Abstract
Chronic alcohol misuse can result in chronically elevated interleukin (IL)-6, a pro-inflammatory cytokine, in the bloodstream. Given that Mindfulness-Based Relapse Prevention (MBRP) has been shown to reduce alcohol misuse, MBRP might also be effective in reducing IL-6 concentrations. Past research has found, however, that IL-6 does not respond consistently to mindfulness-based interventions. Building on prior studies, we examined whether between-person variability in engagement with mindfulness training (i.e., formal mindfulness practice time) is associated with between-person variability in changes in serum IL-6, using data from a randomized controlled trial evaluating MBRP for Alcohol Dependence (MBRP-A). Participants were 72 alcohol dependent adults (mean age = 43.4 years, 63.9% male, 93.1% White) who received a minimum dose (i.e., at least four sessions) of MBRP-A either at the start of the trial (n=46) or after a 26-week delay (n=26). IL-6 concentrations did not significantly change from pre- to post-intervention for the full sample. Nevertheless, greater mindfulness practice time was significantly associated with reduced IL-6 levels (r = −.27). The association between practice time and IL-6 changes remained significant when controlling for intervention timing (i.e., immediate or after the 26-week delay), demographic characteristics, and changes in mindful awareness, obsessive-compulsive drinking, and depressive symptoms. The association between practice time and IL-6 changes was not significant when omitting the minimum treatment dose requirement. Overall, results suggest that the level of engagement in mindfulness training may predict changes in the inflammatory pathophysiology in adults with alcohol dependence.
Keywords: alcohol, mindfulness, meditation, inflammation, interleukin-6
Introduction
Alcohol use disorder (AUD) is among the most prevalent psychiatric disorders, with a 12-month prevalence of about 6% among U.S. adults (Substance Abuse and Mental Health Services Administration, 2018). AUD is highly disabling (Hasin, Stinson, Ogburn, & Grant, 2007) and burdensome on society (Rehm et al., 2009) and has been shown to be causally related to more than 60 different medical conditions, including cardiovascular and gastrointestinal diseases and some cancers (Room, Babor, & Rehm, 2005). According to epidemiological research, AUD accounts for about 3% of adult deaths in the United States (Rehm et al., 2014).
Other lines of work have shown that alcohol is also a potent modulator of the immune system and inflammatory physiology (Neupane, 2016). The prevailing mechanistic explanation is that chronic heavy drinking increases intestinal permeability and circulation of lipopolysaccharides, which stimulate immune cells such as monocytes, macrophages, and T lymphocytes to release pro-inflammatory cytokines, particularly interleukin (IL)-6, which in turn impact multiple organ systems (Neupane, 2016). Over time, high levels of IL-6 may be harmful to these organs, including the liver. There is evidence that chronically elevated IL-6 increases risk for hepatic disease (Achur et al., 2010; Cohen, Horton, & Hobbs, 2011), coronary heart disease (Danesh et al., 2008), some cancers (Grivennikov & Karin, 2011), and premature death (Wassel, Barrett-Connor, & Laughlin, 2010). Wassel et al. (2010) found that each standard deviation increase in serum IL-6 levels is associated with about a 1-year reduction in lifespan.
Research has demonstrated that individuals with AUD present with elevated IL-6 concentrations in the blood as well as persistent inflammatory activity relative to control subjects (Achur, Freeman, & Vrana, 2010; Leclercq et al., 2012, Yen et al., 2017). IL-6 has also been found to be elevated in alcohol-induced liver disease (Achur, Freeman, & Vrana, 2010). Given the existing literature, some researchers have proposed using IL-6 and other cytokines as bioindicators of AUD and alcohol-induced tissue damage (Achur et al., 2010).
Fortunately, plasma IL-6 levels appear to decline after as little as four weeks of alcohol abstinence (Yen et al., 2017). Therefore, the successful treatment of AUD may reduce IL-6 levels and associated inflammation and could conceivably help mitigate alcohol-induced tissue damage. Accordingly, an important line of research is to identify treatment approaches that are optimally effective for AUD and can lead to a decrease in circulating IL-6 levels as well.
One promising approach for treating AUD involves mindfulness-based techniques (Bowen et al., 2014; Goldberg et al., 2018; Li et al., 2017). Mindfulness refers to being aware of the present moment nonjudgmentally, a capacity that can be fostered and strengthened through formal mindfulness practice (e.g., sitting meditation, body scan, mindful yoga; Kabat-Zinn, 2013). A number of training programs have been developed that use formal mindfulness practice as a therapeutic tool, including Mindfulness-Based Stress Reduction (MBSR; Kabat-Zinn, 2013), Mindfulness-Based Cognitive Therapy (MBCT; Segal, Williams, & Teasdale, 2002), and Mindfulness-Based Relapse Prevention (MBRP; Bowen, Chawla, & Marlatt, 2010). MBRP is an 8-week, group-based intervention designed to help patients with addictive disorders to build mindful awareness of internal and external stimuli that trigger drug use. MBRP has been shown through randomized trials to effectively reduce substance use in general (Li et al., 2017) and alcohol use specifically (Bowen et al., 2014).
However, extant research investigating the impact of mindfulness-based interventions on IL-6 has produced mixed results. Mindfulness-based interventions were shown to reduce IL-6 levels from pre-intervention to 16-week follow-up in a small sample (N = 12) of alcohol dependent adults (Zgierska et al., 2008). Mindfulness-based interventions have also reduced IL-6 levels relative to both a relaxation training program with job-seeking adults (Creswell et al., 2016) and a minimal contact control with dysphoric college women (Walsh et al., 2016). Despite these encouraging results, mindfulness-based interventions have often failed to reduce IL-6 levels in pre-post analyses (Creswell et al., 2012; Gallegos et al., 2015; Zautra et al., 2008) and relative to control conditions (Bower et al., 2015; Jedel et al., 2014; Malarkey, Jarjoura, & Klatt, 2013; Oken et al., 2010).
