Abstract
This study tests a socioecological model of relapse and recovery using latent class growth mixture modeling to identify neighborhood, social network and individual-level predictors of alcohol dependence trajectories among a large, longitudinal sample of problem drinkers recruited from substance use treatment settings. We identified four distinct alcohol dependence trajectories: Stable Recovery/Low (Class 1); Relapsing/Rising (Class 2); Late Recovery/Declining (Class 3); and Chronic/High (Class 4). Neighborhood context (poverty and density of bars), social network characteristics (less involvement with Alcoholics Anonymous [AA], continued affiliation with heavy drinkers), and individual predisposing (psychiatric severity) and need (returning to treatment) characteristics each distinguished individuals in the Relapsing/Rising class from individuals in the Stable Recovery/Low class. Social network characteristics (AA involvement and continued affiliation with heavy drinkers) were the primary distinguishing factors for individuals in the Chronic/High class compared to the Late Recovery/Declining class. Study findings can be used to promote recovery and help prevent relapse by: guiding development of community-level interventions to improve social and physical environments; identifying potentially modifiable factors (social network support for sobriety, participation in self-help) to reduce negative consequences among problem drinkers who remain in high-risk neighborhoods; and contributing to ongoing discussions about new and continued licensing of alcohol outlets and regulation of alcohol sales to prevent alcohol problems in high-risk areas and among high-risk people.
Keywords: alcohol dependence, neighborhood environment, social networks, relapse, recovery, socioecological model, longitudinal trajectory
Alcohol problems, including social, legal, and other negative consequences resulting from heavy alcohol use, often are described as part of a chronic, reoccurring condition that requires ongoing care and support.1 Over the past decade, attention has increasingly turned to understanding and characterizing successful recovery from alcohol problems, with clinical researchers examining factors that contribute to attainment of long-term stability and remission of problems. Definitions of recovery vary, but they often include abstinence from or non-problematic use of alcohol (and perhaps other drugs), as well as an acknowledgement of other dimensions of mental and physical health, well-being, and quality of life.2-5 Using data from an existing longitudinal study of alcohol treatment clients supplemented with new information on the neighborhood environment, we develop and test a socioecological model of relapse and recovery from alcohol problems to describe how neighborhood, social network, and individual factors relate to alcohol problems experienced over a seven-year period.
Theoretical framework
Our study is informed by models of relapse prevention6 and environmental prevention theory.7,8 Environmental and community systems prevention focuses on individuals in their environments, which can inform interventions to alter the social, cultural, economic, and physical context to shift conditions away from those that promote relapse to those that support sustained recovery from alcohol problems.8 In addition to affecting targeted individuals at a given time, these approaches have the added benefit of potentially helping individuals who later enter the improved environment.9,10 Similarly, recovery-oriented systems of care emphasize neighborhood-based delivery of services and development of community-based recovery support systems that provide ongoing, integrated services to prevent relapse.11 These notions are consistent with relapse prevention paradigms encouraging a shift from a model of treatment that includes repeated episodes of acute care toward a model of chronic care focused on longer term recovery management.1,12
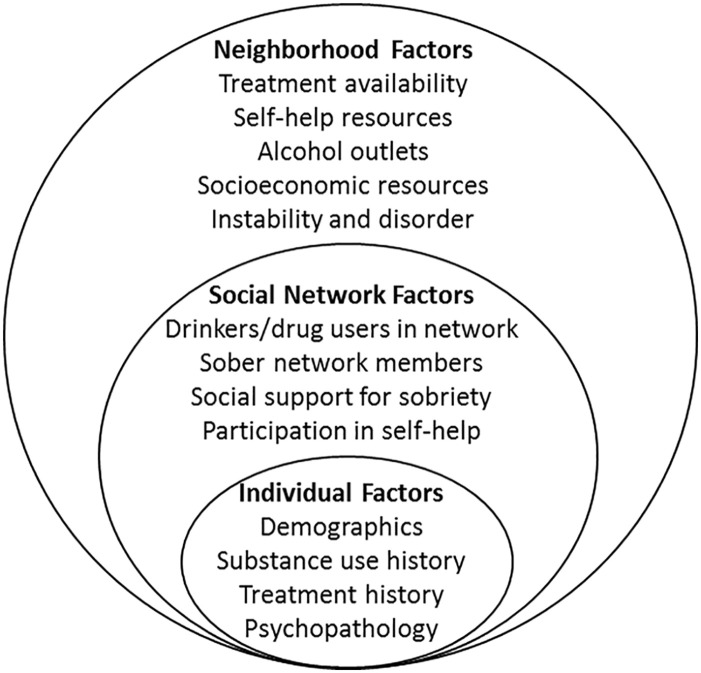
We propose a socioecological model that builds on prior epidemiologic models9,13 and integrates these perspectives to contextualize relapse and recovery over time. Studies of alcohol use patterns,14,15 negative consequences of use,16-18 and dependence19,20 suggest that neighborhood contexts impact alcohol outcomes, but few studies have examined the longitudinal effects of neighborhoods on recovery from alcohol problems. In our conceptual model (Figure), individuals reside in neighborhood contexts that contribute to the probability of recovery after treatment. These principles also have been capitalized on by the Oxford House movement in efforts to promote housing after substance use disorder treatment in group settings located in safe and stable neighborhoods in proximity to recovery resources.21 In our model, relevant neighborhood attributes include locations and characteristics of substance use disorder treatment facilities (public and private), self-help resources (Alcoholics Anonymous meetings), alcohol outlets (off-premise liquor stores, as well as on-premise bars and restaurants), and socioeconomic resources. These are accompanied by relevant social network (drinkers/drug users in network, sober network members, participation in self-help, and pressure to stop drinking or get treatment) and individual characteristics (demographics, mental health, drug use, and treatment history) that affect long-term outcomes.
Figure 1.
Socioecological model of relapse and recovery.
Neighborhood factors related to relapse and recovery
Jacobson22 detailed neighborhood features related to completion of substance use disorder treatment, which also may impact sustained recovery. Neighborhood drug availability can lead to substance use,23 alcohol dependence,24 and relapse into heavy drug use and problems.25 Similarly, living in neighborhoods with easy access to alcohol could increase individuals’ likelihood of relapse, as alcohol outlet density is positively associated with alcohol use26,27 and alcohol problems.20,28-31 However, relatively few studies of treatment clients have used individual-level data on alcohol problems coupled with area-based measures of outlet density, much less with longitudinal data. We examine effects of alcohol outlets on trajectories of alcohol problems, and expect a higher density of alcohol outlets will predict relapse into alcohol problems.
Neighborhood socioeconomic disadvantage also is associated with heavy drinking14,32,33 and alcohol problems,16,34 and it predicts alcohol use disorders up to 12 years after exposure.19 Consequences of heavy substance use, including overdose and incarceration, also may be higher for people living in disadvantaged areas.35 Few longitudinal studies have examined neighborhood SES effects on alcohol problems experienced after someone completes treatment, so we examine effects of neighborhood disadvantage on recovery from alcohol problems. We hypothesize neighborhood disadvantage will predict relapse into problem drinking.
Community resources may impact treatment utilization, self-help involvement, relapse, and recovery from alcohol problems over time. Several studies suggest proximity to mental health and substance use disorder treatment is an important determinant of treatment utilization and quality of care.36-40 Alcoholics Anonymous (AA) attendance and involvement also are important predictors of abstinence over time.41-46 One study of male veterans who received inpatient treatment found that a city’s number of weekly self-help meetings was positively related to self-help involvement post-treatment47; they did not report effects on relapse or recovery. We examine effects of locations and characteristics of substance use disorder treatment facilities and self-help resources on longitudinal trajectories of alcohol problems. We hypothesize that proximity to recovery resources will be positively associated with recovery.
Social network factors related to relapse and recovery
Because it can be difficult to change neighborhoods, we also seek to identify modifiable social network factors that help prevent relapse. Prior work with these data has found that heavy drinkers and drug users in the social network is one of the strongest predictors of higher alcohol volume,48-51 continued problem drinking,52,53 and binge drinking.54 Although some models of relapse prevention include high-risk situations, these typically have been limited to a person’s social network,55,56 without also considering the influence of the neighborhood context on an individual’s alcohol use and problem trajectories.19,57 We did not find any studies comparing effects of social network characteristics with those of exposure to high-risk neighborhoods in relation to relapse or recovery from alcohol problems, although in our prior work with these data, we have shown that social networks and neighborhood contexts jointly influence alcohol use.33,58 Understanding the neighborhood and social network context of alcohol problems among heavy and dependent drinkers can inform service planning to provide continuing care after treatment and support long-term recovery from alcohol problems by people in high-risk neighborhoods.
Individual factors related to relapse and recovery
Key aspects of individuals themselves, such as mental health and co-occurring drug use, also impact relapse and recovery from alcohol problems. As such, our study also is informed by Aday and Andersen’s model of health services utilization.59 Enabling factors and need characteristics indicating severity of alcohol problems are associated with abstinence outcomes,52,60,61 as well as trajectories of alcohol use51 in these data, and other research also supports the consideration of these factors in longitudinal studies of relapse and recovery.62,63 Individual-level risk factors such as psychological problems may indicate someone has fewer resources to cope with stress, and thus they may relapse or continue to drink heavily, even after completing treatment. No identified studies have examined the role of these individual-level risk factors for relapse in concert with neighborhood and social network characteristics in a longitudinal study of adult treatment clients, however. Our study aims to address these gaps.
