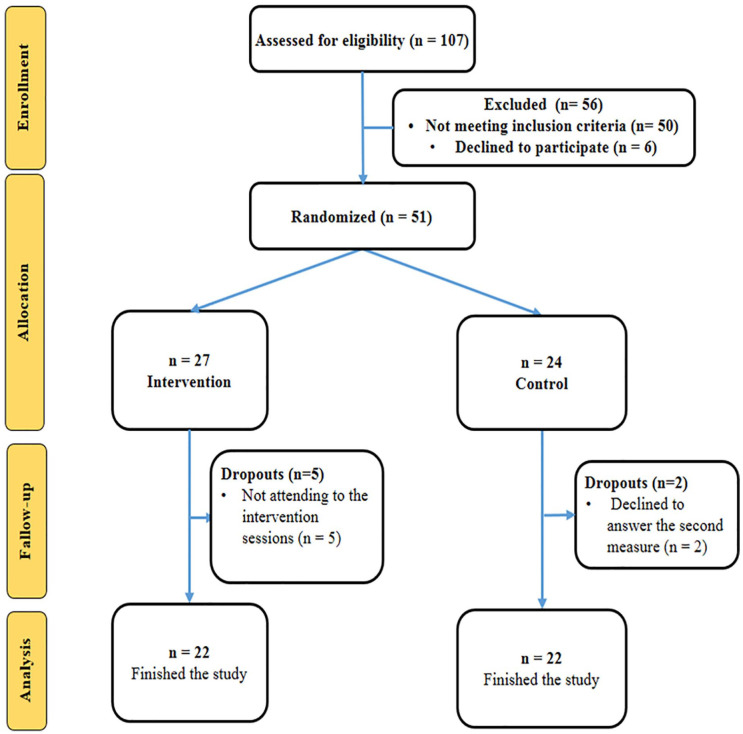
All eligible patients were included in the study using convenience sampling. Of 57 eligible participants (17 patients from Yas center, 10 from the Jawad-al-Aemah Clinic, and 30 from the oncologist’s office), 6 patients refused participation in the study. Finally, 44 patients completed the study (22 participants per group; Figure 1).
Figure 1.
The flow diagram of the study.
Samples were divided into 2 groups (routine care and mindfulness-based stress reduction group therapy) using block randomization. Labels of A, or B (A = MBSR and B = routine care) were assigned to each group, and the block size was considered 4. Then the randomization list was generated by free online software (https://www.sealedenvelope.com/simple-randomiser/v1/lists). The fourth researcher generated the random allocation sequence, and the first researcher enrolled and assigned participants to the groups.
Measurements
Demographic characteristics questionnaire, Beck depression inventory, Beck anxiety inventory, perceived stress scale, and laboratory test form were used in this study.
Demographic Characteristics
Demographic characteristics questionnaire includes age, sex, education, occupation, monthly income, type of insurance, disease duration, type of treatment, type of surgery, lymph node surgery, duration of chemotherapy, history of specific disease, and use of specific chemotherapy drugs.