The lack of consistent effects of mindfulness-based interventions on IL-6 does not necessarily indicate that IL-6 levels are unresponsive to mindfulness training itself. That is, group level analyses can obscure variation in outcomes across participants, some of whom may be more adherent to the training protocol than others. Indeed, research indicates that participants who are more engaged in mindfulness practice during MBRP tend to have better clinical outcomes (Bowen & Kurz, 2012; Enkema & Bowen, 2017; Grow, Collins, Harrop, & Marlatt, 2015; Roos et al., 2018). Of most relevance, Bower et al. (2015) found, in a sample of 39 breast cancer survivors, that higher mindfulness practice frequency during a 6-week mindfulness intervention was significantly associated with lower post-intervention serum IL-6 levels (controlling for pre-intervention levels). The Bower et al. results should be regarded as preliminary, however, as the analysis was post hoc and conducted with a small sample.
In the present study, we investigated whether higher levels of engagement in mindfulness practice is associated with a beneficial reduction in serum IL-6 levels, using data collected from alcohol dependent adults who received MBRP for Alcohol Dependence (MBRP-A). Our primary hypothesis was that more time engaged in mindfulness practice would predict larger pre-post reductions in IL-6. We expected this relationship to be robust to some potential demographic confounds (i.e., age, gender, and income; Irwin & Miller, 2007; Yen et al., 2017). We also explored whether this relationship would be accounted for by clinically relevant psychological processes (i.e., changes in mindful awareness, obsessive-compulsive drinking, and depressive symptoms), some of which have been previously linked to IL-6 levels (Dowlati et al., 2010; Irwin & Miller, 2007; Leclercq et al., 2012).
Method
Data were drawn from a recently conducted randomized controlled trial (RCT; Zgierska et al., 2019 [blinded for review]) testing MBRP adapted for individuals in early recovery from alcohol dependence (MBRP-A). Extensive discussion of trial design, sample characteristics, measures, and primary outcomes can be found in Zgierska et al., 2019. The study was approved by IRB and registered with ClinicalTrials.gov (#NCT01056484).
Study Participants and Design
Participants were recruited from eight treatment programs located in the Midwestern United States. Eligibility included: age ≥18 years old; English fluency; diagnosis of alcohol dependence, confirmed by Structured Clinical Interview for DSM-IV-TR (SCID; First, Spitzer, Gibbon, & Williams, 2002), with drinking “quit date” within the prior 2-14 weeks; completion of 2 or more weeks of individual and/or group outpatient therapy for alcohol dependence; and elevated perceived stress (score ≥14 on the 10-item Perceived Stress Scale; Cohen et al., 1983).
Enrolled participants (n=123) were randomized to either MBRP-A (i.e., MBRP-A adjunctive to usual care, n=64) or Waitlist (i.e., usual care only, n=59). MBRP-A entailed eight weekly, two-hour group therapy sessions, delivered by a trained, experienced therapist, following an established protocol (Zgierska et al., 2008). The MBRP-A curriculum was similar to the MBRP curriculum (Bowen et al, 2010), except that illicit drug-related terms and content were replaced with alcohol-specific equivalents. At the first session, participants receeived a meditation cushion, CDs with guided meditations, and a study binder containing session-specific handouts. Sessions followed a structured format: 1) check-in and review of home practice, 2) mindfulness practice (e.g., raisin exercise, sitting mindfulness of breath meditation, body scan, mindful walking, mindful stretching, mountain meditation, and urge surfing exercise) with subsequent exploration of participant experiences, 3) discussion of alcohol-related concepts (e.g., cravings, high-risk situations, and early warning signs of relapse) and how mindfulness may aid in the prevention of relapse, and 4) home practice assignement. Participants were asked to practice formal mindfulness techniques (e.g., mindful body scan) at home for at least 30 minutes per day, 6 days per week. Additional details about the MBRP-A intervention are described elsewhere (Zgierska et al., 2019). Outcomes were assessed at baseline (T1), 8 weeks (T2), 26 weeks (T3), and 34 weeks (T4). Participants assigned to MBRP-A received MBRP-A from T1 to T2 (immediate intervention group); participants assigned to Waitlist had the opportunity to receive MBRP-A after they completed the T3 assessment, with T3 to T4 constituting their pre-post intervention period (delayed intervention group).
To maximize statistical power, we pooled data across all participants who received MBRP-A, whether immediately after enrollment (n=64) or after the delay (n=33), and statistically controlled intervention timing (immediate or delayed MBRP-A) in our analyses (see Analytic Approach). Kuyken et al. (2010) suggested that tests of treatment-specific effects should only include participants who received a minimum dose of treatment. That is, to understand the effects associated with a treatment-specific ingredient (e.g., mindfulness practice), it is preferred to study only those participants who were adequately exposed to that treatment ingredient. Accordingly, in keeping with the prevailing definition of minimum dose in the mindfulness treatment literature (e.g., Kuyken et al., 2010; Ma & Teasdale, 2004; Teasdale et al., 2000), our primary analyses included only participants who attended at least four sessions; this resulted in a total sample of 72 participants (46 in the immediate intervention group, 26 in the delayed intervention group). However, given that five and six session cut-offs have also been used to designate a minimum mindfulness training dose (e.g., Michalak, Troje, & Heidenreich, 2011), sensitivity analyses were conducted restricted to participants who attended at least five sessions and then at least six sessions (see Analytic Approach). An additional sensitivity analysis did not restrict the sample based on attendance.
Measures
Mindfulness Attention and Awareness Scale (MAAS; Brown & Ryan, 2003).
The MAAS is a widely used measure of mindful awareness. The MAAS has a unidimensional factor structure and has demonstrated high test-retest reliability, discriminant and convergent validity, as well as clinical utility (Brown & Ryan, 2003). In this sample, MAAS Cronbach α = 0.80.
Obsessive Compulsive Drinking Scale (OCDS; Anton, Moak, & Latham, 1995).
The OCDS was used to assess the severity of obsessive-compulsive drinking (i.e., obsessive thoughts about alcohol and compulsive drinking behaviors). The OCDS is positively correlated with measures of alcohol craving and consumption and can differentiate AUD persons who have drinking relapses from those who remain abstinent (Anton et al., 1996). In this sample, OCDS Cronbach α = 0.86.
Symptom Checklist-90-Revised Depression Subscale (SCL-90-R-Dep; Derogatis, 1994).