Aims of current study
Our primary goals were to characterize neighborhoods that support recovery and identify modifiable social network and individual factors that help prevent relapse of alcohol problems in the seven years after attending alcohol treatment. Capitalizing on unique data available from a large sample of problem and dependent drinkers recruited from treatment centers, we used latent class growth mixture models to describe longitudinal trajectories of alcohol dependence symptoms in a sample of over 700 adults recruited from alcohol treatment programs, and then assessed predictors of class membership to inform a socioecological model of relapse and recovery.
Methods
Data
Participants were from a longitudinal study conducted between 1995 and 2006 that recruited clients meeting criteria for problem drinking (defined below) from 10 public and private detoxification, residential, and outpatient alcohol and drug treatment programs in one Northern California county. Additional information on recruitment and data collection procedures is provided elsewhere.64 Clients who were at least 18 years of age and gave their written informed consent participated in an in-person structured interview administered by trained interviewers. A total of 926 clients were recruited for the study within three days after entering treatment (80% participation rate). Data on the neighborhood environment were added later (see methods described below).
The initial inclusion criterion required at least two of three problem drinking criteria over the prior 12 months: (1) drinking five or more drinks per day at least once a month for men OR three or more drinks per day at least once a week for women, (2) one or more of eight alcohol-related social consequences in the past year, and/or (3) one or more of nine alcohol dependence symptoms in the past year. These criteria are consistent with prior studies.33,58,65 Follow-up interviews were conducted one, three, five, and seven years after baseline, using computer assisted telephone interviewing; 783 respondents (84.6%) completed at least one follow-up interview. Respondents were tracked every three months using postcard mailings and telephone check-ins.
Participant addresses at each survey timepoint and each interim tracking check-in were geocoded and linked to neighborhood data using ArcGIS 10.2 (ESRI, 2013). For linkage with US Census data on sociodemographic characteristics, neighborhoods were defined by census tract boundaries. For linkage with all other types of neighborhood data (such as alcohol outlets and recovery resources), the geocoded address was used. Values were assigned based on the weighted average across all known addresses during the 12 months prior to each follow-up interview. For the present analysis, due to data availability limitations, eligible geographic areas of residence were restricted to the four Northern California counties which contained the majority of study participants over the follow-up period and for which we had compiled historical data on recovery resources, including 12-step meeting locations and weekly meeting frequency, as well as availability of alcohol/drug treatment. All study procedures were approved by the Institutional Review Boards at the University of California, San Francisco (IRB #11-05204) and the Public Health Institute, Oakland, CA (IRB #I99-015 & I11-021e).
The final analytic sample included all participants who had valid neighborhood data at baseline and for at least one follow-up interview (n = 722; 92.2% of those completing one or more follow-up interview). The analytic sample was 66% male, 54% White and 32% Black/African American (6% Hispanic/Latino and 8% some other race/ethnicity), with an average age at baseline of 38.6 years. Of the respondents in the analytic sample, 76% participated in all four follow-up interviews, 11% completed three interviews, 8% completed two interviews and 5% completed one follow-up after baseline. Men were less likely than women to participate in at least three follow-up interviews (chi-square(df = 1) = 4.55, P = .03) and respondents with more heavy drinkers in their social networks at baseline were marginally less likely to participate in at least three follow-up interviews (t-test = 1.27, P = .10). No significant differences were found on type of treatment program from which the respondent was recruited, baseline 12-step involvement, or baseline neighborhood context (poverty, alcohol availability, 12-step meeting availability or treatment availability) between those who participated in fewer than three follow-ups and those who participated in at least three follow-ups.
Measures
The outcome modeled in the trajectory analyses was alcohol dependence symptoms experienced over the past year as reported at each follow-up interview. This measure was drawn from the eight alcohol-related social consequences and nine alcohol dependence symptoms that were used to establish initial eligibility for the longitudinal study. Social consequences included events such as traffic accidents while drinking and driving, serious arguments with family members or close others about their drinking, and complaints in the workplace about their drinking. Dependence symptoms included desire to cut down/stop drinking, drinking to relieve withdrawal symptoms, drinking interfering with role responsibilities, and blackouts due to heavy drinking. The combination of social problems and physiological symptoms approximates the criteria used in the DSM-566 classification of alcohol use disorder. Scores represented alcohol dependence severity, ranging from 0 to 16 symptoms reported, with an average of 5.59 at baseline, 3.47 at one year, 2.80 at three years, 2.39 at five years, and 2.26 at seven years.
We included predictor variables at the neighborhood level, as well as social network characteristics and individual-level predisposing and need factors (see Tables 1 and 2). Time-varying characteristics were averaged over the follow-up period so they could be entered as predictors of trajectories of alcohol dependence symptoms (described in Analysis section below).
Table 1.
Sample characteristics (N = 722).
| Mean OR % | |
|---|---|
| Age at baseline | 38.6 |
| Male gender | 66% |
| Race/ethnicity | |
| White | 54% |
| Black | 32% |
| Hispanic | 6% |
| Other | 8% |
| Educational attainment | |
| Less than high school | 22% |
| High school diploma/GED | 51% |
| More than high school | 27% |
| Married/partnered at baseline | 30% |
| Study recruitment site | |
| Outpatient program | 39% |
| Inpatient/residential program | 30% |
| Detoxification program | 30% |
| Household income GE $25 000 | 41% |
| Regular use of alcohol by age 16 | 26% |
Table 2.
Time-varying measures tested as predictors of class membership.
| Baseline | One year after Treatment | Three year follow-up | Five year follow-up | Seven year follow-up | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | LCL 95% CI | UCL 95% CI | Mean | LCL 95% CI | UCL 95% CI | Mean | LCL 95% CI | UCL 95% CI | Mean | LCL 95% CI | UCL 95% CI | Mean | LCL 95% CI | UCL 95% CI | |
| ASI drug severity score | 0.13 | 0.12 | 0.14 | 0.05 | 0.04 | 0.05 | 0.04 | 0.03 | 0.05 | 0.05 | 0.04 | 0.05 | 0.05 | 0.04 | 0.05 |
| ASI psychiatric score | 0.39 | 0.37 | 0.41 | 0.21 | 0.19 | 0.22 | 0.20 | 0.19 | 0.22 | 0.22 | 0.21 | 0.24 | 0.21 | 0.19 | 0.23 |
| Went to treatment in past 12 months, proportiona | 0.70 | 0.67 | 0.73 | 0.40 | 0.36 | 0.44 | 0.29 | 0.25 | 0.32 | 0.22 | 0.18 | 0.25 | 0.19 | 0.15 | 0.23 |
| Alcoholic Anonymous Involvement | 1.29 | 1.20 | 1.37 | 1.68 | 1.56 | 1.80 | 1.25 | 1.13 | 1.38 | 1.07 | 0.94 | 1.20 | 1.13 | 1.00 | 1.26 |
| Suggestions to get help | 0.41 | 0.36 | 0.46 | 0.66 | 0.59 | 0.72 | 0.36 | 0.31 | 0.41 | 0.31 | 0.26 | 0.37 | 0.28 | 0.23 | 0.33 |
| Drinkers in social network | 0.31 | 0.11 | 0.50 | 0.45 | 0.32 | 0.58 | 0.28 | 0.16 | 0.40 | 0.14 | 0.10 | 0.18 | 0.31 | −0.02 | 0.63 |
| Neighborhood residents below poverty (%) | 12.59 | 11.81 | 13.38 | 12.47 | 11.66 | 13.29 | 13.05 | 12.17 | 13.92 | 12.92 | 12.05 | 13.80 | 12.86 | 11.90 | 13.81 |
| Bars and pubs within 1 mile | 4.64 | 3.54 | 5.74 | 3.92 | 2.88 | 4.95 | 5.52 | 3.99 | 7.04 | 5.19 | 3.71 | 6.66 | 5.18 | 3.29 | 7.06 |
| AA meetings each week within 10 miles | 151.14 | 137.75 | 164.54 | 141.75 | 127.13 | 156.37 | 195.15 | 174.91 | 215.39 | 192.10 | 171.70 | 212.49 | 206.59 | 183.77 | 229.41 |
| Inpatient treatment programs within 10 miles | 6.59 | 6.12 | 7.06 | 7.49 | 6.94 | 8.03 | 6.39 | 5.77 | 7.00 | 6.65 | 5.99 | 7.30 | 7.44 | 6.72 | 8.16 |
| Outpatient treatment programs within 10 miles | 11.48 | 10.91 | 12.05 | 11.41 | 10.77 | 12.06 | 10.06 | 9.39 | 10.73 | 10.33 | 9.40 | 11.25 | 12.25 | 11.16 | 13.34 |
| Time to nearest outpatient program (minutes) | 4.16 | 3.84 | 4.49 | 4.27 | 3.89 | 4.65 | 4.75 | 4.37 | 5.12 | 5.03 | 4.59 | 5.48 | 4.31 | 3.95 | 4.67 |
| Distance to nearest outpatient program (miles) | 2.12 | 1.94 | 2.30 | 2.16 | 1.95 | 2.37 | 2.44 | 2.23 | 2.65 | 2.70 | 2.42 | 2.98 | 2.21 | 2.01 | 2.41 |
| Time to nearest inpatient program (minutes) | 6.58 | 6.05 | 7.10 | 5.63 | 5.20 | 6.07 | 9.11 | 8.40 | 9.82 | 8.23 | 7.51 | 8.94 | 8.05 | 7.32 | 8.78 |
| Distance to nearest inpatient program (miles) | 3.67 | 3.32 | 4.02 | 3.02 | 2.74 | 3.29 | 5.33 | 4.84 | 5.81 | 4.90 | 4.39 | 5.41 | 4.72 | 4.22 | 5.23 |
At baseline, refers to 12 months prior to study enrollment.