Beck Anxiety Inventory (BAI)
Beck et al designed the anxiety inventory in 1988.40 The inventory specifically measures the severity of clinical anxiety symptoms. The BAI was scored on a scale value of 0 (not at all) to 3 (severely). The scores totally range from 0 to 63 (scores ranging from 0 to 7 would be considered minimal anxiety, scores ranging from 8 to 15 would be considered mild anxiety, scores ranging from 16 to 25 would be considered moderate anxiety, and scores ranging from 26 to 63 would be considered severe anxiety).40,41 The validity and reliability of the scale have been confirmed in Iran.41
Beck Depression Inventory-II (BDI-II)
Beck et al developed the depression inventory in 1971.42 This questionnaire is the new version of a 21-item self-report questionnaire for measuring depression severity in adults and adolescents over 13 years old. The items of this questionnaire measure the physical, behavioral, and cognitive symptoms of depression. The instrument was scored on the scale value of 0 (no specific sign) to 3 (severe signs). The scores totally range from 0 to 63. The cut-off point of this test is 13, meaning that scores ranging from 0 to 3 would be considered healthy, scores ranging from 14 to 19 would be considered mild depression, scores ranging from 20 to 28 would be considered moderate depression, and scores ranging from 29 to 63 would be considered severe depression. The validity and reliability of the scale have been confirmed in Iran.43
Perceived Stress Scale (PSS)
Cohen et al developed the perceived stress scale.44 The scale was scored based on a 5-point Likert scale (never = 0, almost never = 1, sometimes = 2, often = 3, and most of the time = 4). Phrases 4, 5, 6, 7, 9, 10, and 13 were scored inversely. Therefore, for the 14-item scale used in this study, the scores range from 0 to 56 with the higher score indicating more perceived stress. The validity and reliability of the scale have been confirmed in Iran.45
Laboratory Tests
To assess laboratory data including cortisol and CRP levels, the researcher took 4 cc brachial vein blood samples at 8 am. Fasting was not necessary for these tests. All tests were sent to the laboratory of Afzalipour hospital in Kerman. Only 1 person had to do the laboratory tests with the same device. The normal cortisol level in the morning is 7 to 28 μg/dL.46 The normal CRP level is also 0 to 10 mg/L.39
Data Collection and Intervention
At the beginning of the study, the patients completed demographic information, depression, anxiety, and perceived stress questionnaires and then, the researcher took 4 cc brachial vein blood samples to check laboratory tests for both groups. The intervention and control groups simultaneously recompleted the questionnaires and tests after the last session.
Samples in the control group received the routine care, which included consulting with the psychiatric nurses, and psychologists if requested. In addition, additional information for referral to psychologist offices and centers were provided to each participant.
Samples in the intervention group were divided into 2 groups of 12 to 14. They received the mindfulness-based stress reduction intervention in 90-minute sessions for 8 weeks (1 session a week; Box 1).
Box 1.
The Intervention Protocol.
|
Session 1: The study purpose and a summary of
sessions were explained. Participants were then asked to eat
a dried grape with full sensation, and practiced body scan
meditation for 30 minutes (while drawing their attention to
a part of their body). Session 2: Participants discussed the practice of body scan meditation at home, the obstacles (such as restlessness and mind wandering), the solutions (non-judgment and abandoning intrusive thoughts), and the difference between thoughts and feelings. The participants practiced meditation in a sitting position. Session 3: Participants saw and listened in a non-judging manner for 2 minutes, practiced meditation and breathing in a sitting position with focus on the physical sensations. Session 4: Participants focused on the body sounds and thoughts, discussed about stress responses, reaction to difficult situations, alternative attitudes and behaviors, and practiced mindful walking. Session 5: The participants did meditation in a sitting position and presented the second series of mindful body movements and mountain meditation. Session 6: Participants talked to each other about home practices. Then, the following theme was practiced: the content of thoughts is not often real. Thereafter, 4 types of meditation were practiced in 1 hour. Session 7: 4D meditation and awareness about everything at the present moment were practiced. The main theme of this session was as follows: what is the best way to take care of myself? Then, participants identified pleasant and unpleasant events, and planned an enjoyable program. Session 8: The participants used whatever they learned. They began with body scan meditation and discussed about the obstacles of meditation. |
One of the researchers (AA) skillful in MBSR prepared the intervention package. She trained the first researcher during 6 months, who in return trained participants in the intervention group.
Statistical Analysis
SPSS 18 was used in the study. Chi-square and Fisher’s exact tests were used to compare demographic characteristics between the 2 groups. Wilcoxon and Mann–Whitney tests were used to compare the mean stress scores in and between groups, respectively. Wilcoxon and independent t-tests were used to compare the mean scores of depression and anxiety in and between groups, respectively. Independent t-test and paired t-test were used to compare the mean laboratory data in and between the groups. ANCOVA test was also used to consider the confounding effect of variables. Significance level was considered 0.05.
Ethical Consideration
The Ethics Committee of Kerman University of Medical Sciences approved the present study (Code of Ethics: IR.KMU.REC.1396.2291). The protocol of the study was registered in the Iran clinical trial registration system (Clinical trial registration number: IRCT20180113038333N1). Informed consent was obtained from the participants. Samples were explained about the purpose of the study and were assured that their information would be kept confidential.
Results
The mean ages of the patients in the control and intervention groups were 45.64 and 44.14, respectively. Table 1 shows no significant difference between the 2 groups in the demographic and clinical characteristics except for the type of treatment.
Table 1.