SCL-90-R-Dep was employed to assess depressive symptom severity. The SCL-90-R-Dep is correlated with other depression measures and has high test-retest reliability and good clinical utility (Derogatis, 1994; Steer et al., 1997). Cronbach α for the SCL-90-R-Dep = 0.90.
IL-6.
Serum IL-6 was measured from a venous blood sample (concentrations were determined in duplicate using enzyme-linked immunosorbent assay [high sensitivity Quantikine ELISA, R&D Systems]).
Mindfulness practice time.
Average minutes of formal mindfulness practice/week during MBRP-A were calculated from weekly practice logs.
Alcohol use.
Average number of standard drinks per day over the final four weeks of the MBRP-A intervention was calculated with Timeline Followback data (Sobell & Sobell, 1992).
Demographics.
Gender (male coded 0; female coded 1), age, and annual income (< $35,000 coded 0; ≥ $35,000 coded 1) were obtained via a demographics questionnaire.
Analytic Approach
Data were double-entered into the MySQL database and analyzed with SPSS (Version 25) and R (Version 3.4.4). About 7.6% of the weekly practice data were missing1; following extant literature (e.g., McClintock et al., 2017), missing weekly practice data were replaced with a value of zero to assume that the participant did not engage in that form of practice in that particular week. Missing data for other variables (5.9%) were imputed with the expectation-maximization method (for discussion, see Dempster, Laird, & Rubin, 1977). Study variables were checked for outliers with the Density Based Spatial Clustering Applications with Noise (DBSCAN) method (Ester et al., 1996; Hodge & Austin, 2004); six outliers were detected (as noted in Sensitivity Analyses section below, the pattern of findings was unaltered with outliers excluded). Study variables were checked for normality with histograms and the Shapiro-Wilk test; IL-6 values were log-transformed to reduce skewness, as consistent with research in this area (e.g., Creswell et al., 2016). Normality tests implied that the other study variables were not highly skewed (Shapiro-Wilk statistics ≥ .976, ps ≥ .193).
Paired sample t-tests were used to examine changes from pre- to post-intervention. Within-group Cohen’s d effect sizes were calculated as the difference in the pre- and post-intervention means divided by the pooled SD, correcting for the dependence between means (Morris & DeShon, 2002). Difference scores (Castro-Schilo & Grimm, 2018) were calculated for IL-6, mindful awareness, obsessive-compulsive drinking, and depressive symptoms by subtracting pre-intervention scores from post-intervention scores (i.e., a higher IL-6 change score implies a poorer response).
Bivariate correlations (Pearson r) were used to examine associations between variables and to specifically test the relation between mindfulness practice time (minutes) and changes in IL-6. A regression model then examined the relation between mindfulness practice time and changes in IL-6 when controlling for intervention timing (immediate or delayed MBRP-A), age, gender, income, and changes in mindful awareness, obsessive-compulsive drinking, and depressive symptoms.
Sensitivity analyses assessed the robustness of any practice—IL-6 relationship. Specifically, we examined the association between mindfulness practice time and changes in IL-6 when: 1) excluding outliers, 2) excluding participants with any missing data, 3) controlling for post-intervention psychological covariates (mindful awareness, obsessive-compulsive drinking, and depressive symptoms) rather than difference scores, 4) controlling for psychological covariates residualized change scores rather than difference scores (see Castro-Schilo & Grimm, 2018 for a discussion), 5) controlling for alcohol consumption during last four weeks of the intervention, 6) restricting to participants who attended at least five sessions, 7) restricting to participants who attended at least six sessions, and 8) placing no restriction on session attendance.
Results
The mean age of participants was 43.4 years (SD=12.0). About 93.1% of the sample was White, 63.9% male, and 58.3% employed. About 58.3% of participants reported an annual income below $35,000, and 41.7% reported income of $35,000 or higher. Participants attended a mean of 6.42 sessions (SD=1.46) and reported a mean of 180.97 minutes (SD=63.20) of formal mindfulness practice/week during MBRP-A and a mean of 0.21 drinks/day (SD=0.50) during the final four weeks of MBRP-A.2
From pre- to post-intervention, there was an increase in mindful awareness, t(71)=2.67, p=.009, d=0.32, and decreases in obsessive-compulsive drinking, t(71)=−4.01, p<.001, d=−0.48, and depressive symptoms, t(71)=−5.49, p<.001, d=−0.66. IL-6 levels did not change from pre- to post-intervention for the whole sample, t(71)=1.12, p=.267, d=0.13; in terms of raw change, IL-6 levels increased for 59.7% and decreased for 40.3% of the sample.
Means, standard deviations, and bivariate correlations are presented in Table 1. Notably, the standard deviation for IL-6 changes (1.66) was almost five times as large as the mean (0.34), indicating that there was marked variability in IL-6 changes within the sample. Post-intervention mindful awareness and depressive symptoms were significantly associated with post-intervention IL-6 (rs=−.23 and .28, respectively; see Table 1).
Table 1.