LCL, lower confidence limit; UCL, upper confidence limit; CI, confidence interval.
Neighborhood variables were all time-varying, and they included the proportion of residents below poverty, number of bars and pubs within one mile of the respondent’s residence (representing approximately a 10-minute walk; this measure of density was more strongly related to the outcome than either the distance in miles or time in minutes to the nearest bar or pub), number of Alcoholics Anonymous (AA) meetings within 10 miles of the respondent’s residence (weekly meeting total tallied across all meeting sites), inpatient treatment availability (measured by the number of treatment programs within 10 miles of the respondent’s residence, the distance to nearest inpatient program in miles, and the time to the nearest inpatient program in minutes), and outpatient treatment availability (measured by the number of treatment programs within 10 miles of the respondent’s residence, the distance to nearest outpatient program in miles, and the time to the nearest outpatient program in minutes). We also tested a composite measure of neighborhood disadvantage (based on the proportion of residents without a high school diploma, proportion residents over age 16 in blue-collar jobs, percent with income below poverty and proportion without access to a car), as well as measures of off-premise alcohol availability (based on the number of liquor and convenience stores in proximity to the participants’ residential address), but these were not as informative as the measures of neighborhood poverty and on-premise alcohol availability (respectively), so they were dropped from further consideration.
Social network characteristics were heavy drinkers in the network (number of people who supported the respondent’s continued drinking at each wave, which was more strongly related to the outcome than the number of non-drinkers in the network, which was dropped from further consideration), AA involvement (this included meeting attendance and engagement with prescribed behaviors including doing service, having a sponsor, being a sponsor, and reading literature, with composite scores calculated for each wave), and suggestions to seek treatment (from medical, mental health, legal or social welfare service providers in the past 12 months, possible range = 0-4 at each wave). Other measures of pressure to get help—the number of friends and number of family members suggesting respondent seek treatment (coded as 0 compared with at least 1)—were less informative than suggestions from formal service providers, so they were dropped from further consideration.
Time-varying individual-level variables were drug and psychiatric co-morbidities (scores on the Addiction Severity Index or ASI67 for past 30-day drug severity and psychiatric severity at each wave) and receipt of treatment (from either a driving under the influence (DUI) program or alcohol or drug specialty treatment program in the past 12 months; at baseline, this referred to the year prior to the enrollment event). Time-invariant individual characteristics were collected at baseline, including the type of treatment program from which the respondent was recruited (detoxification, inpatient, or outpatient, used as referent), gender (female as referent), age (continuous), race/ethnicity (White compared to Black/African American, Hispanic/Latino, or other), educational attainment (less than high school and more than high school education, with high school diploma or equivalent as referent), marital status (married/partnered compared to all others who were separated/divorced, widowed, and never married), household income (greater than or equal to $25 000 compared to all others), and early onset of regular alcohol use (15% reported using alcohol 3 or more times per month by age 14, and 26% reported using alcohol 3 or more times per month by age 16).
Analysis
We used Mplus version 7.468 to generate latent class growth mixture models to depict trajectories of our outcome measure (count of dependence symptoms and social consequences) in the post-treatment period and to simultaneously determine predictors of class membership.69 In latent class growth analysis (LCGA), the mixture corresponds to different latent trajectory classes wherein no variation across individuals is allowed within classes, that is, the variance and covariance estimates for the growth factors within each class are assumed to be fixed to zero.70,71 The goal is to find classes that differ with respect to their average trajectories, with individual variation around each trajectory regarded as random error. We first fit a series of unconditional latent trajectory models (without covariates) to determine the number of classes that best fit our symptom count outcome. Goodness of fit was determined by comparing the AIC, BIC, and sample-size adjusted BIC indices (lower is better) across models, as well as entropy (>.80 desirable) and trajectory shapes and sizes.72-76 For these unconditional models, we used data from all 783 cases that had data at baseline and at least one follow-up interview, as the neighborhood-level covariates were not required.
We next fit a model wherein the four-class latent trajectory model was re-fit, now including auxiliary predictor variables. Predictors were allowed to influence the intercept and slope, as well as class membership. It was at this stage that we limited our analysis to the 722 cases that had neighborhood data for at least one follow-up interview. Candidate predictors of class membership were added individually or as conceptual blocks (eg, demographic covariates); those with predictive value were retained in a final model where all predictors were entered simultaneously in the regression model. A potential disadvantage of this approach is that the addition of auxiliary variables may affect the latent class formation, and some individuals may be assigned to a different class. If the classification changes dramatically when covariates are included, further analysis is suggested to determine reasons for changes in class membership.77,78 However, this was not the case with our analysis; the classification structure was similar for the unadjusted and adjusted models. All analyses were weighted to account for differential recruitment probability across the treatment program universe in the target county at baseline and to adjust for non-response and drop-out over time.
Results
Trajectory class structure
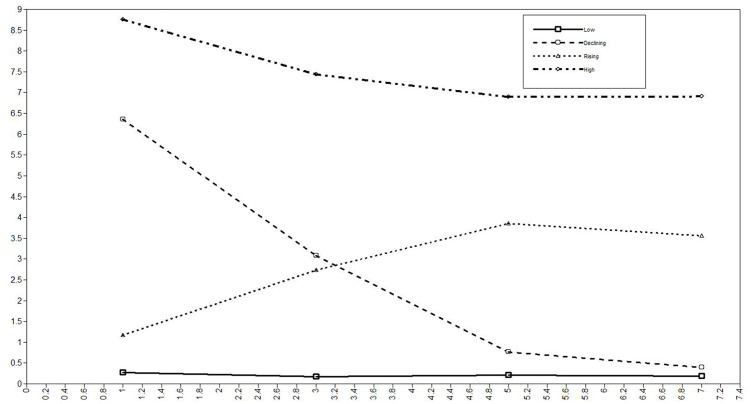
We determined that a 4-class solution provided the best fit and overall interpretation.76,79 Fit statistics for the unconditional models are displayed in Table 3. Entropy was good in all models. While the 5-class solution provided lower fit statistics, the 4-class solution provided a more parsimonious conceptual representation of the data. In particular, the 5-class solution would have divided the declining class into two smaller groups based on whether declines in alcohol dependence symptoms began three or five years after baseline. Figure 2 displays the unconditional class trajectories for the 4-class model.
Table 3.
Comparing class structure from unconditional LCGA models (N = 783 cases).
| Number of Classes | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| AIC | 17 960 | 12 866 | 11 964 | 11 310 | 10 974 |
| BIC | 17 974 | 12 898 | 12 016 | 11 379 | 11 062 |
| ABIC | 17 965 | 12 876 | 11 980 | 11 332 | 11 002 |
| Log likelihood | −8977 | −6426 | −5971 | −5640 | −5468 |
| Entropy | NA | .929 | .870 | .853 | .836 |
| LRT | NA | P < .05 | P < .05 | P > .05 | P > .05 |
AIC, Akaike information criterion; BIC, Bayesian information criterion; ABIC, adjusted Bayesian information criterion; LRT, Lo-Mendell-Rubin likelihood ratio test.
Figure 2.
Latent classes from 4-class unconditional LCGA models (sample mean scores for alcohol dependence symptoms at each follow-up interview). Proportions in each class: low = 38.5%; declining = 20.7%; rising = 20.5%; high = 20.3%.
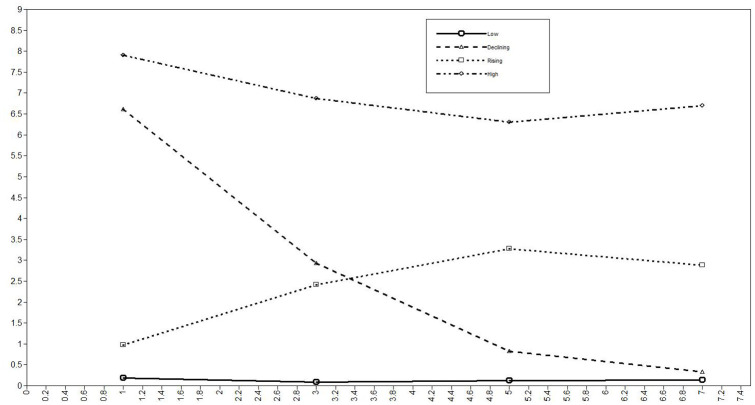
Table 4 displays information for the conditional 4-class model. Class sizes ranged from 19% to 34%. We labeled these as low (stable recovery; n = 249), rising (relapsing; n = 156), declining (late recovery; n = 137), and high (chronic; n = 172). See Figure 3. Entropy remained high and similar to that in the unconditional model.
Table 4.
Conditional 4-class model (N = 722 cases).
| Final Classification | Number of Cases (%) | Mean of the Class-membership Probabilities in Class (%) | Mean est. (SE) | Intercept (SE) | Slope (SE) | |||
|---|---|---|---|---|---|---|---|---|
| Class 1 | Class 2 | Class 3 | Class 4 | |||||
| Class 1 (low) | 249 (34.4) | .937 | .039 | .023 | .000 | .046 (.055) | −1.96 (.824) | −.36 (.496) |
| Class 2 (rising) | 165 (22.8) | .033 | .908 | .031 | .029 | −.087 (.036) | −1.69 (.580) | .95 (.263) |
| Class 3 (declining) | 137 (18.9) | .022 | .029 | .925 | .024 | −.022 (.033) | 1.61 (.338) | −.33 (.217) |
| Class 4 (high) | 172 (23.8) | .000 | .031 | .038 | .930 | .017 (.012) | 1.39 (.324) | −.12 (.100) |
| AIC = 9938; BIC = 10 396; ABIC = 10 078; entropy = .872 | ||||||||
Figure 3.