Comparison of Demographic Characteristics Between Intervention and Control Groups.
| Group Variable |
Control Group |
Intervention Group |
Statistical Test | P Value | ||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| Age (years) | 45.64 | 10.11 | 44.14 | 11.19 | t = 0.47 | .64 |
| Disease duration (months) | 14.82 | 10.0 | 27.14 | 32.11 | Z = −1.27 | .20 |
| Frequency | % | Frequency | % | |||
| Education level | ||||||
| Uneducated | 3 | 13.6 | 2 | 9.1 | Fisher’s exact test = 1.91 | .81 |
| Middle/high school | 2 | 9.2 | 4 | 18.2 | ||
| Diploma | 4 | 18.2 | 5 | 22.7 | ||
| Associate/bachelor | 12 | 54.5 | 9 | 40.9 | ||
| Master/higher | 1 | 4.5 | 2 | 9.1 | ||
| Job | ||||||
| Housewife | 5 | 22.7 | 11 | 50 | χ2 = 3.96 | .18 |
| Employed | 12 | 54.6 | 9 | 40.9 | ||
| Self-employed | 5 | 22.7 | 2 | 9.1 | ||
| Insurance type | ||||||
| Self-employed | 3 | 13.6 | 1 | 4.5 | χ2 = 3.73 | .18 |
| Social security | 13 | 59.1 | 9 | 40.9 | ||
| Therapeutic services | 6 | 27.3 | 12 | 54.5 | ||
| Monthly family income | ||||||
| <1 million | 3 | 13.6 | 7 | 31.8 | χ2 = 3.34 | .36 |
| 1-2 million | 10 | 45.5 | 5 | 22.7 | ||
| 2-3 million | 6 | 27.3 | 7 | 31.8 | ||
| >3 million | 3 | 13.6 | 3 | 13.6 | ||
| History of other diseases | ||||||
| Yes | 21 | 95.5 | 21 | 95.5 | — | — |
| No | 1 | 4.5 | 1 | 4.5 | ||
| Type of treatment | ||||||
| Chemotherapy | 10 | 45.5 | 3 | 13.6 | Fisher’s exact test = 12.10 | .009 |
| Radiotherapy | 1 | 4.5 | 0 | 0 | ||
| Surgery | 3 | 13.6 | 0 | 0 | ||
| Chemotherapy and radiotherapy | 0 | 0 | 1 | 4.5 | ||
| Chemotherapy and surgery | 1 | 4.5 | 4 | 18.2 | ||
| Chemotherapy, radiotherapy and surgery | 7 | 31.8 | 14 | 63.6 | ||
| Chemotherapy sessions | ||||||
| ≤6 | 12 | 54.5 | 7 | 31.8 | χ2 = 2.32 | .11 |
| >6 | 10 | 45.5 | 15 | 68.2 | ||
Abbreviations: T, independent-t test; Z, Mann–Whitney U test.
The mean scores of anxiety in the control group were 25.41 and 35 before and after the study, respectively. In other words, anxiety increased in the control group over time. The mean score of anxiety in the intervention group decreased from 31.18 to 23.50 after the intervention. Mean anxiety score was significantly different after the intervention (Table 2). ANCOVA test was used to control the confounding effect of treatment type indicating a significant anxiety score between the intervention and control groups after the intervention (P = .01, mean difference = −10.88).
Table 2.
Comparison of Scores of Psychological Responses Between the Control and Intervention Groups Before and After the Intervention.