Means, Standard Deviations, and Bivariate Correlations, n=72 (Participants Attending at Least 4 Sessions)
|
M (SD) |
1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mindfulness Practice Time (1) | 180.97 (63.20) |
--- | ||||||||||||
| IL-6 Pre (2) | 1.85 (2.59) |
.08 | --- | |||||||||||
| IL-6 Post (3) | 2.19 (3.54) |
−.15 | .65** | --- | ||||||||||
| IL-6 Change (4) | 0.34 (1.66) |
−.27* | −.45** | .39** | --- | |||||||||
| Mindful Awareness Pre (5) | 3.86 (0.93) |
−.02 | −.01 | −.04 | −.04 | --- | ||||||||
| Mindful Awareness Post (6) | 4.11 (0.80) |
.14 | −.09 | −.23* | −.16 | .59** | --- | |||||||
| Mindful Awareness Change (7) | 0.25 (0.79) |
.16 | −.09 | −.19 | −.11 | −.58** | .31* | --- | ||||||
| Obsessive-Compulsive Drinking Pre (8) | 9.19 (5.52) |
.00 | .02 | −.05 | −.09 | −.32* | −.21 | .16 | --- | |||||
| Obsessive-Compulsive Drinking Post (9) | 6.81 (4.64) |
−.01 | −.01 | .02 | .03 | −.14 | −.12 | .04 | .52** | --- | ||||
| Obsessive-Compulsive Drinking Change (10) | −2.39 (5.05) |
−.01 | −.03 | .07 | .13 | .22 | .12 | −.14 | −.62** | .35* | --- | |||
| Depressive Symptoms Pre (11) | 1.26 (0.84) |
.05 | .04 | .17 | .15 | −.59** | −.47** | .22 | .30* | .08 | −.26* | --- | ||
| Depressive Symptoms Post (12) | 0.79 (0.64) |
.05 | .22 | .28* | .06 | −.30* | −.51** | −.16 | .22 | .23* | −.03 | .54** | --- | |
| Depressive Symptoms Change (13) | −0.47 (0.73) |
−.01 | .15 | .05 | −.12 | 42** | .10 | −.40** | −.15 | .12 | .28* | −.67** | .26* | --- |
| Average Drinks/Day Last 4 Weeks of MBRP-A (14) | 0.21 (0.50) |
−.14 | .10 | −.03 | .08 | .16 | .06 | −.12 | .03 | .29* | .22 | −.19 | −.03 | .16 |
Note. Raw IL-6 scores were used to calculate means and standard deviations; log-transformed IL-6 scores were used for correlations
p<.05;
p<.001
Primary Analyses
Consistent with our primary hypothesis, mindfulness practice time was inversely associated with changes in IL-6 (r=−.27, p=.022; see Table 1 and scatterplot in Figure 1). The association of practice time with IL-6 changes remained significant (β=−.34, p=.004) when controlling for intervention timing (immediate or delayed MBRP-A), age, gender, income, and changes in mindful awareness, obsessive-compulsive drinking, and depressive symptoms (see Table 2). Income level was the only other significant predictor of IL-6 changes in the model (β=−.34, p=.004; see Table 2).
Figure 1.
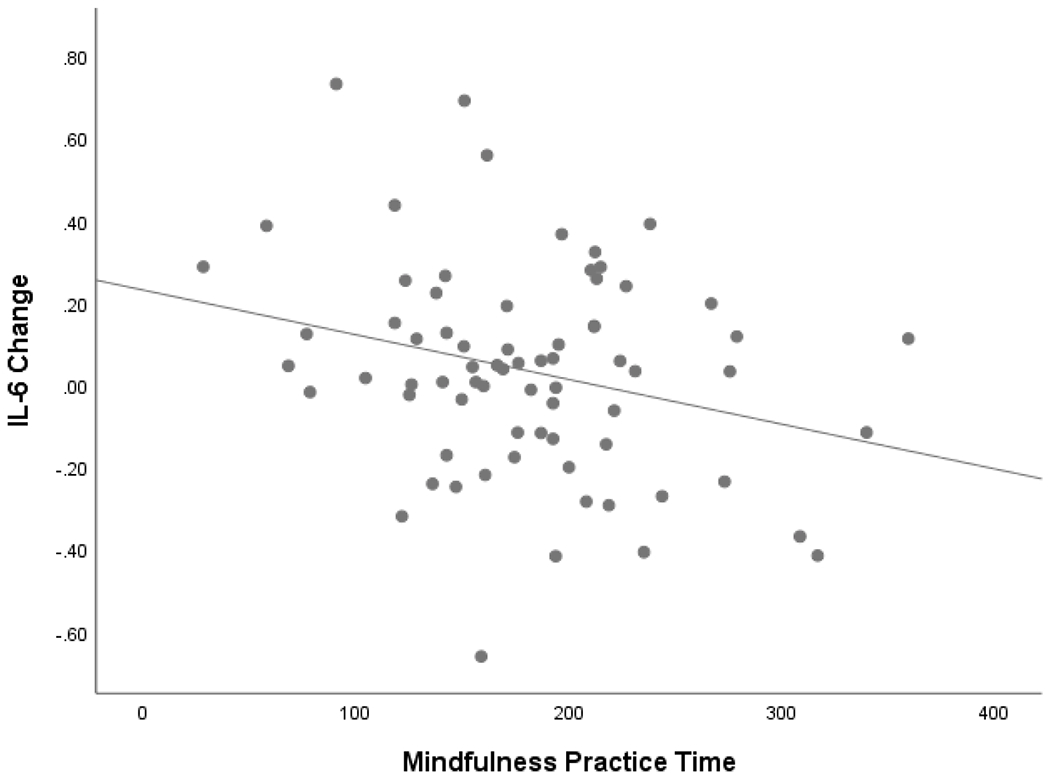
Scatterplot Mindfulness Practice Time by IL-6 Change, n=72 (Participants Attending at Least 4 Sessions).
Note. Log-transformed IL-6 scores were used for scatterplot.
Table 2.
Regression Analysis, n=72 (Participants Attending at Least 4 Sessions)
| Criterion | Predictors | β | t | p |
|---|---|---|---|---|
| IL-6 Change | ||||
| Mindfulness Practice Time | −.34 | −2.98 | .004 | |
| Intervention Timing | .10 | 0.85 | .396 | |
| Age | −.06 | −0.49 | .627 | |
| Gender | .14 | 1.19 | .238 | |
| Income | −.34 | −2.99 | .004 | |
| Mindful Awareness Change | −.14 | −1.11 | .270 | |
| Obsessive-Compulsive Drinking Change | .13 | 1.04 | .301 | |
| Depressive Symptoms Change | −.11 | −0.88 | .381 |
Note. Log-transformed IL-6 scores were used in regression analysis; intervention timing (received MBRP-A immediately or after delay)
Sensitivity Analyses
The results of sensitivity analyses are shown in Table 3. Mindfulness practice time remained a significant predictor of IL-6 changes when: 1) excluding outliers (n=66), 2) excluding participants with any missing data (n=63), 3) controlling for post-intervention (rather than changes in) mindful awareness, obsessive-compulsive drinking, and depressive symptoms (n=72), 4) controlling for residualized change scores rather than difference scores (n=72), 5) controlling for average drinks/day during last four weeks of the intervention (n=72), 6) only including participants who attended at least five sessions (n=60), and 7) only including participants who attended at least six sessions (n=53). However, setting a minimum treatment dose (i.e., with four, five, or six session cut-offs) appeared to be critically important; when placing no restriction on session attendance (n=97), mindfulness practice time did not significantly predict IL-6 changes.