Latent classes from 4-class conditional LCGA models (sample mean scores for alcohol dependence symptoms at each follow-up interview).
Proportions in each class: low = 33.5%; declining = 19.9%; rising = 23.3%; high = 23.3%.
We found some movement of individuals between classes when covariates were included in the conditional joint model. Shapes of the four latent class trajectories, however, remained consistent across models. Compared with the unconditional model, intercept values and slopes varied slightly in the conditional model (see Table 5 notes). The number of drinkers in the social network, returning to treatment, early onset of regular alcohol use, and low levels of education were associated with trajectory intercepts, while neighborhood poverty, suggestions to get help and early onset were associated with trajectory slopes over time.
Table 5.
Associations of predictors with class membership.
| Class #1 (Low) as Referent | Class #2 (Rising) as Referent | Class #3 (Declining) as Referent | ||||
|---|---|---|---|---|---|---|
| Estimate (SE) | p-Value | Estimate (SE) | p-Value | Estimate (SE) | p-Value | |
| C#2 (rising) ON | ||||||
| Neighborhood poverty | 0.043(0.020) | .031 | ||||
| Bar/pub density | 0.040(0.023) | .084 | ||||
| Suggestions to get help | 1.406(0.690) | .042 | ||||
| AA involvement | −0.376(0.149) | .012 | ||||
| Drinkers in social network | 0.633(0.294) | .032 | ||||
| Returned to alcohol/drug treatment | 1.680(0.757) | .026 | ||||
| ASI psychiatric severity | 2.535(1.101) | .021 | ||||
| ASI drug severity | −2.823(4.097) | |||||
| Recruited from detoxification program | 0.771(0.513) | |||||
| Recruited from inpatient program | 0.363(0.362) | |||||
| Early onset of regular drinking | 0.200(0.368) | |||||
| Male gender | −0.216(0.325) | |||||
| Income above $25K | 0.238(0.333) | |||||
| Married/partnereda | 0.052(0.308) | |||||
| Less than high school | 0.550(0.412) | |||||
| More than high school | 0.037(0.355) | |||||
| Whitea | 0.341(0.346) | |||||
| C#3 (declining) ON | ||||||
| Neighborhood poverty | −0.004(0.025) | −0.047 (0.029) | ||||
| Bar/pub density | 0.055(0.024) | .020 | 0.014 (0.013) | |||
| Suggestions to get help | 2.563(0.537) | .000 | 1.157 (0.723) | |||
| AA involvement | −0.401(0.142) | .005 | −0.025 (0.172) | |||
| Drinkers in social network | −0.273(0.555) | −0.906 (0.481) | .060 | |||
| Returned to alcohol/drug treatment | 1.127(0.694) | −0.554 (0.803) | ||||
| ASI psychiatric severity | 0.153(1.516) | −2.382 (1.658) | ||||
| ASI drug severity | 2.293(4.627) | 5.117 (3.640) | ||||
| Recruited from detoxification program | 0.830(0.632) | 0.059 (0.734) | ||||
| Recruited from inpatient program | −0.535(0.404) | −0.897 (0.453) | .048 | |||
| Early onset of regular drinking | 0.576(0.396) | |||||
| Male gender | 0.489(0.370) | 0.705 (0.473) | ||||
| Income above $25K | −0.014(0.368) | −0.252 (0.385) | ||||
| Married/partnereda | 0.221(0.313) | 0.169 (0.386) | ||||
| Less than high school | 0.009(0.426) | −0.541 (0.543) | ||||
| More than high school | −0.192(0.379) | −0.229 (0.496) | ||||
| Whitea | 0.486(0.408) | 0.145 (0.496) | ||||
| C#4 (high) ON | ||||||
| Neighborhood poverty | 0.038(0.026) | −0.005 (0.025) | 0.042 (0.032) | |||
| Bar/pub density | 0.044(0.024) | .064 | 0.004 (0.013) | −0.011 (0.013) | ||
| Suggestions to get help | 3.303(0.914) | .000 | 1.898 (1.223) | 0.741 (0.807) | ||
| AA involvement | −0.751(0.216) | .001 | −0.375 (0.236) | −0.350 (0.210) | .095 | |
| Drinkers in social network | 0.706(0.294) | .016 | 0.073 (0.105) | 0.978 (0.483) | .043 | |
| Returned to alcohol/drug treatment | 2.061(1.025) | .044 | 0.381 (1.240) | 0.934 (0.891) | ||
| ASI psychiatric severity | 4.904(1.582) | .002 | 2.369 (1.658) | 4.751 (1.493) | ||
| ASI drug severity | 1.352(4.011) | 4.176 (2.784) | −0.941 (3.405) | |||
| Recruited from detoxification program | −0.157(0.756) | −0.928 (0.875) | −0.987 (0.733) | |||
| Recruited from inpatient program | −0.305(0.477) | −0.667 (0.453) | 0.230 (0.491) | |||
| Early onset of regular drinking | 0.410(0.443) | 0.209 (0.409) | −0.167 (0.388) | |||
| Male gender | 0.855(0.394) | .030 | 1.071 (0.419) | .011 | 0.366 (0.480) | |
| Income above $25K | 0.146(0.399) | −0.092 (0.389) | 0.160 (0.414) | |||
| Married/partnereda | −0.132(0.380) | −0.184 (0.410) | −0.353 (0.388) | |||
| Less than high school | −0.347(0.638) | −0.897 (0.783) | −0.356 (0.622) | |||
| More than high school | 0.079(0.470) | 0.042 (0.557) | 0.271 (0.426) | |||
| Whitea | −0.330(0.456) | −0.671 (0.500) | −0.353 (0.388) | |||
Compared to all others.
Notes: Auxiliary variables exerting influence on the latent trajectory intercept (Drinkers in social network, P = .061; Returned to treatment, P = .092; Early onset, P = .070; Less than high school education, P = .066) and slope (Neighborhood poverty, P = .008; Suggestions to get help, P = .086; Early onset, P = .007).
Predictors of class membership
Predictors of class membership are shown in Table 5. Compared to individuals in Class 1 (stable recovery, with low levels of alcohol dependence symptoms post-treatment), individuals in Class 2 (relapsing, with rising alcohol dependence symptoms post-treatment) lived in neighborhoods with higher levels of poverty, had more bars/pubs within one mile of their home (marginally significant), received more suggestions to go to treatment, were less involved in AA, had more heavy drinkers in their social network, returned to treatment, and had higher psychiatric severity. Compared to individuals in Class 1 (stable recovery/low symptoms), individuals in Class 3 (late recovery, with declining alcohol dependence symptoms post-treatment) had more bars/pubs near their homes, received more suggestions to go to treatment, and were less involved in AA, and compared to individuals in Class 2 (relapsing/rising symptoms), those in Class 3 (late recovery/declining) had marginally fewer drinkers in their social network and they were significantly less likely to be recruited from an inpatient program (compared to outpatient programs). Finally, compared to individuals in Class 1 (stable recovery/low symptoms), individuals in Class 4 (chronic, with high alcohol dependence symptoms post-treatment) had more bars/pubs near their homes (marginally significant), received more suggestions to go to treatment, were less involved in AA, had more drinkers in their social network, were more likely to return to treatment, had higher psychiatric severity, and were more likely to be male. Compared to individuals in Class 2 (relapsing/rising symptoms), those in Class 4 (chronic/high) were significantly more likely to be male, and compared to individuals in Class 3 (late recovery/declining) had marginally lower AA involvement and significantly more drinkers in their social network.
Table 6 presents values for the time-varying predictors for each trajectory class. At baseline, individuals in Class 1 (stable recovery/low) had the lowest number of dependence symptoms and those in Class 4 (chronic/high) had the highest number of dependence symptoms; those in Classes 1 (stable recovery/low) and 3 (late recovery/declining) had the lowest drug severity and the lowest number of drinkers in their social networks; and those in Class 1 (stable recovery/low) had the lowest psychiatric severity, received the fewest suggestions to get help, lived in neighborhoods with fewer residents below poverty and had fewer bars/pubs close to their home. As shown in Supplemental Table S1, the patterns of past 30-day abstinence and ASI alcohol severity scores followed similar patterns as the dependence symptoms measure across the four trajectory classes, suggesting validity of the classification.
Table 6.