| Time Group |
Before Intervention |
After Intervention |
Wilcoxon Test | P Value | Pre- and Posttest Mean
Difference |
||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||||
| Anxiety | Control | 25.41 | 14.99 | 35.0 | 13.52 | 3.04 | .006 | 9.59 | 14.77 |
| Intervention | 31.18 | 14.05 | 23.50 | 11.35 | −2.96 | .007 | −7.68 | 12.17 | |
| Independent-t test | −1.32 | 3.06 | 4.23 | ||||||
| P value | .20 | .004 | <.001 | ||||||
| Depression | Control | 21.04 | 11.17 | 21.59 | 11.97 | 0.17 | .86 | 0.54 | 14.91 |
| Intervention | 29.00 | 13.01 | 17.18 | 9.46 | −4.35 | <.001 | −11.82 | 12.75 | |
| Independent-t test | −2.18 | 1.36 | 2.96 | ||||||
| P value | .04 | .18 | .005 | ||||||
| Perceived stress | Control | 28.64 | 3.0 | 28.04 | 2.28 | −0.86 | .39 | −0.6 | 3.38 |
| Intervention | 33.68 | 7.29 | 28.09 | 4.82 | −3.30 | .001 | −5.6 | 6.21 | |
| Mann–Whitney U test | −2.32 | −1.12 | −2.96 | ||||||
| P value | .02 | .26 | .003 | ||||||
The mean depression scores in the control group were 21.04 and 21.59 before and after the study, respectively. The mean depression score in the intervention group decreased from 29 to 17.18 after the intervention. Since the pre-intervention score was different between the 2 groups, the pre- and post-test score difference was calculated. The results showed a significant difference between the 2 groups (Table 2). ANCOVA test was performed to control the effects of pre-test score and the type of treatment indicating no significant difference in the depression score between the 2 groups after the intervention (P = .15).
The mean scores of perceived stress in the control group were 28.64 and 28.04 before and after intervention, respectively. The mean score of perceived stress in the intervention group decreased from 33.68 to 28.09 after the intervention. The perceived stress of the intervention group was significantly higher than that of the control group before the intervention, but this difference was not significant after the intervention (Table 2). Considering the confounding effect of treatment type and perceived stress score before the study, ANCOVA test showed no significant difference in perceived stress score after intervention (P = .14).
The mean CRP levels of the control group were 12.09 mg/dL and 11.50 mg/dL before and after the study, respectively. The mean CRP levels in the intervention group were 15.50 mg/dL and 14.32 mg/dL before and after the intervention, respectively. The mean CRP was not significantly different between the 2 groups before and after the intervention (Table 3). Considering the confounding effect of treatment, ANCOVA test showed no significant difference in the CRP score between the intervention and control groups after intervention (P = .61, mean difference = 1.15).
Table 3.
Comparison of Mean CRP and Cortisol Levels Between Control and Intervention Groups Before and After Intervention.
| Time Group |
Before Intervention |
After Intervention |
Paired-t test | P Value | Pre- and Posttest Mean
Difference |
||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||||
| CRP | Control | 12.09 | 6.24 | 11.50 | 6.28 | −2.35 | .03 | −0.59 | 1.18 |
| Intervention | 15.50 | 5.21 | 14.32 | 5.26 | −3.42 | .003 | −1.18 | 1.62 | |
| Independent t-test | −1.97 | −1.61 | 1.38 | ||||||
| P value | .06 | .11 | .18 | ||||||
| Cortisol | Control | 16.45 | 3.78 | 16.68 | 3.98 | 0.60 | .55 | 0.23 | 1.77 |
| Intervention | 18.77 | 4.05 | 18.27 | 4.28 | −1.33 | .2 | −0.5 | 1.77 | |
| Independent t-test | −1.96 | −1.28 | 1.36 | ||||||
| P value | .06 | .21 | .18 | ||||||
The mean cortisol levels of the control group were 16.45 μg/dL and 16.68 μg/dL before and after the study, respectively. The mean cortisol levels in the intervention group were 18.77 μg/dL and 18.27 μg/dL before and after the intervention, respectively. The mean cortisol level was not significantly different between the 2 groups before and after the intervention (Table 3). Considering the confounding effect of treatment, the ANCOVA test showed no significant difference in the mean cortisol level between the intervention and control groups after intervention (P = .08, mean difference = 2.31). In addition, the participants reported no adverse effect during the study.
Discussion
The results showed the effectiveness of MBSR in improving anxiety of the patients with breast cancer. Although, MBSR clinically improved patients’ stress and depression, it was not statistically significant. Furthermore, MBSR had no significant effect on the reduction of cortisol and CRP levels.
Many studies have supported the effect of mindfulness on psychological variables. The current study only showed the effect of mindfulness on anxiety. Zeinal et al15 have confirmed this result. Some studies showed the effectiveness of psychological interventions in the autonomic nervous system and endocrine system leading to reduction of anxiety. Some articles such as that of Khoury et al showed ineffectiveness of mindfulness in anxiety.47 Patients with breast cancer experience great anxiety, so they may follow mindfulness practices more. In addition, participants had severe anxiety at the beginning of the study. This may be a reason why the MBSR has been more effective in patients with breast cancer than healthy individuals.