Table 3.
Regression Sensitivity Analyses
| Criterion | Predictors | β | t | p |
|---|---|---|---|---|
| Model excluding outliers (n=66) and including mindfulness practice time, intervention timing, age, gender, income, mindful awareness change, obsessive-compulsive drinking change, and depressive symptoms change | ||||
| IL-6 Change | Mindfulness Practice Time | −.25 | −2.12 | .039 |
| Model excluding participants with any missing data (n=63) and including mindfulness practice time, intervention timing, age, gender, income, mindful awareness change, obsessive-compulsive drinking change, and depressive symptoms change | ||||
| IL-6 Change | Mindfulness Practice Time | −.33 | −2.57 | .013 |
| Model (n=72) including mindfulness practice time, intervention timing, age, gender, income, post-intervention mindful awareness, post-intervention obsessive-compulsive drinking, and post-intervention depressive symptoms | ||||
| IL-6 Change | Mindfulness Practice Time | −.35 | −2.98 | .004 |
| Model (n=72) including mindfulness practice time, intervention timing, age, gender, income, mindful awareness RCS, obsessive-compulsive drinking RCS, and depressive symptoms RCS | ||||
| IL-6 RCS | Mindfulness Practice Time | −.31 | −2.74 | .008 |
| Model (n=72) including mindfulness practice time, intervention timing, and average drinks/day last four weeks of MBRP-A | ||||
| IL-6 Change | Mindfulness Practice Time | −.38 | −3.17 | .002 |
| Model with participants attending at least five sessions (n=60) and including mindfulness practice time, intervention timing, age, gender, income, mindful awareness change, obsessive-compulsive drinking change, and depressive symptoms change | ||||
| IL-6 Change | Mindfulness Practice Time | −.42 | −3.50 | .001 |
| Model with participants attending at least six sessions (n=53) and including mindfulness practice time, intervention timing, age, gender, income, mindful awareness change, obsessive-compulsive drinking change, and depressive symptoms change | ||||
| IL-6 Change | Mindfulness Practice Time | −.43 | −3.36 | .002 |
| Model without session restriction (n=97) and including mindfulness practice time, intervention timing, age, gender, income, mindful awareness change, obsessive-compulsive drinking change, and depressive symptoms change | ||||
| IL-6 Change | Mindfulness Practice Time | −.16 | −1.23 | .198 |
Note. Log-transformed IL-6 scores were used in all regression sensitivity analyses; intervention timing (received MBRP-A immediately or after delay); RCS = residualized change scores
Discussion
The current study examined whether higher levels of engagement in mindfulness meditation practice was associated with larger reductions in serum IL-6 levels among alcohol dependent adults receiving a mindfulness-based intervention designed to prevent alcohol relapse (MBRP-A). Among participants who received a minimum dose of treatment (i.e., at least four sessions of MBRP-A; Kuyken et al., 2010; Ma & Teasdale, 2004; Teasdale et al., 2000), results indicated that more mindfulness practice during MBRP-A was significantly associated with reduced IL-6 levels. This association was of small-to-moderate magnitude (r = −.27) by Cohen’s (1988) standards and persisted when controlling for a number of potential confounds including intervention timing (immediate or delayed MBRP-A), demographic characteristics (age, gender, and income), and changes in several psychological variables (mindful awareness, obsessive-compulsive drinking, and depressive symptoms). Further, practice time remained a significant predictor of IL-6 reductions across six sensitivity analyses modifying: the definition of minimum treatment dose (i.e., at least five sessions or at least six sessions), the management of outliers and missing data, and the modeling of psychological covariates. This relationship was no longer significant when omitting the minimum treatment dose requirement. Given that this link between practice and IL-6 appeared to be relatively robust and that inflammatory cytokines are likely mediators in the development of alcohol-related illnesses (Yen et al., 2017), our results underscore the potential value of future larger-scale research investigating the effects of mindfulness training engagement on inflammatory activity and health conditions associated with AUD.
Descriptive analyses revealed that participants were generally compliant with mindfulness homework. The mean amount of practice (i.e., about 181 minutes/week) was close to MBRP-A’s practice recommendation (i.e., at least 180 minutes/week) as well as the average amount of practice reported in a recent meta-analysis of MBSR and MBCT studies (i.e., 174 minutes/week; Parsons et al., 2017). Psychological improvements were also observed over the course of MBRP-A; self-reported mindful awareness significantly increased and obsessive-compulsive drinking and depressive symptoms significantly decreased from pre- to post-treatment; these effects (ds=0.32, −0.48, and −0.66, respectively) are comparable in size to ones documented in recent meta-analyses of mindfulness-based interventions for substance use disorders (Goldberg et al., 2018; Li et al., 2017).
Interestingly, despite significant pre-post improvements in self-reported outcomes, we did not observe a significant pre-post reduction in IL-6 levels, which is consistent with three previous studies (Creswell et al., 2012; Gallegos et al., 2015; Zautra et al., 2008). Rather, changes in IL-6 were highly variable, with some participants showing an improvement and others appearing to have worse IL-6 over time.
Our primary aim was to explain this between-person variability in IL-6 changes. We found some evidence that the between-person variability in IL-6 changes may be attributable to the between-person variability in mindfulness practice, a putative “active ingredient” of MBRP-A. Specifically, in our two main analyses using participants who received a minimum treatment dose, mindfulness practice time accounted for between 7.3 and 11.6% of the variability in IL-6 changes. These results complement a previous report (Bower et al., 2015) suggesting that individual differences in engagement with mindfulness training may predict changes in AUD-related inflammatory cytokine activity. Future studies could determine (perhaps experimentally by manipulating practice dosage) if increased mindfulness practice plays a causal role in reducing inflammatory cytokine activity, improving immune health, and attenuating risk for physical health conditions associated with elevated IL-6 (e.g., cancer, heart and liver diseases; Cohen et al., 2011; Danesh et al., 2008; Grivennikov & Karin, 2011).