Time-varying measures retained in latent class growth mixture model as predictive of class membership.
| Baseline | One year after Treatment | Three year follow-up | Five year follow-up | Seven year follow-up | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | LCL 95% CI | UCL 95% CI | Mean | LCL 95% CI | UCL 95% CI | Mean | LCL 95% CI | UCL 95% CI | Mean | LCL 95% CI | UCL 95% CI | Mean | LCL 95% CI | UCL 95% CI | |
| # Dependence symptoms (LCGA outcome) | |||||||||||||||
| Class 1 low | 4.0 | 3.4 | 4.5 | 0.2 | 0.1 | 0.2 | 0.1 | 0.0 | 0.1 | 0.1 | 0.1 | 0.2 | 0.1 | 0.1 | 0.2 |
| Class 2 rising | 5.3 | 4.6 | 6.0 | 0.8 | 0.6 | 1.0 | 2.6 | 2.1 | 3.1 | 3.5 | 2.9 | 4.1 | 2.8 | 2.1 | 3.4 |
| Class 3 declining | 6.5 | 5.7 | 7.2 | 6.4 | 5.7 | 7.1 | 2.8 | 2.0 | 3.5 | 0.8 | 0.4 | 1.2 | 0.3 | 0.2 | 0.5 |
| Class 4 high | 8.0 | 7.3 | 8.7 | 8.0 | 7.4 | 8.6 | 6.8 | 6.1 | 7.6 | 6.0 | 5.3 | 6.7 | 6.8 | 6.1 | 7.6 |
| ASI drug severity score | |||||||||||||||
| Class 1 low | 0.115 | 0.099 | 0.132 | 0.029 | 0.021 | 0.038 | 0.022 | 0.015 | 0.029 | 0.029 | 0.020 | 0.038 | 0.025 | 0.017 | 0.033 |
| Class 2 rising | 0.139 | 0.115 | 0.164 | 0.033 | 0.021 | 0.045 | 0.031 | 0.021 | 0.041 | 0.048 | 0.034 | 0.062 | 0.060 | 0.041 | 0.079 |
| Class 3 declining | 0.110 | 0.088 | 0.132 | 0.046 | 0.032 | 0.060 | 0.042 | 0.027 | 0.058 | 0.031 | 0.021 | 0.042 | 0.030 | 0.017 | 0.044 |
| Class 4 high | 0.135 | 0.115 | 0.156 | 0.080 | 0.062 | 0.097 | 0.074 | 0.054 | 0.094 | 0.080 | 0.060 | 0.101 | 0.081 | 0.064 | 0.099 |
| ASI psychiatric score | |||||||||||||||
| Class 1 low | 0.328 | 0.295 | 0.361 | 0.116 | 0.095 | 0.136 | 0.124 | 0.101 | 0.147 | 0.143 | 0.118 | 0.168 | 0.145 | 0.118 | 0.173 |
| Class 2 rising | 0.421 | 0.383 | 0.460 | 0.188 | 0.151 | 0.226 | 0.225 | 0.183 | 0.266 | 0.245 | 0.206 | 0.284 | 0.221 | 0.176 | 0.267 |
| Class 3 declining | 0.403 | 0.364 | 0.442 | 0.174 | 0.130 | 0.219 | 0.160 | 0.122 | 0.199 | 0.163 | 0.125 | 0.201 | 0.154 | 0.108 | 0.201 |
| Class 4 high | 0.455 | 0.416 | 0.494 | 0.348 | 0.309 | 0.386 | 0.333 | 0.289 | 0.376 | 0.361 | 0.321 | 0.401 | 0.342 | 0.300 | 0.385 |
| Suggestions to get help | |||||||||||||||
| Class 1 low | 0.27 | 0.20 | 0.35 | 0.36 | 0.28 | 0.44 | 0.14 | 0.09 | 0.19 | 0.10 | 0.06 | 0.14 | 0.10 | 0.05 | 0.15 |
| Class 2 rising | 0.55 | 0.41 | 0.70 | 0.58 | 0.45 | 0.71 | 0.27 | 0.19 | 0.35 | 0.33 | 0.23 | 0.43 | 0.24 | 0.14 | 0.35 |
| Class 3 declining | 0.43 | 0.30 | 0.57 | 0.93 | 0.77 | 1.09 | 0.42 | 0.27 | 0.56 | 0.28 | 0.18 | 0.39 | 0.29 | 0.16 | 0.43 |
| Class 4 high | 0.61 | 0.49 | 0.72 | 0.93 | 0.80 | 1.07 | 0.73 | 0.59 | 0.86 | 0.67 | 0.51 | 0.83 | 0.62 | 0.48 | 0.77 |
| Drinkers in social network | |||||||||||||||
| Class 1 low | 0.13 | 0.05 | 0.22 | 0.25 | 0.10 | 0.40 | 0.05 | 0.02 | 0.09 | 0.14 | 0.06 | 0.22 | 0.11 | 0.00 | 0.21 |
| Class 2 rising | 0.77 | −0.29 | 1.83 | 0.32 | 0.10 | 0.53 | 0.59 | 0.18 | 0.99 | 0.21 | 0.08 | 0.33 | 0.17 | 0.05 | 0.30 |
| Class 3 declining | 0.16 | 0.00 | 0.33 | 0.13 | 0.03 | 0.24 | 0.14 | 0.05 | 0.24 | 0.04 | 0.00 | 0.08 | 0.11 | 0.01 | 0.22 |
| Class 4 high | 0.50 | 0.15 | 0.85 | 1.12 | 0.68 | 1.57 | 0.46 | 0.13 | 0.78 | 0.14 | 0.06 | 0.21 | 0.95 | −0.57 | 2.47 |
| Went to treatment in past 12 months, proportion | |||||||||||||||
| Class 1 low | 0.61 | 0.55 | 0.67 | 0.28 | 0.21 | 0.34 | 0.12 | 0.08 | 0.16 | 0.10 | 0.05 | 0.14 | 0.09 | 0.05 | 0.13 |
| Class 2 rising | 0.66 | 0.58 | 0.74 | 0.38 | 0.29 | 0.47 | 0.31 | 0.22 | 0.39 | 0.23 | 0.14 | 0.31 | 0.24 | 0.16 | 0.33 |
| Class 3 declining | 0.74 | 0.66 | 0.82 | 0.50 | 0.40 | 0.60 | 0.34 | 0.24 | 0.45 | 0.21 | 0.12 | 0.29 | 0.16 | 0.08 | 0.25 |
| Class 4 high | 0.75 | 0.68 | 0.82 | 0.55 | 0.46 | 0.63 | 0.45 | 0.36 | 0.53 | 0.39 | 0.30 | 0.48 | 0.35 | 0.25 | 0.44 |
| Alcoholic anonymous involvement score | |||||||||||||||
| Class 1 low | 1.20 | 1.03 | 1.37 | 1.86 | 1.64 | 2.08 | 1.39 | 1.15 | 1.63 | 1.19 | 0.95 | 1.43 | 1.06 | 0.83 | 1.29 |
| Class 2 rising | 1.47 | 1.26 | 1.68 | 1.76 | 1.48 | 2.05 | 1.14 | 0.87 | 1.41 | 0.99 | 0.71 | 1.27 | 1.24 | 0.95 | 1.53 |
| Class 3 declining | 1.34 | 1.11 | 1.56 | 1.76 | 1.49 | 2.03 | 1.48 | 1.16 | 1.80 | 1.09 | 0.77 | 1.40 | 1.17 | 0.87 | 1.48 |
| Class 4 high | 1.36 | 1.16 | 1.56 | 1.45 | 1.23 | 1.68 | 1.19 | 0.94 | 1.44 | 1.11 | 0.84 | 1.37 | 1.27 | 1.02 | 1.53 |
| Neighborhood % below poverty | |||||||||||||||
| Class 1 low | 10.10 | 8.98 | 11.22 | 10.28 | 9.08 | 11.47 | 11.10 | 9.77 | 12.44 | 10.73 | 9.40 | 12.06 | 10.65 | 9.32 | 11.98 |
| Class 2 rising | 13.85 | 12.04 | 15.67 | 14.32 | 12.39 | 16.25 | 14.26 | 12.18 | 16.33 | 15.31 | 13.24 | 17.38 | 14.44 | 12.16 | 16.72 |
| Class 3 declining | 12.08 | 10.21 | 13.96 | 11.69 | 9.85 | 13.53 | 12.00 | 9.72 | 14.28 | 11.43 | 9.31 | 13.56 | 12.77 | 10.24 | 15.30 |
| Class 4 high | 14.10 | 12.35 | 15.84 | 14.28 | 12.34 | 16.22 | 15.43 | 13.65 | 17.20 | 15.32 | 13.49 | 17.16 | 15.32 | 13.15 | 17.49 |
| # Bars and pubs within 1 mi | |||||||||||||||
| Class 1 low | 2.35 | 1.98 | 2.71 | 3.35 | 1.41 | 5.30 | 2.57 | 2.15 | 3.00 | 2.50 | 1.95 | 3.06 | 2.47 | 1.87 | 3.07 |
| Class 2 rising | 3.33 | 2.73 | 3.94 | 3.13 | 2.53 | 3.74 | 4.62 | 2.73 | 6.51 | 6.89 | 2.48 | 11.30 | 4.73 | 1.40 | 8.06 |
| Class 3 declining | 6.01 | 2.27 | 9.76 | 5.83 | 1.97 | 9.68 | 6.68 | 1.63 | 11.74 | 4.86 | 1.35 | 8.37 | 9.98 | 1.43 | 18.53 |
| Class 4 high | 5.06 | 2.89 | 7.23 | 4.25 | 2.50 | 6.00 | 9.25 | 4.49 | 14.01 | 8.21 | 4.23 | 12.20 | 6.84 | 2.76 | 10.93 |
LCL, lower confidence limit; UCL, upper confidence limit; CI, confidence interval.
Discussion
We tested a socioecological model of relapse and recovery using latent class growth mixture modeling to identify predictors of longitudinal alcohol dependence trajectories among a large sample of problem drinkers recruited from substance use treatment programs. Based on the seven-year trajectories, we identified four classes. The groups characterized as Stable Recovery/Low (Class 1) and Relapsing/Rising (Class 2) both started with very few dependence symptoms (less than one) in the year after treatment, but the Relapsing/Rising class showed recurrence of problems by five years after treatment. The groups characterized as Late Recovery/Declining (Class 3) and Chronic/High (Class 4) both started with high levels of dependence symptoms (more than 6) in the year after treatment, but the Late Recovery/Declining class showed evidence of improvement by five years after treatment. Prior analyses of these data showed that respondents’ drinking patterns changed over time, and people either became non-problem drinkers or remained problem drinkers, rather than fluctuating between problem and non-problem drinking.53 Our findings add to our understanding of long-term outcomes of treatment clients, and these results may inform treatment planning in the future, particularly if they are substantiated by further studies in other diverse samples.