The present study showed no significant effect of MBSR on depression. Khoury et al showed no significant effect of the MBSR method on depressed healthy subjects because of subjects’ bias in filling questionnaires, inadequate number of sessions, or improper quality of training.19 On the other hand, Johns et al examined the effectiveness of mindfulness-based stress reduction program in the US breast and colorectal cancer survivors. MBSR has been effective in reducing depression.48 Armani Kian et al also showed the effectiveness of mindfulness in emotional health, depression, and glucose control in patients with type-II diabetes mellitus.49 Different results may be due to self-report questionnaires, which might be completed by patients pessimistically. Other possible causes may be the quantity and quality of interventions, different types of disease and their effects on patients’ general condition, different treatments or medications and their side effects on general condition, cultural differences, support, patients’ interest, and mindfulness practices at home. In addition, participants had moderate depression at the beginning of the study showing that the MBSR was less effective in alleviating depression of the patients with breast cancer in the present study.
Mindfulness had no significant effect on stress in the current study. Nyklíček and Kuijpers in the Netherlands performed MBSR on men with distress symptoms and found no significant difference between the 2 groups.50 However, Zhang et al in China studied the effectiveness of Mindfulness-Based Stress Reduction Program (MBSR) in post-traumatic growth of the breast cancer survivors and showed a significant decrease in their stress 8 weeks after intervention.35 The ineffectiveness of MBSR in the present study may be due to the disease type, its psychological effects, and inadequate social support. Shaban et al reported that cancer patients undergoing chemotherapy in Iran experienced several problems. The Iranian society has less addressed the patients’ quality of life and its associated factors.51 Different results may be due to different tools, type of illness, number and arrangement of educational sessions, cultural differences including family self-care communication, social, organizational, and governmental support, different health care costs in different countries or even different beliefs. According to Pourghane et al, stress coping strategies employed by people in stressful situations can be influenced by religious beliefs, culture, social support, and knowledge.52
Some studies supported the ineffectiveness of MBSR in inflammatory factors. Matchim et al showed ineffectiveness of mindfulness in regulating laboratory tests (lymphocytes in cancer patients, melatonin, and cortisol), blood pressure, and heart rate.32 Moreover, Pascoe et al showed the effectiveness of mindfulness in decreasing cortisol level, heart rate, blood pressure, and TNF, but little effect on CRP.53 Some studies also confirmed the effect of mindfulness on inflammatory factors.31,32 Meyer et al showed the effectiveness of mindfulness in reducing CRP levels of the healthy individuals.34 These differences can be due to the number of intervention sessions, the number of samples, the amount of stress, support, the study population, and the type of drug therapy affecting the body and the immune system.
The psychological responses of people are intense after cancer diagnosis depending on the prognosis of the disease, the experiences of pain and suffering, and the costs of treatment. Therefore, health care providers, particularly physicians and nurses, should support patients, their families, and psychological interventions. It is recommended that psychological techniques be considered for both patients and families. In addition to changing educational and counseling techniques, governmental organizations should support patients to reduce their stress and improve their quality of life.
The present study had some limitations. Many individual and family characteristics, and individual motivations might influence the study results, however the researcher has attempted to choose participants with the most similarities. Since patients with cancer and their families were experiencing a stressful situation, several were reluctant to participate in the study. Many patients with breast cancer were unaware of their disease or treatment process, so the sampling process lasted nearly a year; this long period of study may influence the results. Finally, these results should be generalized to other populations with caution.
Conclusion
The results of the present study suggest the effectiveness of MBSR only in anxiety of the women with breast cancer, however the clinical effect of MBSR on stress and depression should not be ignored. MBSR also had no effect on inflammatory factors such as cortisol and CRP. Further studies are recommended to investigate the effect of MBSR on psychological responses and inflammatory factors of both patients with cancer and their spouses.
Acknowledgments
We would thank all patients for their cooperation. The approved research project code was 96000440.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Considerations: The Ethics Committee of Kerman University of Medical Sciences approved the present study (code of ethics: IR.KMU.REC.1396.2291 and the clinical trial code no. IRCT20180113038333N1). Before the sampling, a written letter of introduction from Razi School of Nursing and Midwifery was presented to the authorities of the study setting. Informed consent was obtained from the participants. Samples were adequately explained about the purpose of the study and were assured that their information would be kept confidential.