Although mindfulness practice time was significantly related to IL-6 changes in the primary analyses and across six sensitivity analyses, it was not significantly related to IL-6 changes in the model that did not place a restriction on session attendance. This result suggests that mindfulness practice may have little-to-no association with IL-6 among participants who received an inadequate dose of mindfulness training, as defined by Kuyken et al. (2010) and others (e.g., Ma & Teasdale, 2004; Teasdale et al., 2000). One theoretical possibility is that mindfulness practice functions differently for those who attend an adequate number of MBRP-A sessions perhaps due to a deeper understanding of mindfulness and mindfulness practices that change the nature of the relationship between home practice and inflammatory activity. Perhaps the quality of these participants’ home practice differs, leading to different physiological outcomes (Goldberg, Del Re, Hoyt, & Davis, 2014). Of course, these interpretations are speculative and need additional empirical scrutiny.
Of note, income level was negatively associated with IL-6 changes in the full regression model, indicating that higher income participants showed larger IL-6 reductions. It could be fruitful to examine income (or socioeconomic status) as a moderator of treatment effects in future studies using a randomized design. Mindful awareness and depressive symptoms were also significantly associated with IL-6 at post-intervention, suggesting potential links between these psychological variables and inflammatory physiology. However, alcohol consumption and changes in mindful awareness, obsessive-compulsive drinking, and depressive symptoms were not significantly related to IL-6 changes. While it did not appear to be the case in the current analyses, it may be worthwhile examining in a larger sample whether changes in these or other psychological variables mediate the link between practice time and reduced IL-6. One possibility is that the link between practice time and reduced IL-6 is mediated by a specific facet of mindfulness, like acceptance or nonreactivity (Baer, Smith, Hopkins, Krietemeyer, & Toney, 2006). Another potential mediator is stress, which has been previously linked to mindfulness practice engagement (Carmody & Baer, 2008) and IL-6 levels (Dowlati et al., 2010). Identifying psychological processes underlying benefits could be valuable in treatment development and clinical practice. For example, patients in mindfulness training could be routinely monitored (Wampold, 2015) with respect to processes that are known to mediate the beneficial effects of mindfulness training on inflammatory physiology.
A number of limitations of the current study should be acknowledged. First, with 72 participants, our study was likely underpowered for detecting small effects. Second, participants were predominantly White, and so caution is advised before generalizing the current findings to people of color. Third, of the 59 participants assigned to Waitlist, only 33 accepted the invitation to participate in MBRP-A, which may have introduced self-selection bias and led to an unrepresentative sample. Fourth, while we statistically controlled for intervention timing (immediate or delayed MBRP-A), it may nonetheless be the case that this pooling introduced unmeasured variability that influenced our results. Fifth, although conducted within the context of an RCT, our study did not experimentally manipulate the extent of mindfulness practice time. An experimental design that randomizes participants to standard MBRP-A or MBRP-A with little-to-no practice homework could provide a more rigorous test of mindfulness practice effects on IL-6. On the other hand, there are several notable strengths of this study including a clinically-relevant AUD sample, the use of multi-method assessment (e.g., IL-6 levels measured from serum; practice time measured with self-report), and the focus on an important biomarker (IL-6) implicated in cancer, heart and liver diseases, and premature death.
Our results indicate that alcohol dependent adults have varied IL-6 responses to MBRP-A. We found some evidence that these individual differences in IL-6 response may be partly attributable to differential levels of engagement with mindfulness training. Notably, the association between mindfulness practice time and IL-6 response was detected only when including participants who received a minimum treatment dose, suggesting that it is critical that participants both attend at least 50% of the training sessions and adhere to the home practice assignments in order to achieve a better IL-6 response. The present results highlight the need for larger-scale research examining the benefits of mindfulness training engagement for reducing inflammatory activity and the health problems associated with AUDs.
Highlights.
In MBRP-A, mindfulness practice time predicted pre-post changes in serum IL-6.
Practice—IL-6 link remained when controlling demographic/psychological variables.
Results imply that practice engagement predicts changes in inflammatory activity.
Acknowledgments
Funding: The study was supported by the K23AA017508 award from the National Institutes of Health (NIH) National Institute on Alcohol Abuse and Alcoholism awarded to the fourth author and by the Clinical and Translational Science Award (CTSA) program through the NIH National Center for Advancing Translational Sciences (NCATS) grant UL1TR000427. The first author was supported by research fellowship T32HP10010. The second author was supported by the University of Wisconsin-Madison, Office of the Vice Chancellor for Research and Graduate Education with funding from the Wisconsin Alumni Research Foundation.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Regarding participants who attended fewer than four sessions (n=25), about 9.1% of the weekly practice data were missing.
Regarding participants who attended fewer than four sessions (n=25), mean age was 38.6 years (SD=10.4). About 80.0% of this sample was White, 40.0% male, and 52.0% employed. About 76.0% of participants reported an annual income below $35,000, and 24.0% reported income of $35,000 or higher. These participants attended a mean of 1.67 sessions (SD=0.96) and reported a mean of 94.49 minutes (SD=104.50) of formal mindfulness practice/week during MBRP-A and a mean of 0.30 drinks/day (SD=0.96) during the final four weeks of MBRP-A.
Declarations of interest: none
Contributor Information
Andrew S. McClintock, University of Wisconsin-Madison.
Simon B. Goldberg, University of Wisconsin-Madison.
Christopher L. Coe, University of Wisconsin-Madison.
Aleksandra E. Zgierska, University of Wisconsin-Madison.