The neighborhood context (poverty and density of bars), social network characteristics (less AA involvement, continued affiliation with heavy drinkers), and individual predisposing (psychiatric severity) and need (returning to treatment) characteristics each distinguished individuals in the Relapsing/Rising class from individuals in the Stable Recovery/Low class. Social network characteristics (AA involvement and continued affiliation with heavy drinkers) were the primary distinguishing factors for individuals in the Chronic/High class compared to the Late Recovery/Declining class. Overall, the individuals in the Stable Recovery/Low class lived in neighborhoods that could better support recovery (fewer residents below poverty and fewer bars/pubs), were in social networks that could help prevent relapse (lowest number of drinkers), and had fewer indicators of complex treatment needs (lowest drug severity, lowest psychiatric severity). Similarly, the individuals in the Late Recovery/Declining class also were in social networks with fewer drinkers, and they had lower drug severity. These results suggest that, particularly for treatment clients living in high-risk neighborhoods, supportive social networks are important to long-term recovery, reiterating earlier findings from an outpatient treatment subsample.58 Although most treatment programs work to actively engage clients with recovery support resources such as AA after treatment,80-82 it is less common that programs address neighborhood risk factors for relapse. Neighborhood-based delivery of services and community-based recovery support systems are key elements in recovery-oriented systems of care to prevent relapse.11 Without support and engagement in these comprehensive care systems, it is unlikely that clients will be able to make substantial changes in their neighborhood environments on their own.83
The individuals in the Chronic/High class were the most complex in terms of co-morbidities (use of other drugs, psychiatric problems), but they also continued to be involved with heavy-drinking social networks and they lived in high-risk neighborhoods. Although they continued to receive suggestions that they should seek help and they repeatedly re-engaged with the treatment system, their levels of dependence symptoms remained high over time. Without ongoing support to address the neighborhood and social network factors that contribute to alcohol problems, these high-need clients are likely to continue to experience significant symptoms of alcohol dependence for many years, as other studies have shown a strong relationship between serious psychiatric problems and drug use for people living in poverty.84 Despite evidence of effectiveness,85-87 wraparound services, including housing support and other strategies to build recovery capital, are not commonly integrated into drug and alcohol treatment.88 These services may help the most complex and chronic patients recover from their alcohol and other drug problems.
Study strengths and limitations
Our study is unique in the longitudinal coverage of alcohol dependence symptoms for seven years after treatment intake. Capitalizing on the large sample, we examined predictors of alcohol problems at the individual, social network, and neighborhood levels, which is another strength of our analysis. However, the results should be interpreted taking some limitations into account. First, we focused on one outcome (alcohol problems in the years after treatment), so further research is needed to examine how neighborhoods and social networks might influence other aspects of successful recovery from alcohol (and drug) problems,89 including mental and physical well-being, developing a sense of purpose and enhancing quality of life, which were not an explicit focus here. There also are some limitations to using the ASI67 to measure drug and psychiatric co-morbidities. For example, although the psychiatric composite score has shown generally high internal consistency across studies, indicators of reliability are lower for the drug composite score, and in some samples, the specificity of the psychiatric score is lower than acceptable.90 Future work could use more detailed measures of mental health co-morbidities to build on our findings. Finally, latent class growth mixture modeling has some noted limitations as well,91 such as an inability to account for within-class variability and a tendency to over-extract mean trajectories with non-normal outcomes.92,93 Thus, our results suggesting that people experience different recovery and relapse trajectories after entering alcohol treatment should be interpreted within these analytic limitations, and future studies should use complementary methods to validate our findings. Qualitative research on elements of recovery among people from these different problem drinking groups over time would be particularly informative.
Implications
Despite the aforementioned limitations, our study has practical implications for prevention. Based on the identified risk factors for continued alcohol problems after treatment (exemplified by those in the Chronic/High class) as well as risk factors for relapse after a period of remission (exemplified by those in the Rising/Relapsing class), priorities for intervention should be to increase AA involvement and decrease the number of drinkers in people’s social networks and to provide services to address psychiatric comorbidities. Additionally, to reduce the risk of relapse, it also may be important to include supportive housing services or poverty reduction strategies to accompany treatment programming. Finally, reductions in local bar density or specialized interventions to help clients manage environmental triggers in their home neighborhoods after treatment also may increase the likelihood of long-term recovery.
Study results also can guide development of effective community-level interventions designed to improve the social and physical environment, which may have synergistic effects that enhance the success of formal substance use disorder treatment.94 Findings also suggest different intervention approaches may be helpful in high-risk neighborhoods. In terms of treatment, understanding how neighborhoods contribute to alcohol problems after treatment could help health providers and clients become more effective in setting realistic treatment goals and expectations. This also could inform individual treatment planning by identifying and developing strategies to cope with potential neighborhood triggers for relapse. A housing mobility study95 found women who moved from high-poverty neighborhoods to public housing in middle-class neighborhoods often developed new social networks, which is an important step in the recovery process from alcohol problems.48-51
Our evidence about neighborhood triggers for relapse and buffering factors that support recovery can be used by treatment professionals to assist patients as they return home after treatment. Providers could integrate support services for people who want to move to a neighborhood that will support their recovery process, and incentives or ancillary programs could be provided to facilitate housing changes by clients with limited financial resources. We also identified potentially modifiable factors (social network support for sobriety, participation in self-help) that may reduce negative consequences among problem and dependent drinkers who remain in high-risk neighborhoods. Effective interventions such as Making Alcoholics Anonymous Easier (MAAEZ)96 exist to facilitate participation in self-help groups; these could be implemented with treatment programs serving clients from high-risk neighborhoods. Finally, findings will contribute to ongoing discussions about new and continued licensing of alcohol outlets and regulation of alcohol sales to prevent alcohol problems in high-risk areas and among high-risk people.27
Supplemental Material
Supplemental material, SAT933631_Supplemental_Material_CLN for Testing a Socioecological Model of Relapse and Recovery from Alcohol Problems by Katherine J Karriker-Jaffe, Jane Witbrodt, Amy A Mericle, Douglas L Polcin and Lee Ann Kaskutas in Substance Abuse: Research and Treatment
Acknowledgments
The authors would like to thank Ms. Shalika Gupta for assistance with geocoding and Drs. Kevin Delucchi and Libo Li for feedback on the analysis strategy.
Footnotes
Funding:The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the US National Institutes of Health’s National Institute on Alcohol Abuse and Alcoholism (NIAAA) under Grant R01AA020328, with writing further supported by the National Institute on Drug Abuse (NIDA) under Grant R01DA042938. The original longitudinal study was supported by NIAAA under Grants R01AA09750, P50AA005595, and R01AA015927. The NIAAA and NIDA had no role in the study design; collection, analysis or interpretation of the data; writing the manuscript; or the decision to submit the paper for publication.
Declaration of conflicting interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: KKJ-J contributed to funding acquisition, data curation, conceptualization, data interpretation, and writing the original draft. JW contributed to conceptualization, formal analysis, data interpretation, and writing the original draft. AAM contributed to data interpretation and writing (review and editing). DLP contributed to data interpretation and writing (review and editing). LAK contributed to funding acquisition, conceptualization, data interpretation and writing (review and editing). All authors materially participated in the work and have approved the final manuscript.
ORCID iD: Katherine J Karriker-Jaffe  https://orcid.org/0000-0002-2019-0222
https://orcid.org/0000-0002-2019-0222
Supplemental material: Supplemental material for this article is available online.