ORCID iD: Mahlagha Dehghan  https://orcid.org/0000-0002-4205-829X
https://orcid.org/0000-0002-4205-829X
References
- 1. Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095-2128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69:7-34. [DOI] [PubMed] [Google Scholar]
- 3. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394-424. [DOI] [PubMed] [Google Scholar]
- 4. Farhood B, Geraily G, Alizadeh A. Incidence and mortality of various cancers in Iran and compare to other countries: a review article. Iran J Public Health. 2018;47:309-316. [PMC free article] [PubMed] [Google Scholar]
- 5. Asgarian F, Mirzaei M, Asgarian S, Jazayeri M. Epidemiology of breast cancer and the age distribution of patients over a period of ten years. Iran J Breast Dis. 2016;9:31-36. [Google Scholar]
- 6. Nafissi N, Khayamzadeh M, Zeinali Z, Pazooki D, Hosseini M, Akbari ME. Epidemiology and histopathology of breast cancer in Iran versus other Middle Eastern countries. Middle East J Cancer. 2018;9:243-251. [Google Scholar]
- 7. Greenlee H, Balneaves LG, Carlson LE, et al. Clinical practice guidelines on the use of integrative therapies as supportive care in patients treated for breast cancer. J Natl Cancer Inst Monogr. 2014;2014:346-358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Yang H, Brand JS, Fang F, et al. Time-dependent risk of depression, anxiety, and stress-related disorders in patients with invasive and in situ breast cancer. Int J Cancer. 2017;140:841-852. [DOI] [PubMed] [Google Scholar]
- 9. Gheibizadeh M, Pourghane P, Mosaffa Khomami H, Heidari F, Atrkar Roushan Z. The relationship between stressors and coping strategies employed by retired elderly. J Nurs Educ. 2017;4:36-43. [Google Scholar]
- 10. Lengacher CA, Reich RR, Paterson CL, et al. Examination of broad symptom improvement resulting from mindfulness-based stress reduction in breast cancer survivors: a randomized controlled trial. J Clin Oncol. 2016;34:2827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Maass SW, Roorda C, Berendsen AJ, Verhaak PF, de Bock GH. The prevalence of long-term symptoms of depression and anxiety after breast cancer treatment: a systematic review. Maturitas. 2015;82:100-108. [DOI] [PubMed] [Google Scholar]
- 12. Wefel JS, Kesler SR, Noll KR, Schagen SB. Clinical characteristics, pathophysiology, and management of noncentral nervous system cancer-related cognitive impairment in adults. CA Cancer J Clin. 2015;65:123-138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. O’Connor M, Christensen S, Jensen AB, Møller S, Zachariae R. How traumatic is breast cancer? Post-traumatic stress symptoms (PTSS) and risk factors for severe PTSS at 3 and 15 months after surgery in a nationwide cohort of Danish women treated for primary breast cancer. Br J Cancer. 2011;104:419-426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Mitchell AJ, Ferguson DW, Gill J, Paul J, Symonds P. Depression and anxiety in long-term cancer survivors compared with spouses and healthy controls: a systematic review and meta-analysis. Lancet Oncol. 2013;14:721-732. [DOI] [PubMed] [Google Scholar]
- 15. Zainal NZ, Booth S, Huppert FA. The efficacy of mindfulness-based stress reduction on mental health of breast cancer patients: A meta-analysis. Psychooncology. 2013;22:1457-1465. [DOI] [PubMed] [Google Scholar]
- 16. Reis JC, Antoni MH, Travado L. Emotional distress, brain functioning, and biobehavioral processes in cancer patients: a neuroimaging review and future directions. CNS Spectr. 2020;25:79-100. [DOI] [PubMed] [Google Scholar]
- 17. Howren MB, Lamkin DM, Suls J. Associations of depression with C-reactive protein, IL-1, and IL-6: a meta-analysis. Psychosom Med. 2009;71:171-186. [DOI] [PubMed] [Google Scholar]