References
- Achur RN, Freeman WM, & Vrana KE (2010). Circulating cytokines as biomarkers of alcohol abuse and alcoholism. Journal of Neuroimmune Pharmacology, 5, 83–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anton RF, Moak DFL, & Latham P (1995). The Obsessive Compulsive Drinking Scale: A self-rated instrument for the quantification of thoughts about alcohol and drinking behavior. Alcoholism: Clinical and Experimental Research, 19, 92–99. [DOI] [PubMed] [Google Scholar]
- Anton RF, Moak DFL, & Latham PK (1996). The obsessive compulsive drinking scale: a new method of assessing outcome in alcoholism treatment studies. Archives of General Psychiatry, 53, 225–231. [DOI] [PubMed] [Google Scholar]
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, & Toney L (2006). Using self-report assessment methods to explore facets of mindfulness. Assessment, 13, 27–45. [DOI] [PubMed] [Google Scholar]
- Bowen S, Chawla N, & Marlatt A (2010). Mindfidness-based relapse prevention for addictive behaviors: A clinician’s guide. New York, NY: Guilford Press. [Google Scholar]
- Bowen S, & Kurz AS (2012). Between- session practice and therapeutic alliance as predictors of mindfulness after mindfulness- based relapse prevention. Journal of Clinical Psychology, 68, 236–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen S, Witkiewitz K, Clifasefi SL, Grow J, Chawla N, Hsu SH, … & Larimer ΜE (2014). Relative efficacy of mindfulness-based relapse prevention, standard relapse prevention, and treatment as usual for substance use disorders: A randomized clinical trial. JAMA Psychiatry, 71, 547–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bower JE, Crosswell AD, Stanton AL, Crespi CM, Winston D, Arevalo J, … & Ganz PA (2015). Mindfulness meditation for younger breast cancer survivors: A randomized controlled trial. Cancer, 121, 1231–1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown KW, Ryan RM, & Creswell JD (2007). Mindfulness: Theoretical foundations and evidence for its salutary effects. Psychological Inquiry, 18, 211–237. [Google Scholar]
- Castro-Schilo L, & Grimm KJ (2018). Using residualized change versus difference scores for longitudinal research. Journal of Social and Personal Relationships, 35, 32–58. [Google Scholar]
- Cohen J (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale, NJ: Erlbaum. [Google Scholar]
- Cohen JC, Horton JD, & Hobbs ΗH (2011). Human fatty liver disease: Old questions and new insights. Science, 332, 1519–1523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R (1983). A global measure of perceived stress. J Health Soc Behav, 24, 385–396. [PubMed] [Google Scholar]
- Creswell JD, Irwin MR, Burklund LJ, Lieberman MD, Arevalo JM, Ma J, … & Cole SW (2012). Mindfulness-based stress reduction training reduces loneliness and pro-inflammatory gene expression in older adults: A small randomized controlled trial. Brain, Behavior, and Immunity, 26, 1095–1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creswell JD, Taren AA, Lindsay EK, Greco CM, Gianaros PJ, Fairgrieve A, … & Ferris JL (2016). Alterations in resting-state functional connectivity link mindfulness meditation with reduced interleukin-6: A randomized controlled trial. Biological Psychiatry, 80, 53–61. [DOI] [PubMed] [Google Scholar]
- Danesh J, Kaptoge S, Mann AG, Sarwar N, Wood A, Angleman SB, … & Gudnason V (2008). Long-term interleukin-6 levels and subsequent risk of coronary heart disease: Two new prospective studies and a systematic review. PLoS Medicine, 5, e78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dempster AP, Laird NM, & Rubin DB (1977). Maximum likelihood from incomplete data via the EM algorithm. Journal of the Royal Statistical Society, Series B (methodological), 1–38. [Google Scholar]
- Derogatis LR (1994). SCL-90-R: Administration, scoring, and procedures manual (3rd ed.). Minneapolis, MN: NCS Pearson. [Google Scholar]
- Dowlati Y, Herrmann N, Swardfager W, Liu H, Sham L, Reim EK, & Lanctot KL (2010). A meta-analysis of cytokines in major depression. Biological Psychiatry, 67, 446–457. [DOI] [PubMed] [Google Scholar]
- Enkema MC, & Bowen S (2017). Mindfulness practice moderates the relationship between craving and substance use in a clinical sample. Drug and Alcohol Dependence, 179, 1–7. [DOI] [PubMed] [Google Scholar]
- Ester M, Kriegel HP, Xu X (1996). A density-based algorithm for discovering clusters in large spatial datasets with noise. Processings of the 2nd ACM International Conference on Knowledge Discovery and Data Mining (KDD), Portalnd, OR. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW (2002). Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Non-patient Edition New York, NY: Biometrics Research, New York State Psychiatric Institute. [Google Scholar]
- Gallegos AM, Lytle MC, Moynihan JA, & Talbot NL (2015). Mindfulness-based stress reduction to enhance psychological functioning and improve inflammatory biomarkers in trauma-exposed women: A pilot study. Psychological Trauma: Theory, Research, Practice and Policy, 7, 525–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg SB, Del Re AC, Hoyt WT, & Davis JM (2014). The secret ingredient in mindfulness interventions? A case for practice quality over quantity. Journal of Counseling Psychology, 61, 491–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg SB, Tucker RP, Greene PA, Davidson RJ, Wampold BE, Kearney DJ, & Simpson TL (2018). Mindfulness-based interventions for psychiatric disorders: A systematic review and meta-analysis. Clinical Psychology Review, 59, 52–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grivennikov SI, & Karin M (2011). Inflammatory cytokines in cancer: Tumour necrosis factor and interleukin 6 take the stage. Annals of the Rheumatic Diseases, 70, i104–8. [DOI] [PubMed] [Google Scholar]
- Grow JC, Collins SE, Harrop EN, & Marlatt GA (2015). Enactment of home practice following mindfulness-based relapse prevention and its association with substance-use outcomes. Addictive Behaviors, 40, 16–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Stinson FS, Ogburn E, & Grant BF (2007). Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry, 64, 830–842. [DOI] [PubMed] [Google Scholar]
- Hodge V, & Austin J (2004). A survey of outlier detection methodologies. Artificial Intelligence Review, 22, 85–126. [Google Scholar]
- Irwin MR, & Miller AH (2007). Depressive disorders and immunity: 20 years of progress and discovery. Brain, Behavior, and Immunity, 21, 374–383. [DOI] [PubMed] [Google Scholar]