References
- 1. White WL, Boyle M, Loveland D. Alcoholism/addiction as a chronic disease: from rhetoric to clinical reality. Alcohol Treat Q. 2002;20:107–129. [Google Scholar]
- 2. Kaskutas LA, Borkman TJ, Laudet A, et al. Elements that define recovery: the experiential perspective. J Stud Alcohol Drugs. 2014;75:999–1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kelly JF, Hoeppner B. A biaxial formulation of the recovery construct. Addict Res Theory. 2015;23:5–9. [Google Scholar]
- 4. U.S. Department of Health and Human Services, Office of the Surgeon General. Facing addiction in America: the Surgeon General’s report on alcohol, drugs, and health. WebCite®. Washington, DC, November 2016. http://www.webcitation.org/6onCCszJk. Accessed July 3, 2017. [PubMed] [Google Scholar]
- 5. Ashford RD, Brown A, Brown T, et al. Defining and operationalizing the phenomena of recovery: a working definition from the recovery science research collaborative. Addict Res Theory. 2019;27:179–188. [Google Scholar]
- 6. Marlatt GA, Witkiewitz K. Relapse prevention for alcohol and drug problems. In: Marlatt GA, Donovan DM. (eds) Relapse Prevention: Maintenance Strategies in the Treatment of Addictive Behaviors. 2nd ed. New York: The Guilford Press; 2005:1–44. [Google Scholar]
- 7. Gruenewald PJ, Holder HD, Treno AJ. Environmental approaches to prevention. In: Graham AW, Schultz TK, Mayo-Smith MF, Ries RK, Wilford BB. (eds) Principles of Addiction Medicine. 3rd ed. Chevy Chase, MD: American Society of Addiction Medicine, Inc.; 2003:383–394. [Google Scholar]
- 8. Holder HD. Alcohol and the Community: A Systems Approach to Prevention. New York: Cambridge University Press; 1999. [Google Scholar]
- 9. Thomas YF. The social epidemiology of drug abuse. Am J Prev Med. 2007;32(suppl 6):S141–S146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rose G. Sick individuals and sick populations. Int J Epidemiol. 1985;14:31–38. [DOI] [PubMed] [Google Scholar]
- 11. Sheedy CK, Whitter M. Guiding Principles and Elements of Recovery-Oriented Systems of Care: what do we know from the research? (HHS Publication No. (SMA) 09-4439). Rockville, MD: Center for Substance Abuse Treatment, Substance Abuse and Mental Health Services Administration; August 2009. WebCite®. http://www.webcitation.org/6YDADCmUP. Accessed: May 1, 2015. [Google Scholar]
- 12. White WL, Kurtz E, Sanders M. (eds). Recovery Management. Chicago, IL: Great Lakes Addiction Technology Transfer Center; (ATTC) Network; 2006. [Google Scholar]
- 13. Galea S, Nandi A, Vlahov D. The social epidemiology of substance abuse. Epidemiol Rev. 2004;26:36–52. [DOI] [PubMed] [Google Scholar]
- 14. Stimpson JP, Ju H, Raji MA, Eschbach K. Neighborhood deprivation and health risk behaviors in NHANES III. Am J Health Behav. 2007;31:215–222. [DOI] [PubMed] [Google Scholar]
- 15. Karriker-Jaffe KJ, Zemore SE, Mulia N, Jones-Webb R, Bond J, Greenfield TK. Neighborhood disadvantage and adult alcohol outcomes: differential risk by race and gender. J Stud Alcohol Drugs. 2012;73:865–873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Jones-Webb R, Snowden L, Herd D, Short B, Hannan P. Alcohol-related problems among black, Hispanic, and white men: the contribution of neighborhood poverty. J Stud Alcohol. 1997;58:539–545. [DOI] [PubMed] [Google Scholar]
- 17. Karriker-Jaffe K, Liu H, Kaplan LM. Understanding associations between neighborhood socioeconomic status and negative consequences of drinking: a moderated mediation analysis. Prev Sci. 2016;17:513–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Jones-Webb RJ, Karriker-Jaffe KJ. Neighborhood disadvantage, high alcohol content beverage consumption, drinking norms, and consequences: a mediation analysis. J Urban Health. 2013;90:667–684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Buu A, Mansour M, Wang J, Refior SK, Fitzgerald HE, Zucker RA. Alcoholism effects on social migration and neighborhood effects on alcoholism over the course of 12 years. Alcohol Clin Exp Res. 2007;31:1545–1551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Karriker-Jaffe KJ, Ohlsson H, Kendler KS, Cook WK, Sundquist K. Alcohol availability and onset and recurrence of alcohol use disorder: examination in a longitudinal cohort with cosibling analysis. Alcohol Clin Exp Res. 2018;42:1105–1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ferrari JR, Jason LA, Blake R, Davis MI, Olson BD. ‘This is my neighborhood’: comparing United States and Australian Oxford House neighborhoods. J Prev Interv Community. 2006;31:41–49. [DOI] [PubMed] [Google Scholar]
- 22. Jacobson JO. Place and attrition from substance abuse treatment. J Drug Issues. 2004;34:23–50. [Google Scholar]
- 23. Lambert SF, Brown TL, Phillips CM, Ialongo NS. The relationship between perceptions of neighborhood characteristics and substance use among urban African American adolescents. Am J Community Psychol. 2004;34:205–218. [DOI] [PubMed] [Google Scholar]
- 24. Kadushin C, Reber E, Saxe L, Livert D. The substance use system: social and neighborhood environments associated with substance use and misuse. Subst Use Misuse. 1998;33:1681–1710. [DOI] [PubMed] [Google Scholar]
- 25. Bradizza CM, Stasiewicz PR. Qualitative analysis of high-risk drug and alcohol use situations among severly mentally ill substance abusers. Addict Behav. 2003;28:157–168. [DOI] [PubMed] [Google Scholar]
- 26. Gruenewald PJ, Ponicki WR, Holder HD. The relationship of outlet densities to alcohol consumption: a time series cross-sectional analysis. Alcohol Clin Exp Res. 1993;17:38–47. [DOI] [PubMed] [Google Scholar]
- 27. Gruenewald PJ. The spatial ecology of alcohol problems: niche theory and assortative drinking. Addiction. 2007;102:870–878. [DOI] [PubMed] [Google Scholar]
- 28. Treno AJ, Grube JW, Martin SE. Alcohol availability as a predictor of youth drinking and driving: a hierarchical analysis of survey and archival data. Alcohol Clin Exp Res. 2003;27:835–840. [DOI] [PubMed] [Google Scholar]
- 29. Theall KP, Scribner R, Cohen D, et al. The neighborhood alcohol environment and alcohol-related morbidity. Alcohol Alcohol. 2009;44:491–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Branas CC, Elliott MR, Richmond TS, Culhane DP, Wiebe DJ. Alcohol consumption, alcohol outlets, and the risk of being assaulted with a gun. Alcohol Clin Exp Res. 2009;33:906–915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Gruenewald PJ, Remer LG, Treno AJ. Alcohol outlets, crime, and disorder in the United States of America. In: Hadfield P. (ed.) Nightlife and Crime: Social Order and Governance in International Perspective. New York: Oxford University Press; 2009:195–206. [Google Scholar]
- 32. Karvonen S, Rimpelä AH. Urban small area variation in adolescents’ health behaviour. Soc Sci Med. 1997;45:1089–1098. [DOI] [PubMed] [Google Scholar]
- 33. Karriker-Jaffe KJ, Au V, Frendo M, Mericle AA. Offsetting the effects of neighborhood disadvantage on problem drinking. J Community Psychol. 2017;45:678–684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Mulia N, Ye Y, Greenfield TK, Zemore SE. Disparities in alcohol-related problems among white, black, and Hispanic Americans. Alcohol Clin Exp Res. 2009;33:654–662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Carra G, Crocamo C, Borrelli P, et al. Area-level deprivation and adverse consequences in people with substance use disorders: findings from the psychiatric and addictive dual disorder in Italy (PADDI) study. Subst Use Misuse. 2017;52:451–458. [DOI] [PubMed] [Google Scholar]
- 36. Lindrooth RC, Lo Sasso AT, Lurie IZ. The effect of distance to provider on employee response to change in mental health benefits. Health Econ. 2006;15:1133–1141. [DOI] [PubMed] [Google Scholar]
- 37. Fortney J, Rost K, Zhang M, Warren J. The impact of geographic accessibility on the intensity and quality of depression treatment. Med Care. 1999;37:884–893. [DOI] [PubMed] [Google Scholar]
- 38. Beardsley K, Wish ED, Fitzelle DB, O'Grady K, Arria AM. Distance traveled to outpatient drug treatment and client retention. J Subst Abuse Treat. 2003;25:279–285. [DOI] [PubMed] [Google Scholar]
- 39. Fortney JC, Booth BM, Blow FC, Bunn JY, Cook CAL. The effects of travel barriers and age on the utilization of alcoholism treatment aftercare. Am J Drug Alcohol Abuse. 1995;21:391–406. [DOI] [PubMed] [Google Scholar]
- 40. Schmitt SK, Phibbs CS, Piette JD. The influence of distance on utilization of outpatient mental health aftercare following inpatient substance abuse treatment. Addict Behav. 2003;28:1183–1192. [DOI] [PubMed] [Google Scholar]
- 41. Kaskutas LA, Turk N, Bond J, Weisner C. The role of religion, spirituality and alcoholics anonymous in sustained sobriety. Alcohol Treat Q. 2003;21:1–16. [Google Scholar]
- 42. Roland EJ, Kaskutas LA. Alcoholics Anonymous and church involvement as predictors of sobriety among three ethnic treatment populations. Alcohol Treat Q. 2002;20:61–77. [Google Scholar]
- 43. Kaskutas LA, Bond J, Humphreys K. Social networks as mediators of the effect of alcoholics anonymous. Addiction. 2002;97:891–900. [DOI] [PubMed] [Google Scholar]
- 44. Bond J, Kaskutas LA, Weisner C. The persistent influence of social networks and alcoholics anonymous on abstinence. J Stud Alcohol. 2003;64:579–588. [DOI] [PubMed] [Google Scholar]
- 45. Kaskutas LA, Ammon L, Delucchi K, Room R, Bond J, Weisner C. Alcoholics anonymous careers: patterns of AA involvement five years after treatment entry. Alcohol Clin Exp Res. 2005;29:1983–1990. [DOI] [PubMed] [Google Scholar]
- 46. Kaskutas LA, Bond J, Avalos LA. 7-year trajectories of alcoholics anonymous attendance and associations with treatment. Addict Behav. 2009;34:1029–1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Mankowski ES, Humphreys K, Moos RH. Individual and contextual predictors of involvement in twelve-step self-help groups after substance abuse treatment. Am J Community Psychol. 2001;29:537–563. [DOI] [PubMed] [Google Scholar]