- 18. Villasenor A, Flatt SW, Marinac C, Natarajan L, Pierce JP, Patterson RE. Postdiagnosis C-reactive protein and breast cancer survivorship: findings from the WHEL study. Cancer Epidemiol Biomarkers Prev. 2014;23:189-199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Khoury JE, Enlow MB, Plamondon A, Lyons-Ruth K. The association between adversity and hair cortisol levels in humans: a meta-analysis. Psychoneuroendocrinology. 2019;103:104-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Finch CE. The Biology of Human Longevity: Inflammation, Nutrition, and Aging in the Evolution of Lifespans. Boston, MA: Elsevier; 2010. [Google Scholar]
- 21. Runowicz CD, Leach CR, Henry NL, et al. American cancer society/American society of clinical oncology breast cancer survivorship care guideline. CA Cancer J Clin. 2016;66:43-73. [DOI] [PubMed] [Google Scholar]
- 22. Praissman S. Mindfulness-based stress reduction: a literature review and clinician’s guide. J Am Acad Nurse Pract. 2008;20:212-216. [DOI] [PubMed] [Google Scholar]
- 23. Ng CG, Boks MP, Zainal NZ, de Wit NJ. The prevalence and pharmacotherapy of depression in cancer patients. J Affect Disord. 2011;131:1-7. [DOI] [PubMed] [Google Scholar]
- 24. Sauer S, Baer RA. Mindfulness and decentering as mechanisms of change in mindfulness-and acceptance-based interventions. In: Baer RA, ed. Assessing Mindfulness and Acceptance Processes in Clients: Illuminating the Theory and Practice of Change. Oakland, CA: Context Press/New Harbinger Publications; 2010:25-50. [Google Scholar]
- 25. Crane B. Full catastrophe living; using the wisdom of your body and mind to face stress, pain and illness. Jon Kabat-Zinn, 1996 Publisher: Piatkus, London ISBN: 0-749-915-854. Spiritual Health Int. 2002;3:52-52. [Google Scholar]
- 26. Crane R, Brewer J, Feldman C, et al. What defines mindfulness-based programs? The warp and the weft. Psychol Med. 2017;47:990-999. [DOI] [PubMed] [Google Scholar]
- 27. Dreyfus G. Is mindfulness present-centred and non-judgmental? A discussion of the cognitive dimensions of mindfulness. Contemporary Buddhism. 2011;12:41-54. [Google Scholar]
- 28. Birnie K, Garland SN, Carlson LE. Psychological benefits for cancer patients and their partners participating in mindfulness-based stress reduction (MBSR). Psychooncology. 2010;19:1004-1009. [DOI] [PubMed] [Google Scholar]
- 29. Singh SK, Gorey KM. Relative effectiveness of mindfulness and cognitive behavioral interventions for anxiety disorders: meta-analytic review. Soc Work Ment Health. 2018;16:238-251. [Google Scholar]
- 30. Garland SN, Carlson LE, Antle MC, Samuels C, Campbell T. I-CAN SLEEP: rationale and design of a non-inferiority RCT of mindfulness-based stress reduction and cognitive behavioral therapy for the treatment of insomnia in CANcer survivors. Contemp Clin Trials. 2011;32:747-754. [DOI] [PubMed] [Google Scholar]
- 31. Janusek LW, Tell D, Mathews HL. Mindfulness based stress reduction provides psychological benefit and restores immune function of women newly diagnosed with breast cancer: a randomized trial with active control. Brain Behav Immun. 2019;80:358-373. [DOI] [PubMed] [Google Scholar]
- 32. Matchim Y, Armer JM, Stewart BR. Mindfulness-based stress reduction among breast cancer survivors: a literature review and discussion. Oncol Nurs Forum. 2011;38:E61-E71. [DOI] [PubMed] [Google Scholar]
- 33. Hsiao F-H, Jow G-M, Kuo W-H, et al. The long-term effects of mindfulness added to family resilience-oriented couples support group on psychological well-being and cortisol responses in breast cancer survivors and their partners. Mindfulness. 2016;7:1365-1376. [Google Scholar]
- 34. Meyer JD, Hayney MS, Coe CL, Ninos CL, Barrett BP. Differential reduction of IP-10 and C-reactive protein via aerobic exercise or mindfulness-based stress-reduction training in a large randomized controlled trial. J Sport Exerc Psychol. 2019;41:96-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Zhang J-Y, Zhou Y-Q, Feng Z-W, Fan Y-N, Zeng G-C, Wei L. Randomized controlled trial of mindfulness-based stress reduction (MBSR) on posttraumatic growth of Chinese breast cancer survivors. Psychol Health Med. 2017;22:94-109. [DOI] [PubMed] [Google Scholar]