- Jedel S, Hoffman A, Merriman P, Swanson B, Voigt R, Rajan KB, … & Keshavarzian A (2014). A randomized controlled trial of mindfulness-based stress reduction to prevent flare-up in patients with inactive ulcerative colitis. Digestion, 89, 142–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabat-Zinn J (2013). Full catastrophe living (revised edition): Using the wisdom of your body and mind to face stress, pain, and illness. New York, NY: Bantam Books. [Google Scholar]
- Kuyken W, Watkins E, Holder E, White K, Taylor RS, Byford S, … & Teasdale JD (2010). How does mindfulness-based cognitive therapy work? Behaviour Research and Therapy, 48, 1105–1112. [DOI] [PubMed] [Google Scholar]
- Leclercq S, Cani PD, Neyrinck AM, Stärkel P, Jamar F, Mikolajczak M, … & de Timary P (2012). Role of intestinal permeability and inflammation in the biological and behavioral control of alcohol-dependent subjects. Brain, Behavior, and Immunity, 26, 911–918. [DOI] [PubMed] [Google Scholar]
- Li W, Howard MO, Garland EL, McGovern P, & Lazar M (2017). Mindfulness treatment for substance misuse: A systematic review and meta-analysis. Journal of Substance Abuse Treatment, 75, 62–96. [DOI] [PubMed] [Google Scholar]
- Ma SH, & Teasdale JD (2004). Mindfulness-based cognitive therapy for depression: Replication and exploration of differential relapse prevention effects. Journal of Consulting and Clinical Psychology, 72, 31. [DOI] [PubMed] [Google Scholar]
- Malarkey WB, Jarjoura D, & Klatt M (2013). Workplace based mindfulness practice and inflammation: A randomized trial. Brain, Behavior, and Immunity, 27, 145–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClintock AS, Brown R, Coe CL, Zgierska A, & Barrett B (2019). Mindfulness practice and stress following mindfulness-based stress reduction: Examining within-person and between-person associations with latent curve modeling. Mindfulness, doi: 10.1007/si2671-019-01159-x. [DOI] [Google Scholar]
- Michalak J, Troje N, & Heidenreich T (2011). The effects of mindfulness-based cognitive therapy on depressive gait patterns. Journal of Cognitive and Behavioral Psychotherapies, 11, 13–27. [Google Scholar]
- Morris SB, & DeShon RP (2002). Combining effect size estimates in meta-analysis with repeated measures and independent-groups designs. Psychological Methods, 7, 105–125. [DOI] [PubMed] [Google Scholar]
- Neupane SP (2016). Neuroimmune interface in the comorbidity between alcohol use disorder and major depression. Frontiers in Immunology, 7, 655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oken BS, Fonareva I, Haas M, Wahbeh H, Lane JB, Zajdel D, & Amen A (2010). Pilot controlled trial of mindfulness meditation and education for dementia caregivers. The Journal of Alternative and Complementary Medicine, 16, 1031–1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons CE, Crane C, Parsons L,J, Fjorback LO, & Kuyken W (2017). Home practice in mindfulness-based cognitive therapy and mindfulness-based stress reduction: A systematic review and meta-analysis of participants’ mindfulness practice and its association with outcomes. Behaviour Research and Therapy, 95, 29–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehm J, Dawson D, Frick U, Gmel G, Roerecke M, Shield KD, & Grant B (2014). Burden of disease associated with alcohol use disorders in the United States. Alcoholism: Clinical and Experimental Research, 38, 1068–1077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, & Patra J (2009). Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. The Lancet, 373, 2223–2233. [DOI] [PubMed] [Google Scholar]
- Room R, Babor T, & Rehm J (2005). Alcohol and public health. Lancet, 365, 519–530. [DOI] [PubMed] [Google Scholar]
- Roos CR, Kirouac M, Stein E, Wilson AD, Bowen S, & Witkiewitz K (2018). An open trial of rolling admission mindfulness-based relapse prevention (rolling MBRP): Feasibility, acceptability, dose-response relations, and mechanisms. Mindfidness, 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segal ZV, Williams JMG, & Teasdale JD (2002). Mindfidness-basedcognitive therapy for depression. New York, NY: Guilford Publications. [Google Scholar]
- Sobell LC, & Sobell MB (1992). Timeline Followback: A technique for assessing self-reported alcohol consumption In Litten RZ & Allen J (Eds). Measuring alcohol consumption: psychosocial and biological methods. New Jersey: Humana Press. [Google Scholar]
- Steer RA, Ball R, Ranieri WF, & Beck AT (1997). Further evidence for the construct validity of the Beck Depression Inventory-II with psychiatric outpatients. Psychological Reports, 80, 443–446. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (2018). 2017 National Survey on Drug Use and Health: Detailed Tables. Rockville, MD. [PubMed] [Google Scholar]
- Teasdale JD, Segal ZV, Ridgeway VA, & Soulsby JM (2000). Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. Prevention, 68, 615–623. [DOI] [PubMed] [Google Scholar]
- Walsh E, Eisenlohr-Moul T, & Baer R (2016). Brief mindfulness training reducsed salivarity IL-6 and TNF-α in young women with depressive symptomatology. Journal of Consulting and Clinical Psychology, 84, 887–897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wampold BE (2015). Routine outcome monitoring: Coming of age - with the usual developmental challenges. Psychotherapy, 52, 458–462. [DOI] [PubMed] [Google Scholar]
- Wassel CL, Barrett-Connor E, & Laughlin GA (2010). Association of circulating C-reactive protein and interleukin-6 with longevity into the 80s and 90s: The Rancho Bernardo Study. The Journal of Clinical Endocrinology & Metabolism, 95, 4748–4755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yen CH, Ho PS, Yeh YW, Liang CS, Kuo SC, Huang CC, … & Lu RB (2017). Differential cytokine levels between early withdrawal and remission states in patients with alcohol dependence. Psychoneuroendocrinology, 76, 183–191 [DOI] [PubMed] [Google Scholar]
- Zautra AJ, Davis MC, Reich JW, Nicassio P, Tennen H, Finan P, … & Irwin MR (2008). Comparison of cognitive behavioral and mindfulness meditation interventions on adaptation to rheumatoid arthritis for patients with and without history of recurrent depression. Journal of Consulting and Clinical Psychology, 76, 408–421. [DOI] [PubMed] [Google Scholar]
- Zgierska A, Burzinski CA, Mundt MP, McClintock AS, Cox J, Coe C, … & Fleming M (2019). Mindfulness-based relapse prevention for alcohol dependence: Findings from a randomized controlled trial. Journal of Substance Abuse Treatment, 100, 8–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zgierska A, Rabago D, Zuelsdorff M, Coe C, Miller M, & Fleming M (2008). Mindfulness meditation for alcohol relapse prevention: A feasibility pilot study. Journal of Addiction Medicine, 2, 165–173. [DOI] [PMC free article] [PubMed] [Google Scholar]