- 48. Weisner C, Delucchi K, Matzger H, Schmidt L. The role of community services and informal support on five-year drinking trajectories of alcohol dependent and problem drinkers. J Stud Alcohol. 2003;64:862–873. [DOI] [PubMed] [Google Scholar]
- 49. Matzger H, Delucchi K, Weisner C, Ammon L. Does marital status predict long-term drinking? Five-year observations of dependent and problem drinkers. J Stud Alcohol. 2004;65:255–265. [DOI] [PubMed] [Google Scholar]
- 50. Ammon L, Bond J, Matzger H, Weisner C. Gender differences in the relationship of community services and informal support to seven-year drinking trajectories of alcohol-dependent and problem drinkers. J Stud Alcohol Drugs. 2008;69:140–150. [DOI] [PubMed] [Google Scholar]
- 51. Delucchi KL, Matzger H, Weisner C. Dependent and problem drinking over 5 years: a latent class growth analysis. Drug Alcohol Depend. 2004;74:235–244. [DOI] [PubMed] [Google Scholar]
- 52. Weisner C, Matzger H, Kaskutas LA. How important is treatment? One-year outcomes of treated and untreated alcohol-dependent individuals. Addiction. 2003;98:901–911. [DOI] [PubMed] [Google Scholar]
- 53. Delucchi KL, Weisner C. Transitioning into and out of problem drinking across seven years. J Stud Alcohol Drugs. 2010;71:210–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Delucchi KL, Matzger H, Weisner C. Alcohol in emerging adulthood: 7-year study of problem and dependent drinkers. Addict Behav. 2008;33:134–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Witkiewitz K, Marlatt GA. Relapse prevention for alcohol and drug problems: that was Zen, this is Tao. Am Psychol. 2004;59:224–235. [DOI] [PubMed] [Google Scholar]
- 56. Witkiewitz K, Marlatt GA. Modeling the complexity of post-treatment drinking: it’s a rocky road to relapse. Clin Psychol Rev. 2007;27:724–738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Tucker JA, Vuchinich RE, Gladsjo JA. Environmental influences on relapse in substance use disorders. Int J Addict. 1991;25(S7–S8):1017–1050. [DOI] [PubMed] [Google Scholar]
- 58. Mericle AA, Kaskutas LA, Polcin DL, Karriker-Jaffe KJ. Independent and interactive effects of neighborhood disadvantage and social network characteristics on problem drinking after treatment. J Soc Clin Psychol. 2018;37:1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Aday LA, Andersen R. A framework for the study of access to medical care. Health Serv Res. 1974;9:208–220. [PMC free article] [PubMed] [Google Scholar]
- 60. Weisner C, Matzger H. A prospective study of the factors influencing entry to alcohol and drug treatment. J Behav Health Serv Res. 2002;29:126–137. [DOI] [PubMed] [Google Scholar]
- 61. Weisner C, Matzger H, Tam T, Schmidt L. Who goes to alcohol and drug treatment? Understanding utilization within the context of insurance. J Stud Alcohol. 2002;63:673–682. [DOI] [PubMed] [Google Scholar]
- 62. Moos RH, Moos BS. Rates and predictors of relapse after natural and treated remission from alcohol use disorders. Addiction. 2006;101:212–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Grella CE, Scott CK, Foss MA, Dennis ML. Gender similarities and differences in the treatment, relapse, and recovery cycle. Eval Rev. 2008;32:113–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Matzger H, Weisner C. Nonmedical use of prescription drugs among a longitudinal sample of dependent and problem drinkers. Drug Alcohol Depend. 2007;86:222–229. [DOI] [PubMed] [Google Scholar]
- 65. Delucchi K, Kaskutas LA. Following problem drinkers over eleven years: understanding changes in alcohol consumption. J Stud Alcohol Drugs. 2010;71:831–836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5). Washington, DC: American Psychiatric Publishing, Incorporated; 2013. [Google Scholar]
- 67. McLellan AT. Addiction severity index (ASI). In: Rush AJ, Jr, Pincus HA, Jr, First MB, et al. (eds) Handbook of Psychiatric Measures. Washington, DC: American Psychiatric Association; 2000:472–474. [Google Scholar]
- 68. Mplus Version 7.4 [computer program]. Los Angeles, CA: Muthén & Muthén; 2015. [Google Scholar]
- 69. Clark SL, Muthén B. Relating latent class analysis results to variables not included in the analysis, 2009. https://www.statmodel.com/download/relatinglca.pdf
- 70. Nagin DS. Analyzing developmental trajectories: a semiparametric, group-based approach. Psychol Methods. 1999;4:139–157. [DOI] [PubMed] [Google Scholar]
- 71. Mplus Version 5 [computer program]. Los Angeles, CA: Muthén & Muthén; 2007. [Google Scholar]
- 72. Akaike H. A new look at the statistical model identification. IEEE Trans Autom Control. 1974; 19:716–723. [Google Scholar]
- 73. Schwartz G. Estimating the dimension of a model. Ann Stat. 1978;6:461–464. [Google Scholar]
- 74. Sclove SL. Application of model-selection criteria to some problems in multivariate-analysis. Psychometrika. 1987;52:333–343. [Google Scholar]
- 75. Tofighi D, Enders CK. Identifying the correct number of classes in growth mixture models. In: Hancock GR, Samuelsen KM. (eds) Advances in Latent Variable Mixture Models. Charlotte: Information Age Publishing; 2008:317–341. [Google Scholar]
- 76. Wickrama KAS, Lee TK, O'Neal CW, Lorenz FO. Higher-Order Growth Curves and Mixture Modeling With Mplus: A Practical Guide. New York, NY: Routledge; 2016. [Google Scholar]
- 77. Asparouhov T, Muthén B. Auxiliary variables in mixture modeling: three-step approaches using Mplus. Struct Equ Model. 2014;21:329–341. [Google Scholar]
- 78. Bray BC, Lanza ST, Tan X. Eliminating bias in classify-analyze approaches for latent class analysis. Struct Equ Model. 2014;22:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Jung T, Wickrama KAS. An introduction to latent class growth analysis and growth mixture modeling. Soc Personal Psychol Compass. 2008;2:302–317. [Google Scholar]
- 80. Finney JW, Moos RH. The effectiveness of inpatient and outpatient treatment for alcohol abuse: effect sizes, research design issues and explanatory mechanisms. Addiction. 1996;91:1813–1820. [PubMed] [Google Scholar]
- 81. Thomassen L. AA utilization after introduction in outpatient treatment. Subst Use Misuse. 2002;37:239–253. [DOI] [PubMed] [Google Scholar]
- 82. Gossop M, Harris J, Best D, et al. Is attendance at alcoholics anonymous meetings after inpatient treatment related to improved outcomes? A 6-month follow-up study. Alcohol Alcohol. 2003;38:421–426. [DOI] [PubMed] [Google Scholar]
- 83. Karriker-Jaffe KJ, Witbrodt J, Subbaraman MS, Kaskutas LA. What happens after treatment? Long-term effects of continued substance use, psychiatric problems and help-seeking on social status of alcohol-dependent individuals. Alcohol Alcohol. 2018;53:394–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Carra G, Bartoli F, Riboldi I, Trotta G, Crocamo C. Poverty matters: cannabis use among people with serious mental illness: findings from the United States survey on drug use and health, 2015. Int J Soc Psychiatry. 2018;64:656–659. [DOI] [PubMed] [Google Scholar]
- 85. McLellan AT, Hagan TA, Levine M, et al. Supplemental social services improve outcomes in public addiction treatment. Addiction. 1998;93:1489–1499. [DOI] [PubMed] [Google Scholar]
- 86. Milby JB, Schumacher JE, Raczynski JM, et al. Sufficient conditions for effective treatment of substance abusing homeless persons. Drug Alcohol Depend. 1996;43:39–47. [DOI] [PubMed] [Google Scholar]
- 87. Institute of Medicine. Broadening the Base of Treatment for Alcohol Problems. Washington, DC: National Academy Press; 1990. [PubMed] [Google Scholar]
- 88. Paino M, Aletraris L, Roman P. The relationship between client characteristics and wraparound services in substance use disorder treatment centers. J Stud Alcohol Drugs. 2016;77:160–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Kelly JF, Abry AW, Milligan CM, Bergman BG, Hoeppner BB. On being “in recovery”: a national study of prevalence and correlates of adopting or not adopting a recovery identity among individuals resolving drug and alcohol problems. Psychol Addict Behav. 2018;32:595–604. [DOI] [PubMed] [Google Scholar]
- 90. Mäkelä K. Studies of the reliability and validity of the addiction severity index. Addiction. 2004;99:398–410. [DOI] [PubMed] [Google Scholar]
- 91. Sher KJ, Jackson KM, Steinley D. Alcohol use trajectories and the ubiquitous cat’s cradle: cause for concern? J Abnorm Psychol. 2011;120:322–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Bauer DJ, Curran PJ. Distributional assumptions of growth mixture models: implications for overextraction of latent trajectory classes. Psychol Methods. 2003;8:338–363. [DOI] [PubMed] [Google Scholar]
- 93. Guerra-Pena K, Steinley D. Extracting spurious latent classes in growth mixture modeling with nonnormal errors. Educ Psychol Meas. 2016;76:933–953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Sánchez F, Wang X, Castillo-Chávez C, Gorman DM, Gruenewald PJ. Drinking as an epidemic: a simple mathematical model with recovery and relapse. In: Witkiewitz K, Marlatt GA. (eds) Therapists’ guide to evidence-based relapse prevention. Boston, MA: Elsevier, Inc.; 2007:353–368. [Google Scholar]
- 95. Fauth RC, Leventhal T, Brooks-Gunn J. Short-term effects of moving from public housing in poor to middle-class neighborhoods on low-income, minority adults’ outcomes. Soc Sci Med. 2004;59:2271–2284. [DOI] [PubMed] [Google Scholar]
- 96. Kaskutas LA, Subbaraman MS, Witbrodt J, Zemore SE. Effectiveness of making alcoholics anonymous easier: a group format 12-step facilitation approach. J Subst Abuse Treat. 2009;37:228–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, SAT933631_Supplemental_Material_CLN for Testing a Socioecological Model of Relapse and Recovery from Alcohol Problems by Katherine J Karriker-Jaffe, Jane Witbrodt, Amy A Mericle, Douglas L Polcin and Lee Ann Kaskutas in Substance Abuse: Research and Treatment