- 36. Johansen S, Cvancarova M, Ruland C. The effect of cancer patients’ and their family caregivers’ physical and emotional symptoms on caregiver burden. Cancer Nurs. 2018;41:91-99. [DOI] [PubMed] [Google Scholar]
- 37. Carlson LE, Speca M, Faris P, Patel KD. One year pre-post intervention follow-up of psychological, immune, endocrine and blood pressure outcomes of mindfulness-based stress reduction (MBSR) in breast and prostate cancer outpatients. Brain Behav Immun. 2007;21:1038-1049. [DOI] [PubMed] [Google Scholar]
- 38. Carlson LE, Beattie TL, Giese-Davis J, et al. Mindfulness-based cancer recovery and supportive-expressive therapy maintain telomere length relative to controls in distressed breast cancer survivors. Cancer. 2015;121:476-484. [DOI] [PubMed] [Google Scholar]
- 39. Fischbach FT, Dunning MB. A Manual of Laboratory and Diagnostic Tests. Philadelphia, PA: Lippincott Williams & Wilkins; 2009. [Google Scholar]
- 40. Beck AT, Steer RA, Carbin MG. Psychometric properties of the Beck depression inventory: twenty-five years of evaluation. Clin Psychol Rev. 1988;8:77-100. [Google Scholar]
- 41. Khesht-Masjedi MF, Omar Z, Masoleh SMK. Psychometrics properties of the Persian version of Beck anxiety inventory in North of Iranian adolescents. Int J Educ Psychol Res. 2015;1:145. [Google Scholar]
- 42. Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56:893. [DOI] [PubMed] [Google Scholar]
- 43. Dadfar M, Kalibatseva Z. Psychometric properties of the Persian version of the short beck depression inventory with Iranian psychiatric outpatients. Scientifica. 2016;2016: 8196463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983:385-396. [PubMed] [Google Scholar]
- 45. Safai M, Shokri O. Assessing stress in cancer patient: factorial validity of the stress scale in Iran. Iran J Psychiatr Nurs. 2014;2:13-22. [Google Scholar]
- 46. McPherson RA, Pincus MR. Henry’s Clinical Diagnosis and Management by Laboratory Methods E-Book. Philadelphia, PA: Elsevier Health Sciences; 2011. [Google Scholar]
- 47. Khoury B, Sharma M, Rush SE, Fournier C. Mindfulness-based stress reduction for healthy individuals: a meta-analysis. J Psychosom Res. 2015;78:519-528. [DOI] [PubMed] [Google Scholar]
- 48. Johns SA, Brown LF, Beck-Coon K, et al. Randomized controlled pilot trial of mindfulness-based stress reduction compared to psychoeducational support for persistently fatigued breast and colorectal cancer survivors. Support Care Cancer. 2016;24:4085-4096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Armani Kian A, Vahdani B, Noorbala A, et al. The impact of mindfulness-based stress reduction on emotional wellbeing and glycemic control of patients with type 2 diabetes mellitus. J Diabetes Res. 2018;2018:1986820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Nyklíček I, Kuijpers KF. Effects of mindfulness-based stress reduction intervention on psychological well-being and quality of life: is increased mindfulness indeed the mechanism? Ann Behav Med. 2008;35:331-340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Shaban M, Monjamed Z, Mehran A, Hasanpour Dehkordi A. The relation between the cancer characteristics and quality of life in the patients under chemotherapy. Hayat. 2004;10:79-84. [Google Scholar]
- 52. Pourghane P, Sharif Azar E, Zaer Sabet F, Khorsandi M. Survey the effect of religious beliefs in stress reduction in students of langroud faculty of medical sciences. J Holist Nurs Midwifery. 2010;20:10-15. [Google Scholar]
- 53. Pascoe MC, Thompson DR, Jenkins ZM, Ski CF. Mindfulness mediates the physiological markers of stress: systematic review and meta-analysis. J Psychiatr Res. 2017;95:156-178. [DOI] [PubMed] [Google Scholar]